To the Editor: Despite the numerous morphological and biomechanical studies on the anterior cruciate ligament (ACL), this anatomical structure is still under investigation; in particular, there is a discussion about its anatomical composition in relation to biomechanics. At present, in general, it is assumed that ACL comprises a structure of two bundles: anteromedial and posterolateral. Sometimes, even three bundles are distinguished; however, the presumption that ACL is an integral and continuous structure is constantly mentioned in the literature. It is known that ACL is not isometric, and the length of ACL fibers varies along with knee flexion and extension: in flexion, the length of anteromedial bundle increases (tightens), while posterolateral bundle decreases (slackens). At the same time, during knee flexion and extension, femoral part of ACL rotates, while its tibial part moves minutely.[1] It might be considered that the foreign body embedded at the distal part of ACL should have less potency for migration.
The symptoms depend on the location of the foreign body in the knee, since there are differences if the foreign body is seated in the joint cavity or at its recesses, inside the intra-articular structures, or in the periarticular subcutaneous soft tissue. Intra-articular foreign bodies can mimic different pathologies, for example, a monoarticular arthritis, a torn meniscus, and a chondral lesion, that cause recurrent pain or locking of the knee, especially if the foreign body is mobile within the knee joint. Fragments that have slight movements are embedded in the subcutaneous soft tissues, within the synovial capsule or in other synovial structures, and are often asymptomatic. Diagnosis of a foreign body in the knee is particularly confusing in case of absent definite history of injury and if no obvious scar is seen over the knee joint. Sometimes, foreign bodies in the knee might stay silent and undiagnosed for many years. The local reactions caused by foreign bodies vary widely.[2,3,4]
Injury of muscles or ligaments initiates a sequence of cellular responses, including generally neutrophil invasion and sequential increases of macrophage. Therefore, in terms of laboratory findings, macrophages are important for foreign body reactions. Polymorphonuclear leukocytes and monocytes secrete proinflammatory and/or pro-wound healing cytokines and growth factors that influence subsequent healing events. In vivo, bacterial contamination of biomaterials delays the foreign body reaction. Endotoxins, such as lipopolysaccharides, major constituents of the bacterial cell wall, are potent stimulators of the immune system in vitro and in vivo. Typical phases of injury and healing are inflammation, granulation tissue formation, matrix formation, and also remodeling. But as some authors reported, in an ACL tear, the torn fibers may disappear over time and therefore cellular response may be nontypical.[5]
A 21-year-old male college student developed anterior right knee pain and joint swelling for no apparent reason. When seen by his family doctor, the onset was insidious without mechanical symptoms. There was no obvious scar, wound, or redness over the knee joint, and no trauma was reported by the patient. Physical examination revealed only slight warmth and limited motion with mild swelling in the knee. A diagnosis of nonspecific synovitis was established, and the anti-inflammatory medication was started. The symptoms persisted approximately for one year, improved temporarily after medication, but worsened again after sports and physical activity.
After a year of complaints, the student finally recalled that one year before being seen he was kneeling on both knees and had felt a sharp pain in his right knee. On inspection, he found a sewing needle sticking out of the front of his knee. He removed the needle and disinfected the skin. The wound healed, and the student was symptom free, but several months later, he began to experience activity-related right knee pain and swelling. He recalled the needle incident and told his family doctor only after 1 year. Plain X-rays were obtained, and the lateral radiograph showed an obvious thin metal foreign body in the region of the ACL [Figure 1a].
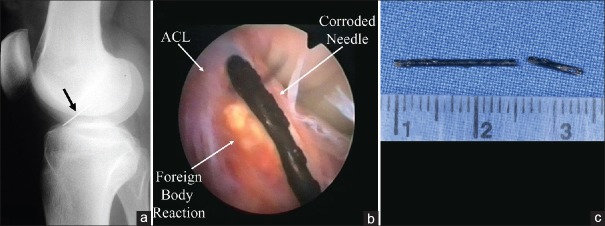
Figure 1.
A 21-year-old male with nonspecific synovitis. (a) View of the sewing needle on lateral X-ray of the knee; (b) arthroscopic view of the needle embedded in the anterior cruciate ligament (ACL); and (c) two pieces of extracted corroded needle.
The patient was referred to an orthopedic surgeon for treatment. The repeated X-rays before the surgery ensured that the foreign body did not change the position. During the arthroscopy, a corroded needle was noted to be partially embedded into the anteromedial bundle of the ACL and surrounded by inflammatory and granulomatous tissue [Figure 1b]. During the extraction with grasping forceps, the needle unexpectedly broke into two pieces [Figure 1c], and the smaller fragment sank into the posteromedial corner. During surgery, the larger part of the needle was removed by longitudinal extraction with a grasping instrument, but the smaller part was changing position because of the water turbulence in the knee. To grip, this fragment was rather tricky, and there was danger to trim this fragment into even smaller fragments. A magnetic retriever was used to catch the fragment of the broken needle and to deliver it into the anterior part of the knee. Then, grasping forceps were used to eliminate the rest of the needle from the knee. The granulomatous tissue was removed with 3.2-mm diameter shaver blade, leaving the ACL uninjured. Postoperatively, the patient was covered with prophylactic antibiotics and underwent routine rehabilitation. The patient was discharged from the hospital on the 2nd day after the operation. After half a year postoperative on the control examination, no swelling of the knee or pain was found, there was full range of motion, and the patient had uneventful recovery. Stability tests, Lachman test, and anterior drawer test showed that ACL is intact; thus, there was no need to perform magnetic resonance imaging examination.
