Abstract
Background
Emergency intubation carries a higher risk of complications than elective airway management. Video laryngoscopy (VL) could potentially improve patient safety. The goal of this study was to determine whether VL is superior to direct laryngoscopy for the emergency intubation of adults in the inpatient setting.
Methods
Pertinent studies were retrieved by a systematic literature search in the MEDLINE, Embase, and CENTRAL databases. The selection of studies, data extraction, and assessment of the potential for bias were carried out independently by two of the authors. Effect sizes were reported as odds ratios (OR) or mean differences (MD). The primary endpoint was successful intubation at the first attempt. Further variables were considered as secondary endpoints.
Results
1098 titles and abstracts were retrieved, and the full texts of 43 articles were examined. Eight randomized and controlled trials, with a total of 1796 patients, were analyzed. VL was not found to confer any statistically significant advantage with respect to successful intubation at the first attempt (OR 0.72, 95% confidence interval [0.47; 1.12]) or with respect to the time to successful intubation (MD -8.99 seconds [-24.00; 6.01]). On the other hand, the use of VL was significantly associated with a lower number of intubation attempts (MD -0.17 [-0.31; -0.03]) and with a lower frequency of esophageal intubation (OR 0.27 [0.10; 0.75]).
Conclusion
The routine use of VL for airway management in emergency medicine might improve patient safety, as VL is associated with a lower number of intubation attempts and with a lower frequency of esophageal intubation. Further randomized controlled trials are needed before any definitive conclusions can be drawn about the advantages of video laryngoscopy.
Airway management is a life-saving measure for severely injured and critically ill patients. According to the German Trauma Surgery Society (Deutsche Gesellschaft für Unfallchirurgie), 22% of severely injured patients admitted to hospitals via the emergency room in 2016 were intubated at the site of injury and a further 15% in the emergency room itself. Of the patients transferred to the intensive care unit, 39% were intubated and mechanically ventilated (1). There are no recent data revealing the absolute number of emergency intubations in the hospital setting in Germany.
The standard procedure for securing the airway is endotracheal intubation by means of conventional direct laryngoscopy (DL). Despite the unpredictability and urgency of emergency intubation, the success rate of DL usually exceeds 85% (2, 3). However, intubation safety may be affected by the short preparation time, the possible lack of control over events in the vicinity, the varying degree of training of the persons performing the intubation, and the patient’s unstable state and lowered cardiorespiratory reserves. Compared with elective intubation, emergency intubation is therefore associated with an elevated risk of procedure-related complications and severe adverse events such as aspiration, a fall in oxygen saturation, or even death.
There are indications of a strongly positive correlation between the number of intubation attempts and the rate of complications (4, 5). To increase the safety of intubation, therefore, the number of intubation attempts should be minimized and the first-pass success rate maximized. Video laryngoscopy (VL) may be advantageous in this regard because it visualizes the vocal cord level indirectly by means of an inbuilt camera and a video screen, thus significantly improving the view of the glottis (6). For this reason, VL has proved to be particularly beneficial for less experienced users and in patients with difficult airways (7). Moreover, VL can be used in the event of failure to achieve intubation with DL (8).
Recent systematic reviews of the use of VL in emergency airway management have concerned themselves with studies from one of two areas: out-of-hospital emergency medicine (9) or intensive care (10– 12). There are no systematic reviews based on randomized controlled trials from the emergency room or a combination of the two hospital settings (emergency department and intensive care unit). Therefore, in order to accurately reflect the complex clinical reality of hospital emergency intubation, characterized by heterogeneity of settings, devices, and levels of training, we included studies from both the emergency room and the intensive care unit in our review.
The results of the three recent systematic reviews point to superiority of VL. The difference is not statistically significant, however, as only three (10), five (11), and four (12) randomized controlled trials were included. Some of these studies excluded patients with difficult airways and are therefore not representative of clinical practice.
Our aim was to determine whether or not video laryngoscopy is superior to direct laryngoscopy for emergency intubation of adults in the hospital setting.
Methods
This systematic review was performed in line with the recommendations of the Cochrane Handbook for Systematic Reviews of Interventions (Cochrane Handbook) (13) and the PRISMA Statement (14). It was registered with PROSPERO (CRD42017065015) (15).
Inclusion criteria
We included randomized controlled trials that compared video laryngoscopy and direct laryngoscopy for urgent intubation of adults in the hospital setting and reported data for at least one of the predefined endpoints. Our primary endpoint was successful intubation at the first attempt. The following variables were used as secondary endpoints: overall success of intubation, number of attempts at intubation, time to successful intubation, and complications or serious adverse events.
Literature survey
The databases MEDLINE, Embase, and CENTRAL (Cochrane Central Register of Controlled Trials) were searched for relevant studies. The search strategy (eTable 1) was formed of relevant keywords and trade names and an RCT filter (RCT, randomized controlled trial) provided by the Cochrane Collaboration (16). No restrictions were imposed on language, publication date, or publication type. All searches were last updated in November 2017. Additional information on screening and other sources of data can be found in eBox 1.
eTable 1. Search strategies for database search.
|
Database (date of first search) |
Search strategy |
|
MEDLINE (24 May 2017) |
(Video[TiAb] OR Video-laryngoscopy[TiAb] OR videolaryngoscopy[TiAb] OR videolaryngoscope[TiAb] OR ‧videolaryngoscopies[TiAb] OR videolaryngoscopes[TiAb] OR video laryngoscopy[TiAb] OR ‧video-laryngoscope[TiAb] OR video laryngoscope[TiAb] OR video-laryngoscopes[TiAb] OR ‧video ‧laryngoscopes[TiAb] OR video-laryngoscopies[TiAb] OR video laryngoscopies[TiAb] OR GlideScope[TiAb] OR ‧Verathon[TiAb] OR C-MAC[TiAb] OR CMAC[TiAb] OR AWS-S200[TiAb] OR McGrath[TiAb] OR STORZ[TiAb] OR “McGrath MAC”[TiAb] OR MAC[TiAb] OR EMS[TiAb] OR “Infinium ClearVue”[TiAb] OR UESCOPE[TiAb] OR ‧“UE Medical”[TiAb] OR ‧IntuBrite[TiAB] OR Marshall[TiAb] OR “VLS 6630”[TiAB] OR MEDAN[TiAb] OR ‧APA[TiAb] OR Coopdech[TiAb] OR VLP-100[TiAb] OR Venner Medical[TiAb] OR Kanlife[TiAb] OR ‧PENTAX[TiAb] OR ‧Novamed[TiAb] OR Pentax-AWS[TiAb] OR “King Vision”[TiAb] OR CoPilot[TiAb] OR ‧Rusch[TiAb] OR Airtraq[TiAb] OR “Truview PCD”[TiAb]) AND (laryngoscop*[TiAb] OR ‧“laryngoscopy”[MeSh Terms] OR direct laryngoscopy[TiAb] OR direct ‧laryngoscope[TiAb] OR ‧direct ‧laryngoscopies[TiAb] OR direct laryngoscopes[TiAb] OR macintosh[TiAb] OR ‧standard ‧laryngoscope[TiAb] OR standard laryngoscopes[TiAb] OR standard laryngoscopy[TiAb] OR ‧conventional ‧laryngoscopy[TiAb] OR conventional laryngoscope[TiAb] OR conventional laryngoscopes[TiAb]) AND (randomized controlled trial[Publication Type] OR controlled clinical trial[Publication Type] OR randomized[TiAb] OR ‧randomised[TiAb] OR placebo[TiAb] OR “drug therapy”[Subheading] OR randomly[TiAb] OR trial[TiAb] OR groups[TiAb] NOT (“animals”[MeSh terms] NOT “humans”[MeSh terms])) |
