Abstract
Background
Early readmissions are important indicators of quality of care. Limited data exist describing hospital readmissions in ulcerative colitis (UC). The aim of this study was to describe unplanned, 30-day readmissions among adult UC patients and to assess readmission predictors.
Methods
We analyzed the 2013 United States National Readmission Database and identified UC admissions using administrative codes in patients from 18 to 80 years of age. Our primary outcome was a 30-day, unplanned readmission rate. We used chi-square tests, t tests, and Wilcoxon rank-sum tests for descriptive analyses and survey logistic regression to calculate adjusted odds ratios (aORs) and 95% confidence intervals (CIs) for associations with readmissions adjusting for confounders.
Results
Among 26,094 hospitalizations with a primary UC diagnosis, there were 2757 (10.6%) 30-day, unplanned readmissions. The most common readmission diagnoses were reasons related to UC (58%), complications of surgical procedures/medical care (5.5%), Clostridium difficile (4.8%), and septicemia (4.3%). In multivariable analysis, length of stay ≥7 days (aOR 1.54, 95% CI, 1.24–1.90), not having an endoscopy (aOR 1.20, 95% CI, 1.04–1.38), and depression (aOR 1.40, 95% CI, 1.16–1.66) were significantly associated with readmission. 58.2% of readmissions had at least one of these factors. Patients were also less likely to be admitted if they were women or had self-pay payer status. Having a colectomy did not significantly increase readmissions (aOR 1.14, 95% CI, 0.86–1.52).
Conclusions
On a national level, 1 in 10 hospitalizations for UC was followed by an unplanned readmission within 30 days. Not having an endoscopy on the index hospitalization and depression were independently associated with readmissions. Further studies should examine if strategies that address these predictors can decrease readmissions.
Keywords: hospitalization, depression, length of stay, inflammatory bowel disease
Reducing hospital readmissions has become a priority for health care throughout the United States to improve quality of care and decrease costs. It has been estimated that up to one-fifth of Medicare patients are readmitted within 30 days with an annual cost of $17.4 billion because of unplanned readmissions of which one-third may be preventable.1–3 Around 27% of hospital read-missions may be avoidable, although some estimates are as high as 79%.2 Decreasing readmissions is of importance to health care systems given financial disincentives and penalties around reimbursement for 30-day readmissions and to patients by avoiding the direct and indirect burden and costs of hospitalizations.
It is estimated that at least 3 million people in the United States have inflammatory bowel disease (IBD) with around half having ulcerative colitis (UC).4 The incidence of IBD has been rising over time.5 The total direct and indirect costs of UC in the United States are estimated to be between $8.1 and $14.9 billion annually, of which hospitalizations account for up to one half.6,7 Half of all UC patients have at least 1 hospitalization during their lifetime.8 Despite significant advances in medical therapy, hospitalization rates for UC have not decreased and may have even increased recently with rates ranging from 8.2 to 12.4 per 100,000 per year.9,10 In addition, the number of hospitalization days is now considered an outcome measure for quality of care in IBD according to a set of IBD quality indicators developed by an expert panel.11
Although hospitalizations are a significant driver of health care utilization among UC patients, relatively little is known about the epidemiology and risk factors for 30-day readmissions for UC in the United States. Most prior data on UC readmissions have been from single center experiences or other countries.12–16 Therefore, we analyzed an all-payer, nationally representative database to describe unplanned 30-day readmissions and to assess predictors of readmission among adult UC patients in the United States.
MATERIALS AND METHODS
Data Source
We used the National Readmissions Database (NRD) which is sponsored by the Agency for Healthcare Research as part of the quality Healthcare Cost and Utilization Project (HCUP).17 The NRD is derived from HCUP State Inpatient Databases and includes weighted discharge data with over 100 clinical and nonclinical variables for each hospital stay. Data are from 21 geographically diverse states accounting for 49.3% of the U.S. population. It includes approximately 14 million unweighted discharges (49.1% of all U.S. discharges) corresponding to 36 million annual discharges nationwide. The only publicly released NRD data is from 2013 which was used for this study.
Study Population and Design
We queried the NRD using the International Classification of Diseases, Ninth Revisions, Clinical Modification (ICD-9-CM) diagnosis code 556.x to identify all admissions for patients with UC. We only included hospitalizations of adult patients with age ≥18 or <80 years at the time of index admission. Patients 80 years or older were excluded to limit misclassification of conditions such as ischemic colitis.18 Exclusion criteria included ICD-9-CM for both UC and CD, pregnancy, chemotherapy, death on index hospitalization, lack of discharge disposition data, and length of stay (LOS) less than 24 hours. In addition, index admissions from December 2013 were excluded because they lacked 30 days for accrual of readmissions.
Index admissions were any hospitalization without any other hospitalizations within the prior 30 days. Readmissions were identified as any unplanned hospitalization within 30 days of a prior admission; therefore, an individual patient could have several readmissions associated with a single index admission. The primary diagnosis on admission was defined according to the Clinical Classification Software codes. We classified patients as having a primary diagnosis of UC on index hospitalization or as having UC as a secondary diagnosis. The top Clinical Classification Software diagnoses were selected to describe the primary diagnoses for 30-day readmissions.
Definition of Covariates
Covariates included patient demographics such as age, sex, comorbidities, and quartile classification of median household income extrapolated from ZIP code. We used All Patient Refined—Diagnosis Related Group (APR-DRG) scores as an indicator for severity of illness.4 Case-mix adjustment was performed using the updated Elixhauser Agency for Healthcare Research and Quality-Web ICD-9-CM comorbidity algorithms (Agency for Healthcare Research and Quality, Rockville, MD), which include congestive heart failure, chronic pulmonary disease, diabetes without complications, and depression.19 Other comorbidities included malnutrition, primary biliary cirrhosis, primary sclerosing cholangitis, smoking, hepatitis, nonalcoholic fatty liver disease, and osteoarthritis. Index hospitalization information included hospital region, hospital teaching status, hospital size, hospital administration, discharge disposition, LOS, and payer type. The NRD has grouped payer types as Medicaid (fee-for-service and managed care Medicaid patients), Medicare, private (commercial carriers, private HMOs and PPOs), self-pay, no charge, and other payer (including Worker’s Compensation, Civilian Health and Medical Program of the Uniformed Services, Civilian Health and Medical Program of the Department of Veterans Affairs, Title V, and other government programs).
