Abstract
Background
Nearly half of Americans with diagnosed hypertension (HTN) have uncontrolled blood pressure (BP), while some integrated healthcare systems such as Kaiser Permanente Northern California (KPNC) have achieved control rates upwards 90%.
Methods and Results
We adapted KP’s evidence-based treatment protocols in a racially and ethnically diverse population at 12 safety-net clinics in the San Francisco Health Network. The intervention consisted of four elements: a HTN registry, a simplified treatment intensification protocol that included fixed-dose combination medications containing diuretics, standardized BP measurement protocol, and BP check visits led by registered nurse and pharmacist staff. The study population comprised patients with HTN who made ≥1 primary care visits within the past 24 months (N=15,917) and had a recorded BP measurement within the past 12 months. We conducted a post-intervention time series analysis from August 2014 to August 2016 to assess the effect of the intervention on BP control over 24 months for the pilot site and over 15 months for 11 other SFHN clinics combined. Secondary outcomes were changes in use of guideline-recommended medication prescribing. Rates of BP control increased at the pilot site (68% to 74%, P<0.01) and the 11 other SFHN clinic sites (69% to 74%, P<0.01). Statistically significant improvements in BP control rates (P<0.01) at the 11 SFHN clinic sites occurred in all racial and ethnic groups (Blacks 60% to 66%, Whites 69% to 75%, Latinos 67% to 72%, Asians 78% to 82%). Use of fixed-dose combination medications increased from 10% to 13% (P <0.01 value) and the percentage of ACE-inhibitor prescriptions dispensed in combination with a thiazide diuretic increased from 36% to 40% (P <0.01).
Conclusions
Evidence-based system approaches to improving BP control can be implemented in safety net settings and could play a pivotal role in achieving improved population BP control and reducing HTN disparities.
INTRODUCTION
Improving blood pressure (BP) control is a critical focus area for clinical medicine; treating U.S. adults with uncontrolled hypertension (HTN) to achieve currently recommended BP goals has the potential to prevent 56,000 cardiovascular events, 13,000 deaths and save $4.5 billion annually.1 The US Department of Health and Human Services has prioritized better management of HTN through implementation of evidence-based treatment protocols as a key population health strategy in national efforts to prevent 1 million strokes and 1 million heart attacks.2 Today, well-established standards of care exist and nearly 90% of patients with uncontrolled HTN have made a doctor’s visit in the last year, yet more than 40% of patients with HTN have BPs above their recommended goals1, 3, 4 The barriers to blood pressure control therefore do not stem primarily from lack of knowledge of how to control BP or access to medical care, but rather from missed opportunities in clinical practice to effectively implement evidence-based hypertension management.5
Integrated and well-resourced health delivery systems such as Kaiser Permanente Northern California (KPNC) have achieved BP control rates approaching 90% through implementation of multi-component system-level interventions including an evidence-based treatment protocol. To date, there has been no published evidence on whether robust health system HTN management interventions such as KPNC’s can be successfully adapted and implemented in safety-net clinics to improve BP control.6, 7 Safety-net clinics provide care to predominantly minority and low-income patients and have disproportionally low BP control rates8 Improving HTN management in these settings will be essential to achieving national population health priorities for improving BP control and reducing racial cardiovascular disease disparities. Adapting proven health system interventions for safety-net settings can be a key strategy to meeting national hypertension control priorities.
We adapted the KPNC hypertension control intervention and then evaluated it in a network of 12 safety-net clinics caring for a low income and racially and ethnically diverse patient population, specifically, to assess the effectiveness of the intervention on BP control rates in patients with HTN and differential effects in racial and ethnic subgroups.
METHODS
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Study design
Our study is a post-intervention time-series analysis to assess the effectiveness of a health system intervention for hypertension management in 12 safety-net clinics that comprise a large county-operated health network. The study was approved by the University of California San Francisco Human Research Protection Program Committee on Human Research.
