Abstract
Background:
There is limited evidence about the association between ambient temperature and the incidence of pediatric hand, foot, and mouth disease (HFMD) nationwide in China.
Objectives:
We examined the childhood temperature-HFMD associations across mainland China, and we projected the change in HFMD cases due to projected temperature change by the 2090s.
Methods:
Data on daily HFMD (children 0–14 y old) counts and weather were collected from 362 sites during 2009–2014. Daily temperature by the 2090s was downscaled under the Representative Concentration Pathway (RCP) 4.5 and 8.5 scenarios. Temperature-HFMD associations were quantified using a two-stage Poisson regression with a distributed lag nonlinear model. The impact of changes in temperature on the incidence of HFMD was estimated by combining the fitted temperature-HFMD associations with projected temperatures under each scenario, assuming a constant population structure. Sensitivity analyses were performed to assess the influence of primary model assumptions.
Results:
During 2009–2014, HFMD cases were reported. In most regions, the temperature-HFMD association had an inverted U shape with a peak at approximately , but the association leveled off or continued to increase in the Inner Mongolia and Northeast regions. When estimates were pooled across all regions and the population size was held constant, the projected incidence of HFMD increased by 3.2% [95% empirical confidence interval (eCI): , 20.0%] and 5.3% (95% eCI: , 44.0%) by the 2090s under the RCP 4.5 and 8.5 scenarios, respectively. However, regional projections suggest that HFMD may decrease with climate change in temperate areas of central and eastern China.
Conclusion:
Our estimates suggest that the association between temperature and HFMD varies across China and that the future impact of climate change on HFMD incidence will vary as well. Other factors, including changes in the size of the population at risk (children 0–14 y old) will also influence future HFMD trends. https://doi.org/10.1289/EHP3062
Introduction
Hand, foot, and mouth disease (HFMD) is a common illness that predominantly affects young children. It is caused by a group of enteroviruses and is readily transmitted through coughs or sneezes or through contact with infected feces or contaminated surfaces (WHO 2012). HFMD is the primary childhood infectious disease in China: In 2016, HFMD infections (including 195 deaths) were reported nationwide, accounting for 35.2% of all 39 categories of notifiable diseases (Class A, 2; Class B, 26; Class C, 11) (National Health and Family Planning Commission of the People’s Republic of China 2017a). The majority of HFMD cases are characterized by mild and self-limiting symptoms lasting between seven and ten days, whereas others may develop severe complications affecting the central nervous and cardiopulmonary systems (WHO 2011).
Currently, there are no specific antiviral drugs or specific treatments for the disease. A vaccine against enterovirus type 71 (EV71), one of viruses causing HFMD, was approved in 2016 in China (China CDC 2016). However, the protective efficacy, safety, and affordability of this vaccine at the population level remain unknown (China CDC 2016; Chang 2016). Moreover, the vaccine may be ineffective at preventing infections from other HFMD viruses. Hence, combined with its high prevalence and morbidity, HFMD constitutes a substantial component of the burden of disease among children in China and consequently has generated widespread public health concerns in recent years (WHO 2011, 2012).
Epidemics of HFMD occur every year in China but exhibit spatiotemporal variation: The epidemic peaks in June in northern areas of the country but in May and October in some southern cities (China CDC 2015). This seasonality suggests a potential association between ambient temperature and HFMD incidence, with recent evidence indicating that it is nonlinear and lagged (Xu et al. 2015; Yin et al. 2016; Zhang et al. 2016). The use of different statistical models and exposure parameters makes it difficult to compare findings from previous studies of temperature and HFMD incidence in individual provinces or cities (Xu et al. 2015; Yin et al. 2016; Zhu et al. 2015), but these findings suggest that the association between temperature and HFMD may vary according to geographical location (Guo et al. 2016; Xiao et al. 2017). Thus, a national study using a unified statistical approach is needed to examine associations between temperature and HFMD throughout China.
Climate change has been regarded as the single largest global health issue of the 21st century (IPCC 2014). Compared with 1986–2005, the average temperature in China is projected to increase by to between 2081 and 2100 under a series of climate change scenarios, with the warming rate exhibiting spatial and seasonal differences (Tian et al. 2015). Given the association between temperature and the incidence of HFMD, we hypothesize that changes in temperature due to climate change will influence future trends in HFMD incidence. Information on possible changes in the incidence of HFMD as a consequence of climate change is needed to inform effective public health strategies to reduce the future impact of HFMD. Therefore, we conducted a study with the following aims: a) to quantify the association between temperature and HFMD across mainland China using nationally representative historical data covering the years 2009–2014; and b) to estimate the change in the incidence of HFMD associated with temperature change under different climate change scenarios by the 2090s.
Methods
Study Area
Located in East Asia along the coastline of the Pacific Ocean, China covers an area of approximately , with a north–south width of and a west–east width of (National Bureau of statistics of the People’s Republic of China 2000). There are five main landscapes in mainland China, varying from plateaus in the west to basins in the middle to plains in the east. The diversity in China’s topography, and the broad width in geography, result in various climatic zones: cold temperate in the far north, tropical in the far south, and a highland climate in the Qinghai–Tibet Plateau. The administrative divisions in mainland China follow a three-level structure: There are 31 regions at the province level [including four municipalities that in previous studies have been regarded as “megacities” (Xu et al. 2015; Zhang et al. 2017)], 333 regions at the prefecture level (including 288 prefecture cities), and 2,854 regions at the county level [including 25 counties under the jurisdiction of province (CJPs), which are of a similar administrative level to prefectures] as of the end of 2014 (National Bureau of Statistics of the People’s Republic of China 2015). For the purposes of this study, the unit of data collection and analysis was defined as municipality/prefecture/CJP. In this study, we treated Yangling district as a CJP because it is under the joint jurisdiction of Xianyang city and Shaanxi province.
Data Sources
Historical data.
Information on daily HFMD cases was collected from four municipalities, 332 prefectures, and 26 CJPs in mainland China between 1 January 2009 and 31 December 2014, with the exception of Sansha city (a prefecture set in 2012 under Hainan province). Daily data were provided by Chinese Center for Disease Control and Prevention (China CDC) through the China Information System for Disease Control and Prevention (CISDCP). Variables included age, sex, date of onset, and the site of residence.
By law, all HFMD cases must be reported directly to the China CDC within 24 h of diagnosis through CISDCP. The CISDCP covers 100% of county-level CDCs, 98% of county-level hospitals, and 94% of township clinics (National Health and Family Planning Commission of the People’s Republic of China 2015; Information Office of the State Council of the People’s Republic of China 2012). For areas without access to a telephone network, the doctor is required to inform the local CDC immediately, and the latter must report to the CISDCP within 24 h after case confirmation.
Daily meteorological data during 2009–2014, including mean temperature, relative humidity, rainfall, air pressure, wind velocity, and sunshine hours, were provided by the China Methodological Data Sharing Service System. For sites with more than one meteorological monitoring station, data closest to the center of the sites were used. The missing values were interpolated by the average of neighboring days. Population data were extracted from National Bureau of Statistics of China during the same period. Standard population data were extracted from the World (2000-2025) Standard database (Ahmad et al. 2001).
Future temperature and population data.
Daily minimum and maximum temperatures by the 2090s were downscaled as follows: Monthly projections from 28 general climate models (GCMs) (see Table S1) were first extracted from the data set of Coupled Model Intercomparison Project phase 5 (CMIP5). Data were downscaled to specific sites using an inverse interpolation method. The GCM-projected monthly values and the historical observed climate for the same period (1961–2000) were used to establish the relationship using a quantile-quantile (q-q) plot technique for bias correction. We then disaggregated daily temperature variables using a modified weather generator: Model for Generating Daily Weather Variables (WGEN) (Richardson and Wright 1984). Details of the downscaling procedure have been described in a previous study (Liu and Zuo 2012). Finally, daily mean temperature, the arithmetic mean of the minimum and maximum temperatures, was used for projecting HFMD incidence.
