Abstract
Objective
Although transfusion guidelines have changed considerably over the past two decades, the adoption of patient blood management programs has not been fully realized across hospitals in the United States.
Patients and Methods
We evaluated trends in red blood cell (RBC), platelet and plasma transfusion at three Veterans Health Administration (VHA) hospitals from 2000 through 2010.
Results
There were 176,521 hospitalizations in 69,621 patients; of these, 13.6% of hospitalizations involved transfusion of blood products (12.7% RBCs, 1.4% platelets, 3.0% plasma). Transfusion occurred in 25.2% of surgical and 5.3% of medical hospitalizations. Transfusion use peaked in 2002 for surgical hospitalizations and declined afterwards (p<0.001). There was no significant change in transfusion use over time (p=0.126) for medical hospitalizations. In hospitalizations that involved transfusions, there was a 20.3% reduction in the proportion of hospitalizations in which ≥3 units of RBCs were given (from 51.7% to 41.1%; p<0.001) and a 73.6% increase when one RBC unit was given (from 8.0% to 13.8%; p<0.001) from 2000–2010. Of the hospitalizations with RBC transfusion, 9.6% involved the use of one unit over the entire study period. The most common principal diagnoses for medical patients receiving transfusion were anemia, malignancy, heart failure, pneumonia and renal failure. Over time, transfusion utilization increased in patients who were admitted for infection (p=0.009).
Conclusion
Blood transfusions in three VHA hospitals have decreased over time for surgical patients but remained the same for medical patients. Further study examining appropriateness of blood products in medical patients appears necessary.
Keywords: transfusion, red blood cells, plasma, platelets, Veterans
INTRODUCTION
Transfusion practices during hospitalization have changed considerably over the past two decades. Guided by evidence from randomized controlled trials, patient blood management programs have been expanded [1]. Such programs include recommendations regarding minimization of blood loss during surgery, prevention and treatment of anemia, strategies for reducing transfusions in both medical and surgical patients, improved blood utilization, education of health professionals, and standardization of blood management-related metrics [2]. Some of the guidelines have been incorporated into the Choosing Wisely initiative of the American Board of Internal Medicine Foundation, including: (a) don’t transfuse more units of blood than absolutely necessary, (b) don’t transfuse red blood cells for iron deficiency without hemodynamic instability, (c) don’t routinely use blood products to reverse warfarin, and (d) don’t perform serial blood counts on clinically stable patients [3]. Although there has been growing interest in blood management, only 37.8% of the 607 AABB (formerly, American Association of Blood Banks) facilities in the United States reported having a patient blood management program in 2013 [2].
While the importance of blood safety is recognized, data regarding the overall trends in practices are conflicting. A study using the Nationwide Inpatient Sample indicated that there was a 5.6% annual mean increase in the transfusion of blood products from 2002 to 2011 in the United States [4]. This contrasts with the experience of Kaiser Permanente in Northern California, in which the incidence of RBC transfusion decreased by 3.2% from 2009 to 2013 [5]. A decline in rates of intraoperative transfusion was also reported among elderly Veterans in the United States from 1997 to 2009 [6].
We conducted a study in hospitalized Veterans with two main objectives: (a) to evaluate trends in utilization of red blood cells (RBC), platelets and plasma over time, and (b) to identify those groups of Veterans who received specific blood products. We were particularly interested in transfusion use in medical patients.
METHODS
Participants were hospitalized Veterans at three Department of Veterans Affairs (VA) medical centers. Data from all hospitalizations were collected from January of 2000 through December of 2010. Blood bank data (including the type and volume of products administered) were available electronically from each hospital. These files were linked to inpatient data, which included ICD-9-CM diagnoses (principal and secondary) and procedures during hospitalization.
Statistical analyses were conducted using generalized linear models to evaluate trends over time. The unit of observation was hospitalization, with categorization by type. Surgical hospitalizations were defined as admissions in which any surgical procedure occurred, whereas medical hospitalizations were defined as admissions without any surgery. Alpha was set at 0.05, 2-tailed. All analyses were conducted in Stata/MP 14.1. The study received human subjects institutional review board approval from the VA Ann Arbor Healthcare System.