|
Embase (24 May 2017) |
(‚video‘:ti,ab OR ‚video-laryngoscopy‘:ti,ab OR ‚videolaryngoscopy‘:ti,ab OR ‚videolaryngoscope‘:ti,ab OR ‧‚videolaryngoscopies‘:ti,ab OR ‚videolaryngoscopes‘:ti,ab OR ‚video laryngoscopy‘:ti,ab OR ‧‚video-laryngoscope‘:ti,ab OR ‚video laryngoscope‘:ti,ab OR ‚video-laryngoscopes‘:ti,ab OR ‧‚video ‧laryngoscopes‘:ti,ab OR ‚video-laryngoscopies‘:ti,ab OR ‚video laryngoscopies‘:ti,ab OR ‚glidescope‘:ti,ab OR ‧‚verathon‘:ti,ab OR ‚c-mac‘:ti,ab OR ‚cmac‘:ti,ab OR ‚aws-s200‘:ti,ab OR ‚mcgrath‘:ti,ab OR ‚storz‘:ti,ab OR ‚mcgrath mac‘:ti,ab OR ‚mac‘:ti,ab OR ‚ems‘:ti,ab OR ‚infinium clearvue‘:ti,ab OR ‚uescope‘:ti,ab OR ‚ue ‧medical‘:ti,ab OR ‧‚intubrite‘:ti,ab OR ‚marshall‘:ti,ab OR ‚vls 6630‘:ti,ab OR ‚medan‘:ti,ab OR ‚apa‘:ti,ab OR ‧‚coopdech‘:ti,ab OR ‚vlp-100‘:ti,ab OR ‚venner medical‘:ti,ab OR ‚kanlife‘:ti,ab OR ‚pentax‘:ti,ab OR ‧‚novamed‘:ti,ab OR ‚pentax-aws‘:ti,ab OR ‚king vision‘:ti,ab OR ‚copilot‘:ti,ab OR ‚rusch‘:ti,ab OR ‚airtraq‘:ti,ab OR ‚truview pcd‘:ti,ab) AND ‧(‚laryngoscop*‘:ti,ab OR ‚laryngoscopy‘/de OR ‚direct laryngoscopy‘:ti,ab OR ‧‚direct ‧laryngoscope‘:ti,ab OR ‚direct ‧laryngoscopies‘:ti,ab OR ‚direct laryngoscopes‘:ti,ab OR ‚macintosh‘:ti,ab OR ‚standard laryngoscope‘:ti,ab OR ‧‚standard laryngoscopes‘:ti,ab OR ‚standard laryngoscopy‘:ti,ab OR ‧‚conventional laryngoscopy‘:ti,ab OR ‧‚conventional laryngoscope‘:ti,ab OR ‚conventional laryngoscopes‘:ti,ab) AND (‚crossover procedure‘:de OR ‧‚double-blind procedure‘:de OR ‚randomized controlled trial‘:de OR ‧‚single-blind ‧procedure‘:de OR random*:de,ab,ti OR factorial*:de,ab,ti OR crossover*:de,ab,ti OR (cross NEXT/1 over*):de,ab,ti OR placebo*:de,ab,ti OR (doubl* ‧NEAR/1 blind*):de,ab,ti OR (singl* ‧NEAR/1 blind*):de,ab,ti OR assign*:de,ab,ti OR allocat*:de,ab,ti OR volunteer*:de,ab,ti) |
|
CENTRAL (24 May 2017) |
#1 MeSH descriptor: [Laryngoscopy] #2 “video”:ti,ab #3 Video-laryngoscopy:ti,ab #4 „videolaryngoscopy“:ti,ab #5 videolaryngoscope:ti,ab #6 videolaryngoscopies:ti,ab #7 videolaryngoscopes:ti,ab #8 video laryngoscopy:ti,ab #9 video-laryngoscope:ti,ab #10 video laryngoscope:ti,ab #11 video-laryngoscopes:ti,ab #12 video laryngoscopes:ti,ab #13 video-laryngoscopies:ti,ab #14 video laryngoscopies:ti,ab #15 GlideScope:ti,ab #16 Verathon:ti,ab #17 C-MAC:ti,ab #18 CMAC:ti,ab #19 AWS-S200:ti,ab #20 McGrath:ti,ab #21 STORZ:ti,ab #22 McGrath MAC:ti,ab #23 “MAC EMS”:ti,ab #24 UE Medical:ti,ab #47 (#3 or #39 or #40 or #41 or #42 or #43 or #44 or #45 or #46) and (#1 or #2 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29 or #30 or #31 or #32 or #33 or #34 or #35 or #36 or #37 or #38) |
eBOX 1. Other sources and literature screening.
The reference lists of relevant systematic reviews and studies were hand-searched for further potentially eligible randomized controlled trials. Furthermore, ClinicalTrials.gov was searched for ongoing or not yet published studies, and Google Scholar was scrutinized for gray literature.
Two authors (TR, DP) independently examined the titles and abstracts of the identified records, reading the full text if necessary, to determine whether the publications fulfilled the inclusion criteria. Discrepancies were resolved by face-to-face discussion. All eligible studies were selected for qualitative synthesis. Those in which the results regarding the endpoints were reported in a fashion suitable for statistical analysis were also selected for quantitative synthesis (meta-analysis). If any necessary data were missing, the authors of the study concerned were contacted by e-mail.
Data extraction and assessment of risk of bias
Two authors (TR, DP) independently recorded data on study characteristics and results using standardized data extraction sheets. The risk of bias for the included studies was evaluated by means of the Cochrane Collaboration’s tool for assessing risk of bias in randomized trials (13), and any disagreements were resolved by face-to-face discussion. If further information was needed, the authors of the study concerned were contacted by e-mail.
Data synthesis and analysis
All statistical analyses (for detailed information see eBox 2) were carried out with the Review Manager software (RevMan, version 5.3; Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014).
eBOX 2. Statistical analysis.
Preplanned subgroup analyses were conducted for all endpoints for which the studies were analyzed separately according to setting or type of video laryngoscope used. Moreover, a subgroup analysis was carried out to compare studies with self-defined experienced operators (at least second-year resident) to those with less well trained users. Furthermore, a sensitivity analysis excluding studies with a high risk of bias was performed to verify the robustness of the findings.
A random-effects model was used for analysis, and 95% confidence intervals (CI) were calculated for all effect sizes. The I2 statistic was used to measure heterogeneity among the results of the different studies. Broadly, values of 0 to 40% indicated low, 30 to 60% moderate, 50 to 90% high, and 75 to 100% very high heterogeneity. A funnel plot was generated to assess the risk of publication bias.
The effect sizes for dichotomous endpoints were expressed as odds ratios (OR; Mantel–Haenszel method) and continuous endpoints as mean differences (MD; inverse variance method).
Results
Study selection and characteristics
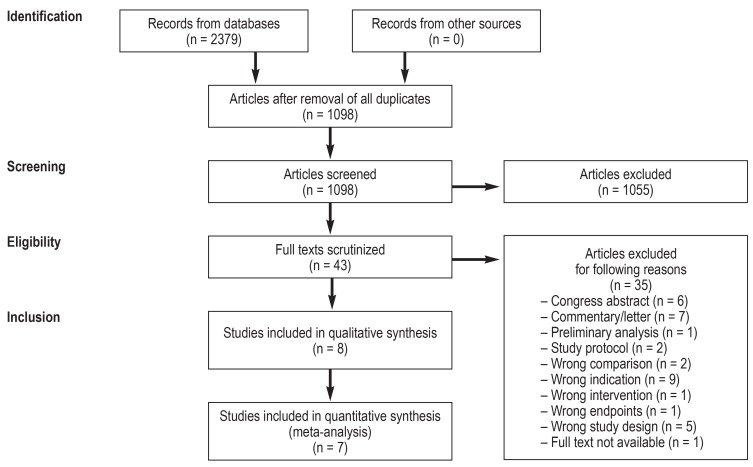
Figure 1 presents the systematic literature search and study selection process. The electronic database search identified 2379 records; no further records were retrieved from other sources. After removal of duplicates, we screened the titles/abstracts of the remaining 1098 records and assessed 43 full texts. Of these 43 publications, 33 articles and 2 abstracts (Janz D, Semler M, Lentz R, et al.: Randomized trial of video laryngoscopy for endotracheal intubation of critically ill adults. Crit Care Med 2015; 43 (12 Suppl. 1): 212–3; Silverberg M, Li N, Kory P: Efficacy of video laryngoscopy vs. direct laryngoscopy during urgent endotracheal intubation: a randomized controlled trial. Chest 2013; 144 [4 meeting abstract], no pagination) were excluded for various reasons (e1– e33), leaving 8 randomized controlled trials (17– 24) with a total of 1796 patients for analysis. All study authors were contacted, but not all ambiguities could be resolved. As a result, one study that did not provide absolute numbers of patients analyzed per group had to be excluded from the meta-analysis (24).