The CMIP5 temperature projections consist of four Representative Concentration Pathways (RCPs): RCP 2.6, RCP 4.5, RCP 6.0, and RCP 8.5 scenarios, which describe different trajectories of the future temperature change under various assumptions in greenhouse gas emissions and socioeconomic factors (Reclamation 2013). Specifically, the RCP 8.5 scenario hypothesizes no abatement in emissions by 2100, whereas the RCP 4.5 scenario assumes that climate polices and technological development will reduce the artificial emissions in a relatively practical way (Van Vuuren et al. 2011). In line with previous studies, we applied the RCP 4.5 and 8.5 scenarios, which represent relatively “better case” and “worse case” situations for future greenhouse gas emissions, respectively (Kendrovski et al. 2017; Kingsley et al. 2016; Weinberger et al. 2017).
Projections (per five years) on population 0–14 y old by 2100 were downloaded from the United Nations Population Division (UN DESA/Population Division 2017). Annual population projections were interpolated using linear regression models.
Statistical Analysis
Temperature-HFMD association.
A two-stage analysis was performed (Guo et al. 2016; Zhao et al. 2017). In the first stage, the temperature-HFMD association for each municipality, prefecture, or CJP was modeled using quasi-Poisson regression with distributed lag nonlinear model (DLNM) (Gasparrini et al. 2010). The model is described as follows:
| [1] |
where refers to the daily counts of HFMD cases diagnosed on day t in the municipality/prefecture/CJP i; is the intercept; and are the cross-basis functions modeling the nonlinear lagged effects of daily mean temperature and relative humidity, respectively; is a categorical variable of the year and calendar month to control for the long-term trend and seasonality (Xu et al. 2015; Zhu et al. 2016); is day of the week on day t; is a binary variable for adjusting the potential effect of public holidays and winter/summer school holidays; is the autoregressive term of daily HFMD counts on the logarithmic scale at lag 1–5 d to control for the autocorrelations in the residuals (Guo et al. 2016; WHO 2012; Xiao et al. 2017); and , , , and are the coefficients of the corresponding terms. A maximum lag of 14 d was used to explore the lag structure of temperature and relative humidity effects (Hii et al. 2011; Zhu et al. 2015); natural cubic splines with three degrees of freedom (dfs) were used for the spaces of temperature, relative humidity, and lag (Onozuka and Hashizume 2011; Zhu et al. 2016).
In the second stage, a multivariate random-effect meta-analysis was conducted to obtain the overall temperature-HFMD associations at the province level and at the regional level by pooling the prefecture/CJP-specific estimates (Gasparrini et al. 2012; Gasparrini and Armstrong 2013). Multivariate extensions of Cochran’s Q test and the statistic were applied to assess the residual heterogeneity (Gasparrini et al. 2012).
Our initial analysis suggested a strong negative correlation between temperature and air pressure (average coefficient: ) and a strong positive correlation between relative humidity and rainfall (average coefficient: 0.57) across all 362 sites. To avoid collinearity, air pressure and rainfall were not included in the final analysis.
Sensitivity analyses were performed to assess the robustness of temperature-HFMD associations to a change in the maximum lag from the default value of 14 d to maximum lags of 15–19 d and to additional adjustment for daily wind velocity and daily sunshine hours. We also used natural cubic splines with 7–9 dfs per year to control for seasonality and long-term trend as an alternative to using the indicator term for year and month.
Projecting future changes in HFMD cases due to changes in temperature.
The number of daily additional HFMD cases in municipality i due to daily mean temperatures differing from the reference value was calculated as follows:
| [2] |
where Pop is the size of the population 0–14 y old, represents the baseline daily incidence rate of HFMD, and ERC represents the percentage change in the risk of HFMD between the daily mean temperature and the reference temperature value, derived from equation [1]. The annual additional HFMD cases were calculated and then the percentage changes in the 2030s, the 2050s, and the 2090s were computed by comparing with the 2009–2014 average. The prefecture/CJP-specific HFMD projections were calculated using the province-level association between temperature and HFMD, the prefecture/CJP-specific reference values for daily mean temperature, and the prefecture/CJP-specific projections of future daily mean temperature. Projections using models including natural cubic splines (with 7–9 dfs per year) for seasonality and trend control were performed to assess whether changing to more flexible splines would substantially affect our findings.
Our initial analysis indicated that in the majority of municipalities/prefectures/CJPs, HFMD cases were not diagnosed on days with daily mean temperatures below (see Figure S1). This finding is consistent with laboratory evidence indicating that HFMD pathogens are only infective within a limited range of temperatures (Yeager and O’Brien 1979; Zhu et al. 2016). Therefore, when estimating the relative risk of HFMD in association with daily mean temperature, we used as the reference value for all sites where the lowest daily mean temperature at which HFMD cases were diagnosed was , and we used the actual lowest daily mean temperature at which HFMD cases were diagnosed as the reference value for all other sites (see Table S2).
In the main projection, to isolate the role of future climate, we assumed no change in the population size of children 0–14 y old or in the baseline incidence rate. In other words, our estimates of HFMD incidence related to future temperature represent the impact of climate change alone, not the combined impact of climate change, population trends, incidence rate, and other factors. Another reason for not considering future population change is that it would introduce excess uncertainty because projecting long-term changes in the population of Chinese children is unreliable because it is largely affected by the changing population policies (Xu et al. 2016; Zeng and Hesketh 2016). In comparison, fixing population to the present-day baseline may benefit health policy and planning in the context of climate change by providing projections exclusively caused by temperature anomalies (Gasparrini et al. 2017; Weinberger et al. 2017). However, we also estimated changes in HFMD after accounting for projected changes in the population size of 0–14 y old children at each site, assuming no change in the baseline HFMD incidence rate.
Uncertainties for the projection.
There are other two sources of uncertainty in projecting future HFMD incidence related to ambient temperature, including the estimates of the exposure–response relationships and the variability in temperature projections (Gasparrini et al. 2017). These quantities are represented by the variance of the model coefficient and the variability of the 28 future daily temperature series generated in each GCM, respectively. We quantified this uncertainty by generating 1,000 samples of the coefficients through Monte Carlo simulations, assuming a normal distribution for the estimated coefficients, and then generating results for each of the 28 GCMs. We report the results as point estimates, using the average across climate models (GCM-ensemble) obtained by the estimated coefficients, and as empirical confidence intervals (eCI), defined as the 2.5th and 97.5th percentiles of the empirical distribution across coefficient samples and GCMs.
R software (version 3.4.1; R Development Core Team) were used for data analysis.