Study setting and population
The San Francisco Health Network comprises 12 adult primary care clinics that provide care for 65, 447 active patients who are low-income and racially and ethnically diverse. All 12 clinics share the same electronic health record (EHR) system. SFHN defines active patients as patients who made at least one clinic visit over the past 24 months. We defined patients with HTN based on having any HTN diagnosis coded in the medical record. Our analysis included patients ages 20 to 84 and excluded patients who have not had a recorded BP measurement within the past 12 months as being lost to follow up. Because of differences in timing and implementation of the intervention, we analyzed phase 1 (the pilot site) and phase 2 (the remaining 11 SFHN clinics) separately. See online appendix Table 1 for more details on differences in implementation by clinic site. Patients at SHFN received drug coverage primarily from Medicaid (59%) and Medicare (14 %%).
Intervention
Over the course of twelve months, we engaged stakeholders from KPNC and SFHN to understand the elements of KPNC’s program that could be adapted for SFHN within the existing personnel, budget, and health information technology infrastructure at SFHN. We also sought to adapt the program to account for formulary of the major insurers, medication affordability, ease of use, patient complexity, and provider preferences that are pertinent to healthcare safety-net settings and the patient populations they care for. (Tables 1 and 2) Our adapted program, Bring it Down San Francisco, consisted of 4 key elements (Table 1) that paralleled KPNC’s program: 1) development of an internal hypertension patient registry to facilitate provider performance feedback and panel management outreach to schedule patients with uncontrolled HTN for BP visits, 2) a simplified evidence-based treatment intensification protocol, 3) a standardized BP measurement protocol, and 4) blood pressure check visits led by registered nurse and pharmacist staff. Performance feedback data on BP control was shared with clinics and providers for total and also Black patients with HTN.
Table 1.
Key elements of the Kaiser Permanente Northern California (KPNC) hypertension program adopted in Bring it Down San Francisco
| Program components | KPNC Hypertension Program | Bring it Down San Francisco |
|---|---|---|
| Evidence-based treatment protocol | Designed to accomplish
|
Protocol modified to account for:
|
| BP check visits led by non-physician professional staff |
|
|
| Standard BP measurement protocol |
|
|
| Hypertension patient registry |
|
|
| Performance reports |
|
|
Table 2.
Adjustments to the KPNC treatment protocol tailored for the San Francisco Health Network based on stakeholder engagement
| KPNC Protocol | Bring it Down Protocol | Rationale for adjustment |
|---|---|---|
| Initiate treatment with FDC* drugs | Two optional pathways:
|
Reduce need for lab monitoring – a key consideration for a population with lower access to clinic visits and lower attendance rates |
| Max dose of hydrochlorothiazide: 50mg | Max dose of hydrochlorothiazide: 25mg | SFHN stakeholders perceived a higher risk for adverse effects for safety-net patient populations |
| Spironolactone or Labetalol for resistant HTN | More emphasis on Spironolactone for resistant HTN | Stronger evidence for efficacy of spironolactone |
| Medication recommendations adjusted according to drug formulary | There are varying health plans and drug formularies that cover SFHN patients as opposed to the single-payer system that exists at KPNC |
FDC = fixed-dose combination
Measurements and outcomes
Our primary outcome of interest was BP control based on the most recent EHR-recorded BP. We ascertained BP control at baseline (August 2014) and monthly over 24 months post-intervention for the pilot site (phase 1) and 15 months for the other 11 clinics combined (phase 2). We defined BP control as having a systolic BP below 140 mmHg and diastolic BP below 90 mmHg for patients who are either younger than 60 years or have diabetes or chronic kidney disease. For patients age 60 years and above without diabetes or chronic kidney disease (CKD), we defined BP control as systolic BP less than 150 mmHg and diastolic BP less than 90 mmHg. We chose this definition in accordance with the 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults published by the JNC8 Panel Member Report 9 and the National Committee for Quality Assurance (NCQA) Healthcare Effectiveness Data and Information Sets (HEDIS) specifications for HTN control as of August 2014.10 The recommendations of the JNC8 Panel Member Report were and continue to be the standard of care in the clinic sites. However, newer guidelines by the American College of Cardiology and American Heart Association have recommend lower BP targets, and so, as a sensitivity analysis, we repeated our analysis with BP control defined per NCQA HEDIS specifications before 201411 as SBP less than 140mmHg and DBP less than 90 mmHg regardless of age or diabetes and CKD status. We ascertained the BP control rate each month during the post-intervention period as the proportion of patients with BP control among all patients with HTN and BP control rates within race/ethnic groups. Clinic blood pressures were measured using Omron 7 Automated sphygmomanometers. Medical assistants were instructed to repeat the BP in one to three minutes whenever the first measurement is elevated; fidelity to this protocol across sites was not assessed.