Discharge disposition was grouped into routine or self-care, short-term hospital nursing facility, home health care, against medical advice (AMA), and discharged alive (unknown). We identified admissions through emergency department by the HCUP indicator of emergency department record criteria and elective admissions per data available from source hospitals. Detailed description of NRD data is accessible online (https://www.hcup-us.ahrq.gov/nrdoverview.jsp).
Statistical Analyses
Our primary outcome was any 30-day unplanned readmission after an index admission for UC. Secondary outcomes included rate of readmissions among patients with UC as a secondary diagnosis on index admission and primary diagnosis for 30-day readmission. Descriptive statistics for patient and hospitalization variables were compiled comparing patients with and without at least one 30-day readmission. We used chi-square tests for categorical variables, student’s t test for normally distributed continuous variables, and Wilcoxon rank-sum tests for non-normally distributed continuous variables. Although both weighted and unweighted admissions are reported in the study flow diagram, only weighted numbers were analyzed.
We used survey logistic regression to assess the relationship between predictors of readmission and odds of having at least 1 30-day unplanned readmission. This analysis was chosen given the NRD data which involves nested, weighted observations that are inherently stratified in clusters to produce national estimates.20 We adjusted for patient, hospital, and index admission characteristics. Patient characteristics included age, sex, endoscopy or colectomy performed, comorbidities, and median household income. Hospital characteristics included bed size, hospital type/administration, and urban–rural designation. Index admission characteristics included APR-DRG Severity Scale, LOS, primary payer type, discharge disposition, and emergency or elective admission status. We performed all associations using designated weighted values provided by HCUP to produce nationally representative estimates and considered a 2-tailed P value ≤0.05 as statistically significant. We used SAS 9.4 (SAS Institute Inc., Cary, NC) for all analyses.
Ethical Considerations
Because this study involved de-identified, publicly available data it was exempted from institutional review board approval.
RESULTS
After applying all inclusion and exclusion criteria, we identified 75,093 index admissions with a UC diagnosis (Fig. 1). 26,904 index admissions had UC as the primary diagnosis whereas 48,189 admissions had UC as a secondary diagnosis. The 30-day unplanned readmission rate after an index admission with a primary UC diagnosis was 10.6%. The study population characteristics with univariate analyses are presented in Table 1.
FIGURE 1.
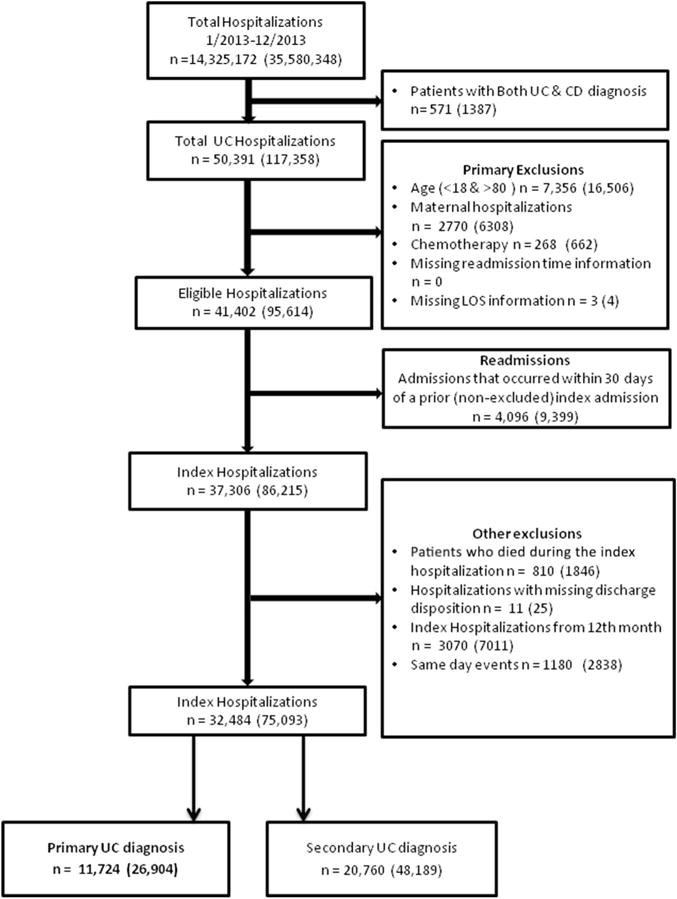
Flowsheet of creation of study cohort. Number of patients (weighted number). Admissions with no prior admissions within 30 days; index hospitalizations with 30-day nonelective readmission were flagged; elective readmissions were not considered as readmissions.
TABLE 1.