Figure 1.
PRISMA flow chart
One half of the studies were performed in emergency departments, the other half in intensive care units. The intubators’ experience ranged from novices to experienced anesthesiologists, and the indications for intubation also varied among the studies. Some studies excluded patients who were known or could be anticipated to have difficult airways, an immobilized cervical spine, maxillofacial trauma, or cardiac arrest (19, 22– 24). The patients were given sedatives or hypnotics in all studies. In all but one study (22) muscle relaxants were administered. No study was industrially sponsored, but most of them were funded by their institution or by national funding bodies. Apart from one study (18), they were all registered with ClinicalTrials.gov. Detailed information on study characteristics can be found in Table 1.
Table 1. Study characteristics.
| Study | Location | Setting | Recruitment | Patients*1 (VL/DL) |
Age (mean ± SD) |
Men (%) | Type of laryngoscope |
Experience of operator*8 |
Indication for intubation *2 |
Exclusion criteria |
| Driver 2016 (17) |
Minneapolis, USA |
ER | Nov 2011 – Feb 2013 |
198 (103/95) |
VL: 52.6 ± 17.1 DL: 51.6 ± 18.8 |
VL: 60 DL: 66 |
VL: C-MAC DL: C-MAC*5 |
94% PGY 3 or greater |
Altered mental state/ AW protection 64 vs. 55% |
Pregnancy, imprisonment, DL not planned for first ‧attempt |
| Goksu 2016 (18) |
Antalya, Turkey |
ER | May 2013 – Oct 2014 |
150 (75/75) |
VL: 39 ± 19 DL: 35 ± 15.5 |
VL: 93.3 DL: 97.3 |
VL: C-MAC DL: Macintosh |
PGY 3 (median) | Head injury 40 vs. 27% |
Penetrating trauma, age <16 years, already ‧intubated on arrival |
| Griesdale 2012 (19) |
Vancouver, Canada |
ITU | Aug 2009 – Jan 2011 |
40 (20/20) |
VL: 68 ± 16 DL: 61 ± 16 |
VL: 75 DL: 65 |
VL: GlideScope DL: Macintosh |
PGY 2 (median) | Respiratory failure 70 vs. 50% |
Preceding cardiac arrest, ‧CS support, suspicion of difficult AW (among others) |
| Janz 2016 (20) |
Nashville, USA |
ITU | Feb 2014 – Feb 2015 |
150 (74 /76) |
VL: 59 (49–68)*3 DL: 60 (51–67)* 3 |
VL: 63.5 DL: 57.9 |
VL: McGrath*6 DL: Macintosh*7 |
PCCM fellows | Respiratory failure*10 54 vs. 59% |
Waking intubation planned, other procedure preferred |
| Lascarrou 2017 (21) |
Multicenter, France |
ITU | May 2015 – Dec 2015 |
371 (186/185) |
VL: 62.7 ± 15.3 DL: 62.8 ± 16.3 |
VL: 65.6 DL: 61.1 |
VL: McGrath DL: Macintosh |
84% non-‧expert*9 | Neurological emergency 38 vs. 41% |
Unstable CS, ‧pregnancy, imprisonment, age <18 years (among others) |
| Silverberg 2015 (22) |
New York, USA |
ITU | Not reported | 117 (57/60) |
VL: 65.4 DL: 69.6 |
VL: 45 DL: 57 |
VL: GlideScope DL: Macintosh, Miller |
PGY 4 to 8 | Not reported | Suspicion of difficult AW, oxygen saturation <92% |
| Sulser 2016 (23) |
Zurich, Switzerland |
ER | Nov 2014 – Dec 2015 |
150 (75/75) |
VL: 53 ± 21 DL: 54 ± 17 |
VL: 68 DL: 55 |
VL: C-MAC DL: Macintosh |
PGY 7 or greater | Mild trauma*11 39% overall |
Severe facial injury, unstable CS, ongoing resuscitation (among others) |
| Yeatts 2013 (24) |
Baltimore, USA |
ER | Jul 2008 – May 2010 |
623 (303/320) |
VL: 42 (18–119)*4 DL: 43 (18–94)*4 |
VL: 71.3 DL: 76.3 |
VL: GlideScope DL: Macintosh |
PGY 2 (median) | Severe CI 51 vs. 48% |
Thyroid/facial injury, CS injury, cardiac arrest |
*1Randomized, *2most frequent, *3median and interquartile distance, *4mean and range, *5with concealed screen, *6in 99% of cases; a GlideScope was used in the other 1%, *7 in 93% of cases; a laryngoscope with Miller blade was used in the other 7%, *8according to the American system, *9made the first intubation attempt, *10hypoxic or hypercapnic, *11including injuries of the extremities
AW, airway; CI, cognitive impairment; CS, cervical spine; DL, direct laryngoscopy; ER, emergency room; ITU, intensive care unit; PCCM, pneumonology and critical care medicine; PGY, postgraduate year; SD, standard deviation;
VL, videolaryngoscopy
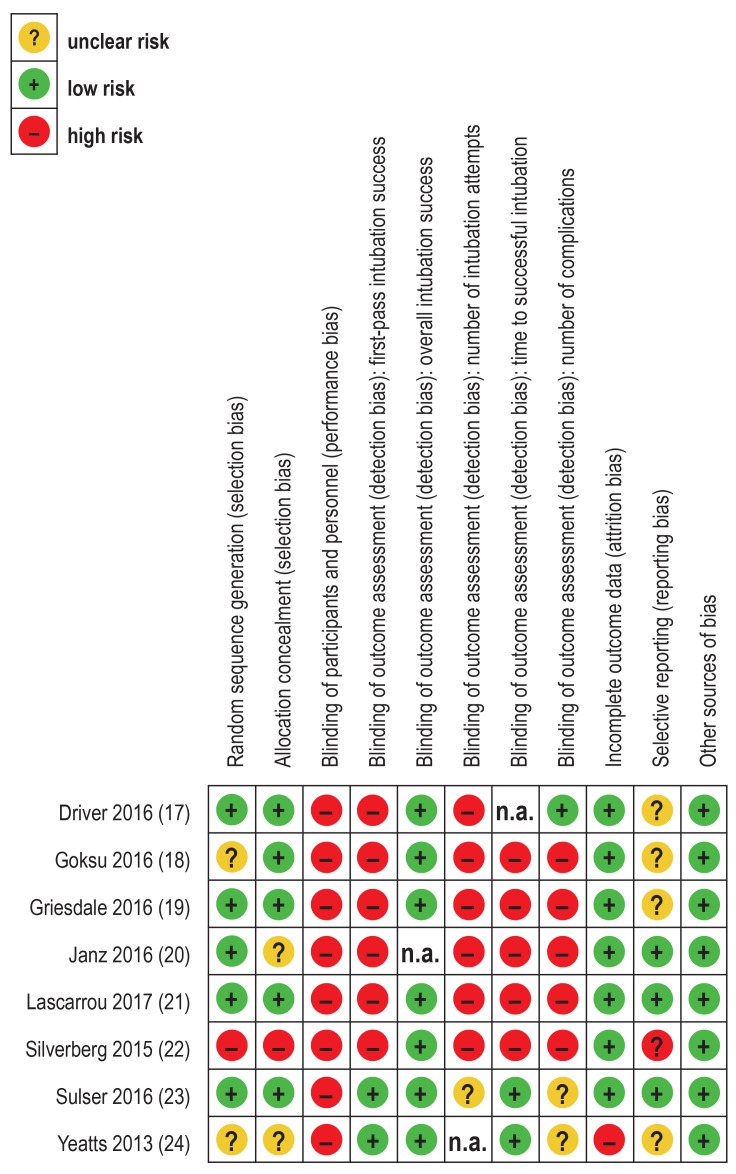
Risk of bias
Overall, the risk of bias of the included studies was moderate (efigure 1). In one study the randomization sequence was not properly generated and group allocation was not concealed (22). However, randomization was carried out correctly in all other studies, so altogether the risk of selection bias was low. Owing to the nature of the intervention, it was not possible to blind the intubators or other study personnel. Hence, the risk of performance bias was high for all studies and all endpoints. The risk of detection bias was also high, unless waveform capnography was used to determine the endpoints objectively. Given the short time spans between randomization, intubation, and endpoint measurement, no or only very little information regarding endpoints or study discontinuation was missing. The risk of attrition bias was therefore low, except in one study that reported relatively high rates of missing data (24). The risk of reporting bias was low for all studies for which a study protocol was provided (20, 21, 23); it remained unclear for the remaining studies (17– 19, 22, 24). Other sources of bias were not found.
eFigure 1.