RESULTS
From 2000 through 2010, there were 176,521 hospitalizations in 69,621 patients. Within this cohort, 6% were <40 years of age, 66% were 40–69 years of age, and 28% were 70 years or older at the time of admission. In this cohort, 96% of patients were male. Overall, 13.6% of all hospitalizations involved transfusion of a blood product (12.7% RBCs, 1.4% platelets, 3.0% plasma).
Transfusion occurred in 25.2% of surgical hospitalizations and 5.3% in medical hospitalizations. For surgical hospitalizations, transfusion use peaked in 2002 (when 30.9% of the surgical hospitalizations involved a transfusion) and significantly declined afterwards (p<0.001). By 2010, 22.5% of the surgical hospitalizations involved a transfusion. Most of the surgeries where blood products were transfused involved cardiovascular procedures. For medical hospitalizations only, there was no significant change in transfusion use over time, either from 2000 to 2010 (p=0.126) or from 2002 to 2010 (p=0.072). In 2010, 5.2% of the medical hospitalizations involved a transfusion.
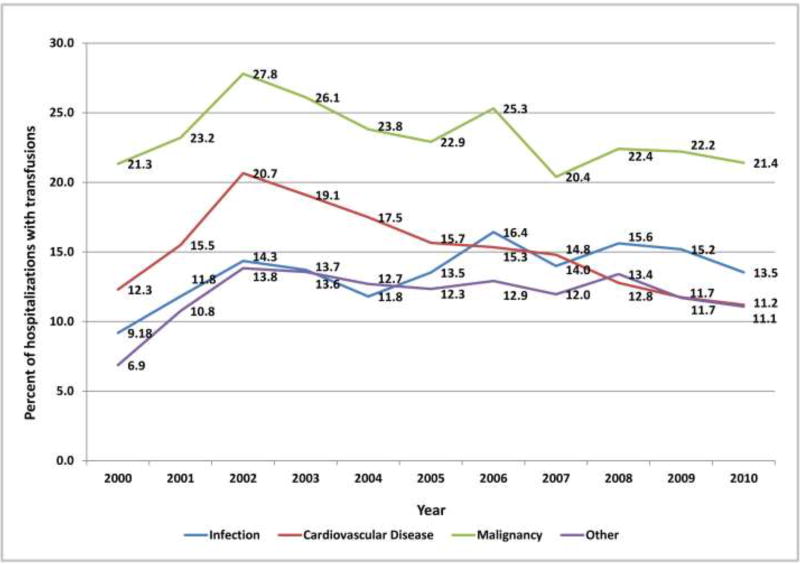
Rates of transfusion varied by principal diagnosis (Figure 1). For patients admitted with a principal diagnosis of infection (n= 20,981 hospitalizations), there was an increase in the percentage of hospitalizations in which transfusions (RBC, platelet, plasma) were administered over time (p=0.009) (Figure 1). For patients admitted with a principal diagnosis of malignancy (n=12,904 hospitalizations), cardiovascular disease (n=40,324 hospitalizations), and other diagnoses (n=102,312 hospitalizations), there were no significant linear trends over the entire study period (p=0.191, p=0.052, p=0.314, respectively). Rather, blood utilization peaked in year 2002 and significantly declined afterwards for patients admitted for malignancy (p<0.001) and for cardiovascular disease (p<0.001).
Figure 1.
Percentage of Hospitalizations with Transfusion, by Principal Diagnosis and Year
The most common principal diagnoses for medical patients receiving any transfusion (RBCs, platelet, plasma) are listed in Table 1. For medical patients with a principal diagnosis of anemia, 88% of hospitalizations involved a transfusion (Table 1). Transfusion occurred in 6–11% of medical hospitalizations with malignancies, heart failure, pneumonia or renal failure (Table 1). A considerable proportion (43%) of medical patients with gastrointestinal hemorrhage received a transfusion.
Table 1.