Study Population Characteristics
| No Readmissions (n = 24,147) |
At Least One 30-Day Readmission (n = 2757) | P | |
|---|---|---|---|
| Patient characteristics | |||
| Age in years, n (%) | 0.0005 | ||
| Median (IQR) | 43.93 (29.48–58.49) | 41.05 (28.29–58.47) | |
| 18–34 | 8166 (33.82) | 1035 (37.63) | |
| 35–49 | 5935 (24.58) | 652 (23.63) | |
| 50–64 | 5814 (24.08) | 599 (21.72) | |
| ≥65 | 4232 (17.53) | 469 (17.02) | |
| Sex, n (%) | <0.0001 | ||
| Men | 11,536 (47.78) | 1472 (53.37) | |
| Women | 12,610 (52.22) | 1286 (46.63) | |
| Endoscopy performed | 9393 (38.9) | 1018 (36.92) | 0.04 |
| Colectomy | 2132 (8.83) | 237 (8.60) | 0.68 |
| Comorbidities, n (%) | |||
| Congestive heart failure | 518 (2.15) | 57 (2.07) | 0.8 |
| Chronic pulmonary disease | 2682 (11.11) | 281 (10.18) | 0.14 |
| Depression | 2642 (10.94) | 370 (13.42) | <0.0001 |
| Diabetes mellitus | 2466 (10.21) | 287 (10.41) | 0.75 |
| Hypertension | 6934 (28.72) | 737 (26.73) | 0.03 |
| Osteoarthritis | 907 (3.76) | 78 (2.82) | 0.01 |
| Malnutrition | 1397 (5.79) | 182 (6.59) | 0.09 |
| Smoking | 5532 (22.91) | 616 (22.32) | 0.49 |
| Primary sclerosing cholangitis | 215 (0.89) | 37 (1.32) | 0.03 |
| Primary biliary cirrhosis | 15 (0.06) | 0 (0) | 0.19 |
| Nonalcoholic fatty liver disease | 341 (1.41) | 20 (0.72) | 0.003 |
| Median household income category for patient’s ZIP code, n (%)a | 0.01 | ||
| 0–25th percentile | 5610 (23.23) | 714 (25.88) | |
| 26th–50th percentile | 6106 (25.29) | 645 (23.4) | |
| 51st–75th percentile | 6342 (26.27) | 712 (25.83) | |
| 76th–100th percentile | 5752 (23.82) | 652 (23.64) | |
| Index admission characteristics | |||
| Admission source, n (%)b | 0.09 | ||
| Non-emergency department | 7257 (30.05) | 786 (28.51) | |
| Emergency department | 16,890 (69.95) | 1971 (71.49) | |
| Admission type, n (%) | 0.18 | ||
| Nonelective | 19,607 (81.2) | 2268 (82.26) | |
| Elective | 4513 (18.69) | 487 (17.66) | |
| APR-DRG Severity Scale, n (%)c | <0.0001 | ||
| Minor loss of function | 5271 (21.83) | 603 (21.87) | |
| Moderate loss of function | 13,751 (56.95) | 1470 (53.3) | |
| Major loss of function | 4421 (18.31) | 576 (20.89) | |
| Extreme loss of function | 704 (2.92) | 109 (3.94) | |
| LOS in days, n (%) | <0.0001 | ||
| Median (IQR) | 3.52 (2.06–5.74) | 3.99 (2.24–6.54) | |
| <2 | 5772 (23.9) | 594 (21.53) | |
| 3–4 | 8131 (33.67) | 790 (28.66) | |
| 5–6 | 4706 (19.49) | 571 (20.72) | |
| ≥7 | 5538 (22.93) | 802 (29.09) | |
| Primary payer type, n (%) | <0.0001 | ||
| Medicare | 5234 (21.67) | 598 (21.69) | |
| Medicaid | 3134 (12.98) | 412 (14.94) | |
| Private | 12,169 (50.4) | 1422 (51.56) | |
| Self-pay | 3573 (14.8) | 326 (11.81) | |
| Discharge disposition | 0.58 | ||
| Routine | 20,355 (84.3) | 2292 (83.13) | |
| Short-term hospital | 155 (0.64) | 19 (0.71) | |
| Nursing facility | 722 (2.99) | 94 (3.39) | |
| Home health care | 2660 (11.02) | 321 (11.65) | |
| Against medical advice | 256 (89.19) | 31 (10.81) | |
| Cost of hospitalization in USD, median (IQR) | 7467 (4780.1–12,680) | 7913.3 (4911.7–14,082) | |
| Hospital characteristics | |||
| Hospital bed size, n (%)d | 0.31 | ||
| Small | 3000 (12.42) | 346 (12.56) | |
| Medium | 5368 (22.23) | 646 (23.44) | |
| Large | 15,778 (65.34) | 1764 (63.99) | |
| Hospital type, n (%)e | 0.05 | ||
| Metropolitan nonteaching | 8763 (36.29) | 970 (35.17) | |
| Metropolitan teaching | 13,219 (54.74) | 1570 (56.92) | |
| Non-metropolitan hospital | 2165 (8.96) | 218 (7.91) | |
| Hospital administration, n (%)f | 0.66 | ||
| Government, nonfederal | 2820 (11.68) | 306 (11.1) | |
| Private, not for profit | 17,903 (74.14) | 2060 (74.72) | |
| Private, for profit | 3424 (14.18) | 390.96 (14.18) | |
| Hospital urban–rural designation, n (%) | 0.06 | ||
| Large urban (>1 million) | 14,689 (60.83) | 1745 (63.29) | |
| Small urban (<1 million) | 7293 (30.2) | 794 (28.8) | |
| Rural (<10,000) | 1582 (6.55) | 163 (5.92) | |
| Other | 583 (2.41) | 55 (1.99) |
Frequencies (%) in the columns may not sum up to 100% because there might be missing data.
This represents a quartile classification of the estimated median household income of residents in the patient’s ZIP Code. These values are derived from ZIP Code demographic data obtained from Claritas.
HCUP criteria for evidence of ED services includes: (1) Emergency department revenue code of 450–459 on record; (2) Positive emergency department charge, when revenue center codes are not available; (3) Emergency department CPT code of 99,281–99,285 reported on record; (4) Condition Code of P7 (NUBC preferred coding for public reporting as of July 1, 2010); (5) Point of origin of ED (NUBC preferred coding from October 1, 2007 to June 30, 2010); (6) Admission source of ED (NUBC preferred coding before October 1, 2007).
The All Patient Refined-Diagnosis Related Groups (APR-DRGs) are assigned using software developed by 3M Health Information Systems.
Bed size categories are based on hospital beds and are specific to the hospital’s location and teaching status. Bed size assesses the number of short-term acute beds in a hospital. Hospital information was obtained from the AHA Annual Survey of Hospitals.
The hospital’s teaching status was obtained from the AHA Annual Survey of Hospitals. A hospital is considered to be a teaching hospital if it has an AMA-approved residency program, is a member of the Council of Teaching Hospitals (COTH) or has a ratio of full-time equivalent interns and residents to beds of 0.25 or higher. Non-metropolitan hospitals were not split according to teaching status as rural teaching hospitals were rare. The metropolitan categorization is a simplified adaptation of the 2003 version of the Urban Influence Codes and includes both large and small metropolitan areas.