Assessment of the risk of bias in the included studies. n.a., not applicable
Results
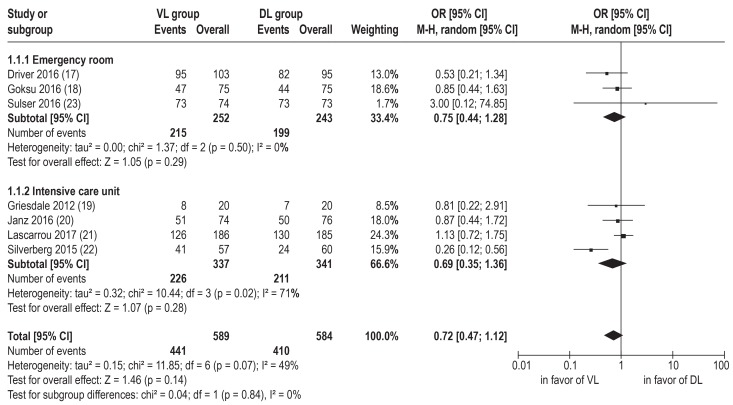
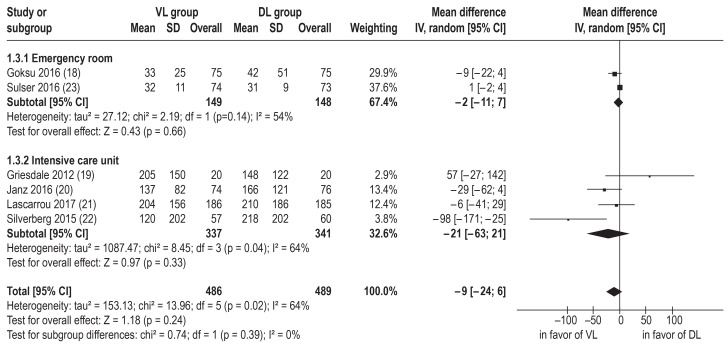
There was no difference in first-pass intubation success rate between video laryngoscopy and direct laryngoscopy (p = 0.14); however, the data point to superiority of video laryngoscopy (OR 0.72, 95% confidence interval [CI] [0.47; 1.12], n = 1173 (17– 23), I2= 49%) (figure 2).
Figure 2.
Meta-analysis of first-pass intubation success: studies divided by setting.
DL, direct laryngoscopy; M-H, Mantel–Haenszel method; OR, odds ratio; VL, video laryngoscopy; 95% CI, 95% confidence interval
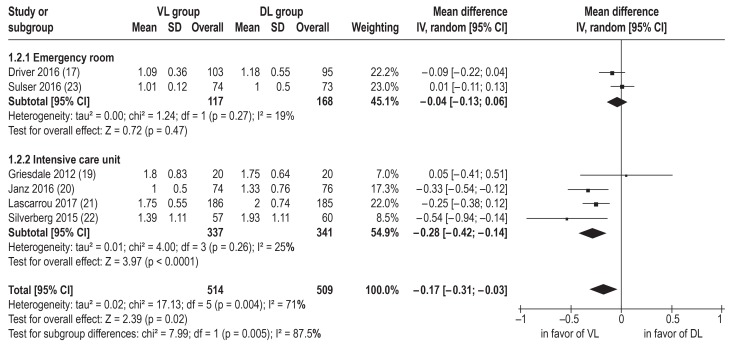
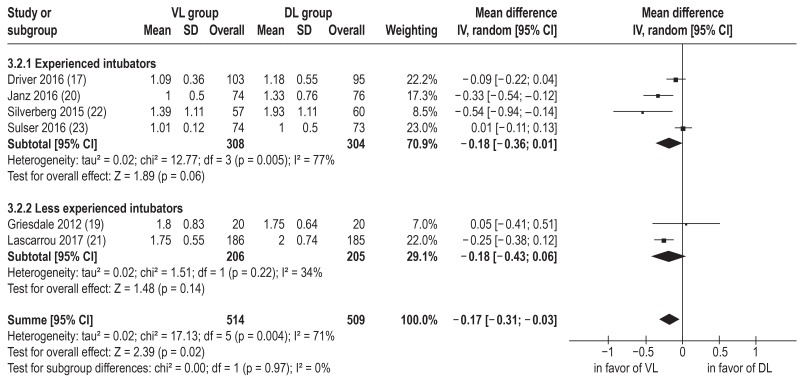
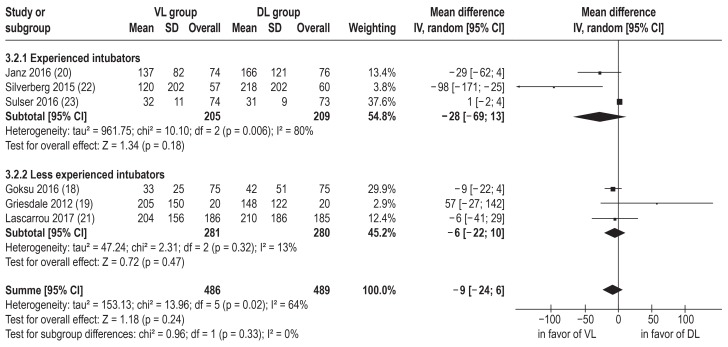
Because the overall intubation success rate in four (19, 21– 23) of the five studies that reported this endpoint was 100% for either one of the two intubation techniques, the study results for this endpoint were not subjected to meta-analysis. In the remaining study (18), 92% of patients in the VL group and 96% in the DL group were intubated. The number of intubation attempts was lower for video laryngoscopy than for direct laryngoscopy in intensive care studies (MD -0.28 [-0.42; -0.14], n = 678, I2 = 25%), but not in emergency room studies (MD -0.04 [-0.13; 0.06], n = 345, I2 = 19%). Overall, however, the number of intubation attempts was lower for video laryngoscopy than for direct laryngoscopy (MD -0.17 [-0.31; -0.03], n = 1023 (17, 19–23), I2 = 71%) (figure 3). No effect of video laryngoscopy was observed on the time to successful intubation (MD -8.99 s [-24.00; 6.01], n = 975 (18–23), I2 = 64%) (efigure 2).
Figure 3.
Meta-analysis of number of intubation attemps studies divided by setting.
DL, direct laryngoscopy; IV, inverse variance method; SD, standard deviation; VL, video laryngoscopy; 95% CI, 95% confidence interval
eFigure 2.
Meta-analysis of time to successful intubation in seconds: studies divided by setting.