Transfusion Use for the Most Frequent Principal Diagnoses in Medical Hospitalizations
| Transfusion | No Transfusion | |||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Principal Diagnosis: | Number (%) of Hospitalizations |
LOS, median (IQR) |
In-Hospital Mortality (%) |
Number (%) of Hospitalizations |
LOS, median (IQR) |
In-Hospital Mortality (%) |
| Anemia | 1151 (88%) | 2 (1–3) | 3 (0.3%) | 158 (12%) | 2 (1–3) | 2 (1%) |
| Malignancy/Chemotherapy | 474 (11%) | 5 (3–9) | 49 (10%) | 3789 (89%) | 2 (1–5) | 265 (7%) |
| Heart failure | 298 (6%) | 5 (3–8) | 22 (7%) | 4855 (94%) | 3 (2–5) | 60 (1%) |
| Pneumonia/Influenza | 241 (6%) | 6 (4–9) | 17 (7%) | 3601 (94%) | 3 (2–5) | 107 (3%) |
| Renal failure | 203 (11%) | 5 (3–8) | 13 (6%) | 1650 (89%) | 3 (2–5) | 48 (3%) |
| Gastrointestinal hemorrhage | 187 (43%) | 3 (2–4) | 17 (9%) | 246 (57%) | 2 (1–3) | 9 (4%) |
| Urinary tract infection | 127 (7%) | 6 (3–8) | 4 (3%) | 1713 (93%) | 3 (2–5) | 20 (1%) |
| Chronic obstructive pulmonary disease | 113 (2%) | 5 (3–8) | 3 (3%) | 4626 (98%) | 3 (2–4) | 55 (1%) |
| Acute myocardial infarction | 113 (12%) | 5 (3–8) | 9 (8%) | 812 (88%) | 3 (2–5) | 68 (8%) |
| Respiratory failure | 61 (13%) | 8 (5–14) | 31 (51%) | 393 (87%) | 5 (3–9) | 94 (24%) |
Abbreviations: LOS, length of stay; IQR, interquartile range.
Among blood products, transfusion of RBCs was most common (Table 2). Medical patients received RBCs in 12% (403/3497) of the hospitalizations where the principal diagnosis was malignancy, 4% (814/20,008) of the hospitalizations where the principal diagnosis was cardiovascular disease, 5% (643/12,111) of the hospitalizations where the principal diagnosis was infection, and 5% (3,211/67,104) of the hospitalizations for other principal diagnoses (Table 2). Coronary atherosclerosis was the most common principal diagnosis in patients who received RBCs, followed by hemorrhage of the gastrointestinal tract, anemia, and acute kidney failure (Table 3). In these patients, 90-day mortality (from hospital admission) was 30.9% in patients with a principal diagnosis of pneumonia, 27.3% in those with congestive heart failure and 26.4% in those with acute kidney failure. The most common surgical procedures associated with RBC transfusion were cardiac, excisional debridement, amputation, and hip/knee replacement (Table 3).
TABLE 2.
Number of Hospitalizations with Transfusion, by Principal Diagnosis and Surgery
| RBC | Platelets | Plasma | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| Principal Diagnosis: | Number Transfused |
Number Not Transfused |
Percent Transfused |
Number Transfused |
Number Not Transfused |
Percent Transfused |
Number Transfused |
Number Not Transfused |
Percent Transfused |
|
|
|
|
|||||||
| Cancer | |||||||||
| Cardiac Surgery | 587 | 517 | 53% | 89 | 1015 | 8% | 159 | 945 | 14% |
| Other Surgery | 1706 | 6597 | 21% | 104 | 8199 | 1% | 262 | 8041 | 3% |
| No Surgery | 403 | 3094 | 12% | 40 | 3457 | 1% | 36 | 3461 | 1% |
| Cardiovascular disease | |||||||||
| Cardiac Surgery | 4293 | 10136 | 30% | 1148 | 13281 | 8% | 1480 | 12949 | 10% |
| Other Surgery | 677 | 5210 | 11% | 21 | 5866 | <1% | 136 | 5751 | 2% |
| No Surgery | 814 | 19194 | 4% | 33 | 19975 | <1% | 108 | 19900 | 1% |
| Infection | |||||||||
| Cardiac Surgery | 1270 | 2902 | 30% | 124 | 4048 | 3% | 375 | 3797 | 9% |
| Other Surgery | 707 | 3991 | 15% | 44 | 4654 | 1% | 210 | 4488 | 4% |
| No Surgery | 643 | 11468 | 5% | 33 | 12078 | <1% | 71 | 12040 | 1% |
| Other | |||||||||
| Cardiac Surgery | 2914 | 5284 | 36% | 302 | 7896 | 4% | 888 | 7310 | 11% |
| Other Surgery | 5119 | 21891 | 19% | 253 | 26757 | 1% | 1134 | 25876 | 4% |
| No Surgery | 3211 | 63893 | 5% | 195 | 66909 | <1% | 388 | 66716 | 1% |
Table 3.