Our secondary outcomes were the use of three guideline-concordant medication treatment practices targeted by the BID-SF intervention in the treatment protocol: 1) use of fixed-dose combination drugs among patients with two or more antihypertensive medications, 2) use of angiotensin converting enzyme (ACE) inhibitor therapy in combination with thiazide diuretics, and 3) use of aldosterone antagonists in patients with resistant HTN whose BP are above goal while taking four or more classes of antihypertensive medications. We defined resistant HTN as patients taking at least four classes BP medications or have uncontrolled HTN despite being on three classes BP medications at presentation.
Statistical Analysis
We assessed post-intervention improvements in the BP control rate and use of three guideline-concordant medication treatment practices over 24 post-intervention months for the pilot site and 15 months for the other 11 SFHN clinics using two separate analyses, one for the pilot site and one for the remaining 11 SFHN clinics combined. We used the Cochran Armitage test for trend to assess trends in BP control rates. To assess for potential differences by race, we performed unadjusted linear regressions for each race (White, Black, Latino, and Asian) separately with time in months as the primary predictor. We used mixed-effects multivariable logistic regression models adjusted for age, race, and gender to account for clustering and separate trends by clinic and individual patients and with a primary predictor of time in months since the intervention. We used Chi-square tests to assess for significant change in use of the four guideline-concordant medication treatment practices mentioned above. Due to initial limitations in resources and data infrastructure we could not ascertain medication treatment practices at baseline. We did not have complete medication data until February 2015 for the pilot site (6 months post-intervention) and Feb 2016 for SFHN (9 months post-intervention). Therefore, we compared these practices at 6 months vs 24 months post-intervention for the pilot site and 9 months vs 15 months for the other 11 SFHN clinics.
RESULTS
At the start of the intervention, we identified 15,917 patients with hypertension across SFHN clinics between ages 20 and 84 who had a BP measurement within the past 12 months. More than half of patients were women (52%) and 23% was Black. Among 5,510 patients with uncontrolled HTN, 22% had stage II HTN (by JNC 7 definitions), and 27% met criteria for resistant HTN. [Table3]
Table 3.