The hospital’s administration category was obtained from the AHA Annual Survey of Hospitals and includes categories for government nonfederal (public), private not for profit (voluntary) and private investor-owned (proprietary).
IQR, interquartile range.
Patients with a primary UC index hospitalization who subsequently had a 30-day unplanned readmission were more likely to be younger, men, less likely to have had a colonoscopy on index admission, had significantly higher rates of depression and PSC, lower median household income, and more severe loss of function on the APR-DRG scale. Thirty-day readmissions were also significantly associated with longer LOS (≥7 days), Medicaid or private insurance, and index hospitalization at a metropolitan teaching hospital. The most common primary diagnoses for readmissions were UC (58.2%), complications of surgical/medical care (5.5%), Clostridium difficile infection (4.8%), septicemia (4.3%), and intestinal obstruction (2.3%).
Among 48,189 index admissions that had UC as a secondary diagnosis, there were 3419 unplanned 30-day readmissions (7.0%). The most common reasons for the index admission were septicemia (7.6%), intestinal infection (6.2%), intestinal obstruction (4.1%), other gastrointestinal disorders (3.9%), complications related to surgical/medical care (3.2%), and pneumonia (2.4%). The most common primary diagnoses for 30-day readmissions among patients with index admission with UC as secondary diagnosis included UC (13.2%), septicemia (7.3%), complications of surgical/medical care (5.9%), complications of device (4.7%), and C. difficile infection (3.8%).
Lastly, we conducted multivariable analyses to assess which covariates are associated with increased risk of 30-day unplanned readmission after index hospitalization with UC as primary diagnosis (Table 2). After adjusting for patient, hospital, comorbidity, and admission confounders, not having a colonoscopy on index hospitalization was associated with 20% higher odds for readmissions (adjusted odds ratio 1.20, 95% confidence interval [CI], 1.04–1.38) and depression was associated with 40% higher odds (adjusted odds ratio 1.40, 95% CI, 1.16–1.66). A length of stay of LOS ≥7 days on index hospitalization was associated with 54% higher odds of readmission (OR 1.54, 95% CI, 1.24–1.90). 58.2% of readmissions had at least one of these predictors during the index hospitalization. In addition, patients were less likely to be readmitted if they were women or if the hospitalization was covered by self-pay (Table 2). Colectomy during index admission did not significantly increase 30-day readmission risk (adjusted odds ratio 1.14, 95% CI, 0.86–1.52).
TABLE 2.
Association of Variables From Index UC Hospitalization With Unplanned 30-Day Readmission
| Adjusted OR | P | |
|---|---|---|
| Patient characteristics | ||
| Age in years, n (%) | ||
| 18–34 | Referent | |
| 35–49 | 0.85 (0.71–1.02) | 0.09 |
| 50–64 | 0.81 (0.66–0.99) | 0.04 |
| ≥65 | 0.85 (0.643–1.14) | 0.28 |
| Sex, n (%) | ||
| Men | Referent | |
| Women | 0.77 (0.66–0.89) | 0.0003 |
| No endoscopy performed | 1.20 (1.04–1.38) | 0.01 |
| Colectomy | 1.14 (0.86–1.52) | 0.35 |
| Comorbidities, n (%) | ||
| Depression | 1.40 (1.13–1.66) | 0.001 |
| Nonalcoholic fatty liver disease | 0.50 (0.26–0.93) | 0.03 |
| Primary sclerosing cholangitis | 1.37 (0.77–2.44) | 0.29 |
| Osteoarthritis | 0.81 (0.55–1.20) | 0.29 |
| Hypertension | 0.93 (0.77–1.12) | 0.43 |
| Hepatitis | 0.81 (0.48–1.38) | 0.44 |
| Chronic pulmonary disease | 0.93 (0.74–1.17) | 0.52 |
| Diabetes mellitus | 1.07 (0.85–1.35) | 0.58 |
| Congestive heart failure | 0.88 (0.53–1.44) | 0.6 |
| Smoking | 0.98 (0.83–1.15) | 0.81 |
| Malnutrition | 0.99 (0.75–1.32) | 0.97 |
| Median household income category for patient’s ZIP code, n (%)a | ||
| 0–25th percentile | Referent | |
| 26th–50th percentile | 0.83 (0.68–1.01) | 0.06 |
| 51st–75th percentile | 0.85 (0.69–1.05) | 0.14 |
| 76th–100th percentile | 0.83 (0.67–1.01) | 0.07 |
| Index admission characteristics | ||
| Admission source, n (%)b | ||
| Non-emergency department | 0.90 (0.72–1.13) | 0.37 |
| Emergency department | Referent | |
| Admission type, n (%) | ||
| Nonelective | 1.10 (0.83–1.18) | 0.52 |
| Elective | Referent | |
| APR-DRG Severity Scale, n (%)c | ||
| Minor loss of function | Referent | |
| Moderate loss of function | 0.94 (0.79–1.11) | 0.45 |
| Major loss of function | 1.07 (0.85–1.34) | 0.57 |
| Extreme loss of function | 1.07 (0.70–1.61) | 0.78 |
| LOS in days, n (%) | ||
| <2 | Referent | |
| 3–4 | 0.99 (0.82–1.18) | 0.88 |
| 5–6 | 1.30 (1.04–1.62) | 0.02 |
| ≥7 | 1.54 (1.23–1.90) | <0.0001 |
| Primary payer type, n (%) | ||
| Medicaid | Referent | |
| Medicare | 0.98 (0.74–1.29) | 0.87 |
| Private | 1 (0.77–1.14) | 0.54 |
| Self-pay or no charge or others | 0.70 (0.56–0.88) | 0.001 |
| Discharge disposition | ||
| Routine | Referent | |
| Skilled nursing care | 0.91 (0.63–1.32) | 0.62 |
| Short-term hospital | 1.10 (0.52–2.34) | 0.81 |
| Home health care | 0.98 (0.79–1.23) | 0.87 |
| Against medical advice | 1.13 (0.65–1.98) | 0.67 |
| Hospital characteristics | ||
| Hospital bed size, n (%)d | ||
| Small | 1.07 (0.86–1.33) | 0.56 |
| Medium | 1.10 (0.92–1.31) | 0.28 |
| Large | Referent | |
| Hospital type, n (%)e | ||
| Metropolitan teaching | Referent | |
| Metropolitan nonteaching | 0.95 (0.880–1.13) | 0.56 |
| Non-metropolitan hospital | 0.80 (0.44–1.43) | 0.45 |
| Hospital administration, n (%)f | ||
| Government, nonfederal | Referent | |
| Private, not for profit | 1.02 (0.83–1.24) | 0.87 |
| Private, for profit | 1.03 (0.78–1.37) | 0.81 |
| Hospital urban–rural designation, n (%) | ||
| Large urban (>1 million) | Referent | |
| Small urban (<1 million) | 0.90 (0.77–1.05) | 0.17 |
| Rural (<10,000) | 1.06 (0.53–2.12) | 0.87 |
Table 2 analyses adjusted for age, sex, endoscopy or colectomy performed, comorbidities, median household income, hospital bed size, hospital type/administration, urban–rural designation, APR-DRG Severity Scale, LOS, primary payer type, discharge disposition, and emergency or elective admission status.
