Abstract
Aims and Objectives:
The aim of this work was to assess the advantages and disadvantages of magnetic resonance imaging (MRI) versus computed tomography (CT) in the initial evaluation of maxillofacial space infections by comparing various parameters of the imaging studies and comparing them on a three-point scale.
Materials and Methods:
We prospectively evaluated 15 patients with head and neck space infections. All patients underwent CT and MRI using similar slice thickness. We reviewed all imaging studies with special attention to location, extension, source of infection, extent of bone involvement, odontogenic or nonodontogenic, and presence of gas/calcium in the lesions. All the parameters were graded based on a three-point scale and were compared statistically by paired t-test.
Results:
According to the results we arrived at, MRI was superior to CT in regard to lesion conspicuity, extension, number of anatomic spaces involved, and source on infection. Although not significant, MRI detected a greater number of abscess collections. However, in the aspects of detection of intralesional gas and calcium and motion artifacts, CT was superior to MRI. However, these advantages of CT over MRI are not significantly better than those of MRI.
Conclusion:
MRI was considered superior to CT in the initial evaluation of head and neck space infections. Our study thus concludes that MRI may be used as the primary modality to evaluate patients with head and neck infections when clinically feasible.
Keywords: Computed tomography, diagnostic tool, magnetic resonance imaging, space infection
INTRODUCTION
Potential or actual spaces between fascia and muscles which contain nerves, blood vessels and connective tissue may become pathways in the presence of infection. Infections which originate in deeper structures are severe which progress rapidly and may cause prolonged morbidity, long-term complications as well as potentially endangered life. High-resolution computed tomography (CT) and magnetic resonance imaging (MRI) play a major role in the diagnosis and management of head and neck infections. Apart from clinical examination and occasionally laboratory data, the examining surgeon must determine the need for advanced imaging studies. Difference of opinions still exists as to whether CT or MRI is the best imaging modality for acute neck infection. The most accepted opinion is that the least invasive and least expensive examination that adequately evaluates the patient is to be used.[1,2,3,4]
We carried out a prospective study that evaluated 15 patients with newly diagnosed head and neck space infections at CKS Teja Dental College, Tirupati, Andhra Pradesh, and assessed the advantages and shortcomings of both modalities.
A similar study was conducted where 19 patients with small cell neuroendocrine carcinoma in the paranasal sinuses by MRI (n = 19) and CT and MRI (n = 18) were retrospectively studied. CT and MRI were undertaken to investigate tumor features.[5]
MATERIALS AND METHODS
INCLUSION CRITERIA
Upon receiving the approval of Ethical committee of our dental college (letter no. 10352), who suggested the sample size of 15 patients after discussing the model of study. We prospectively examined 15 consecutive patients with clinically suspected acute maxillofacial space infections who were referred to the Department of Oral and Maxillofacial surgery, CKS Theja Institute of Dental Sciences and Research, from January 2013 to December 2013. Hence, the study participants who were meeting the inclusion criteria are selected depending on feasibility and convenience, so the number of participants in the study is rounded up to 15. Informed consent is taken from all patients, and initial clinical examination is carried out. Common minor space infections that can be easily drained by surgery were excluded from the study. All imaging studies were performed before any surgical procedure. Final diagnosis was achieved by percutaneous aspiration, surgical exploration and drainage, or follow-up after successful antibiotic treatment.
RESULTS
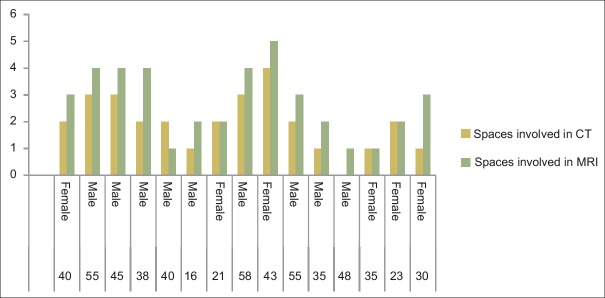
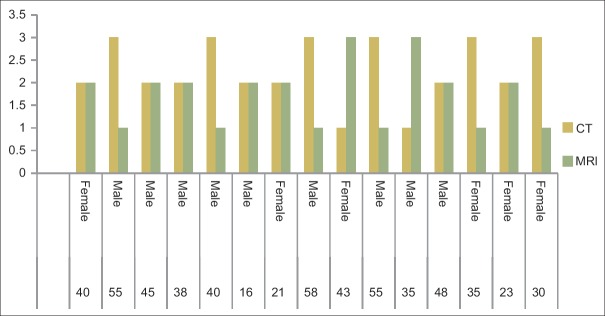
Figure 1 represents data regarding demographic distribution of study participants. Fifteen participants with odontogenic infection were included in the study. Nine of the study participants were male and 6 were female with a mean age of 38.8 years.