Patient characteristics of the SFHN patients with hypertension at the start of BID-SF
| Pilot site | Other SFHN clinics | |
|---|---|---|
| Total number of patients with HTN | 2,449 | 13,468 |
| Demographics | N (%) | N (%) |
| Age (mean, sd) | 61.1 (11.2) | 59.8 (10.8) |
| 20 – 34 | 43 (1.8) | 310 (2.3) |
| 35 – 64 | 1493 (61.0) | 8811 (65.4) |
| 65 – 79 | 734 (32.0) | 3918 (29.1) |
| 80 – 85 | 129 (5.3) | 429 (3.2) |
| Female | 1201 (49.0) | 7017 (52.1) |
| Race | ||
| White | 376 (15.4) | 2335 (17.3) |
| Black | 496 (20.3) | 3101 (23.0) |
| Asian | 718 (29.3) | 4788 (35.6) |
| Hispanic | 747 (30.5) | 2783 (20.7) |
| Other | 112 (4.6) | 459 (3.4) |
| Medical history | ||
| Diabetes | 1119 (46.1) | 4849 (36.0) |
| Chronic kidney disease | 446 (18.2) | 2912 (21.6) |
| Blood Pressure | ||
| Mean systolic BP (SD) | 132.5 (19.6) | 133.8 (17.8) |
| Mean diastolic BP (SD) | 77.3 (10.9) | 79.8 (13.6) |
| Uncontrolled hypertension‡ | 856 (35.0) | 4654 (34.6) |
| Stage of uncontrolled hypertension | ||
| Stage I: 140 – 159/90 – 99 | 616 (72.0) | 3304 (71.0) |
| Stage 2: 160 – 179/100 – 109 | 188 (22.0) | 1047 (22.5) |
| Severe HTN: ≥ 180/≥110 | 52 (6.07) | 303 (6.5) |
| Prevalence of Resistant hypertension‖ | 507(20.0) | 2038 (15.9) |
| Uncontrolled HTN on ≥ 3 BP medications | 300 (59.2) | 1187 (58.2) |
| # of antihypertensive medications (mean, sd) | 2.08 (1.3) | 1.90 (1.2) |
| 0 | 227 (8.9) | 1634 (12.8) |
| 1 | 654 (25.8) | 3329 (26.0) |
| 2 | 793 (31.2) | 4113 (32.1) |
| 3+ | 865 (34.1) | 3725 (29.1) |
RFPC = Richard Fine People’s Clinic at the Zuckerberg San Francisco General Hospital
SFHN = San Francisco Health Network
Percentages are reported as column %
The start of BID-SF is 08/2014 for SFPC and 05/2015 for the other 11 SFHN clinics
uncontrolled hypertension per 2014 guidelines: BP ≥150/90 for patients 60 or older without CKD or diabetes and BP ≥140/90 for all other patients
Resistant hypertension: patient on ≥ 4 BP medications or has uncontrolled hypertension with 3 BP medications at presentation
Note: Because meds data are not available for baseline months, prevalence of resistant HTN and med counts are as of Dec 2014 for the pilot site (n=2539) and Feb 2016 for SFHN (n=12801), respectively
Following the implementation of the adapted BP algorithm and other components of Bring it Down San Francisco, BP control rate at the pilot site increased over the 24 months from 68% in August, 2014, to 74% in August, 2016 (P for trend< 0.01). Improved BP control occurred in Blacks (63% to 67%, P for trend<0.01) Whites (67% to 72%, p for trend<0.01), Latinos (66% to 72%, p for trend<0.01), and Asians (74% to 79%, p for trend<0.01). [Figure 1] The difference in BP control between Whites and other racial groups did not decrease over time, with a persistent disparity in BP control between Blacks (67%) and Whites (72%) at 24 months.
Figure 1. Trend in BP control by race over 24 months at Richard Fine People’s Clinic (RFPC) and 15 months at the other 11 clinics in the San Francisco Health Network (SFHN).
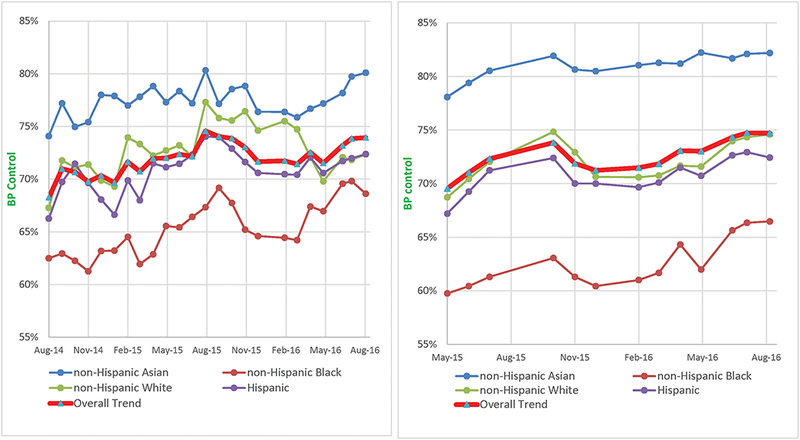
The panel on the left displays trends at RFPC and the panel on the right displays trends at the other 11 clinics.