Most Frequent Principal Diagnoses and Surgical Procedures in Patients Receiving Red Blood Cells
| Rank | Code | Description | Number of Hospitalizations |
Mortality1 |
|---|---|---|---|---|
| Diagnoses | ||||
| 1 | 414.01 | Coronary atherosclerosis of native coronary artery | 1697 | 4.3% |
|
| ||||
| 2 | 578.9 | Hemorrhage of gastrointestinal tract, unspecified | 633 | 16.4% |
|
| ||||
| 3 | 285.9 | Anemia, unspecified | 530 | 17.4% |
|
| ||||
| 4 | 584.9 | Acute kidney failure, unspecified | 436 | 26.6% |
|
| ||||
| 5 | 428.0 | Congestive heart failure, unspecified | 433 | 27.5% |
|
| ||||
| 6 | 280.9 | Iron deficiency anemia, unspecified | 422 | 8.1% |
|
| ||||
| 7 | 486 | Pneumonia, organism unspecified | 382 | 30.9% |
|
| ||||
| 8 | 410.71 | Subendocardial infarction, initial episode of care | 378 | 19.3% |
|
| ||||
| 9 | 441.4 | Abdominal aneurysm without mention of rupture | 365 | 7.4% |
|
| ||||
| 10 | V57.89 | Care involving other specified rehabilitation procedure | 353 | 5.4% |
|
| ||||
| 11 | 185 | Malignant neoplasm of prostate | 333 | 9.6% |
|
| ||||
| 12 | 424.1 | Aortic valve disorders | 297 | 9.1% |
|
| ||||
| Surgical Procedures | ||||
|
|
||||
| 1 | 3961 | Extracorporeal circulation auxiliary to open heart surgery | 1954 | 6.0% |
|
| ||||
| 2 | 3615 | Single internal mammary-coronary artery bypass | 1648 | 4.6% |
|
| ||||
| 3 | 3612 | (Aorto)coronary bypass of two coronary arteries | 802 | 6.1% |
|
| ||||
| 4 | 3613 | (Aorto)coronary bypass of three coronary arteries | 585 | 4.6% |
|
| ||||
| 5 | 3929 | Other (peripheral) vascular shunt or bypass | 528 | 8.3% |
|
| ||||
| 6 | 8622 | Excisional debridement of wound, infection, or burn | 431 | 10.9% |
|
| ||||
| 7 | 3611 | (Aorto)coronary bypass of one coronary artery | 408 | 4.9% |
|
| ||||
| 8 | 8415 | Other amputation below knee | 345 | 9.6% |
|
| ||||
| 9 | 8151 | Total hip replacement | 343 | 4.4% |
|
| ||||
| 10 | 3925 | Aorta-iliac-femoral bypass | 336 | 5.4% |
|
| ||||
| 11 | 8154 | Total knee replacement | 332 | 1.8% |
|
| ||||
| 12 | 3522 | Other replacement of aortic valve | 324 | 8.0% |
90-day mortality from hospital admission.
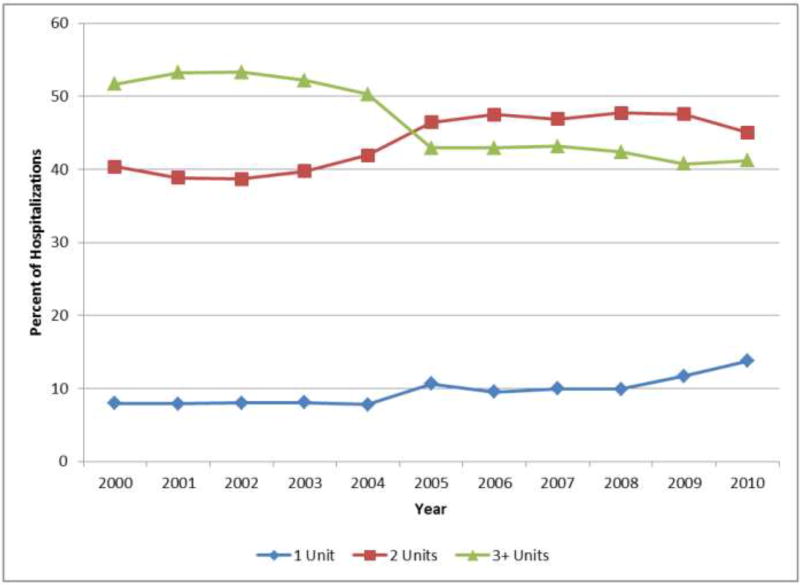
There was variation in the volume of RBCs used over the time period of the study (Figure 2). Of all the hospitalizations in which a RBC transfusion occurred, 9.6% (2,154/22,344) involved the use of only one unit, 43.8% (9,791/22,344) involved two units, and 46.5% (10,399/22,344) involved three or more units during the hospitalization. From 2000 through 2010, there was a 20.3% reduction in the proportion of hospitalizations in which three or more units of RBCs were given (from 51.7% to 41.1%; p<0.001). That is, among those hospitalizations in which a RBC transfusion occurred, a smaller proportion of hospitalizations involved the administration of three or more units of RBCs from 2000 through 2010 (Figure 2). There was an 11.5% increase in the proportion of hospitalizations in which two units of RBCs were used (from 40.4% to 45.0%; p<0.001). In addition, there was a 73.6% increase in the proportion of hospitalizations in which one RBC unit was given (from 8.0% to 13.8%; p=0.001).