Figure 1.
Demographic details
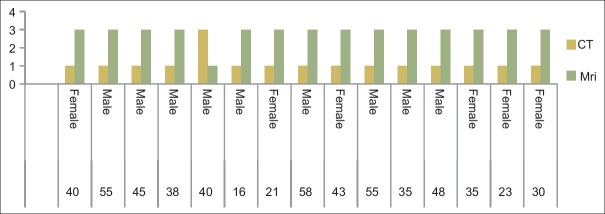
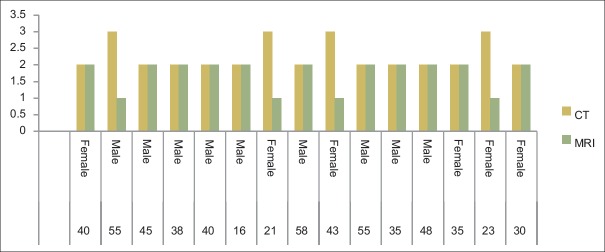
Table 1 represents description of all the parametres under CT and MRI. MRI was more conspicuous in examining a lesion as compared to CT [Figure 2].
Table 1.
Consolidated table of all parameters
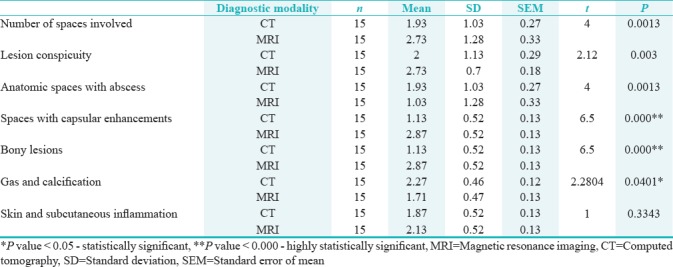
Figure 2.
Lesion conspicuity
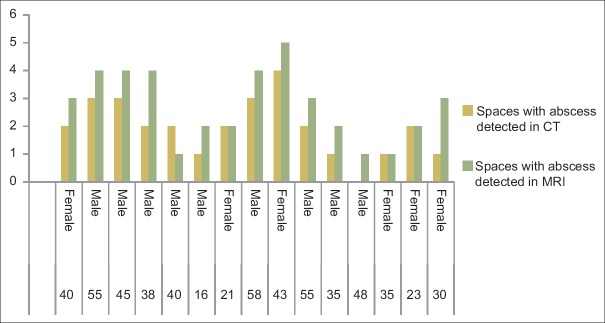
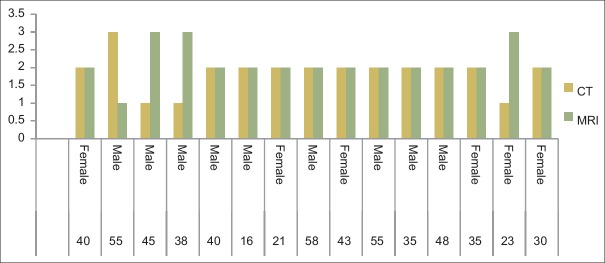
Comparison was made regarding identification of diseased anatomical spaces using CT and MRI. CT was proved to be more effective in detection of these spaces [Figure 3].
Figure 3.
Anatomic spaces with abscess detected
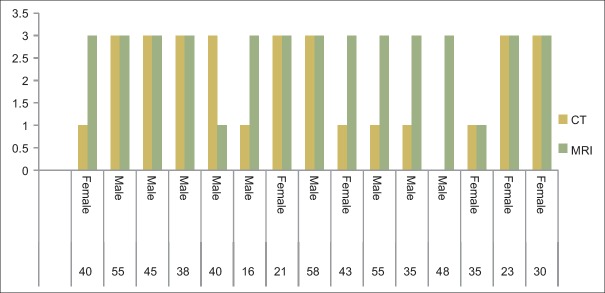
Capsule enhancement was clearly elicited under MRI among all the study participants as compared to CT, and this difference was found to be highly statistically significant (P = 0.000) [Table 1 and Figure 4].
Figure 4.
Detection of areas of capsular enhancement (abscesses)
Bony lesions were more conspicuous under MRI rather than CT, and this difference was found to be highly statistically significant (P = 0.000) [Table 1 and Figure 5].
Figure 5.
Detection of bony lesions
When comparison was made regarding intralesional gas and calcification detection, CT was found to be more conspicuous as compared to MRI, and this difference was also found statistically significant (P ≤ 0.05) [Figure 6].