Unadjusted trend in monthly BP control rates; BP control was defined as <150/90 mmHg for patient who are 60 years or older and do not have diabetes and <140/80mgHg for all other patients. The points on the graph represent the overall BP control monthly BP control rates calculated at the clinic level (# of patients with BP control divided by # of active patients with hypertension).
The BP control rate at the other 11 SFHN clinics similarly increased over 15 months after implementation of BID-SF from 69% in April, 2015, to 74% in August, 2016 (p <0.01). Improved BP control occurred in Blacks (60% to 66%, p for trend<0.01) Whites (69% to 75%, p for trend<0.01), Latinos (67% to 72%, p for trend<0.01) and Asians at (78% to 82%, p for trend<0.01). [Figure 1 and Appendix table 2] In our adjusted mixed-effect model however, the predicted rate of improvement in BP control was greater in Blacks as compared to Whites (0.35% per month vs 0.10% per month, p = 0.03). [Appendix Table 4 and Figure 2] Predicted rates of improvements for Asians (0.06% per month, P = 0.70 and Latinos (0.23% per month, p = 0.15) did not differ compared with Whites. (Figure 1) Sensitivity analyses with BP control defined as less than 140/90 mmHg regardless of age or diabetes and CKD yielded similar patterns of improving trends in BP control (65% to 71% at both the pilot site and the other 11 SFHF clinics; p for trend <0.01). See Appendix Table 3 and Figure 1.
Use of fixed-dose combination drugs increased from 11% to 14% (P <0.01) at the pilot site and 10% to 13% (P <0.01value) at the other 11 SFHN clinics. The percentage of ACE inhibitor prescriptions dispensed in combination with a thiazide diuretic increased from 35% to 42% (P<0.01) at the pilot site and 36% to 40% (P <0.01) at the other SFHN clinics. Use of aldosterone antagonist for uncontrolled resistant HTN did not change over the course of the intervention period. [Table 4]
Table 4.
Changes in guideline-concordant practice patterns in hypertension treatment at SFHN
| Pilot site | Other SFHN clinics | |||||
|---|---|---|---|---|---|---|
| 02/2015 6 months* | 08/2016 24 months | P-value | 02/2016 9 months* | 08/2016 15 months | P-value | |
| Prevalent use of fixed-dose combination drugs in patients taking ≥2 BP medications | 171/1612 (10.6%) | 282/1963 (14.4%) | <0.01 | 770/7838 (9.8%) | 1134/8806 (12.9%) | <0.01 |
| Percentage of ACE Inhibitor dispensed in combination with a thiazide diuretic† | 420/1199 (35.0%) | 559/1324 (42.2%) | <0.01 | 1895/5286 (35.9%) | 2434/6032 (40.4%) | <0.01 |
| Prevalent use of aldosterone antagonists among patients with uncontrolled BP on ≥ 4 BP meds | 18/127 (14.2%) | 37/144 (25.7%) | 0.02 | 77/442 (17.4%) | 87/463 (15.8%) | 0.55 |
SFHN = San Francisco Health Network
Due to initial limitations in resources and data infrastructure we could not ascertain medication prescription practices at baseline. Feb 2015 and Feb 2016 represent the earliest times we had reliable medication data for the pilot site and SFHN, respectively.
