Abstract
Hyperdense middle cerebral artery (MCA) is a classic sign of acute thromboembolic disease. Simultaneous bilateral occurrence is uncommon and traditionally attributed to physiological hemoconcentration or attributable to imaging artifact. We present the case of a 71-year-old man whose admission noncontrast computed tomography (CT) demonstrated bilateral hyperdense middle cerebral arteries without other radiographic evidence of acute stroke. CT angiography confirmed bilateral MCA, M1 segment vascular occlusion and follow-up noncontrast CT demonstrated MCA territory infarctions.
Keyword: Bilateral hyperdense middle cerebral arteries
1. Introduction
The advent of computed tomography (CT) in the 1970s revolutionized the evaluation of acute stroke. Initially, clinical utility was limited to evaluation of hemorrhagic etiologies; however, several classic findings are now known to be indicators of acute ischemic stroke: loss of lentiform nucleus or insular ribbon outline, sulcal effacement, and dense middle cerebral artery (MCA) [1], [2].
A unilateral hyperdense MCA is defined as a segment with Hounsfield units (HU) greater than 43 and 1.2 times the contralateral segment. It is considered an insensitive, yet highly specific, indicator of acute ischemic stroke and negative correlate for clinical outcome [2], [3]. Although unilateral pathology correlates well with thromboembolic disease, bilateral pathology is considered, in almost all cases, due to underlying physiological dysfunction or image artifact. This occurs, for physiological dysfunction, with elevated hematocrit, and with image volume averaging artifact, either from vascular calcification or proximate parenchymal hypodensity [2], [4].
To the best of our knowledge, there are only three reported cases in literature of bilateral hyperdense MCAs in acute ischemic stroke [5], [6], [7]. In only one of these cases, is CT angiography (CTA) confirmation of vascular occlusion documented [7]. This report describes a unique case of acute, embolic, bilateral, hyperdense MCA in the setting of poorly managed atrial fibrillation. In this instance, tissue plasminogen activator (t-PA) was contraindicated due to coagulopathy.
2. Presentation of the case
A 71-year-old man with a history of chronic atrial fibrillation, managed with Coumadin, presented following a syncopal event. Physical examination demonstrated Glasgow Coma Scale and National Institute of Health Stroke Scale scores of 3 and 31, respectively. Noncontrast CT demonstrated bilateral increased MCA, M1 segment, density concerning for thromboembolic disease in the setting of an otherwise unremarkable imaging study and laboratory data (Fig. 1). Due to the patient's clinical presentation and abnormal imaging study, a CTA was performed. CTA revealed bilateral MCA, M1 segment, hypodensity without distal contrast flow consistent with acute thromboembolism (Fig. 2). Intubation was performed for airway protection and the patient transferred to a medical intensive care unit for further management. The subsequent day, ventilator spontaneous breathing trials were unsuccessful and a follow-up noncontrast CT demonstrated classical MCA territory infarctions (Fig. 3) with diffuse cerebral edema. The patient consequently died from brainstem herniation.
Fig. 1.
Bilateral hyperdense middle cerebral arteries on initial presentation. Axial non–contrast 5 mm computed tomography image of the head. Bilateral increased middle cerebral artery M1 segment density, measuring 55 HU, is noted.
