To the Editor: Percutaneous nephrolithotomy (PCNL) is a surgical procedure commonly used to treat large kidney stones. It is usually accompanied by severe pain and discomfort postoperatively. Intravenous opioids and local anesthetic infiltration have been conventionally used to control postoperative pain. In addition, regional blocks, for example, the paravertebral block and intercostal block, have been attempted. However, the efficacy of these blocks for analgesia has not been established yet.[1] Erector spinae plane block (ESPB) reportedly provides effective analgesia after thoracic and abdominal surgery.[2,3] We describe a patient in whom continuous ESPB was used to provide highly effective analgesia after PCNL.
This study was approved by our hospital's institutional review board. A 67-year-old man (weight 61 kg and height 171 cm) was admitted to undergo PCNL for a right kidney stone. He had controlled hypertension and diabetes mellitus, and his laboratory test values were unremarkable. PCNL was performed under general anesthesia in the lateral position.
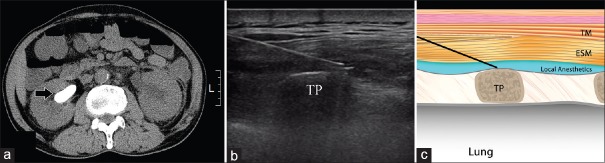
Postoperatively, nephrostomy tubes were placed, and ESPB was performed. The location of the eighth rib was found using a counting down approach from the first rib under ultrasonography (WS 80A, Samsung Medicine, Seoul, Korea) and marked on the skin. The skin was sterilized using chlorhexidine. After placing a 5–12 MHz linear probe parallel to the vertebral axis at the level of the eighth rib, the probe was moved from the lateral side to medial side transversely to identify any change in shape that transited the rib and transverse process (TP). When the round shadow of the rib shifted into the rectangular shape of the TP, an 18-gauge Tuohy needle (Perifix, B. Braun Melsungen AG, Melsungen, Germany) was inserted toward the trapezius and erector spinae and the TP of T8 using the plane technique in a cephalad-to-caudal direction [Figure 1a]. After the needle made contact with the TP, we confirmed that this fascial plane was well separated by injecting 2 ml of saline. Then, we injected the prepared mixture of 0.75% ropivacaine (10 ml, Naropin, AstraZeneca, Luton, UK) and saline (10 ml) with epinephrine (1:200,000), and a 19-gauge catheter was inserted 2 cm over the tip of the needle under real-time ultrasound guidance [Figure 1b and 1c].
Figure 1.
Representative image of the patient. (a) Computed tomography scan. Arrow, the staghorn calculi in the right kidney. (b) Ultrasound-guided erector spinae plane block. (c) Schematic diagram. Local anesthetic is injected between the ESM and TP. ESM: Erector spinae muscle; TM: Trapezius muscle; TP: Transverse process.
The patient received intravenous ketorolac (30 mg) and fentanyl (50 mcg) postoperatively. Postoperative multimodal analgesia was performed according to our hospital's acute pain service protocol, which includes oral zaltoprofen (80 mg twice daily) and manual ESPB catheter injection of a 1:1 mixture of 0.75% ropivacaine (10 ml) and saline (10 ml) with epinephrine (1:200,000) every 12 h for 5 days. Resting and dynamic ambulation pain scores were assessed postoperatively using the visual analog scale (VAS) score. Rescue analgesia with intravenous tramadol (25 mg) was prescribed if the patient's resting VAS score was more than four.
Immediately after transfer to the postanesthesia care unit, the patient's vital signs were stable and resting VAS score was 3. Two hours postoperatively, the resting/dynamic VAS scores were 0/1. The patient did not complain of pain during rest. The dermatome of sensory blockade by pinprick was T4–L1 on the midaxillary line. The resting/dynamic VAS scores were maintained below 1 from 12 to 36 h postoperatively. After 36 h postoperatively, resting and dynamic VAS scores were both zero. No additional rescue analgesics were administered.
The main sources of acute pain after PCNL are visceral pain originating from the kidneys and ureters and somatic pain from the incision site. Renal pain is conducted through the T10–L1 spinal nerves, and ureter pain is conducted through T10–L2.[4] Moreover, cutaneous innervation of the incision site is predominantly supplied by T10–T11 (T8–T12) because the incision site and tract for PCNL is usually used in the tenth to eleventh intercostal space, or in the subcostal area.[4]
The ultrasound-guided ESPB is a simple fascial plane block, and a catheter is easily inserted into the plane. It can provide wide sensory blockade from T2–L4 to L1–L2.[2,3] A cadaveric investigation showed that dye spreads to the thoracic paravertebral space and provides visceral analgesia.[2]
In general, the total amount of morphine consumption is 43 mg for 24 h after PCNL.[5] However, the patient did not require any analgesic agents including opioids during the first 5 days postoperatively other than the local anesthetic and zaltoprofen. This indicates that ESPB provided effective postoperative analgesia.
Therefore, we believe that ESPB might be a good option for analgesia after PCNL. Further case-controlled, prospective trials are needed to evaluate the efficacy of ESPB.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published, and due efforts will be made to conceal his identity but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Peng Lyu
REFERENCES
- 1.Choi SW, Cho SJ, Moon HW, Lee KW, Lee SH, Hong SH, et al. Effect of intercostal nerve block and nephrostomy tract infiltration with ropivacaine on postoperative pain control after tubeless percutaneous nephrolithotomy: A prospective, randomized, and case-controlled trial. Urology. 2018;114:49–55. doi: 10.1016/j.urology.2017.12.004. doi: 10.1016/j.urology.2017.12.004. [DOI] [PubMed] [Google Scholar]
- 2.Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block: A Novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016;41:621–7. doi: 10.1097/AAP.0000000000000451. doi: 10.1097/AAP.0000000000000451. [DOI] [PubMed] [Google Scholar]
- 3.Restrepo-Garces CE, Chin KJ, Suarez P, Diaz A. Bilateral continuous erector spinae plane block contributes to effective postoperative analgesia after major open abdominal surgery: A case report. A A Case Rep. 2017;9:319–21. doi: 10.1213/XAA.0000000000000605. doi: 10.1213/XAA.0000000000000605. [DOI] [PubMed] [Google Scholar]
- 4.Liu Y, Yu X, Sun X, Ling Q, Wang S, Liu J, et al. Paravertebral block for surgical anesthesia of percutaneous nephrolithotomy: Care-compliant 3 case reports. Medicine (Baltimore) 2016;95:e4156. doi: 10.1097/MD.0000000000004156. doi: 10.1097/MD.0000000000004156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ak K, Gursoy S, Duger C, Isbir AC, Kaygusuz K, Ozdemir Kol I, et al. Thoracic paravertebral block for postoperative pain management in percutaneous nephrolithotomy patients: A randomized controlled clinical trial. Med Princ Pract. 2013;22:229–33. doi: 10.1159/000345381. doi: 10.1159/000345381. [DOI] [PMC free article] [PubMed] [Google Scholar]