Thiazide diuretic: hydrochlorothiazide or chlorthalidone
Discussion
This study used implementation science methodologies to adapt and implement Kaiser Permanente’s HTN management program in 12 urban safety net clinics leading to significant improvements in BP control over 15 and 24 months follow-up period. We found that a proven HTN population management protocol could be successfully adapted to and implemented in a safety net setting and contribute to improved BP control and reduced HTN disparities. This intervention was associated with an absolute increase in proportion BP controlled of 6% within nine months that was maintained at 15 months, rates that compare favorably with the national trend in control rates that have increased 1 percent per year, and even Kaiser’s control rates that increased from 44% to 80% over 10 years.11
Several facets of the intervention may have contributed to its successful adoption and the observed post-intervention improvement in BP control. We selected a simple evidence-based treatment protocol from KPNC and engaged stakeholders in an iterative process to adapt it for ease of use, patient complexity, provider preference, and drug formularies relevant to the SFHN context; additionally, we aligned the timing of implementation with quality improvement goals and priorities. This process likely engendered trust and removed barriers for physician adoption and use of treatment protocols – a strategy the Centers for Disease Control (CDC) has singled out as a nation-wide priority for improving HTN management.2 We created a new longitudinal registry of HTN patients that facilitated performance monitoring and monthly reports of clinic-level BP control rates. BP check visits led by non-physicians facilitated access, more frequent visits, and treatment intensification.
While we cannot determine whether improvements in BP control rates are attributed directly to our intervention, improvements in many of the process measures are consistent with this intervention contributing to control rates. We observed a pattern toward greater use of evidence-based treatment of HTN in the post-intervention period. We observed a significant increase in use of fixed-dose combination drugs and percentage of ACE inhibitors prescribed in combination with a thiazide diuretic. These are important improvements because fixed-dose combination medications have several advantages, including faster titration to BP goal, improved adherence and lower patient cost, and are associated with improved blood pressure control.12–16 Additionally, combining thiazide diuretics with ACE inhibitor improves efficacy and may be particularly important for the effective use of ACE inhibitors in Black patients.9, 17
Our pragmatic practice-based intervention and observational study was not designed to determine what components of the intervention had the greatest effect on improvements. However, evidence from systematic reviews and computer simulation suggest that interventions to increase treatment intensification and visit frequency are the most effective at improving HTN control.5, 18 Also, it is likely that deployment of the intervention had a systemic effect of raising awareness and prioritization of hypertension that led to reduced clinical inertia (more frequent clinic visits and treatment intensification for HTN).
Significant improvements in BP control occurred in Whites, Blacks, Latinos, and Asians. By standard quality improvement metrics for BP control, the gap between Blacks and Whites persisted but did not widen. After adjusting for age and gender, we found that post-intervention improvements in BP control were greater in Blacks as compared to Whites likely because clinics with higher concentrations of Blacks started with lower BP control and experienced higher rates of improvement. Our findings underscore what has been observed in other settings - that effective health system interventions in clinical settings may improve health outcomes for groups disproportionately affected by a condition, but may not eliminate disparities between groups.19 Improving BP control in Black patients may require dual efforts focused on clinical settings that care for Black patients and also on the barriers specific to the population, and may include interventions targeting modifiable experiences, behaviors, and perhaps physiology that are pertinent to Black patients.
We note some limitations to consider in interpreting these findings. This is an observational post-intervention time series analysis and thus is limited in the ability to directly attribute the effect to the intervention because of possible secular trend or alternative explanations. However, the magnitude of the effect and the improvement in the process measures are consistent with the intervention contributing to the improvements in blood pressure control that we observe. Our intervention was endorsed and coordinated by central management in partnership with local quality improvement leaders, so there were no concurrent hypertension interventions to explain our observed BP control improvements. The health network in this study benefits from centralized management with experience in implementing successful quality improvement initiatives, as evidenced by the high baseline BP control rate we observed. This may limit the generalizability of our findings to other safety-net clinical settings with similar resources or managerial commitment, but suggests that significant improvements in BP control is possible in patient populations that receive care at safety-net clinics if given appropriate resources and management infrastructure to employ evidence-based policies. As with many multi-component interventions, including the one from which this is adapted, we are unable to directly determine which of the components is responsible for the effect or whether all four components are necessary. Finally, although the diverse nature of the population treated in this setting allows for an examination of the effects across racial and ethnic sub-groups, these analyses may not be fully powered to determine heterogeneity of effects.