Results
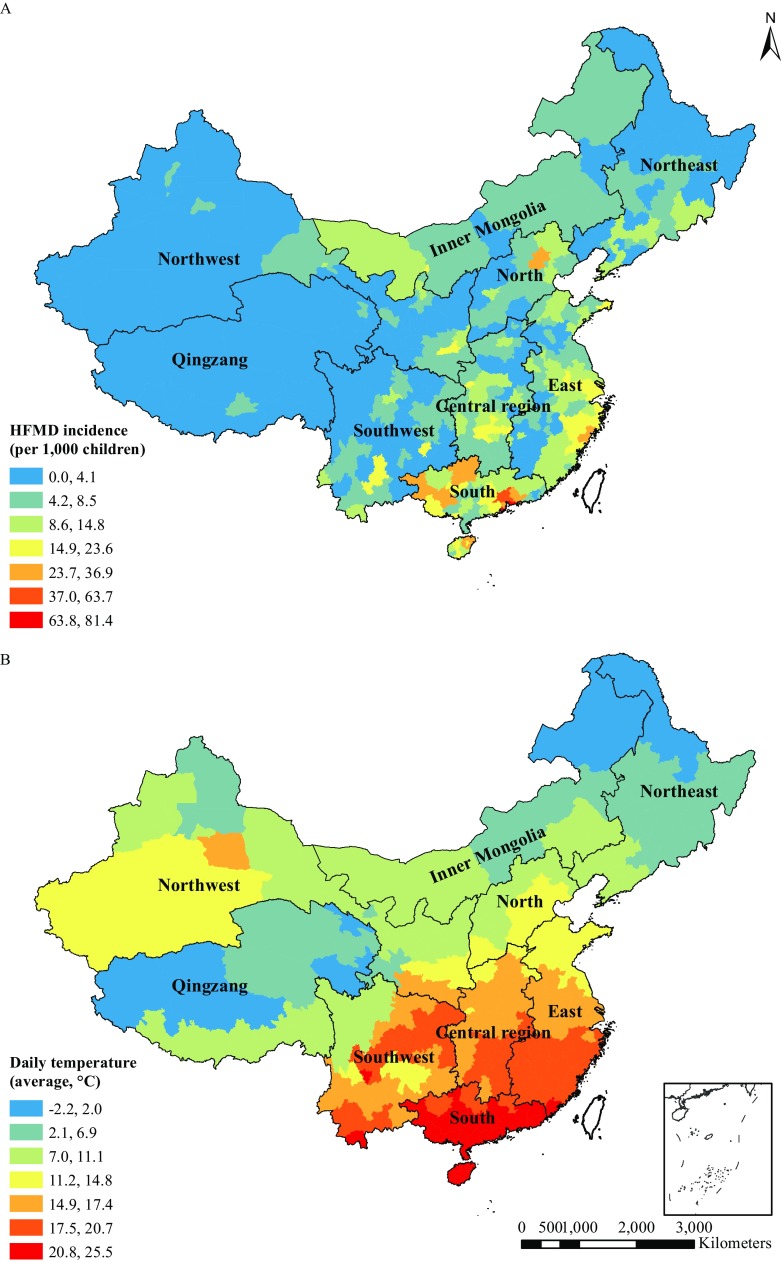
A total of 11,395,677 HFMD cases (7,059,869 boys and 4,335,805 girls) in children 0–14 y old were reported from four municipalities, 332 prefectures, and 26 CJPs in mainland China during 2009–2014, which accounted for 99.5% of all HFMD reports. The annual childhood incidence rate standardized by age (ASR) was 8.4‰ (raw rate: 8.5‰) across the 362 sites. The ASR was higher in boys (9.9‰) than in girls (6.8‰). Children 1–2 y old and those 3–5 y old had an age-specific morbidity rate of 32.7‰ and 16.5‰, respectively. Infants and children 6–14 y old both had lower incidences of approximately 1‰. The majority of sites in northern and western China had a morbidity rate under 8‰, whereas HFMD was most prevalent in the south and in the coastal regions of the east (Figure 1A). During 2009–2014, the average mean daily temperature across the 362 sites was approximately 14.5°C and warmed from the northwest to the south and east (Figure 1B). As an example, there was a clear seasonal trend of HFMD incidence in nine Chinese regions, with the highest incidence occurring from May to July and the lowest incidence occurring in January and February (see Figure S2).
Figure 1.
(A) Annual HFMD morbidity standardized by age (per 1,000 children 0–14 y old) and (B) average daily mean temperature () in four municipalities, 332 prefectures, and 26 counties under the jurisdiction of province (CJPs) in mainland China, 2009–2014. Data on daily hand, foot, and mouth disease (HFMD) and weather for each city were provided by Chinese Center for Disease Control and Prevention through the China Information System for Disease Control and Prevention and the China Meteorological Data Sharing Service System. Population data for calculating HFMD morbidity were extracted from National Bureau of Statistics of China. Maps in this publication were generated using ArcMap (version 10.5; ESRI, Inc.) with topographical basemap content from GADM.
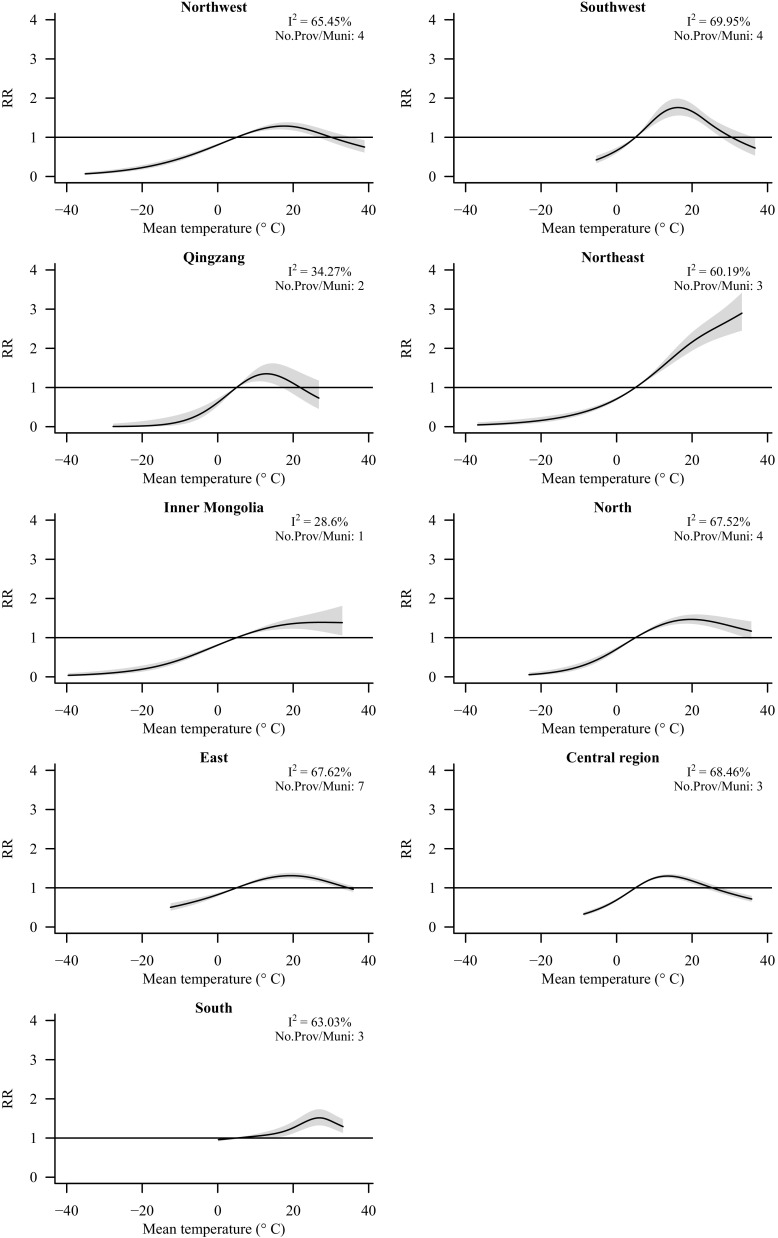
Figure 2 shows the associations between temperature and HFMD at the regional level (see Figures S3–S6 for the province- and municipality-specific relationships). Associations between temperature and HFMD were similar across sites within Inner Mongolia and Qingzang ( and 34%, respectively), whereas there were moderate levels of heterogeneity across sites within other regions ( values of 60–70%). For example, provinces in Qingzang, namely Qinghai province and the Tibet Autonomous Region, had convergent HFMD-temperature relationships, indicating almost no risk of HFMD below , above which temperature an inverted U-shaped pattern could be observed. The risk of HFMD increased with higher temperatures in the northeast, Inner Mongolia, and certain provinces in the northwest and the north. The infection risk in other regions, however, peaked at moderate temperatures around 20°C: the temperatures associated with the highest risk of HFMD infections were 27°C in the south, 19°C in the north and the east, and approximately 17°C in the northwest and the southwest. The lowest temperature of highest risk was approximately 13°C, in the central region and Qingzang (see Table S3 for the results of Cochran’s Q test and for the values of the statistic for all provinces). The statistic suggested the residual heterogeneities among prefectures or CJPs in the same province were not high for most provinces, with an average value of 49% (median value: 51%; range: 12% to 70%).