Figure 6.
Detection of gas and calcifications
When comparison was made between CT and MRI in detection of skin and subcutaneous inflammation, MRI showed to be more effective as compared to CT [Figures 1 and 7].
Figure 7.
Detection of skin and subcutaneous lesions
DISCUSSION
The most common odontogenic infections are periapical abscess, pericoronitis, and periodontal abscess. These infections are a public health concern and are most common in underserved patients lacking access to health care, who often obtain their health care through the emergency room of a publically funded hospital.
Although CT and MRI are useful for depiction of the extent of odontogenic infection, the spread to the submandibular space has not completely been elucidated.
CT scan is guiding treatment in emergency cases: if it reveals only inflammatory changes (cellulitis), then antibiotic therapy should be started.
MRI has a better view of soft tissue than CT without exposure to radiation. In addition, MRI is more accurate than CT in detecting complications from deep neck infections such as internal jugular vein thrombosis or erosion of the abscess into the carotid sheath. Backdraws of MRI include longer scanning time, lack of availability, higher cost, and the potential for claustrophobia.
ACCURACY OF COMPUTED TOMOGRAPHY
Miller et al.[6] performed a prospective study on deep neck infections in adult patients, the study compared the efficacy of contrast-enhanced CT to clinical examination in detecting the presence of a drainable fluid collection.
ACCURACY OF MAGNETIC RESONANCE IMAGING
Kozuch O et al.[7] stated that MRI was superior to CT in regard to lesion conspicuity, number of anatomic spaces involved, extension, and source. CT was superior to MRI in the detection of intralesional gas and calcium and showed fewer motion artifacts.
Our study was performed over head and neck infections. In 12 of the patients, the cause of head and neck infection was odontogenic in origin. This is in accordance with other reports, stating that dental infections have become one of the most important sources of deep neck infections in the western world, particularly involving the masticator, parapharyngeal, and submandibular spaces.[8] This is due to the close relationship between the dental roots and the adjacent muscles of the mandible and floor of the mouth.
In 3 of our patients, nonodontogenic was the cause of the infection. In one case, extension of disease and involvement of a carotid artery wall are visualized using CT which is superior to MRI. Common vascular complication of infections is suppurative internal jugular vein thrombosis.
Two patients had adult supraglottitis, an acute infection of the epiglottis and supraglottic structures. In accurate diagnosis of such cases in addition to clinical grounds, cross-sectional studies are also needed. In both patients, CT and MRI showed findings similar to those reported elsewhere. CT was superior to MRI in terms of lesion conspicuity in one patient with an extensive neck abscess containing gas had a long-standing pharyngoesophageal achalasia. Gas was poorly seen on MRI, and that study was degraded by motion.
Based on our observations, MRI as used here was superior to CT in the assessment of acute neck infections. MRI was superior for anatomic discrimination, lesion conspicuity, and extension of the lesion and to identify the number of anatomic spaces involved in 11 patients of our study. MRI detected the underlying lesion regardless of its origin. When both techniques are compared on the basis of odontogenic origin, the number of spaces detected by CT was statistically less than those seen by MRI. These data suggest that MRI has high diagnostic than CT and that odontogenic processes may be more difficult to assess accurately by CT.
Both CT and MR studies showed a dental lesion on the one side and the inflammatory process was located on the other side of the mandible, and in some cases, chronic dental infections are incidental, and the source of acute infection, detected in imaging studies made the dental lesions misleading in both techniques. MRI was also helpful when specific anatomic regions were seen. On CT, soft tissue landmarks may not be detected certainity if dental amalgam is encountered or the lesion is adjacent to it. We evaluated two patients with infections in this location. In one of them, MRI demonstrated the location of the lesion on the floor of the mouth clearly than that seen on CT.
It has been pointed out that the edge of abscess may show fewer enhancements on MRI than is seen on CT. We did not observe this and believe that it may be easily prevented using fat-suppression technique. CT is inferior to MRI in detection of abscesses. In our study, CT is an appropriate imaging tool, used not only for the daignosis of deep neck space infections but also to show the extent of the disease. CT scans are not only beneficial in differentiating between cellulitis and abscesses but also have an important role in the evaluation of serious complications. A contrast CT scan also helps to decide whether a surgical intervention is indicated, as patients with radiological evidence of cellulitis respond well to medical treatment, whereas those with abscess have a higher incidence of complications and usually require surgical management due to the aggressive nature of this condition.[9] MRI was proved to be less accurate for some calcium detection cases such as sialolithiasis.