Our study offers unique advantages that should be noted. First, this is a large, multi-center pragmatic implementation of a health system intervention to improve BP control in safety net clinics, in keeping with the CDC charge for every physician or healthcare organization to adopt or create their own customized evidence-based treatment protocol and evaluate implementation of their protocol within multi-component interventions. Second, our longitudinal registry of HTN patients across 12 safety net clinics allowed us to assess post-intervention trends in BP control stratified by race and ethnicity and describe existing racial disparities in BP control within a low-income population. Our findings suggest elimination of racial disparities in HTN may require targeted interventions focused on improving BP control in Black patients.
Conclusions
This study demonstrates that evidence based treatment protocols are transportable to safety net settings and could play a pivotal role in achieving improved BP control and reducing HTN disparities. Our findings can inform adoption of best practices to improve BP control at safety-net clinics which must play a pivotal role in achieving nationwide improvements in BP control and reducing socioeconomic disparities in HTN.
Supplementary Material
What is known.
Over half of Americans with diagnosed hypertension (HTN) have uncontrolled blood pressure (BP), while some integrated healthcare systems such as Kaiser Permanente Northern California (KPNC) have achieved control rates as high as 90%.
What the study adds.
This is a large, multi-site pragmatic implementation of a health system intervention to improve BP control in a network of safety net clinics.
Careful stakeholder engagement allowed us to tailor a hypertension treatment protocol utilized successfully in Kaiser to safety net clinics.
The intervention was associated with increases in blood pressure control for all racial and ethnic groups with higher rates of improvement for black patients as compared to Whites.
This study demonstrates that evidence-based treatment protocols are transportable to safety net settings and could play a pivotal role in achieving improved BP control and reducing racial disparities in hypertension.
Acknowledgments
The authors would like to acknowledge the intellectual and administrative contributions to this study made by Grace Chang, Antonella Jimenez, Dia Yang, Judith Sansone, and Purba Chatterjee
Sources of Funding
This work was supported and funded by the UCSF Center for Vulnerable Populations at the Zuckerberg San Francisco General Hospital, NINDS grant U54NS081760 and supplement to U54NS081760, and the Kaiser Community Grant Preventing Heart Attack and Strokes Every Day.
Footnotes
Disclosures
The authors have no conflicts of interest to disclose.
References
- 1.Moran AE, Odden MC, Thanataveerat A, Tzong KY, Rasmussen PW, Guzman D, Williams L, Bibbins-Domingo K, Coxson PG and Goldman L. Cost-effectiveness of hypertension therapy according to 2014 guidelines. The New England journal of medicine. 2015;372:447–55. doi: 10.1056/NEJMsa1406751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Frieden TR, King SM and Wright JS. Protocol-based treatment of hypertension: a critical step on the pathway to progress. Jama. 2014;311:21–2. doi: 10.1001/jama.2013.282615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fontil VB-D K, Nguyen O, Guzman D, Goldman LE. Management of Hypertension in Primary Care safety-net clinics in the United States: A Comparison of Community Health Centers and Private Physician’s Offices. Health Services Research. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.AHRQ. Expenditures for Hypertension among Adults Age 18 and Older, 2010: Estimates for the U.S. Civilian Noninstitutionalized Population. 2013;2016. [PubMed] [Google Scholar]