This represents a quartile classification of the estimated median household income of residents in the patient’s ZIP Code. These values are derived from ZIP Code demographic data obtained from Claritas.
HCUP criteria for evidence of ED services includes: (1) Emergency department revenue code of 450–459 on record; (2) Positive emergency department charge, when revenue center codes are not available; (3) Emergency department CPT code of 99,281–99,285 reported on record; (4) Condition Code of P7 (NUBC preferred coding for public reporting as of July 1, 2010); (5) Point of origin of ED (NUBC preferred coding from October 1, 2007 to June 30, 2010); (6) Admission source of ED (NUBC preferred coding before October 1, 2007).
The All Patient Refined-Diagnosis Related Groups (APR-DRGs) are assigned using software developed by 3M Health Information Systems.
Bed size categories are based on hospital beds and are specific to the hospital’s location and teaching status. Bed size assesses the number of short-term acute beds in a hospital. Hospital information was obtained from the AHA Annual Survey of Hospitals.
The hospital’s teaching status was obtained from the AHA Annual Survey of Hospitals. A hospital is considered to be a teaching hospital if it has an AMA-approved residency program, is a member of the Council of Teaching Hospitals or has a ratio of full-time equivalent interns and residents to beds of 0.25 or higher. Non-metropolitan hospitals were not split according to teaching status as rural teaching hospitals were rare. The metropolitan categorization is a simplified adaptation of the 2003 version of the Urban Influence Codes and includes both large and small metropolitan areas.
The hospital’s administration category was obtained from the AHA Annual Survey of Hospitals and includes categories for government nonfederal (public), private not for profit (voluntary) and private investor-owned (proprietary).
DISCUSSION
In a nationally representative U.S. database, patients admitted for UC had a 10.6% 30-day unplanned readmission rate. Over half of the readmissions had UC as the primary diagnosis. On multivariable analysis, patients were significantly more likely to be readmitted if they had depression, did not have an endoscopy on the index admission, and LOS ≥7 days. Most readmissions had at least one of these predictors. To the best of our knowledge, this is one of the first studies to examine UC readmissions in the United States on a national level.
One prior study presented in abstract form used the state inpatient databases and found that 19% of patients with IBD-related hospitalizations were readmitted within 30 days.21 This rate is higher than what we observed in our study, but subgroup data on UC patients were not available, and predictors of readmission were not reported. Other studies that have examined readmission rates in UC have been primarily single center experiences. A study from Cleveland Clinic found that IBD patients admitted to a gastroenterology service had a 30-day all-cause readmission rate of 18%, although the rate for UC alone was not reported.22 This is also higher than the 10.6% 30-day readmission rate found in our study. The difference in findings may reflect the higher severity of patients at a tertiary care center compared with the general hospitalized population which is captured by the NRD. Alternatively, the higher readmission rate may have been driven by Crohn’s disease patients who made up nearly three-fourth of the study population. Factors associated with readmission in this study included narcotics prescription on discharge, benzodiazepines during hospitalization, abscess drainage, and discharge to an assisted-care facility. The 30-day readmission rate in the NRD was similar to the findings from a retrospective study of severe UC patients admitted to the Mount Sinai Medical Center between 2007 and 2011 which reported a 30-day all-cause readmission rate of 11.7%.12 In this study, the only significant independent predictors of 30-day readmission were extensive colitis, albumin on admission, and admission to a housestaff service.
The only national-level studies on IBD readmissions are from Canada. A large study from the pre-biologic era used a national database to examine hospitalizations from 1994 to 2001.16 16.7% of UC patients were readmitted within 2 years with a median time to readmission of 11 months. Thirty-day readmissions were not specifically reported. A more recent study from Canada analyzed over 26,000 patients who were hospitalized for IBD between 2004 and 2010 and found a 1 month readmission rate of 2.4% among UC patients, which is substantially lower than our cohort.14 Predictors of readmission for all IBD patients included younger age, lower IBD volume hospital, and surgery. We were unable to determine IBD volume by hospital based on the NRD data and did not see a significant impact of surgery on readmission risk. There was a trend toward increased readmission risk for the youngest age group (18–34 years), but this was statistically significant only when compared with the 50 to 64 years old age group.
Regarding patient demographics, prior studies on the general Medicare population found that male sex was a risk factor for 30-day readmission.1 Male UC patients were at higher risk of readmissions than female patients in our study. The reasons for this are unclear and warrant further investigation in future studies. In addition, we found that patients who were self-pay and did not have insurance coverage for their index hospitalization were less likely to be readmitted. This likely highlights a socioeconomic group that is less likely to use health services given the cost burden.