Figure 2.
Pooled cumulative associations between daily mean temperature and hand, foot, and mouth disease (HFMD) lagged over 0–14 d for 2009–2014. Black solid lines indicate region-specific associations, and shaded areas indicate 95% confidence interval bands. values and the number of provinces or municipalities included in each pooled estimate are provided. Temperature-HFMD associations were estimated by pooling the site-specific estimates using random-effect meta-analyses. Natural cubic splines (with three degrees of freedom) were used to model temperature and lag days. Note: No.Prov/Muni, the number of provinces or municipalities in the region; RR, relative risk.
Table 1 shows the projected daily mean temperature by province or municipality during 2009–2014 and during the 2030s, the 2050s, and the 2090s. The projected temperatures across all 362 sites under the RCP 4.5 scenario were 0.6°C (range: 0.5°C to 0.9°C), 1.2°C (range: 0.8°C to 1.7°C), and 1.6°C (range: 1.2°C to 2.2°C) higher in 2030s, 2050s, and 2090s, respectively, than the 2009–2014 baseline. The temperature increase under the RCP 8.5 scenario was similar to that under the RCP 4.5 scenario by the 2030s but rose to 1.8°C (range: 1.3°C to 2.6°C) and 3.8°C (range: 2.8°C to 5.7°C) during the 2050s and 2090s.
Table 1.
Prefecture/CJP-specific daily mean temperatures () with standard deviations projected in each province/municipality during 2009–2014 and the 2030s, 2050s, and 2090s
| Province or municipalitya | RCP 4.5 | RCP 8.5 | ||||||
|---|---|---|---|---|---|---|---|---|
| 2009–2014 | 2030s | 2050s | 2090s | 2009–2014 | 2030s | 2050s | 2090s | |
| Northeast | ||||||||
| Heilongjiang | ||||||||
| Jilin | ||||||||
| Liaoning | ||||||||
| Inner Mongolia | ||||||||
| Inner Mongolia | ||||||||
| North | ||||||||
| Beijingb | 13.1 | 13.8 | 14.3 | 14.8 | 13.2 | 14.0 | 15.0 | 17.1 |
| Tianjinb | 13.7 | 14.3 | 14.7 | 15.1 | 13.7 | 14.4 | 15.3 | 17.1 |
| Hebei | ||||||||
| Shanxi | ||||||||
| Northwest | ||||||||
| Xinjiang | ||||||||
| Ningxia | ||||||||
| Gansu | ||||||||
| Shaanxi | ||||||||
| East | ||||||||
| Shandong | ||||||||
| Jiangsu | ||||||||
| Anhui | ||||||||
| Shanghaib | 16.8 | 17.5 | 18.1 | 18.5 | 16.8 | 17.7 | 18.7 | 20.8 |
| Zhejiang | ||||||||
| Jiangxi | ||||||||
| Fujian | ||||||||
| Central region | ||||||||
| Henan | ||||||||
| Hubei | ||||||||
| Hunan | ||||||||
| Qingzang | ||||||||
| Qinghai | ||||||||
| Tibet | ||||||||
| Southwest | ||||||||
| Sichuan | ||||||||
| Chongqingb | 19.4 | 19.8 | 20.4 | 20.8 | 19.3 | 20.0 | 20.9 | 22.6 |
| Guizhou | ||||||||
| Yunnan | ||||||||
| South | ||||||||
| Guangdong | ||||||||
| Guangxi | ||||||||
| Hainan | ||||||||
Note: Temperature projections from 28 general climate models were downscaled from the dataset of Coupled Model Intercomparison Project phase 5. CJP, county under the jurisdiction of province; RCP, Representative Concentration Pathway.
Provinces or municipalities are sorted by region and ordered by latitude from high to low.
No standard deviations are provided for municipalities because they are treated as megacities in this study.
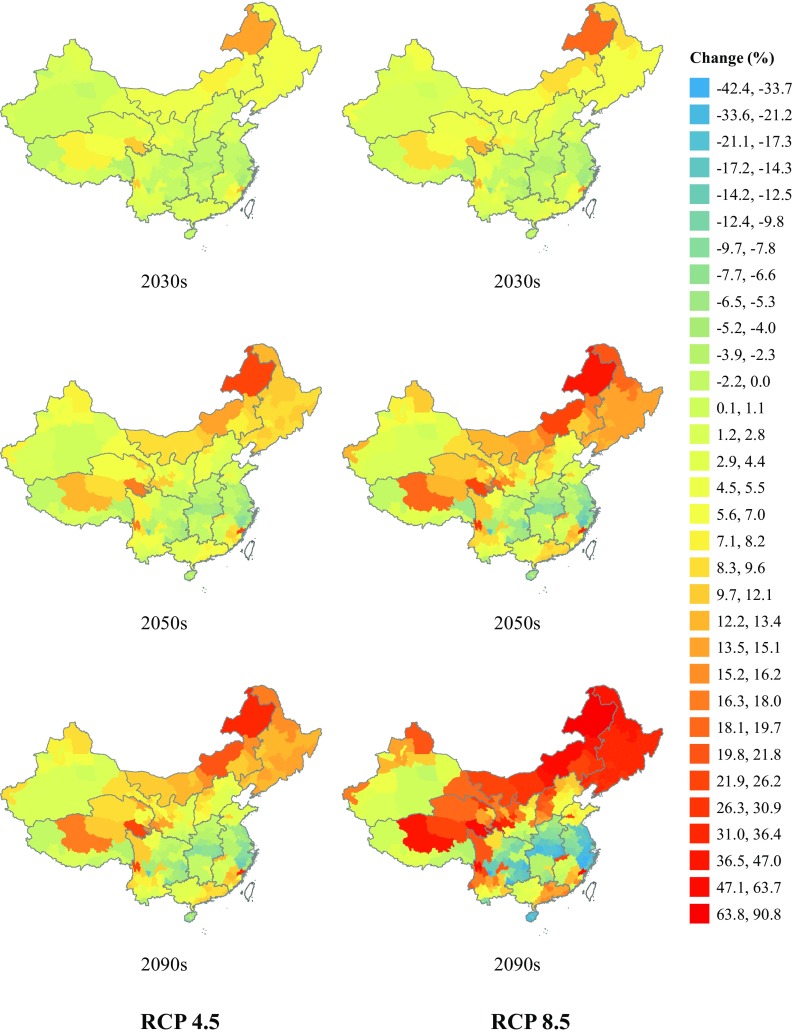
Under the RCP 4.5 scenario compared with the 2009–2014 baseline, and assuming no changes in population structure or associations between temperature and HFMD, pooled estimates over all locations suggest a slight increase in the incidence of HFMD infections for China as a whole [by 1.5% (95% eCI: , 9.1%) in the 2030s and by 3.2% (95% eCI: , 20.0%) in the 2090s] (see Table 2). These pooled estimates reflect projected increases in the Inner Mongolia, Northeast, Qingzang, North, and Northwest regions (particularly the coldest parts of these areas), with the largest regional increase estimated for Inner Mongolia [14.9% (95% eCI: , 33.7%) in the 2090s], and the largest local increase projected for the Inner Mongolian city of Hulunber [33.4% (95% eCI: 2.2%, 64.6%) in the 2090s] (Figure 3; see also Table S4). However, a decrease in HFMD incidence was projected for areas with more moderate temperatures, specifically, the Central region [ (95% eCI: , 5.7%) in the 2090s] and the East region and neighboring areas, with the largest local decline projected for Panzhihua city in Sichuan province (Southwest region) [ (95% eCI: , ) in the 2090s]. Little or no change in HFMD incidence was projected under RCP 4.5 for most of the South region (excluding Guangdong province).