- 5.Fontil V, Bibbins-Domingo K, Kazi DS, Sidney S, Coxson PG, Khanna R, Victor RG and Pletcher MJ. Simulating Strategies for Improving Control of Hypertension Among Patients with Usual Source of Care in the United States: The Blood Pressure Control Model. Journal of general internal medicine. 2015;30:1147–55. doi: 10.1007/s11606-015-3231-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mueller M, Purnell TS, Mensah GA and Cooper LA. Reducing racial and ethnic disparities in hypertension prevention and control: what will it take to translate research into practice and policy? American journal of hypertension. 2015;28:699–716. doi: 10.1093/ajh/hpu233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ogedegbe G, Tobin JN, Fernandez S, Cassells A, Diaz-Gloster M, Khalida C, Pickering T and Schwartz JE. Counseling African Americans to Control Hypertension: cluster-randomized clinical trial main effects. Circulation. 2014;129:2044–51. doi: 10.1161/CIRCULATIONAHA.113.006650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fontil V, Bibbins-Domingo K, Nguyen OK, Guzman D and Goldman LE. Management of Hypertension in Primary Care Safety-Net Clinics in the United States: A Comparison of Community Health Centers and Private Physicians’ Offices. Health Serv Res. 2017;52:807–825. doi: 10.1111/1475-6773.12516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, Smith SC Jr., Svetkey LP, Taler SJ, Townsend RR, Wright JT Jr., Narva AS and Ortiz E. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). Jama. 2014;311:507–20. doi: 10.1001/jama.2013.284427 [DOI] [PubMed] [Google Scholar]
- 10.NCQA Measuring quality Improving health care. Controlling High Blood Pressure. 2018. [Google Scholar]
- 11.Jaffe MG, Lee GA, Young JD, Sidney S and Go AS. Improved blood pressure control associated with a large-scale hypertension program. Jama. 2013;310:699–705. doi: 10.1001/jama.2013.108769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wald DS, Law M, Morris JK, Bestwick JP and Wald NJ. Combination therapy versus monotherapy in reducing blood pressure: meta-analysis on 11,000 participants from 42 trials. Am J Med. 2009;122:290–300. doi: 10.1016/j.amjmed.2008.09.038 [DOI] [PubMed] [Google Scholar]
- 13.Feldman RD, Zou GY, Vandervoort MK, Wong CJ, Nelson SA and Feagan BG. A simplified approach to the treatment of uncomplicated hypertension: a cluster randomized, controlled trial. Hypertension. 2009;53:646–53. doi: 10.1161/HYPERTENSIONAHA.108.123455 [DOI] [PubMed] [Google Scholar]
- 14.Byrd JB, Zeng C, Tavel HM, Magid DJ, O’Connor PJ, Margolis KL, Selby JV and Ho PM. Combination therapy as initial treatment for newly diagnosed hypertension. Am Heart J. 2011;162:340–6. doi: 10.1016/j.ahj.2011.05.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bangalore S, Kamalakkannan G, Parkar S and Messerli FH. Fixed-dose combinations improve medication compliance: a meta-analysis. Am J Med. 2007;120:713–9. doi: 10.1016/j.amjmed.2006.08.033 [DOI] [PubMed] [Google Scholar]
- 16.Hong SH, Wang J and Tang J. Dynamic view on affordability of fixed-dose combination antihypertensive drug therapy. Am J Hypertens. 2013;26:879–87. doi: 10.1093/ajh/hpt035 [DOI] [PubMed] [Google Scholar]
- 17.Izzo JL Jr. and Weir MR. Angiotensin-converting enzyme inhibitors. J Clin Hypertens (Greenwich). 2011;13:667–75. doi: 10.1111/j.1751-7176.2011.00508.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Glynn LG, Murphy AW, Smith SM, Schroeder K and Fahey T. Interventions used to improve control of blood pressure in patients with hypertension. The Cochrane database of systematic reviews. 2010:CD005182. doi: 10.1002/14651858.CD005182.pub4 [DOI] [PubMed] [Google Scholar]
- 19.Nguyen-Huynh MN, Hills NK, Sidney S, Klingman JG and Johnston SC. Race-ethnicity on blood pressure control after ischemic stroke: a prospective cohort study. J Am Soc Hypertens. 2017;11:38–44. doi: 10.1016/j.jash.2016.11.002 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