Figure 2.
Percentage of Hospitalizations by Number of Red Blood Cell Units and Year
Use of platelets or plasma in hospitalized Veterans was considerably lower than that of RBCs (Table 2). When platelets or plasma were used, it was most frequently for patients who underwent cardiac surgery, regardless of the principal diagnosis. The use of platelets and plasma was low in medical patients (<1% and <1% of hospitalizations, respectively). Overall, the mean platelet volume was 12.5 mL/hospitalization in year 2000, declined to 5.2 mL/hospitalization in 2008, and then rose to 16.8 mL/hospitalization in 2010. For plasma, the mean mL/hospitalization was 28.9 in year 2000, increased to 50.1 mL/hospitalization in year 2008, and declined, thereafter, to 35.1 mL/hospitalization in year 2010.
DISCUSSION
In this population of Veterans who received care at three medical centers in the Midwestern United States, patterns of transfusion utilization over time differed in medical and surgical patients. For surgical patients, transfusion rates decreased from 2002 through 2010; in medical patients, blood usage remained constant. Trends in transfusion utilization varied by the principal diagnosis of the patient. For patients admitted for infection, blood product use significantly increased over time. For patients admitted to the hospital for cardiovascular disease or malignancy, the rate of transfusion decreased from 2002 through 2010.
We also observed secular trends in the volume of RBCs administered. There was an increase in the percentage of hospitalizations in which one or two RBC units were used and a decline in transfusion of three or more units. The reduction in the use of three or more RBC units may reflect the adoption and integration of recommendations in patient blood management by clinicians, which encourage assessment of the patients’ symptoms in determining whether additional units are necessary [7]. Such guidelines also endorse the avoidance of routine administration of two units of RBCs if one unit is sufficient [8]. We have previously shown that, after coronary artery bypass grafting, two RBC units doubled the risk of pneumonia [9]; additional analyses indicated that one or two units of RBCs were associated with increased post-operative morbidity [10]. In addition, our previous research indicated that the probability of infection increased considerably between one and two RBC units, with a more gradual increase beyond two units [11]. With this evidence in mind, some studies at single sites have reported that there was a dramatic decline from two RBC units before initiation of patient blood management programs to one unit after the programs were implemented [12,13].
Chen and colleagues monitored intraoperative RBC utilization from 1997 to 2009 in older Veterans who underwent noncardiac surgery [6]. They found a decline in RBC utilization rates over time, which was accompanied by a significant increase in 30-day adjusted mortality in those with lower preoperative hematocrit values or significant blood loss. They reported no significant variation in transfusion rates and mortality over time in patients in which a transfusion was not indicated (higher hematocrit, little blood loss). In a different study, Rehm and colleagues instituted a program to encourage greater use of appropriate transfusions in a Veterans Affairs teaching hospital [14]. Their mandatory implementation of a transfusion request form led to a 26% decline in the use of RBC units with no increase in mortality. Consistent with our findings, others have found that transfusion is common in specific Veteran populations such as those with chronic kidney disease and anemia in inpatient settings [15].