Table 2.
Projected percentage change (and 95% eCI) in hand, foot, and mouth disease (HFMD) incidence among children 0–14 y old due to climate change (RCP 4.5 and 8.5 scenarios) by region and decade relative to baseline estimates for 2009–2014, holding population sizes and temperature-HFMD associations constant over time
| Region | RCP 4.5 (percentage change and 95% eCI) | RCP 8.5 (percentage change and 95% eCI) | ||||
|---|---|---|---|---|---|---|
| 2030s | 2050s | 2090s | 2030s | 2050s | 2090s | |
| Northeast | 5.4 (, 11.8) | 9.5 (0.2, 18.8) | 13.1 (1.0, 25.3) | 6.3 (1.4, 11.1) | 14.2 (6.5, 22.0) | 33.0 (17.2, 48.7) |
| Inner Mongolia | 6.0 (, 16.9) | 10.8 (, 25.2) | 14.9 (, 33.7) | 7.6 (, 18.6) | 16.8 (, 35.2) | 36.5 (, 76.1) |
| North | 2.3 (, 6.4) | 4.2 (, 9.4) | 5.8 (, 13.6) | 3.1 (, 7.2) | 6.7 (, 14.0) | 13.4 (, 28.8) |
| Northwest | 2.0 (, 8.2) | 4.3 (, 12.7) | 5.5 (, 16.2) | 3.2 (, 9.4) | 6.4 (, 17.7) | 11.9 (, 34.2) |
| East | 0.2 (, 7.3) | 0.0 (, 11.6) | (, 15.6) | 0.0 (, 8.3) | (, 16.1) | (, 28.6) |
| Central Region | (, 3.4) | (, 4.4) | (, 5.7) | (, 3.7) | (, 5.8) | (, 8.6) |
| Qingzang | 3.1 (, 13.7) | 5.2 (, 19.6) | 6.9 (, 24.5) | 4.1 (, 15.1) | 7.9 (, 26.9) | 14.4 (, 49.7) |
| Southwest | 0.6 (, 7.3) | 0.8 (, 11.6) | 0.7 (, 16.0) | 0.6 (, 8.2) | 1.0 (, 16.9) | (, 33.9) |
| South | 1.7 (, 7.6) | 2.3 (, 12.7) | 2.8 (, 17.5) | 1.6 (, 8.2) | 2.8 (, 18.1) | (, 34.5) |
| Overall | 1.5 (, 9.1) | 2.5 (, 14.8) | 3.2 (, 20.0) | 1.8 (, 10.3) | 3.6 (, 21.1) | 5.3 (, 44.0) |
Note: Pooled province level temperature-HFMD associations were used for projecting, and long-term trend and seasonality, relative humidity, day of the week, holidays (public holidays and summer and winter school holidays), and autocorrelations were controlled for in the residuals. eCI, empirical confidence interval; RCP, Representative Concentration Pathway.
Figure 3.
Projected percent change in hand, foot, and mouth disease (HFMD) incidence among children 0–14 y old due to climate change [Representative Concentration Pathway (RCP) 4.5 and 8.5 scenarios] relative to baseline estimates for 2009–2014, holding population sizes and temperature-HFMD associations constant over time. Data shown in this figure are the point estimates across 362 sites with the 95% empirical confidence intervals provided in Table S4. Maps in this publication were generated using ArcMap (version 10.5; ESRI, Inc.) with topographical basemap content from GADM.
Under the RCP8.5 scenario (with population structures and associations between temperature and HFMD held constant), pooled estimates suggest nationwide increases of 1.8% (95% eCI: , 10.3%) in the 2030s and 5.3% (95% eCI: , 44.0%) in the 2090s relative to the estimated incidence at baseline in 2009–2014 (Table 2). Geographic patterns were similar to those for the RCP 4.5 scenario (Figure 3), but the projected changes were more pronounced, with the largest regional and local increases by the 2090s again projected for Inner Mongolia and the city of Hulunber [36.5% (95% eCI: , 76.1%) and 90.8% (95% eCI: 55.7%, 125.9%), respectively] and the largest regional and local decreases projected for the Central region and Panzhihua (Sichuan province) [ (95% eCI: , 8.6%) and (95% eCI: , ), respectively] (Table 2; see also Table S4.)
Future population projections for China published by the United Nations in 2017 suggest a large decline in the proportion of the Chinese population between 0 and 14 years of age by 2100 (UN DESA/Population Division 2017), which includes those most at risk of HFMD (94% of cases diagnosed in children 0–5 y old in China in our 2009–2014 data set). Therefore, when the 2017 UN projections were used to predict future populations, the estimated incidence of HFMD declined for all regions and locations, resulting in the following nationwide HFMD incidence projections for the 2030s under the RCP4.5 and RCP 8.5 scenarios: (95% eCI: , 1.7%) and (95% eCI: , 2.8%) lower than in 2009–2014, respectively; the projections were (95% eCI: , ) and (95% eCI: , ) lower by the 2090s, respectively (see Tables S5 and S6). However, estimated reductions due to population change were offset by projected increases due to climate change, resulting in an estimated decline under RCP 8.5 of only (95% eCI: , 14.9%) by the 2090s in Inner Mongolia (see Table S5).
Associations between temperature and HFMD were similar when the maximum lag was increased from 14 d to 15–19 d (see Figure S7) and when models were additionally adjusted for daily wind velocity and sunshine hours (see Figure S8). Our analysis also indicated that estimated temperature-HFMD associations based on models using natural cubic splines (with 7–9 dfs per year) to control for seasonality and long-term trend were similar to estimates based on the primary model (with categorical indicator for year and calendar month) (see Figure S9). Projections (national level) based on the primary model were similar to projections based on models with natural cubic splines with 7–9 dfs per year (see Table S7). This finding suggests that our primary use of an indicator term for year and calendar month was reliable to control for seasonality and long-term trend, and changing to more flexible splines would not substantially affect our results.
Discussion
To our knowledge, this is the largest study to estimate nonlinear lagged association between temperature and childhood incidence of HFMD in China, and it is the first study to explore the potential impact of climate change–related temperature increases on the incidence of HFMD in children by the end of the 21st century. Our findings suggest two distinct patterns of association between temperature and HFMD: In some regions, the estimated risk of HFMD infection increased up to a moderate average daily temperature and then declined, whereas in parts of northern and western China, the estimated risk of HFMD infection continued to increase with increasing temperature. Confirmatory evidence from other countries is limited, but studies in Japan have also identified temperature-HFMD patterns similar to those we reported for northern China (Onozuka and Hashizume 2011; Urashima et al. 2003).
The transmission of HFMD is mainly due to the interaction of pathogen activity, human susceptibility, and environmental factors including temperature (Bo et al. 2014; Park et al. 2010; Ruan et al. 2011). Poor environmental hygiene (e.g., contaminated surface water) and overcrowding associated with certain outdoor activities (e.g., swimming or other aquatic sports) are related to warmer weather, which may contribute to greater risk of HFMD infection (Ashbolt 2004; Wong et al. 2010). As with single-site studies located in southern and eastern China (e.g., Guangdong and Shandong provinces) (Guo et al. 2016; Liu et al. 2013), we observed similar temperature-HFMD associations in the same regions. In these areas, the risk of infection with HFMD rose with increasing temperature and peaked at a moderate temperature before declining during the hottest days [possibly because of a reduction in outdoor activities and inactivity of the HFMD virus at high temperatures (Yin et al. 2016)]. A study from Taiwan previously reported an inverted V-shaped relationship between temperature and HFMD, with the risk of HFMD peaking at 26°C—a result comparable to the one we report for southern China (Chang et al. 2012).