Our observed 30-day unplanned readmission rate for UC is similar or somewhat lower than rates seen in other common inpatient gastrointestinal conditions. The unplanned 30-day readmission rate for upper and lower gastrointestinal bleeding in recent studies varies from 5% to 21% with the range likely attributable to differences in study populations and methods.23–26 Thirty-day readmission rates after hospitalizations for acute pancreatitis are higher at around 20%.27,28 Additionally, 30-day readmission rate among patients admitted for cirrhosis and related complications was 12.9% in a recent population-based study.29
We found that depression significantly increased the odds of readmission by 40%. Depression is a major comorbidity for many UC patients and can have a major impact on IBD in a number of ways including increased symptoms, medication nonadherence, illicit drug use, and negative illness perception30,31 Around 22% of UC patients have depression and rates increase in active disease.32 In a prospective observational study, clinically inactive IBD patients with depression were more likely to have a relapse over an 18 month follow-up period.33 Major depressive disorder increases the chance of treatment failure with infliximab in Crohn’s disease.34 Depression has been associated with readmissions in non-IBD patients. According to a meta-analysis, patients admitted to medical services were more likely to be readmitted within 30 days if they had a history of depressive symptoms (RR 1.73, 95% CI, 1.16–2.58).35 Depression also increased the readmission risk in chronic obstructive pulmonary disease.36 Our results highlight the importance of addressing depression in UC, particularly during and after hospitalization.30–32
Patients in our study were more likely to have a 30-day readmission if they did not have an endoscopy during the index hospitalization. It is generally recommended that patients with severe UC admitted to the hospital undergo a flexible sigmoidoscopy.37 For example, the Toronto consensus statements on hospitalized UC recommend flexible sigmoidoscopy early in the course of hospitalization to assess disease severity and identify superinfections such as cytomegalovirus.38 Endoscopic disease severity can help clinicians risk stratify patients by identifying those more likely to need rescue therapies (biologics or cyclosporine) and those at highest risk of colectomy.37,39 Our data suggest the importance of performing an endoscopic evaluation for patients admitted with UC as it may decrease subsequent readmissions.
Lastly, LOS ≥7 days was a significant predictor of 30-day readmission. Longer LOS has previously been associated with readmissions in other diseases. For example, data on heart failure hospitalizations suggest that patients with longer LOS are significantly more likely to have a 30-day readmission.40 In a study on colorectal resections, patients who required an emergency readmission had longer LOS during their index admissions.41 In contrast to these findings, a large study of Veterans Affairs hospitals found no significant relationship between LOS and overall risk of 30-day readmission although hospitals with a mean risk-adjusted LOS that was lower than expected had a higher readmission rate suggesting a potential inverse relationship.42 For patients admitted primarily for UC, it is likely that a longer LOS may be a surrogate marker for higher disease severity. Although fewer than 10% of the patients in our cohort underwent colectomy during index hospitalization, a national study of UC patients who underwent colectomy more than 6 days after admission had significantly increased morbidity and mortality.43 We were unfortunately unable to assess disease severity with the NRD data. However, it is likely that UC patients who are in the hospital longer are sicker and not responding to first line treatments such as steroids, and are then undergoing rescue therapy with infliximab or cyclosporine which would lead to a longer LOS.
Based on our findings and prior studies, a number of potentially modifiable risk factors for readmission have been identified that hospitals and clinicians can potentially address. First, comorbid mental health issues, in particular depression, can be helped by linking patients with appropriate psychological or psychiatric care. Performing a flexible sigmoidoscopy during an admission for UC should be strongly considered for a number of reasons including getting a more accurate assessment of disease severity which may lead to a better informed treatment plan and decreased risk of readmission. Decreasing LOS, if feasible, may decrease readmission rates but LOS may not be modifiable as it is potentially a marker of disease severity. Readmission rates also may be lower at centers with higher IBD volume. Lastly, admission to a house staff service has been associated with a higher risk of readmission. Careful oversight in these cases will ensure appropriate care and disposition; however, this may be a marker of disease severity as more acute patients are typically admitted to house staff services.
Our study had several limitations. First, the NRD does not provide data on race or ethnicity, and we were therefore unable to account for these potentially confounding variables in our analysis. Second, these data rely on administrative health claims so we could not directly verify the coded diagnoses nor were we able to specifically assess UC disease severity for these admissions. However, we were able to control for general disease severity using the APR-DRG scale and adjusting for the comorbidity index. Because the NRD only contains data from hospitalizations, we were not able to study what occurred in between the index hospitalization and readmission. For example, seeing a physician soon after discharge may potentially decrease the risk of readmission. Although there are inherent limitations to using administrative health claims codes (i.e., verification of diagnoses, accuracy of coding), the NRD allows for careful tracking of readmissions across hospitals and similar administrative data have previously been used to study readmissions among Medicare patients and Veterans.44,45 Lastly, only the primary payer for hospitalization was available so the effect of secondary insurances could not be studied.
In summary, patients in a national database who were admitted for a primary diagnosis of UC had a 10.6% rate of 30-day readmission and were more likely to be readmitted if they had an LOS ≥7 days, did not have an endoscopy on the index hospitalization, or had depression. These factors may be used to identify higher risk UC patients who should be targeted for interventions to decrease risk of readmission such as closely coordinated outpatient follow up, better assessment and treatment of psychosocial factors, or enrollment in a medical home.46 The rate of 30-day readmission in the U.S. NRD is higher than comparable data from Canada and can be used as a baseline to measure the impact of interventions. Future studies are needed to further understand approaches to decreasing unplanned hospitalizations in UC.
Footnotes
The authors have no conflict of interest to disclose.