DL, direct laryngoscopy; IV, inverse variance method; SD, standard deviation; VL, video laryngoscopy; 95% CI, 95% confidence interval
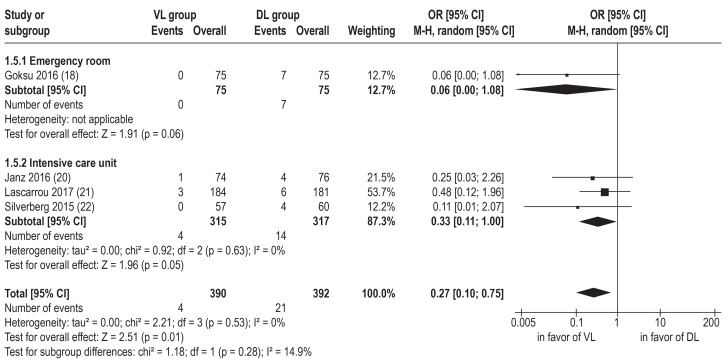
The following complications were reported in at least two studies: airway trauma, dental injuries, aspiration, cardiac arrest, death during intubation, esophageal intubation, hypoxemia, and hypotension (eTable 2). However, the number of studies with adequate reporting of data on airway trauma, dental injuries, aspiration, cardiac arrest, and death during intubation was not high enough for meta-analysis. Because the threshold values for the occurrence of hypoxemia and hypotension varied across studies, only the role of video laryngoscopy in esophageal intubation could be analyzed. Video laryngoscopy lowered the incidence of this complication (OR 0.27 [0.10; 0.75], n = 782 [18, 20–22], I2 = 0%) (figure 4).
eTable 2. Endpoint results of included studies (video laryngoscopy vs. direct laryngoscopy).
| Study |
First-pass success rate |
Overall success rate |
Intubation attempts Ø |
Time to successful intubation |
Airway trauma*1 |
Aspiration |
Cardiac arrest |
Death*2 |
Esophageal intubation |
Hypoxemia | Hypotension |
| Driver 2016 (17) | 92.2 vs. 86.3% |
Not reported | 1.1 (1.0–1.2) vs. 1.2 (1.1–1.3) |
Not reported | Not reported | Not reported | Not reported | Not reported | Not reported | 25.2 vs. 27.3% SaO 2 <93% |
Not reported |
| Goksu 2016 (18) | 62.7 vs. 58.7% |
92 vs. 96% |
Not reported | 33.4 ± 25 vs. 42.4 ± 51 s |
Not reported | Not reported | Not reported | Not reported | 0 vs. 9.3% |
33 vs. 48% SaO 2 <90% |
Not reported |
| Griesdale 2012 (19) | 40 vs. 35% |
100 vs. 100% |
1.8 vs. 1.75 |
221 [103–291] vs. 156 [67–220] s |
Not reported | Not reported | Not reported | 0 vs. 0% |
Not reported | SaO2*3 86vs. 95% |
mmHg*3 81 vs. 77 |
| Janz 2016 (20) | 68.9 vs. 65.8% |
Not reported | 1 [1–1] vs. 1 [1–2] |
126 [89–197] vs. 153 [93–253] s |
1.4 vs. 0% |
1.4 vs. 1.3% |
1.4 vs. 1.3% |
Not reported | 1.4 vs. 5.3% |
19.4 vs. 21.1% SaO2 <80% |
10.8 vs. 9.2% <80 mmhg |
| Lascarrou 2017 (21) | 67.7 vs. 70.3% |
100 vs. 100% |
1 {1–4} vs. 1 {1–5} |
3 [2–4] vs. 3 [2–4] min |
0 vs. 0.6% |
2.2 vs. 2.2% |
2.2 vs. 0% |
0.5 vs. 0% |
1.6 vs. 3.3% |
8.1 vs. 10.9% SaO 2 <90% |
4.4 vs. 2.2% <90 mmhg |
| Silverberg 2015 (22) | 74 vs. 40% |
100 vs. 100% |
1.39 vs. 1.93 |
120 vs. 218 s |
Not reported | 9 vs. 7% |
Not reported | Not reported | 0 vs. 7% |
4 vs. 8% SaO 2 <80% |
11 vs. 13% <70 mmhg |
| Sulser 2016 (23) | 99 vs. 100% |
100 vs. 100% |
1.01 vs. 1 |
32 ± 11 vs. 31 ± 9 s |
0 vs. 0% |
Not reported | Not reported | Not reported | 0 vs. 0% |
1 ± 2% vs. 1 ± 2%*4 |
Not reported |
| Yeatts 2013 (24) | 80 vs. 81% |
Not reported | Not reported | 71.0 (65.3–76.7) vs. 56.5 (51.1–62.0) s |
0 vs. 0% |
0 vs. 0% |
Not reported | Not reported | Not reported | 50 vs. 24% SaO 2 <80%*5 |
Not reported |
*1 Including dental injuries, *2 during intubation, *3 minimum, *4 maximal decrease in SaO2, *5 for a subgroup of patients with severe head injuries
() contain 95% confidence intervals for a mean, [] contain the interquartile range for a median, {} contain the range for a median, ± shows the standard deviation of a mean.
Some values had to be converted for entry into RevMan for meta-analysis. To permit estimation of the standard deviation of a mean based on a 95% confidence interval, an equation from the Cochrane Handbook was used (Higgins JPT, Green S [eds.]: Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available at http://handbook.cochrane.org.). To estimate a mean and standard deviation on the basis of a median and interquartile range, equations from Wan et al. were used (Wan X, Wang W, Liu J, Tong T: Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range, BMC Med Res Methodol 2014; 14: 135.) For estimation of a standard ?deviation based on the mean and a p value, the RevMan pocket calculator was used (available at training.cochrane.org).
Figure 4.
Meta-analysis of esophageal intubation: studies divided by setting.
DL, direct laryngoscopy; M-H, Mantel–Haenszel method; OR, odds ratio; VL, video laryngoscopy; 95% CI, 95% confidence interval
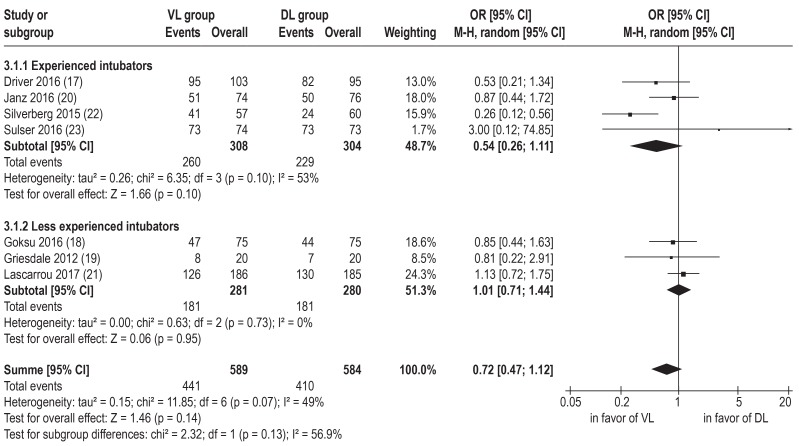
No differences for any endpoint were found among different video laryngoscopy devices (C-MAC, GlideScope, McGrath; data not shown) or among intubators with differing amounts of experience (eFigures 3– 5).
In the course of the planned sensitivity analysis, one study was excluded from meta-analysis because it had a high risk of selection bias and was also the only study in which patients did not routinely receive muscle relaxants and for which the first-pass intubation success rate of direct laryngoscopy was strikingly low (22). Exclusion of this study had no impact on statistical significance (not shown), but the heterogeneity of first-pass intubation success rate was reduced to I2 = 0%.
In an additional sensitivity analysis, the study excluded due to persisting ambiguities (24) was included in the meta-analysis under the assumption of even distribution of the missing data. However, the overall results were not significantly altered (OR for first-pass intubation success rate 0.79 [0.55; 1.13], MD of time to successful intubation -2.49 s [-14.48; 9.49]).
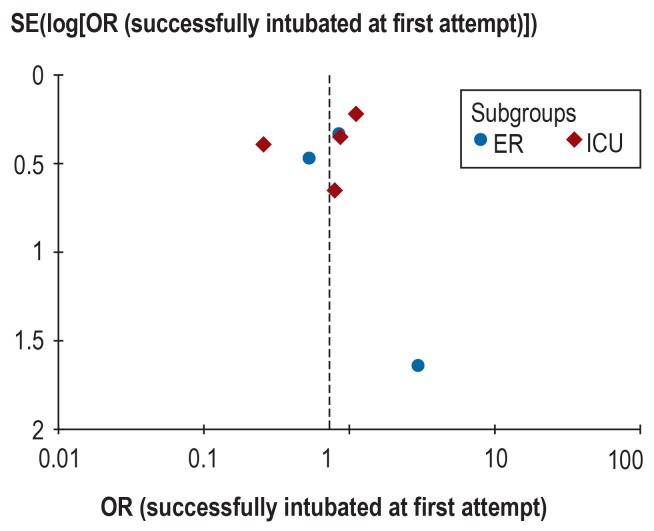
Because fewer than 10 studies were analyzed, publication bias was assessed only by visual evaluation of the funnel plot (eFigure 6). The distribution of results for the primary endpoint seemed to be relatively symmetrical, but nevertheless the risk of publication bias remains unclear.
eFigure 6.