Previous reports of the association between temperature and HFMD incidence have focused mainly on the most developed regions of China. In the present study, we observed that the incidence of HFMD peaked at a lower temperature in Qingzang and the Central region than in southern and eastern areas. The potential mechanism for this discrepancy remains unclear but may be related to the local poor sanitation and the frequent outdoor activities at lower temperatures compared with those in southern and eastern China. We also observed that the temperature-HFMD association was most similar for provinces or municipalities within the same region. This convergence may be due to the homogeneities in climate, level of infrastructure, population density, and behavioral customs of populations inhabiting the same area (National Bureau of statistics of the People’s Republic of China 2015).
Our findings suggest that future climate change will affect the distribution and incidence of HFMD, a major contributor to childhood morbidity in China. When the population size was held constant at the distribution for 2009–2014, pooled estimates from locations throughout China indicated a small increase in HFMD under both the RCP 4.5 and 8.5 scenarios for the country as a whole. The nationwide increase was driven by projected increases in HFMD incidence in northern and western China, particularly in areas with cooler climates. Increases in HFMD with increasing temperatures may be a dual consequence of improved survival of HFMD-causing viruses and an increase in the amount of time that children engage in outdoor activities. Importantly, some of the regions where climate change is expected to increase the risk of HFMD are among the least developed economically, with poorer public health resources, sanitation, and standards of living than in other regions of China (Chen et al. 2015; National Bureau of statistics of the People’s Republic of China 2015; Xu 2017). Our findings suggest that these areas should be the focus of government health initiatives to mitigate the effects of rising temperatures on the incidence of HFMD. In addition, our findings suggest that increasing temperatures will also promote future HFMD incidence in areas along the southeastern coast of China. Although health resources are relatively abundant in these areas, they are also expected to experience the highest population inflows in China during the next decades (Guangdong Government Department of Population and Employment 2013). In contrast, our estimates suggest a decrease in HFMD incidence with increasing temperatures in central and eastern regions of China, where the climate is more moderate. In these areas, the estimated association between temperature and HFMD at baseline had an inverted U-shaped pattern, such that increases in HFMD due to a reduction in the number of days with very low temperatures would be offset by decreases in HFMD as the number of days with very high temperatures increases.
To isolate the potential impact of climate change on HFMD, our primary models accounted for changes in temperature while holding the population size of children 0–14 y old at baseline levels for 2009–2014. We also performed sensitivity analyses using recent UN projections to account for the combined impact of climate change and predicted changes in Chinese population size on the incidence of HFMD. According to these projections, the number of children 0–14 y old would decrease by 7% in the 2030s and by 35% in the 2090s compared with the 2009–2014 average (UN DESA/Population Division 2017). The projected incidence of HFMD based on these models decreased over time in all regions and locations because of the substantial reduction in the size of the population at risk. However, the reduction in HFMD due to population change was less pronounced in areas where higher temperatures are expected to promote HFMD survival and spread. In addition, the number of children 0–14 y old may not reduce as rapidly as previously expected given the end of the one-child policy in 2016 (National Bureau of Statistics of the People’s Republic of China 2017; National Health and Family Planning Commission of the People’s Republic of China 2017b).
This study has several limitations that warrant mention. First, we used ambient temperature data from fixed meteorological monitoring stations instead of individual-level exposure. Although this may have introduced measurement error, it will be randomly distributed, thereby resulting in an underestimate of the temperature-HFMD relationship (Guo et al. 2013). Second, incomplete case ascertainment is likely to have occurred because only symptomatic children presented to the doctor. However, again, the error is likely to have been nondifferential and randomly distributed across the population. Third, we used daily mean temperatures based on prefecture/CJP-specific data, but we projected prefecture/CJP-specific HFMD cases based on province-level associations between temperature and HFMD incidence because the numbers of HFMD cases were too small to estimate reliable values for many locations. Although climatic characteristics, customs, and health policies tend to be similar within provinces, and statistics suggested only low to moderate heterogeneity in associations among locations within each province, estimates based on site-specific associations between temperature and HFMD would be preferable. Fourth, in this study, we assumed that the associations between exposure and outcome would be stationary over time, but they may vary depending on epidemic and nonepidemic periods. However, we could not model the temporal change of the associations because we only have 6 y of data. Further studies are needed to explore this issue when long-term data are available in the future. Fifth, debate remains about the necessity of controlling for residual autocorrelations by including past cases in the time-series regression models for infectious diseases and weather. Some studies argue that it would cause downward bias if past infections were on the causal path of the overall exposure–lag–response association (Barnett et al. 2017; Schisterman et al. 2009). However, other studies suggest that this is a necessary term for modeling, particularly if we consider the impact of weather on disease transmissibility (Imai et al. 2015; Koelle and Pascual 2004; Koelle et al. 2005). In the present study, we thought it was better to control for the autocorrelation. However, further studies are required to clarify this issue more definitively. Finally, the occurrence of El Niño/Southern Oscillation (ENSO) and the North Atlantic Oscillation (NAO) has been regarded as a risk factor for the outbreak of several infectious diseases, particularly in coastline cities (Fisman et al. 2016; Wei et al. 2017). We did not consider their effects because data regarding future ENSO and NAO events were not available, but importantly, the association between temperature and HFMD incidence should be largely independent of ENSO and NAO.
Conclusion
Our study contributes to the limited knowledge of the complex associations between temperature and HFMD in different regions and provinces of China, with two types of exposure–response relationships observed. Projected changes in HFMD incidence as a consequence of changing temperatures due to climate change varied across China. Although future incidence rates will also be influenced by changes in population demographics, our findings suggest that strategies to prevent HFMD should target areas where increasing temperatures are expected to increase the incidence of HFMD, including regions characterized by limited economic development and others with high population inflows.
Supplemental Material
Acknowledgments
We thank all institutes who provided the daily data on meteorological variables and hand, foot, and mouth disease (HFMD) reports. We acknowledge the World Climate Research Programme’s Working Group on Coupled Modeling, which is responsible for Coupled Model Intercomparison Project (CMIP), and we thank the climate modeling groups (listed in Table S1 of this paper) for producing and making available their model output. For CMIP the U.S. Department of Energy’s Program for Climate Model Diagnosis and Intercomparison provides coordinating support and led development of software infrastructure in partnership with the Global Organization for Earth System Science Portals.
The work was supported by grant from the National Mega-Project for the Prevention and Control of Infectious Diseases (No. 2018ZX10713003). Q.Z. was supported by the Monash Graduate Scholarship and the Monash International Postgraduate Research Scholarship. S.L. was supported by the Early Career Fellowship of the Australian National Health and Medical Research Council (NHMRC) (APP1109193) and by seed funding from the NHMRC Centre of Research Excellence–Centre for Air Quality and Health Research and Evaluation (APP1030259). Y.G. was supported by a Career Development Fellowship of the Australian NHMRC (APP1107107).
References
- Ahmad OB, Boschi-Pinto C, Lopez AD, Murray CJ, Lozano R, Inoue M. 2001. Age standardization of rates: A new WHO standard. http://www.who.int/healthinfo/paper31.pdf [accessed 20 May 2017].