MRI findings changed the initial treatment when the lesion conspicuity affected patients care, atleast in three patients. In two of them, small abscesses were discovered by MRI, and in one patient, MRI helped to direct the extension of infection and its surgical approach. The potential of MRI in changing diagnosis and treatment has been reported, particularly in infections involving the tongue and the floor of the mouth.
We used relatively thick (5–7 mm) sections on the CT studies. Since our data were acquired over a 1-year period and thin sections were not available, we are not able to comment on the performance of CT using thinner sections. Although section thickness could have skewed the data to favor MRI, this parameter is not solely responsible for the advantages of MRI over CT.
Our study has several shortcomings. Firstly, The patient population in our study was not selected on radilogical basis. Conversely, most patients with acute swelling, tender, and superficial, suppurative abscess who presented with a draining fistula immediately underwent surgical drainage and were also excluded from the study. After initial CT studies about 10% of the patients, also underwent MRI. It is possible that in these few patients, the natural evolution of the disease promoted changes that were easier to detect on MRI. CT scans with contrast are helpful in detection of neck infections. CT scans indicate the location, boundaries, and relation of infection to surrounding structures. Abscesses are observed as low-density lesions with rim enhancement, occasional air-fluid levels, and loculations, while MRI scans can give excellent soft-tissue resolution to help localize the region of involvement.[10]
CONCLUSION
CT and MRI are quick and accurate methods for the evaluation of head and neck infections. MRI is superior to CT in regard to lesion conspicuity and determining the number of anatomic spaces involved and the degree of extension and the source. MRI scanning is helpful for patients in whom distinction between the mass and surrounding soft-tissue structures on CT is poor. MRI better displays lower neck without any shoulder artifact which is commonly seen in CT. Gas-containing lesions are better demonstrated by computerized topography. We hereby conclude that, in patients with no airway compromis and with an acute infection of neck clinically, MRI can be used for the initial examination and in most patients it allows for definite diagnosis.
FINANCIAL SUPPORT AND SPONSORSHIP
Nil.
CONFLICTS OF INTEREST
There are no conflicts of interest.
REFERENCES
- 1.Zhu Q, Zhu W, Wu J, Zhang H. The CT and MRI observations of small cell neuroendocrine carcinoma in paranasal sinuses. World J Surg Oncol. 2015;13:54. doi: 10.1186/s12957-015-0475-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Muñoz A, Castillo M, Melchor MA, Gutiérrez R. Acute neck infections: Prospective comparison between CT and MRI in 47 patients. J Comput Assist Tomogr. 2001;25:733–41. doi: 10.1097/00004728-200109000-00011. [DOI] [PubMed] [Google Scholar]
- 3.Kozuch O, Mayer V. Pig kidney epithelial (PS) cells: A perfect tool for the study of flaviviruses and some other arboviruses. Acta Virol. 1975;19:498. [PubMed] [Google Scholar]
- 4.Ariji Y, Gotoh M, Kimura Y, Naitoh M, Kurita K, Natsume N, et al. Odontogenic infection pathway to the submandibular space: Imaging assessment. Int J Oral Maxillofac Surg. 2002;31:165–9. doi: 10.1054/ijom.2001.0190. [DOI] [PubMed] [Google Scholar]
- 5.Miller WD, Furst IM, Sàndor GK, Keller MA. A prospective, blinded comparison of clinical examination and computed tomography in deep neck infections. Laryngoscope. 1999;109:1873–9. doi: 10.1097/00005537-199911000-00029. [DOI] [PubMed] [Google Scholar]
- 6.Holliday RA, Peudezgast NC. Imaging inflammatory processes of the oral cavity and suprahyoid neck. Oral Maxillofac Surg Clin North Am. 1992;4:215–40. [Google Scholar]
- 7.Som PM. The present controversy over the imaging method of choice for evaluating the soft tissues of the neck. AJNR Am J Neuroradiol. 1997;18:1869–72. [PMC free article] [PubMed] [Google Scholar]
- 8.Muñoz A, Ballesteros AI, Brandariz Castelo JA. Primary lingual abscess presenting as acute swelling of the tongue obstructing the upper airway: Diagnosis with MR. AJNR Am J Neuroradiol. 1998;19:496–8. [PMC free article] [PubMed] [Google Scholar]
- 9.Kataria G, Saxena A, Bhagat S, Singh B, Kaur M, Kaur G, et al. Deep neck space infections: A study of 76 cases. Iran J Otorhinolaryngol. 2015;27:293–9. [PMC free article] [PubMed] [Google Scholar]
- 10.Murray AD, Meyers AD. Deep Neck Infections. 2017 May 04; [Google Scholar]