Funnel plot of study results with regard to successful first-pass intubation; studies divided by setting.
ICU, intensive care unit; ER, emergency room; OR, odds ratio
Discussion
We evaluated the results of eight randomized controlled trials that compared video laryngoscopy to direct laryngoscopy in adult patients who required emergency airway management in the emergency room or intensive care unit. These studies included a total of 1796 patients, in most of whom there was no reason to expect difficult airways. The risk of bias was moderate.
No statistically significant difference was found between video laryngoscopy and direct laryngoscopy with regard to the primary endpoint of this systematic review, the first-pass success rate for intubation. However, video laryngoscopy reduced the number of intubation attempts and the rate of esophageal intubation: in every sixth patient, an additional intubation attempt was avoided. The number of treatments needed to prevent one esophageal intubation was 24.
Strengths and limitations
One strength of our review is its systematic, predetermined nature. Clinical heterogeneity among the studies as a result of different settings or use of different devices for video laryngoscopy was assessed in subgroup analyses. With regard to the primary endpoint, however, the effect size for emergency room studies (OR 0.75) scarcely differed from that for studies in the intensive care unit (OR 0.69). Furthermore, the calculated effect sizes were not decisively altered by supplementary sensitivity or subgroup analyses, which speaks for their robustness.
Despite our extensive literature search, we found only a small number of relevant randomized controlled trials. Moreover, no ongoing or not yet published studies were registered at ClinicalTrials.gov. The risk of bias of the eight studies included was elevated by the fact that it would hardly have been feasible to blind the study personnel to the type of laryngoscope used. While the risk of other forms of bias was relatively low, the risks of performance bias and detection bias were classed as high for most of the endpoints. Given the particularly critical circumstances in the case of emergency intubation, despite the lack of blinding it is unlikely that the patients were treated dissimilarly or the endpoints systematically measured differently. Apart from the training level of the operator, the setting, and the type of video laryngoscopy device used, there were also other differences among the studies for which no adjustment was possible. Therefore, the findings of our analysis may have been influenced by differences in intubation practice (e.g, in preoxygenation or neuromuscular blockade), by the indication for intubation, or by the definitions of the endpoints. Furthermore, the patients’ basic characteristics were comparable only to a limited degree. The proportion of patients with difficult airways, for instance, was not reported by all studies, which prevented systematic comparison of this variable. Among the studies that reported it, however, there was no difference between the VL and DL groups.
Only one study (24) reported how long video laryngoscopy had already been in use in the authors’ institution. In common with regular airways training, however, duration of use is a factor that may influence individual performance, but could not be considered in our analysis because the available data did not permit quantification. Furthermore, the meta-analyses included no correction for multiple testing, because there is currently no established standard method for tackling this problem. Possible solutions are being debated (25).
Comparison with other systematic reviews
Huang et al. (11) and Zhao et al. (12) have recently published meta-analyses of randomized controlled trials carried out in intensive care units. Their results are in accordance with ours: the first-pass intubation success rate was not significantly improved (p = 0.35 and 0.27) or the time to successful intubation shortened (p = 0.08 and 0.69) by video laryngoscopy, but the incidence of esophageal intubation was reduced (p = 0.03 in both meta-analyses). Neither study investigated the effect of video laryngoscopy on the overall intubation success rate or the number of intubation attempts.
Summary
Video laryngoscopy seems to reduce the number of intubation attempts and the rate of esophageal intubation, so its use in emergency airway management could potentially increase patient safety. Video laryngoscopy also tended to be superior to direct laryngoscopy in terms of first-pass intubation success rate, but the difference was not statistically significant. Moreover, this finding was for patients who in most cases exhibited no evidence of difficult airways. Consequently, no conclusions can be drawn with regard to patients with difficult airways. Neither can routine use of video laryngoscopy be definitively recommended for urgent intubation of adults in the hospital setting, at least until future research, e.g., randomized controlled trials, provides unequivocal evidence.
The clinical perspective. Compared with direct laryngoscopy, video laryngoscopy improves visualization at the level of the vocal cords. For this reason, video laryngoscopy has become established as a useful method particularly in patients with difficult airways, in whom visualization of the glottis is limited. However, no fundamental treatment advantage, independent of operator experience, patient group, or specific intubation scenario, has yet been demonstrated for video laryngoscopy.
For emergency airway management, conventional direct laryngoscopy is still viewed as the gold standard. If both a direct and a video laryngoscope are available for urgent intubation in the hospital setting, the staff member carrying out the laryngoscopy should always choose the technique with which they are more familiar for the first intubation attempt. It must be borne in mind, however, that video laryngoscopy has proved useful in circumstances where direct laryngoscopy is difficult, e.g., limited cervical reclination capacity. In such a case, or if intubation with a direct laryngoscope has failed, use of a video laryngoscope can be considered.
Should intubation also not be achieved with a video laryngoscope, an algorithm-based procedure is recommended to ensure adequate oxygenation. A return to spontaneous breathing is often not possible in the context of emergency intubation, and in this event face-mask ventilation, use of extraglottic airway aids, or surgical airway management are temporary alternatives to intubation.
Video laryngoscopes with Macintosh blades can also be used as direct laryngoscopes and thus combine the advantages of both procedures. This can be useful for training purposes or for rapidly switching from one technique to the other.
Key messages.
Airway management is a life-saving measure in severely injured and seriously ill patients. However, it is associated with an increased risk of complications.
This is the first systematic review and meta-analysis of randomized controlled studies from intensive care units and emergency rooms.
No statistically significant difference was found between the different kinds of video laryngoscopy devices.
The first-pass intubation success rate was not statistically significantly improved by video laryngoscopy. However, video laryngoscopy was associated with fewer intubation attempts and a lower rate of esophageal intubation and might thus enhance patient safety.
Since some of the studies analyzed did not report the proportion of patients with difficult airways, or excluded such patients, the efficacy of video laryngoscopy in this group could not be explicitly assessed.
eFigure 3.
Subgroup analysis of first-pass intubation success: studies divided by intubators’ level of training.
DL, direct laryngoscopy; M-H, Mantel–Haenszel method; OR, odds ratio; VL, video laryngoscopy; 95% CI, 95% confidence interval
eFigure 4.
Subgroup analysis of number of intubation attempts: studies divided by intubators’ level of training
DL, direct laryngoscopy; IV, inverse variance method; SD, standard deviation; VL, video laryngoscopy; 95% CI, 95% confidence interval
eFigure 5.
Subgroup analysis of time to successful intubation: studies divided by intubators’ level of training
DL, direct laryngoscopy; IV, inverse variance method; SD, standard deviation; VL, video laryngoscopy; 95% CI, 95% confidence interval
Acknowledgments
Translated from the original German by the authors and David Roseveare
Acknowledgment
The authors thank Kirsten Hüllebrand for her expert clinical advice.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists.