Medical patients who received a transfusion were often admitted for reason of anemia, cancer, organ failure, or pneumonia. Some researchers are now reporting that blood use, at certain sites, is becoming more common in medical rather than surgical patients, which may be due to an expansion of patient blood management procedures in surgery [16]. There are a substantial number of patient blood management programs among surgical specialties and their adoption has expanded [17]. Although there are fewer patient blood management programs in the non-surgical setting, some have been targeted to internal medicine physicians and specifically, to hospitalists [1,18]. For example, a toolkit from the Society of Hospital Medicine centers on anemia management and includes anemia assessment, treatment, evaluation of RBC transfusion risk, blood conservation, optimization of coagulation, and patient-centered decision-making [19]. Additionally, bundling of patient blood management strategies has been launched to help encourage a wider adoption of such programs [20].
While guidelines regarding use of RBCs are becoming increasingly recognized, recommendations for the use of platelets and plasma are hampered by the paucity of evidence from randomized controlled trials [21,22]. There is moderate-quality evidence for the use of platelets with therapy-induced hypoproliferative thrombocytopenia in hospitalized patients [21], but low quality evidence for other uses. Moreover, a recent review of plasma transfusion in bleeding patients found no randomized controlled trials on plasma use in hospitalized patients although several trials were currently underway [22].
Our findings need to be considered in the context of the following limitations. The data were from three VHA hospitals so the results may not reflect patterns of usage at other hospitals. However, AABB reports that there has been a general decrease in transfusion of allogeneic whole blood and RBC units since 2008 at the AABB-affiliated sites in the United States [2]; this is similar to the pattern that we observed in surgical patients. In addition, we report an overall view of trends without having details regarding which specific factors influenced changes in transfusion during this 11-year period. It is possible that the severity of hospitalized patients may have changed with time which could have influenced decisions regarding the need for transfusion.
In conclusion, the use of blood products decreased in surgical patients since 2002 but remained the same in medical patients in this VHA population. Transfusions increased over time for patients who were admitted to the hospital for reason of infection, but decreased since 2002 for those admitted for cardiovascular disease or cancer. The number of RBC units per hospitalization decreased over time. Additional surveillance is needed to determine whether recent evidence regarding blood management has been incorporated into clinical practice for medical patients, as we strive to deliver optimal care to our Veterans.
Acknowledgments
FUNDING: Department of Veterans Affairs, Clinical Sciences Research & Development Service Merit Review Award (EPID-011-11S). The contents do not represent the views of the U.S. Department of Veterans Affairs or the United States Government.
Footnotes
CONFLICTS OF INTEREST: None.
References
- 1.Hohmuth B, Ozawa S, Ashton M, Melseth RL. Patient-centered blood management. J Hosp Med. 2014;9(1):60–65. doi: 10.1002/jhm.2116. [DOI] [PubMed] [Google Scholar]
- 2.Whitaker B, Rajbhandary S, Harris A. The 2013 AABB blood collection, utilization, and patient blood management survey report. United States Department of Health and Human Services, AABB; 2015. [DOI] [PubMed] [Google Scholar]
- 3.Cassel CK, Guest JA. Choosing wisely: helping physicians and patients make smart decisions about their care. JAMA. 2012;307(17):1801–1802. doi: 10.1001/jama.2012.476. [DOI] [PubMed] [Google Scholar]
- 4.Pathak R, Bhatt VR, Karmacharya P, Aryal MR, Alweis R. Trends in blood-product transfusion among inpatients in the United States from 2002 to 2011: data from the nationwide inpatient sample. J Hosp Med. 2014;9(12):800–801. doi: 10.1002/jhm.2248. [DOI] [PubMed] [Google Scholar]