The knee is under constant movement, usually foreign bodies migrate intra-articularly and cause symptoms. However, the diagnosis of foreign body in the knee might be aggravated, since sometimes foreign bodies can stay silent and undiagnosed for many years and cause delayed complications.[2,3,4]
The foreign body in this case was of the type that should have been detected earlier in case of well-timed recurrence of the patient, clear-cut history of the injury, thorough physical examination, and plain X-rays of the knee. The main reason for the delay in the diagnosis was due to misleading history, which is common, if the penetrating body is relatively minor and does not cause evident symptoms right after the incidence. It also reaffirms how important is accurate history taking and plain radiographs in a routine workup, and that they are essential in detecting radio opaque foreign bodies. When the patient recalled, the needle incident and X-rays were finally obtained and the correct diagnosis was established. The orthopedic surgeon rightfully repeated the films before the surgery to ensure that the position of the needle has not changed as intra-articular foreign bodies are prone to migration.
Removal of intra-articular foreign bodies during the surgery sometimes can be very challenging, loose bodies have a tendency to migrate to the back of the knee, because the arthroscopic patient's position is supine (we also faced this problem in the present case). This case demonstrates why it is very important that the surgeon should be well trained in the instrumentation of all compartments of the knee, including the posterior compartment. This includes being able to instrument the popliteal hiatus and use submeniscal approaches. It is essential to have angled scopes available. Intraoperative X-ray examination is also very important because intra-articular foreign bodies can escape into the popliteal space or other soft tissues and become unseen.[2,3]
It is rather seldom to have a foreign body in the knee, especially without obvious external scarring. We did not find a similar report of a foreign body embedded right in the ACL. Moreover, our patient was able to exercise and had only moderate complaints for a long period of time. The needle was stuck in the anteromedial bundle of the ACL close to its tibial insertion. We presume that the needle was protected from migration because of the following reasons. The connective tissue of ACL is dense and especially firm. During the knee flexion and extension, ACL rotates on a considerable degree at the place of femoral attachment, while the tibial part of ACL moves minutely.[1] Hence, the needle embedded and did not migrate from the lower part of the anteromedial bundle of ACL. On the other hand, the foreign body from the articular cavity could migrate inside or even outside the joint.
Our case report showed moderate local inflammation of the knee when the needle was embedded into the dense tissue of the ACL, probably, due to the tissue reaction to rusting metal and slight movements of the needle within ACL. On admission of the patient, general hematological and biochemical tests showed no abnormalities (only monocytes count had achieved upper normal range – 9.52%). Because the acute phase of inflammation generally is short, laboratory tests often remain in normal range, and this is in concordance with some other similar reports. However, intra-articular foreign bodies usually provoke remarkable inflammation. Often neutrophils are the first subpopulation of leukocytes that appear at the injury site, and neutrophil invasion is followed by sequential increase in the concentrations of macrophage subpopulations. Polymorphonuclear neutrophils are the first cells to take part in the local reactions to foreign body at the aseptic knee. The local reactions caused by foreign bodies vary widely.[5] Thus, in asymptomatic case of intra-articular foreign body, laboratory tests might be also unhelpful.
This case report of exclusively rare injury of tibial part of ACL showed that the diagnosis of foreign body in the knee could sometimes be challenging, as foreign body might be silent for a long time, if embedded within the slightly mobile structure. The present case report highlighted the importance of accurate taking of the injury history and the significance of plain X-rays in case of vague knee arthritis and demonstrates why it is very important that the surgeon should be well trained in instrumentation of all compartments of the knee.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published and due efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We would like to thank Dr. James L. Baldwin from the Portland Knee Clinic for providing valuable advises and revision of English language.
Footnotes
Edited by: Xin Chen
REFERENCES
- 1.Bicer EK, Lustig S, Servien E, Selmi TA, Neyret P. Current knowledge in the anatomy of the human anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2010;18:1075–84. doi: 10.1007/s00167-009-0993-8. doi: 10.1007/s00167-009-0993-8. [DOI] [PubMed] [Google Scholar]
- 2.Oztekin HH, Aslan C, Ulusal AE, Sertoz SZ, Ustaoglu RG, Fowler J, et al. Arthroscopic retrieval of sewing needle fragments from the knees of 3 children. Am J Emerg Med. 2006;24:506–8. doi: 10.1016/j.ajem.2005.12.011. doi: 10.1016/j.ajem.2005.12.011. [DOI] [PubMed] [Google Scholar]
- 3.Yeung Y, Wong JK, Yip DK, Kong JK. A broken sewing needle in the knee of a 4-year-old child: Is it really inside the knee? Arthroscopy. 2003;19:E18–20. doi: 10.1016/s0749-8063(03)00745-x. doi: 10.1016/S0749-8063(03)00745-X. [DOI] [PubMed] [Google Scholar]
- 4.Vaishya R, Vijay V, Singh H, Agarwal AK. Arthroscopic retrieval of bullet from knee. Apollo Med. 2016;13:127–32. doi: 10.1016/j.apme.2016.03.004. [Google Scholar]
- 5.Cohen HC, Joyce EJ, Kao WJ. Biomaterials selectively modulate interactions between human blood-derived polymorphonuclear leukocytes and monocytes. Am J Pathol. 2013;182:2180–90. doi: 10.1016/j.ajpath.2013.02.022. doi: 10.1016/j.ajpath.2013.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]