References
- 1.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 2.van Walraven C, Bennett C, Jennings A, et al. Proportion of hospital readmissions deemed avoidable: a systematic review. CMAJ. 2011;183:E391–E402. doi: 10.1503/cmaj.101860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leppin AL, Gionfriddo MR, Kessler M, et al. Preventing 30-day hospital readmissions: a systematic review and meta-analysis of randomized trials. JAMA Intern Med. 2014;174:1095–1107. doi: 10.1001/jamainternmed.2014.1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dahlhamer JM, Zammitti EP, Ward BW, et al. Prevalence of Inflammatory Bowel Disease Among Adults Aged ≥18 Years – United States, 2015. MMWR Morb Mortal Wkly Rep. 2016;65:1166–1169. doi: 10.15585/mmwr.mm6542a3. [DOI] [PubMed] [Google Scholar]
- 5.Molodecky NA, Soon IS, Rabi DM, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012;142:46–54.e42. doi: 10.1053/j.gastro.2011.10.001. quiz e30. [DOI] [PubMed] [Google Scholar]
- 6.Cohen RD, Yu AP, Wu EQ, et al. Systematic review: the costs of ulcerative colitis in Western countries. Aliment Pharmacol Ther. 2010;31:693–707. doi: 10.1111/j.1365-2036.2010.04234.x. [DOI] [PubMed] [Google Scholar]
- 7.Kappelman MD, Rifas-Shiman SL, Porter CQ, et al. Direct health care costs of Crohn’s disease and ulcerative colitis in US children and adults. Gastroenterology. 2008;135:1907–1913. doi: 10.1053/j.gastro.2008.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Samuel S, Ingle SB, Dhillon S, et al. Cumulative incidence and risk factors for hospitalization and surgery in a population-based cohort of ulcerative colitis. Inflamm Bowel Dis. 2013;19:1858–1866. doi: 10.1097/MIB.0b013e31828c84c5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bewtra M, Su C, Lewis JD. Trends in hospitalization rates for inflammatory bowel disease in the United States. Clin Gastroenterol Hepatol. 2007;5:597–601. doi: 10.1016/j.cgh.2007.01.015. [DOI] [PubMed] [Google Scholar]
- 10.Nguyen GC, Tuskey A, Dassopoulos T, et al. Rising hospitalization rates for inflammatory bowel disease in the United States between 1998 and 2004. Inflamm Bowel Dis. 2007;13:1529–1535. doi: 10.1002/ibd.20250. [DOI] [PubMed] [Google Scholar]
- 11.Melmed GY, Siegel CA, Spiegel BM, et al. Quality indicators for inflammatory bowel disease: development of process and outcome measures. Inflamm Bowel Dis. 2013;19:662–668. doi: 10.1097/mib.0b013e31828278a2. [DOI] [PubMed] [Google Scholar]
- 12.Tinsley A, Naymagon S, Mathers B, et al. Early readmission in patients hospitalized for ulcerative colitis: incidence and risk factors. Scand J Gastroenterol. 2015;50:1103–1109. doi: 10.3109/00365521.2015.1020862. [DOI] [PubMed] [Google Scholar]
- 13.Hanzlik TP, Tevis SE, Suwanabol PA, et al. Characterizing readmission in ulcerative colitis patients undergoing restorative proctocolectomy. J Gastrointest Surg. 2015;19:564–569. doi: 10.1007/s11605-014-2734-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nguyen GC, Bollegala N, Chong CA. Factors associated with readmissions and outcomes of patients hospitalized for inflammatory bowel disease. Clin Gastroenterol Hepatol. 2014;12:1897–1904.e1. doi: 10.1016/j.cgh.2014.02.042. [DOI] [PubMed] [Google Scholar]
- 15.Feuerstein JD, Jiang ZG, Belkin E, et al. Surgery for ulcerative colitis is associated with a high rate of readmissions at 30 days. Inflamm Bowel Dis. 2015;21:2130–2136. doi: 10.1097/MIB.0000000000000473. [DOI] [PubMed] [Google Scholar]
- 16.Bernstein CN, Nabalamba A. Hospitalization, surgery, and readmission rates of IBD in Canada: a population-based study. Am J Gastroenterol. 2006;101:110–118. doi: 10.1111/j.1572-0241.2006.00330.x. [DOI] [PubMed] [Google Scholar]
- 17.Agency for Healthcare Research and Quality. The Nationwide Readmissions Database Overview. Available at: http://www.hcup-us.ahrq.gov/nrdoverview.jsp. Accessed October 18, 2016.
- 18.Picco MF, Cangemi JR. Inflammatory bowel disease in the elderly. Gastroenterol Clin North Am. 2009;38:447–462. doi: 10.1016/j.gtc.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 19.Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Rader KA, Lipsitz SR, Fitzmaurice GM, et al. Bias-corrected estimates for logistic regression models for complex surveys with application to the United States’ Nationwide Inpatient Sample. Stat Methods Med Res. 2015 doi: 10.1177/0962280215596550. [epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sethi S, Wadhwa V, Moss A. U.S. readmission rates and costs following hospitalization for inflammatory bowel disease. Am J Gastroenterol. 2013;108:S541. [Google Scholar]
- 22.Hazratjee N, Agito M, Lopez R, et al. Hospital readmissions in patients with inflammatory bowel disease. Am J Gastroenterol. 2013;108:1024–1032. doi: 10.1038/ajg.2012.343. [DOI] [PubMed] [Google Scholar]
- 23.Strömdahl M, Helgeson J, Kalaitzakis E. Emergency readmission following acute upper gastrointestinal bleeding. Eur J Gastroenterol Hepatol. 2016;29:73–77. doi: 10.1097/MEG.0000000000000746. [DOI] [PubMed] [Google Scholar]
- 24.Sengupta N, Tapper EB, Patwardhan VR, et al. High Glasgow Blatchford Score at admission is associated with recurrent bleeding after discharge for patients hospitalized with upper gastrointestinal bleeding. Endoscopy. 2016;48:9–15. doi: 10.1055/s-0034-1392651. [DOI] [PubMed] [Google Scholar]