References
- 1.Deutsche Gesellschaft für Unfallchirurgie. TraumaRegister DGU Jahresbericht 2017. www.traumaregister-dgu.de/fileadmin/user_upload/traumaregister-dgu.de/docs/Downloads/TR-DGU-Jahresbericht_2017.pdf(last accessed on 30 November 2017) [Google Scholar]
- 2.Sakles JC, Mosier JM, Chiu S, Keim SM. Tracheal intubation in the emergency department: a comparison of GlideScope(R) video laryngoscopy to direct laryngoscopy in 822 intubations. J Emerg Med. 2012;42:400–405. doi: 10.1016/j.jemermed.2011.05.019. [DOI] [PubMed] [Google Scholar]
- 3.Mosier JM, Whitmore SP, Bloom JW, et al. Video laryngoscopy improves intubation success and reduces esophageal intubations compared to direct laryngoscopy in the medical intensive care unit. Crit Care. 2013;17 doi: 10.1186/cc13061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mort TC. Emergency tracheal intubation: complications associated with repeated laryngoscopic attempts. Anesth Analg. 2004;99:607–613. doi: 10.1213/01.ANE.0000122825.04923.15. [DOI] [PubMed] [Google Scholar]
- 5.Sakles JC, Chiu S, Mosier J, Walker C, Stolz U. The importance of first pass success when performing orotracheal intubation in the emergency department. Acad Emerg Med. 2013;20:71–78. doi: 10.1111/acem.12055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lewis SR, Butler AR, Parker J, Cook TM, Smith AF. Videolaryngoscopy versus direct laryngoscopy for adult patients requiring tracheal intubation. Cochrane Database Syst Rev. 2016;11 doi: 10.1002/14651858.CD011136.pub2. Cd011136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Griesdale DEG, Liu D, McKinney J, Choi PT. Glidescope video-laryngoscopy versus direct laryngoscopy for endotracheal intubation: a systematic review and meta-analysis. Can J Anesth. 2012;59:41–52. doi: 10.1007/s12630-011-9620-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Aziz MF, Brambrink AM, Healy DW, et al. Success of intubation rescue techniques after failed direct laryngoscopy in adults. Anesthesiology. 2016;125:656–666. doi: 10.1097/ALN.0000000000001267. [DOI] [PubMed] [Google Scholar]
- 9.Savino PB, Reichelderfer S, Mercer MP, Wang R, Sporer KA. Direct versus video laryngoscopy for prehospital intubation: a systematic review and meta-analysis. Acad Emerg Med. 2017;24:1018–1026. doi: 10.1111/acem.13193. [DOI] [PubMed] [Google Scholar]
- 10.De Jong A, Molinari N, Conseil M, et al. Video laryngoscopy versus direct laryngoscopy for orotracheal intubation in the intensive care unit: a systematic review and meta-analysis. Intensive Care Med. 2014;40:629–639. doi: 10.1007/s00134-014-3236-5. [DOI] [PubMed] [Google Scholar]
- 11.Huang HB, Peng JM, Xu B, Liu GY, Du B. Video laryngoscopy for endotracheal intubation of critically ill adults: a systemic review and meta-analysis. Chest. 2017;152:510–517. doi: 10.1016/j.chest.2017.06.012. [DOI] [PubMed] [Google Scholar]
- 12.Zhao BC, Huang TY, Liu KX. Video laryngoscopy for ICU intubation: a meta-analysis of randomised trials. Intensive Care Med. 2017;43:947–948. doi: 10.1007/s00134-017-4741-0. [DOI] [PubMed] [Google Scholar]
- 13.Higgins JPT, Green S ####(eds.) Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. www.cochrane-handbook.org (last accessed on 30 November 2017) [Google Scholar]
- 14.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62:1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 15.Rombey T, Pieper D. Video versus direct laryngoscopy for emergency endotracheal intubation of adults in a hospital setting: a systematic review and meta-analysis of randomized controlled trials. www.crd.york.ac.uk/prospero/display_record.php?RecordID=65015 last accessed on 30 November 2017 [Google Scholar]
- 16.The Cochrane Collaboration. RCT filters for different databases. www.work.cochrane.org/pubmed (last accessed on 30 November 2017) [Google Scholar]
- 17.Driver BE, Prekker ME, Moore JC, Schick AL, Reardon RF, Miner JR. Direct versus video laryngoscopy using the C-MAC for tracheal intubation in the emergency department, a randomized controlled trial. Acad Emerg Med. 2016;23:433–439. doi: 10.1111/acem.12933. [DOI] [PubMed] [Google Scholar]
- 18.Goksu E, Kilic T, Yildiz G, Unal A, Kartal M. Comparison of the C-MAC video laryngoscope to the Macintosh laryngoscope for intubation of blunt trauma patients in the ED. Turk J Emerg Med. 2016;16:53–56. doi: 10.1016/j.tjem.2016.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Griesdale DE, Chau A, Isac G, et al. Video-laryngoscopy versus direct laryngoscopy in critically ill patients: a pilot randomized trial. Can J Anaesth. 2012;59:1032–1039. doi: 10.1007/s12630-012-9775-8. [DOI] [PubMed] [Google Scholar]
- 20.Janz DR, Semler MW, Lentz RJ, et al. Randomized trial of video laryngoscopy for endotracheal intubation of critically ill adults. Crit Care Med. 2016;44:1980–1987. doi: 10.1097/CCM.0000000000001841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lascarrou JB, Boisrame-Helms J, Bailly A, et al. Video laryngoscopy vs direct laryngoscopy on successful first-pass orotracheal intubation among ICU patients: a randomized clinical trial. JAMA. 2017;317:483–493. doi: 10.1001/jama.2016.20603. [DOI] [PubMed] [Google Scholar]
- 22.Silverberg MJ, Li N, Acquah SO, Kory PD. Comparison of video laryngoscopy versus direct laryngoscopy during urgent endotracheal intubation: a randomized controlled trial. Crit Care Med. 2015;43:636–641. doi: 10.1097/CCM.0000000000000751. [DOI] [PubMed] [Google Scholar]
- 23.Sulser S, Ubmann D, Schlaepfer M, et al. C-MAC videolaryngoscope compared with direct laryngoscopy for rapid sequence intubation in an emergency department: a randomised clinical trial. Eur J Anaesthesiol. 2016;33:943–948. doi: 10.1097/EJA.0000000000000525. [DOI] [PubMed] [Google Scholar]
- 24.Yeatts DJ, Dutton RP, Hu PF, et al. Effect of video laryngoscopy on trauma patient survival: a randomized controlled trial. J Trauma Acute Care Surg. 2013;75:212–219. doi: 10.1097/TA.0b013e318293103d. [DOI] [PubMed] [Google Scholar]
- 25.Simmonds M, Salanti G, McKenzie J, Elliott J. Living systematic reviews: 3 Statistical methods for updating meta-analyses. J Clin Epidemiol. 2017;91:38–46. doi: 10.1016/j.jclinepi.2017.08.008. [DOI] [PubMed] [Google Scholar]
- E1.Ahmadi K, Ebrahimi M, Hashemian AM, Sarshar S, Rahimi-Movaghar V. GlideScope video laryngoscope for difficult intubation in emergency patients: a quasi-randomized controlled trial. Acta Med Iran. 2015;53:738–742. [PubMed] [Google Scholar]
- E2.Alvis BD, Hester D, Watson D, Higgins M, St Jacques P. Randomized controlled trial comparing the McGrath MAC video laryngoscope with the King Vision video laryngoscope in adult patients. Minerva Anestesiol. 2016;82:30–35. [PubMed] [Google Scholar]
- E3.Bailly A, Lascarrou JB. McGRATH MAC videolaryngoscope versus Macintosh laryngoscope for orotracheal intubation in intensive care patients: the randomised multicentre MACMAN trial study protocol. BMJ Open. 2015;5 doi: 10.1136/bmjopen-2015-009855. e009855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E4.Bailly A, Boisramé-Helms J, Champigneulle B, et al. Preoxygenation for intubation in the ICU: an ancillary study of the MACMAN trial. Ann Intensive Care. 2017;7:149–150. [Google Scholar]
- E5.Foulds LT, McGuire BE, Shippey BJ. A randomised cross-over trial comparing the McGrath((R)) Series 5 videolaryngoscope with the Macintosh laryngoscope in patients with cervical spine immobilisation. Anaesthesia. 2016;71:437–442. doi: 10.1111/anae.13384. [DOI] [PubMed] [Google Scholar]