- Ashbolt NJ. 2004. Microbial contamination of drinking water and disease outcomes in developing regions. Toxicology 198(1–3):229–238, PMID: 15138046, 10.1016/j.tox.2004.01.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett AG, Stephen D, Huang C, Wolkewitz M. 2017. Time series models of environmental exposures: Good predictions or good understanding. Environ Res 154:222–225, PMID: 28104512, 10.1016/j.envres.2017.01.007. [DOI] [PubMed] [Google Scholar]
- Bo Y-C, Song C, Wang J-F, Li X-W. 2014. Using an autologistic regression model to identify spatial risk factors and spatial risk patterns of hand, foot and mouth disease (HFMD) in Mainland China. BMC Public Health 14:358, PMID: 24731248, 10.1186/1471-2458-14-358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang HL, Chio CP, Su HJ, Liao CM, Lin CY, Shau WY, et al. 2012. The association between enterovirus 71 infections and meteorological parameters in Taiwan. PLoS One 7(10):e46845, PMID: 23071650, 10.1371/journal.pone.0046845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang Q. 2016. The coming of a vaccine for hand, foot, and mouth disease. Guiyang Daily Guizhou Province, China. http://www.sohu.com/a/109042171_398066 [accessed 4 Aug 2017]. [Google Scholar]
- Chen SM, Du JW, Jin YM, Qiu L, Du ZH, Li DD, et al. 2015. Risk factors for severe hand-foot-mouth disease in children in Hainan, China, 2011-2012. Asia Pac J Public Health 27(7):715–722, PMID: 25850695, 10.1177/1010539515579123. [DOI] [PubMed] [Google Scholar]
- China CDC (Chinese Center for Disease Control and Prevention). 2015. Overview of hand, foot, and mouth disease. http://www.chinacdc.cn/jkzt/crb/szkb/zstd/201212/t20121210_72846.htm [accessed 31 Mar 2017].
- China CDC. 2016. Technical guide for inactivated vaccine against enterovirus type 71. http://nip.chinacdc.cn/zxdt/201606/W020160608713368429047.pdf [accessed 12 Aug 2017].
- Fisman DN, Tuite AR, Brown KA. 2016. Impact of El Niño Southern Oscillation on infectious disease hospitalization risk in the United States. Proc Natl Acad Sci USA 113(51):14589–14594, PMID: 27791069, 10.1073/pnas.1604980113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A, Armstrong B, Kenward M. 2012. Multivariate meta-analysis for non-linear and other multi-parameter associations. Stat Med 31(29):3821–3839, PMID: 22807043, 10.1002/sim.5471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A, Armstrong B, Kenward MG. 2010. Distributed lag non-linear models. Stat Med 29(21):2224–2234, PMID: 20812303, 10.1002/sim.3940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A, Armstrong B. 2013. Reducing and meta-analysing estimates from distributed lag non-linear models. BMC Med Res Methodol 13:1, PMID: 23297754, 10.1186/1471-2288-13-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A, Guo Y, Sera F, Vicedo-Cabrera AM, Huber V, Tong S, et al. 2017. Projections of temperature-related excess mortality under climate change scenarios. Lancet Planet Health, PMID: 29276803, 10.1016/S2542-5196(17)30156-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guangdong Government Department of Population and Employment. 2013. The future population perspective in Guangdong. http://www.gdstats.gov.cn/tjzl/tjfx/201311/t20131115_129886.html [accessed 28 Jan 2018].
- Guo C, Yang J, Guo Y, Ou Q-Q, Shen S-Q, Ou C-Q, et al. 2016. Short-term effects of meteorological factors on pediatric hand, foot, and mouth disease in Guangdong, China: a multi-city time-series analysis. BMC Infect Dis 16:524, PMID: 27682137, 10.1186/s12879-016-1846-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Y, Barnett AG, Tong S. 2013. Spatiotemporal model or time series model for assessing city-wide temperature effects on mortality?. Environ Res 120:55–62, PMID: 23026801, 10.1016/j.envres.2012.09.001. [DOI] [PubMed] [Google Scholar]
- Hii YL, Rocklöv J, Ng N. 2011. Short term effects of weather on hand, foot and mouth disease. PLoS One 6(2):e16796, PMID: 21347303, 10.1371/journal.pone.0016796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai C, Armstrong B, Chalabi Z, Mangtani P, Hashizume M. 2015. Time series regression model for infectious disease and weather. Environ Res 142:319–327, PMID: 26188633, 10.1016/j.envres.2015.06.040. [DOI] [PubMed] [Google Scholar]
- Information Office of the State Council of the People’s Republic of China. 2012. White Paper: Medical and Health Services in China. http://english.gov.cn/archive/white_paper/2014/08/23/content_281474982986476.htm/ [accessed 6 Aug 2017]. [Google Scholar]
- IPCC (Intergovernmental Panel on Climate Change). 2014. Climate Change 2014: Mitigation of Climate Change. Contribution of Working Group III to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Edenhofer O, Pichs-Madruga R, Sokona Y, Farahani E, Kadner S, Seyboth K, et al. , eds. Cambridge, UK:Cambridge University Press; http://www.ipcc.ch/report/ar5/wg3/ [accessed 12 May 2017]. [Google Scholar]
- Kendrovski V, Baccini M, Martinez GS, Wolf T, Paunovic E, Menne B. 2017. Quantifying projected heat mortality impacts under 21st-century warming conditions for selected European countries. Int J Environ Res Public Health 14(7):E729, PMID: 28678192, 10.3390/ijerph14070729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kingsley SL, Eliot MN, Gold J, Vanderslice RR, Wellenius GA. 2016. Current and projected heat-related morbidity and mortality in Rhode Island. Environ Health Perspect 124(4):460–467, PMID: 26251954, 10.1289/ehp.1408826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koelle K, Pascual M. 2004. Disentangling extrinsic from intrinsic factors in disease dynamics: A nonlinear time series approach with an application to cholera. Am Nat 163(6):901–913, PMID: 15266387, 10.1086/420798. [DOI] [PubMed] [Google Scholar]
- Koelle K, Rodó X, Pascual M, Yunus M, Mostafa G. 2005. Refractory periods and climate forcing in cholera dynamics. Nature 436(7051):696–700, PMID: 16079845, 10.1038/nature03820. [DOI] [PubMed] [Google Scholar]
- Liu D, Zuo H. 2012. Statistical downscaling of daily climate variables for climate change impact assessment over New South Wales, Australia. Clim Change 115(3–4):629–666, 10.1007/s10584-012-0464-y. [DOI] [Google Scholar]
- Liu Y, Wang X, Liu Y, Sun D, Ding S, Zhang B, et al. 2013. Detecting spatial-temporal clusters of hfmd from 2007 to 2011 in Shandong Province, China. PLoS One 8(5):e63447, PMID: 23704909, 10.1371/journal.pone.0063447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Bureau of Statistics of the People’s Republic of China 2000. China Statistical Yearbook 2000. Beijing, China:China Statistical Press. [Google Scholar]
- National Bureau of Statistics of the People’s Republic of China 2015. China Statistical Yearbook 2015. Beijing, China:China Statistical Press. [Google Scholar]
- National Bureau of Statistics of the People’s Republic of China 2017. China Statistical Yearbook 2017. Beijing, China:China Statistical Press. [Google Scholar]
- National Health and Family Planning Commission of the People’s Republic of China 2015. Standard for managing reporting information of communicable disease.http://www.nhfpc.gov.cn/jkj/s3577/201511/f5d2ab9a5e104481939981c92cb18a54.shtml [accessed 31 Mar 2017].
- National Health and Family Planning Commission of the People’s Republic of China 2017a. Overview of national notifiable disease 2016. http://www.nhfpc.gov.cn/jkj/s3578/201702/38ca5990f8a54ddf9ca6308fec406157.shtml [accessed 31 Mar 2017].
- National Health and Family Planning Commission of the People’s Republic of China 2017b. The first year of universal two-child policy in China. http://www.nhfpc.gov.cn/interview/webcontroller.do?titleSeq=22841&gecstype=1 [accessed 31 Jan 2018].