- 25.Quan S, Frolkis A, Milne K, et al. Upper-gastrointestinal bleeding secondary to peptic ulcer disease: incidence and outcomes. World J Gastroenterol. 2014;20:17568–17577. doi: 10.3748/wjg.v20.i46.17568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sengupta N, Tapper EB, Patwardhan VR, et al. Risk factors for adverse outcomes in patients hospitalized with lower gastrointestinal bleeding. Mayo Clin Proc. 2015;90:1021–1029. doi: 10.1016/j.mayocp.2015.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Whitlock TL, Repas K, Tignor A, et al. Early readmission in acute pancreatitis: incidence and risk factors. Am J Gastroenterol. 2010;105:2492–2497. doi: 10.1038/ajg.2010.234. [DOI] [PubMed] [Google Scholar]
- 28.Whitlock TL, Tignor A, Webster EM, et al. A scoring system to predict readmission of patients with acute pancreatitis to the hospital within thirty days of discharge. Clin Gastroenterol Hepatol. 2011;9:175–180. doi: 10.1016/j.cgh.2010.08.017. quiz e18. [DOI] [PubMed] [Google Scholar]
- 29.Tapper EB, Halbert B, Mellinger J. Rates of and reasons for hospital readmissions in patients with cirrhosis: a multistate population-based cohort study. Clin Gastroenterol Hepatol. 2016;14:1181–1188.e2. doi: 10.1016/j.cgh.2016.04.009. [DOI] [PubMed] [Google Scholar]
- 30.Brooks AJ, Rowse G, Ryder A, et al. Systematic review: psychological morbidity in young people with inflammatory bowel disease—risk factors and impacts. Aliment Pharmacol Ther. 2016;44:3–15. doi: 10.1111/apt.13645. [DOI] [PubMed] [Google Scholar]
- 31.Neuendorf R, Harding A, Stello N, et al. Depression and anxiety in patients with inflammatory bowel disease: a systematic review. J Psychosom Res. 2016;87:70–80. doi: 10.1016/j.jpsychores.2016.06.001. [DOI] [PubMed] [Google Scholar]
- 32.Mikocka-Walus A, Knowles SR, Keefer L, et al. Controversies revisited: a systematic review of the comorbidity of depression and anxiety with inflammatory bowel diseases. Inflamm Bowel Dis. 2016;22:752–762. doi: 10.1097/MIB.0000000000000620. [DOI] [PubMed] [Google Scholar]
- 33.Mittermaier C, Dejaco C, Waldhoer T, et al. Impact of depressive mood on relapse in patients with inflammatory bowel disease: a prospective 18-month follow-up study. Psychosom Med. 2004;66:79–84. doi: 10.1097/01.psy.0000106907.24881.f2. [DOI] [PubMed] [Google Scholar]
- 34.Persoons P, Vermeire S, Demyttenaere K, et al. The impact of major depressive disorder on the short- and long-term outcome of Crohn’s disease treatment with infliximab. Aliment Pharmacol Ther. 2005;22:101–110. doi: 10.1111/j.1365-2036.2005.02535.x. [DOI] [PubMed] [Google Scholar]
- 35.Pederson JL, Warkentin LM, Majumdar SR, et al. Depressive symptoms are associated with higher rates of readmission or mortality after medical hospitalization: a systematic review and meta-analysis. J Hosp Med. 2016;11:373–380. doi: 10.1002/jhm.2547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Iyer AS, Bhatt SP, Garner JJ, et al. Depression is associated with readmission for acute exacerbation of chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2016;13:197–203. doi: 10.1513/AnnalsATS.201507-439OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hindryckx P, Jairath V, D’Haens G. Acute severe ulcerative colitis: from pathophysiology to clinical management. Nat Rev Gastroenterol Hepatol. 2016;13:654–664. doi: 10.1038/nrgastro.2016.116. [DOI] [PubMed] [Google Scholar]
- 38.Bitton A, Buie D, Enns R, et al. Treatment of hospitalized adult patients with severe ulcerative colitis: Toronto consensus statements. Am J Gastroenterol. 2012;107:179–194. doi: 10.1038/ajg.2011.386. author reply 195. [DOI] [PubMed] [Google Scholar]
- 39.Carbonnel F, Lavergne A, Lémann M, et al. Colonoscopy of acute colitis. A safe and reliable tool for assessment of severity. Dig Dis Sci. 1994;39:1550–1557. doi: 10.1007/BF02088063. [DOI] [PubMed] [Google Scholar]
- 40.Reynolds K, Butler MG, Kimes TM, et al. Relation of acute heart failure hospital length of stay to subsequent readmission and all-cause mortality. Am J Cardiol. 2015;116:400–405. doi: 10.1016/j.amjcard.2015.04.052. [DOI] [PubMed] [Google Scholar]
- 41.Kelly M, Sharp L, Dwane F, et al. Factors predicting hospital length-of-stay and readmission after colorectal resection: a population-based study of elective and emergency admissions. BMC Health Serv Res. 2012;12:77. doi: 10.1186/1472-6963-12-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kaboli PJ, Go JT, Hockenberry J, et al. Associations between reduced hospital length of stay and 30-day readmission rate and mortality: 14-year experience in 129 Veterans Affairs hospitals. Ann Intern Med. 2012;157:837–845. doi: 10.7326/0003-4819-157-12-201212180-00003. [DOI] [PubMed] [Google Scholar]
- 43.Kaplan GG, McCarthy EP, Ayanian JZ, et al. Impact of hospital volume on postoperative morbidity and mortality following a colectomy for ulcerative colitis. Gastroenterology. 2008;134:680–687. doi: 10.1053/j.gastro.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 44.Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309:355–363. doi: 10.1001/jama.2012.216476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nuti SV, Qin L, Rumsfeld JS, et al. Association of admission to veterans affairs hospitals vs non-veterans affairs hospitals with mortality and readmission rates among older men hospitalized with acute myocardial infarction, heart failure, or pneumonia. JAMA. 2016;315:582–592. doi: 10.1001/jama.2016.0278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Regueiro MD, McAnallen SE, Greer JB, et al. The inflammatory bowel disease specialty medical home: a new model of patient-centered care. Inflamm Bowel Dis. 2016;22:1971–1980. doi: 10.1097/MIB.0000000000000819. [DOI] [PubMed] [Google Scholar]