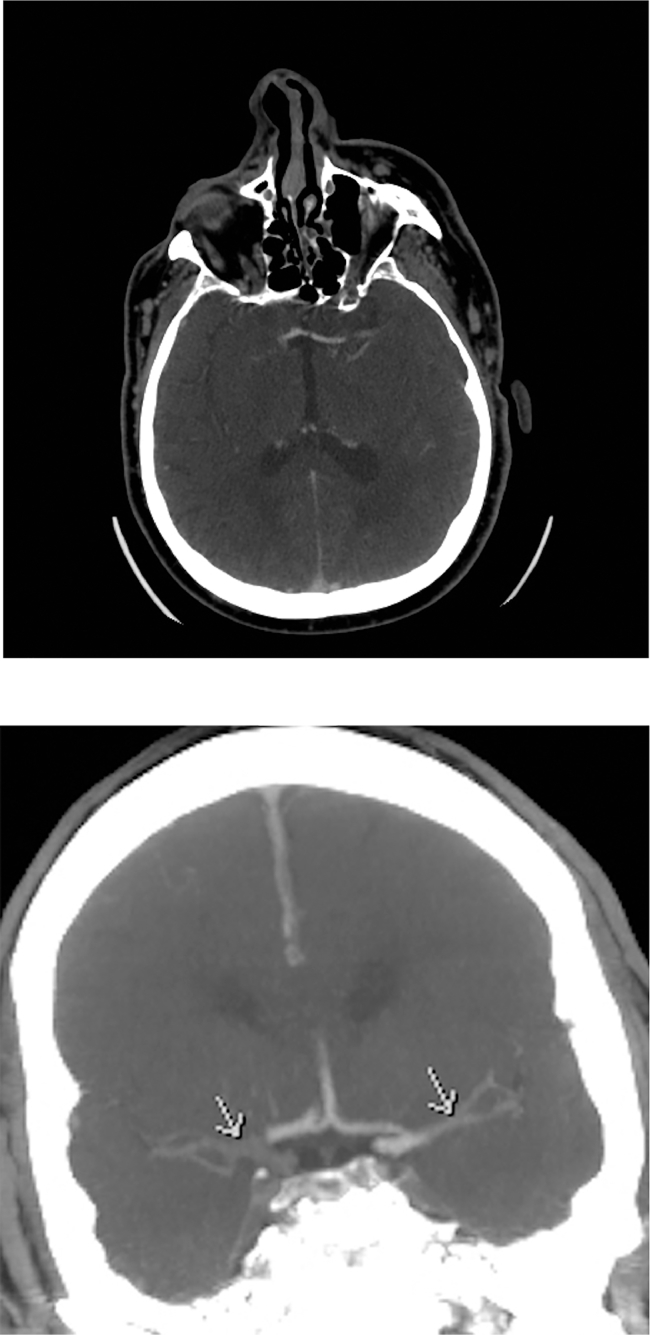
Fig. 2.
Bilateral middle cerebral artery M1 segment occlusion. Axial (A) and coronal (B) computed tomography angiography images of the head show hypodensities (arrows) in bilateral M1 segments with lack of distal contrast flow, indicative of complete occlusion.
Fig. 3.
Bilateral middle cerebral artery territory infarcts. Axial non–contrast 5 mm image of the head. Cerebral edema in the frontal, parietal, temporal lobes, and midbrain.
3. Discussion
Stroke is a major cause of morbidity and the third leading cause of mortality in Western culture. Despite the advent of CT in the 1970s and improved recognition of acute ischemic stroke, the traditional outcome maxim of one thirds; distributed amongst full recovery, significant morbidity and mortality, persisted [8]. It was not until development of t-PA in the 1990s that an intervention existed to improve outcome. The inaugural study demonstrated a near 30% increase in the full recovery cohort compared to placebo [9].
On CT, physiological vascular flow corresponds to a density of 40 HU [10]. Several reported conditions can mimic both unilateral and bilateral thromboembolic disease. Partial volume averaging artifact is a result of the discrepancy between standard CT slice thickness, 5 mm, and MCA cross-sectional diameter, 2-3 mm. This allows averaging from an adjacent atherosclerotic calcification, parenchymal hypodensity, or the skull base to create an apparent intraluminal hyperdensity in the adjacent intracranial vessel. Physiological conditions altering the hematocrit concentration, including polycythemia and dehydration for example, may mimic thrombosis due to the linear relationship between hematocrit concentration and attenuation value on CT [11]. In these instances, homogeneity of physiological milieu and partial volume averaging artifact from the skull base, result in the contralateral vessel exhibiting equivalent artifact [2].