- Onozuka D, Hashizume M. 2011. The influence of temperature and humidity on the incidence of hand, foot, and mouth disease in Japan. Sci Total Environ 410-411:119–125, PMID: 22014509, 10.1016/j.scitotenv.2011.09.055. [DOI] [PubMed] [Google Scholar]
- Park SK, Park B, Ki M, Kim H, Lee K, Jung C, et al. 2010. Transmission of seasonal outbreak of childhood enteroviral aseptic meningitis and hand-foot-mouth disease. J Korean Med Sci 25(5):677–683, PMID: 20436701, 10.3346/jkms.2010.25.5.677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reclamation 2013. Downscaled CMIP3 and CMIP5 climate and hydrology projections: Release of downscaled CMIP5 climate projections, comparison with preceding information, and summary of user needs. Denver, CO: U.S. Department of the Interior, Bureau of Reclamation, Technical Services Center. [Google Scholar]
- Richardson CW, Wright DA. 1984. “WGEN: A model for generating daily weather variables.” ARS-8. Washington, DC: U.S. Department of Agriculture, Agricultural Research Service. https://www.goldsim.com/Downloads/Library/Models/Applications/Hydrology/WGEN.pdf [accessed 12 May 2017].
- Ruan F, Yang T, Ma H, Jin Y, Song S, Fontaine RE, et al. 2011. Risk factors for hand, foot, and mouth disease and herpangina and the preventive effect of hand-washing. Pediatrics 127(4):e898–e904, PMID: 21422083, 10.1542/peds.2010-1497. [DOI] [PubMed] [Google Scholar]
- Schisterman EF, Cole SR, Platt RW. 2009. Overadjustment bias and unnecessary adjustment in epidemiologic studies. Epidemiology 20(4):488–495, PMID: 19525685, 10.1097/EDE.0b013e3181a819a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian D, Guo Y, Dong W. 2015. Future changes and uncertainties in temperature and precipitation over china based on CMIP5 models. Adv Atmos Sci 32(4):487–496, 10.1007/s00376-014-4102-7. [DOI] [Google Scholar]
- UN DESA (United Nations Department of Economic and Social Affairs)/Population Division. 2017. World population prospects 2017. https://esa.un.org/unpd/wpp/Download/Probabilistic/Population/ [accessed 6 Jan 2018].
- Urashima M, Shindo N, Okabe N. 2003. Seasonal models of herpangina and hand-foot-mouth disease to simulate annual fluctuations in urban warming in Tokyo. Jpn J Infect Dis 56(2):48–53, PMID: 12824684. [PubMed] [Google Scholar]
- Van Vuuren DP, Edmonds J, Kainuma M, Riahi K, Thomson A, Hibbard K, et al. 2011. The representative concentration pathways: an overview. Clim Change 109:5, 10.1007/s10584-011-0148-z. [DOI] [Google Scholar]
- Wei Y, Huang Y, Li X, Ma Y, Tao X, Wu X, et al. 2017. Climate variability, animal reservoir and transmission of scrub typhus in Southern China. PLoS Negl Trop Dis 11(3):e0005447, PMID: 28273079, 10.1371/journal.pntd.0005447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinberger KR, Haykin L, Eliot MN, Schwartz JD, Gasparrini A, Wellenius GA. 2017. Projected temperature-related deaths in ten large U.S. metropolitan areas under different climate change scenarios. Environ Int 107:196–204, PMID: 28750225, 10.1016/j.envint.2017.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO (World Health Organization). 2011. A Guide to Clinical Management and Public Health Response for Hand, Foot and Mouth Disease (HFMD). Manila, Philippines: WHO Regional Office for the Western Pacific; http://www.wpro.who.int/publications/docs/GuidancefortheclinicalmanagementofHFMD.pdf [accessed 10 May 2017]. [Google Scholar]
- WHO. 2012. Hand, foot and mouth disease information sheet. http://www.wpro.who.int/emerging_diseases/hfmd.information.sheet/en/ [accessed 17 Mar 2017].
- Wong S, Yip C, Lau S, Yuen K. 2010. Human enterovirus 71 and hand, foot and mouth disease. Epidemiol Infect 138(8):1071–1089, PMID: 20056019, 10.1017/S0950268809991555. [DOI] [PubMed] [Google Scholar]
- Xiao X, Gasparrini A, Huang J, Liao Q, Liu F, Yin F, et al. 2017. The exposure-response relationship between temperature and childhood hand, foot and mouth disease: a multicity study from mainland China. Environ Int 100:102–109, PMID: 28069250, 10.1016/j.envint.2016.11.021. [DOI] [PubMed] [Google Scholar]
- Xu C. 2017. Spatio-temporal pattern and risk factor analysis of hand, foot and mouth disease associated with under-five morbidity in the Beijing–Tianjin–Hebei region of China. Int J Environ Res Public Health 14(4):E416, PMID: 28406470, 10.3390/ijerph14040416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu M, Yu W, Tong S, Jia L, Liang F, Pan X. 2015. Non-linear association between exposure to ambient temperature and children’s hand-foot-and-mouth disease in Beijing, China. PLoS One 10(5):e0126171, PMID: 26010147, 10.1371/journal.pone.0126171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu X, Zuo H, Rao Y, Zhang L, Wang LL, Zhao Y. 2016. Intention to have a second child among chinese women one year after the implementation of selective two-child policy: A cross-sectional survey. Lancet 388:S96, 10.1016/S0140-6736(16)32023-2. [DOI] [Google Scholar]
- Yeager J, O’Brien R. 1979. Enterovirus inactivation in soil. Appl Environ Microbiol 38(4):694–701, PMID: 44178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin F, Zhang T, Liu L, Lv Q, Li X. 2016. The association between ambient temperature and childhood hand, foot, and mouth disease in Chengdu, China: a distributed lag non-linear analysis. Sci Rep 6:27305, PMID: 27248051, 10.1038/srep27305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng Y, Hesketh T. 2016. The effects of China’s universal two-child policy. Lancet 388(10054):1930–1938, PMID: 27751400, 10.1016/S0140-6736(16)31405-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Zhao Q, Zhang W, Li S, Chen G, Han Z, et al. 2017. Are hospital emergency department visits due to dog bites associated with ambient temperature? A time-series study in Beijing, China. Sci Total Environ 598:71–76, PMID: 28437773, 10.1016/j.scitotenv.2017.04.112. [DOI] [PubMed] [Google Scholar]
- Zhang Z, Xie X, Chen X, Li Y, Lu Y, Mei S, et al. 2016. Short-term effects of meteorological factors on hand, foot and mouth disease among children in Shenzhen, China: non-linearity, threshold and interaction. Sci Total Environ 539:576–582, PMID: 26386448, 10.1016/j.scitotenv.2015.09.027. [DOI] [PubMed] [Google Scholar]
- Zhao Q, Zhang Y, Zhang W, Li S, Chen G, Wu Y, et al. 2017. Ambient temperature and emergency department visits: time-series analysis in 12 Chinese cities. Environ Pollut 224:310–316, PMID: 28222977, 10.1016/j.envpol.2017.02.010. [DOI] [PubMed] [Google Scholar]
- Zhu L, Wang X, Guo Y, Xu J, Xue F, Liu Y. 2016. Assessment of temperature effect on childhood hand, foot and mouth disease incidence (0–5 years) and associated effect modifiers: a 17 cities study in Shandong Province, China, 2007–2012. Sci Total Environ 551-552:452–459, PMID: 26891011, 10.1016/j.scitotenv.2016.01.173. [DOI] [PubMed] [Google Scholar]
- Zhu L, Yuan Z, Wang X, Li J, Wang L, Liu Y, et al. 2015. The impact of ambient temperature on childhood HFMD incidence in inland and coastal area: a two-city study in Shandong Province, China. Int J Environ Res Public Health 12(8):8691–8704, PMID: 26213955, 10.3390/ijerph120808691. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.