- 5.Roubinian NH, Escobar GJ, Liu V, et al. Trends in red blood cell transfusion and 30-day mortality among hospitalized patients. Transfusion. 2014;54(10pt2):2678–2686. doi: 10.1111/trf.12825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen A, Trivedi AN, Jiang L, Vezeridis M, Henderson WG, Wu W-C. Hospital blood transfusion patterns during major noncardiac surgery and surgical mortality. Medicine (Baltimore) 2015;94(32):e1342. doi: 10.1097/MD.0000000000001342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carson JL, Guyatt G, Heddle NM, et al. Clinical practice guidelines from the AABB: Red blood cell transfusion thresholds and storage. JAMA. 2016;316(19):2025–2035. doi: 10.1001/jama.2016.9185. [DOI] [PubMed] [Google Scholar]
- 8.Hicks LK, Bering H, Carson KR, et al. The ASH choosing wisely® campaign: five hematologic tests and treatments to question. Blood. 2013;122(24):3879–3883. doi: 10.1182/blood-2013-07-518423. [DOI] [PubMed] [Google Scholar]
- 9.Likosky DS, Paone G, Zhang M, et al. Red blood cell transfusions impact pneumonia rates after coronary artery bypass grafting. Ann Thorac Surg. 2015;100(3):794–801. doi: 10.1016/j.athoracsur.2015.03.089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Paone G, Likosky DS, Brewer R, et al. Transfusion of 1 and 2 units of red blood cells is associated with increased morbidity and mortality. Ann Thorac Surg. 2014;97(1):87–93. doi: 10.1016/j.athoracsur.2013.07.020. discussion 93-4. [DOI] [PubMed] [Google Scholar]
- 11.Rogers MAM, Blumberg N, Heal JM, et al. Role of transfusion in the development of urinary tract–related bloodstream infection. Arch Intern Med. 2011;171(17):1587–1589. doi: 10.1001/archinternmed.2011.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oliver JC, Griffin RL, Hannon T, Marques MB. The success of our patient blood management program depended on an institution-wide change in transfusion practices. Transfusion. 2014;54(10 Pt 2):2617–2624. doi: 10.1111/trf.12536. [DOI] [PubMed] [Google Scholar]
- 13.Yerrabothala S, Desrosiers KP, Szczepiorkowski ZM, Dunbar NM. Significant reduction in red blood cell transfusions in a general hospital after successful implementation of a restrictive transfusion policy supported by prospective computerized order auditing. Transfusion. 2014;54(10 Pt 2):2640–2645. doi: 10.1111/trf.12627. [DOI] [PubMed] [Google Scholar]
- 14.Rehm JP, Otto PS, West WW, et al. Hospital-wide educational program decreases red blood cell transfusions. J Surg Res. 1998;75(2):183–186. doi: 10.1006/jsre.1997.5291. [DOI] [PubMed] [Google Scholar]
- 15.Lawler EV, Bradbury BD, Fonda JR, Gaziano JM, Gagnon DR. Transfusion burden among patients with chronic kidney disease and anemia. Clin J Am Soc Nephrol. 2010;5(4):667–672. doi: 10.2215/CJN.06020809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tinegate H, Pendry K, Murphy M, et al. Where do all the red blood cells (RBCs) go? Results of a survey of RBC use in England and North Wales in 2014. Transfusion. 2016;56(1):139–145. doi: 10.1111/trf.13342. [DOI] [PubMed] [Google Scholar]
- 17.Meybohm P, Herrmann E, Steinbicker AU, et al. Patient blood management is associated with a substantial reduction of red blood cell utilization and safe for patient's outcome: a prospective, multicenter cohort study with a noninferiority design. Ann Surg. 2016;264(2):203–211. doi: 10.1097/SLA.0000000000001747. [DOI] [PubMed] [Google Scholar]
- 18.Corwin HL, Theus JW, Cargile CS, Lang NP. Red blood cell transfusion: impact of an education program and a clinical guideline on transfusion practice. J Hosp Med. 2014;9(12):745–749. doi: 10.1002/jhm.2237. [DOI] [PubMed] [Google Scholar]
- 19.Society of Hospital Medicine. [Accessed, June 9, 2017];Anemia prevention and management program implementation toolkit. Available at: http://www.hospitalmedicine.org/Web/Quality___Innovation/Implementation_Toolkit/Anemia/anemia_overview.aspx.
- 20.Meybohm P, Richards T, Isbister J, et al. Patient blood management bundles to facilitate implementation. Transfus Med Rev. 2017;31(1):62–71. doi: 10.1016/j.tmrv.2016.05.012. [DOI] [PubMed] [Google Scholar]
- 21.Kaufman RM, Djulbegovic B, Gernsheimer T, et al. Platelet transfusion: a clinical practice guideline from the AABB. Ann Intern Med. 2015;162(3):205–213. doi: 10.7326/M14-1589. [DOI] [PubMed] [Google Scholar]
- 22.Levy JH, Grottke O, Fries D, Kozek-Langenecker S. Therapeutic plasma transfusion in bleeding patients: A systematic review. Anesth Analg. 2017;124(4):1268–1276. doi: 10.1213/ANE.0000000000001897. [DOI] [PubMed] [Google Scholar]