The aforementioned artifacts make the diagnosis of bilateral hyperdense vessels a significant challenge. Despite this, recognition of bilateral hyperdense MCAs as an unusual cause of stroke may avoid delay of care and allow for appropriate thromboembolic therapy. In this case, bilateral MCA hyperdensity, compared to the basilar artery, raised suspicion for pathology. Treatment of bilateral hyperdense MCAs, however, was not undertaken due to the patient's coagulopathy acting as an absolute contraindication to t-PA.
Delayed recognition of bilateral thromboembolic disease is commonly described in the few published reports of bilateral hyperdense MCAs [5], [6], [7], however no outcome data exists due to the paucity of reported cases. The outcome of a stroke patient with a unilateral hyperdense vessel, however, has been well established and is an ominous sign. It has consistently been demonstrated to predict a larger stroke volume, greater degree of neurologic deficit, and mortality [12]. As outcomes are so poor, early recognition is critical to initiating aggressive thrombolytic and neurointerventional therapy.
References
- 1.Gerber C.S. Stroke: historical perspectives. Crit Care Nurs Q. 2003;26(4):268–275. doi: 10.1097/00002727-200310000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Radhiana H., Syazarina S.O., Shahizon Azura M.M., Hilwati H., Sobri M.A. Non-contrast computed tomography in acute ischaemic stroke: a pictorial review. Med J Malays. 2013;68(1):93–100. [PubMed] [Google Scholar]
- 3.Leary M.C., Kidwell C.S., Villablanca J.P., Starkman S., Jahan R., Duckwiler G.R. Validation of computed tomographic middle cerebral artery "dot" sign: an angiographic correlation study. Stroke. 2003;34(11):2636–2640. doi: 10.1161/01.STR.0000092123.00938.83. [DOI] [PubMed] [Google Scholar]
- 4.Beauchamp N.J., Barker P.B., Wang P.Y., van Zijl P.C.M. Imaging of acute cerebral ischemia. Radiology. 1999;212:307–324. doi: 10.1148/radiology.212.2.r99au16307. [DOI] [PubMed] [Google Scholar]
- 5.Kuo S.H., El-Hakam L.M. Bilateral, hyperdense middle cerebral arteries predict bihemispheric stroke. Pediatr Neurol. 2008;39(5):361–362. doi: 10.1016/j.pediatrneurol.2008.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lin C.C., Hu S.Y., Tsan Y.T. Bilateral hyperdense middle cerebral artery sign. J Emerg Crit Care Med. 2009;20(10):53–54. [Google Scholar]
- 7.Gadda D. A case of bilateral dense middle cerebral arteries with CT angiographic confirmation of vascular occlusion. Emerg Radiol. 2003;10(3):142–143. doi: 10.1007/s10140-003-0299-y. [DOI] [PubMed] [Google Scholar]
- 8.Ingall T. Stroke-incidence, mortality, morbidity and risk. J Insur Med. 2004;36(2):143–152. [PubMed] [Google Scholar]
- 9.The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med. 1995;333:1581–1587. doi: 10.1056/NEJM199512143332401. [DOI] [PubMed] [Google Scholar]
- 10.New P.F.J., Aronow S. Attenuation measurements of whole blood and fractions in computed tomography. Radiology. 1976;121:635–640. doi: 10.1148/121.3.635. [DOI] [PubMed] [Google Scholar]
- 11.Grossman C.B. 2nd ed. Williams and Wilkins; Baltimore: 1996. Magnetic resonance imaging and computed tomography of the head and spine; pp. 277–280. [Google Scholar]
- 12.Abul-Kasim K., Brizzi M., Petersson J. Hyperdense middle cerebral artery sign is an ominous prognostic marker despite optimal workflow. Acta Neurol Scand. 2010;122:132–139. doi: 10.1111/j.1600-0404.2009.01277.x. [DOI] [PubMed] [Google Scholar]