- E6.Ghanem MT, Ahmed FI. GlideScope versus McCoy laryngoscope: intubation profile for cervically unstable patients in critical care setting. Eg J Anaesth. 2017;33:103–106. [Google Scholar]
- E7.Hattori K, Komasawa N, Kido H, Tatsumi S, Minami T. Muscle relaxant effect on tracheal intubation with Pentax-AWS Airwayscope: a prospective randomized controlled trial. Am J Emerg Med. 2017;34:674–675. doi: 10.1016/j.ajem.2015.11.035. [DOI] [PubMed] [Google Scholar]
- E8.Hemerka J, Yeatts DJ, Dutton RP, Hu PF, et al. Effect of video laryngoscopy on trauma patient survival: A randomized controlled trial. J Trauma Acute Care Surg. 2013;75:212–219. doi: 10.1097/TA.0b013e318293103d. J Emerg Med 2014; 46: 448. [DOI] [PubMed] [Google Scholar]
- E9.Ilyas S, Symons J, Bradley WP, et al. A prospective randomised controlled trial comparing tracheal intubation plus manual in-line stabilisation of the cervical spine using the Macintosh laryngoscope vs the McGrath((R)) series 5 videolaryngoscope. Anaesthesia. 2014;69:1345–1350. doi: 10.1111/anae.12804. [DOI] [PubMed] [Google Scholar]
- E10.Jeon WJ, Kim KH, Yeom JH, Bang MR, Hong JB, Cho SY. A comparison of the Glidescope(R) to the McGrath(R) videolaryngoscope in patients. Korean J Anesthesiol. 2011;61:19–23. doi: 10.4097/kjae.2011.61.1.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E11.Kelly FE, Cook TM. Randomised controlled trials of videolaryngoscopy vs. direct laryngoscopy on intensive care are needed. Intensive Care Med. 2014;40 doi: 10.1007/s00134-014-3262-3. [DOI] [PubMed] [Google Scholar]
- E12.Kim W, Lee Y, Kim C, et al. Comparison of the pentax airwayscope, glidescope video laryngoscope, and macintosh laryngoscope during chest compression according to bed height. Medicine (Baltimore) 2016;95 doi: 10.1097/MD.0000000000002631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E13.Lakticova V, Koenig SJ, Narasimhan M, Mayo PH. Video laryngoscopy is associated with increased first pass success and decreased rate of esophageal intubations during urgent endotracheal intubation in a medical intensive care unit when compared to direct laryngoscopy. J Intensive Care Med. 2015;30:44–48. doi: 10.1177/0885066613492641. [DOI] [PubMed] [Google Scholar]
- E14.Lester M, Semler M, Janz D, Rice T. Association between hypoxemia during endotracheal intubation and mortality in critically ill adults. Crit Care Med. 2015;43 [Google Scholar]
- E15.Mendelson JS, Felner KJ, Kaufman BS. Randomized trial of video laryngoscopy for endotracheal intubation of critically ill adults: more data, more questions. Crit Care Med. 2017;45:e460–###e461. doi: 10.1097/CCM.0000000000002218. [DOI] [PubMed] [Google Scholar]
- E16.Miner JR, Moore J, Rischall M, et al. Randomized controlled trial of endotracheal intubation using the c-mac videolaryngoscope versus standard laryngoscopy in patients undergoing emergent endotracheal intubation in the emergency department. Acad Emerg Med. 2012;19 [Google Scholar]
- E17.Ng I, Sim XL, Williams D, Segal R. A randomised controlled trial comparing the McGrath((R)) videolaryngoscope with the straight blade laryngoscope when used in adult patients with potential difficult airways. Anaesthesia. 2011;66:709–714. doi: 10.1111/j.1365-2044.2011.06767.x. [DOI] [PubMed] [Google Scholar]
- E18.Nishiyama T. Comparison of the airtraq, airway scope, and disposable macintosh laryngoscope blade. Middle East J Anaesthesiol. 2011;21:129–134. [PubMed] [Google Scholar]
- E19.Rali P, Arshad H, Lamba T. Comparison of video laryngoscopy versus direct laryngoscopy during urgent endotracheal intubation; trial of the route of early nutritional support in critically ill adults; and transfusion of plasma, platelets, and red blood cells in a 1:1:1 versus a 1:1:2 ratio and mortality in patients with severe trauma. Am J Respir Crit Care Med. 2015;192:892–894. doi: 10.1164/rccm.201504-0691RR. [DOI] [PubMed] [Google Scholar]
- E20.Sakles JC, Mosier JM, Patanwala AE, Arcaris B, Dicken JM. The utility of the C-MAC as a direct laryngoscope for intubation in the emergency department. J Emerg Med. 2016;51:349–357. doi: 10.1016/j.jemermed.2016.05.039. [DOI] [PubMed] [Google Scholar]
- E21.Saloum D, Chou E, Gillett B, et al. Facilitating instruction of direct laryngoscopy with video assistance: a pilot study. Acad Emerg Med. 2014;21 [Google Scholar]
- E22.Shravanalakshmi D, Bidkar PU, Narmadalakshmi K, Lata S, Mishra SK, Adinarayanan S. Comparison of intubation success and glottic visualization using King Vision and C-MAC videolaryngoscopes in patients with cervical spine injuries with cervical immobilization: a randomized clinical trial. Surg Neurol Int. 2017;8 doi: 10.4103/2152-7806.199560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E23.Smereka J. Comparison of airtraq and miller laryngoscopes for intubation in patients with inline manual neck stabilization. Am J Emerg Med. 2016;34 doi: 10.1016/j.ajem.2016.06.025. [DOI] [PubMed] [Google Scholar]
- E24.St Mont G, Biesler I, Pfortner R, Mohr C, Groeben H. Easy and difficult nasal intubation—a randomised comparison of macintosh vs airtraq(R) laryngoscopes. Anaesthesia. 2012;67:132–138. doi: 10.1111/j.1365-2044.2011.06943.x. [DOI] [PubMed] [Google Scholar]
- E25.Sulser S, Ubmann D, Brueesch M, et al. The C-MAC videolaryngoscope compared with conventional laryngoscopy for rapid sequence intubation at the emergency department: study protocol. Scand J Trauma Resusc Emerg Med. 2015;23 doi: 10.1186/s13049-015-0119-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E26.Teoh WH, Saxena S, Shah MK, Sia AT. Comparison of three videolaryngoscopes: pentax airway scope, C-MAC, glidescope vs the Macintosh laryngoscope for tracheal intubation. Anaesthesia. 2010;65:1126–1132. doi: 10.1111/j.1365-2044.2010.06513.x. [DOI] [PubMed] [Google Scholar]
- E27.Truszewski Z, Bogdanski L, Kurowski A, et al. Does the venner AP. advance video laryngoscope improve success of first intubation attempt of trauma patient? Am J Emerg Med. 2016;34:315–316. doi: 10.1016/j.ajem.2015.10.058. [DOI] [PubMed] [Google Scholar]
- E28.Woo CH, Kim SH, Park JY, et al. Macintosh laryngoscope vs Pentax-AWS video laryngoscope: comparison of efficacy and cardiovascular responses to tracheal intubation in major burn patients. Korean J Anesthesiol. 2012;62:119–124. doi: 10.4097/kjae.2012.62.2.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E29.Xue FS, Yang GZ, Li HX, Liu YY. Comparing direct and video laryngoscopy for urgent intubation during chest compression. Resuscitation. 2017;111 doi: 10.1016/j.resuscitation.2016.10.031. [DOI] [PubMed] [Google Scholar]
- E30.Xue FS, Yang GZ, Sun C. Comparing video and direct laryngoscopy in critically ill patients: rational study design is important. Crit Care Med. 2017;45 doi: 10.1097/CCM.0000000000002191. e326. [DOI] [PubMed] [Google Scholar]
- E31.Yanik BG, Yolcu S, Aydinok G, et al. The quickest and easiest endotracheal intubation device in difficult airway for emergency residents: video laryngoscope, the easiest laryngoscope for emergency residents. Am J Emerg Med. 2014;32:807–809. doi: 10.1016/j.ajem.2014.02.037. [DOI] [PubMed] [Google Scholar]
- E32.Yeatts D, Grissom T, Dutton R, Hu P, Chang YW, Scalea T. Video laryngoscopy does not improve outcomes in emergency intubation. Crit Care Med. 2009;37 [Google Scholar]
- E33.Yu JH, Wang Y. [Clinical study of SMT- video laryngoscope with difficult airway intubation in emergency department] Zhonghua Wai Ke Za Zhi. 2017;55:549–553. doi: 10.3760/cma.j.issn.0529-5815.2017.07.014. [DOI] [PubMed] [Google Scholar]