Abstract
Lipomas of the gastrointestinal tract are uncommon benign tumors of mature adipocytes and may occur in any portion along the gut. Depending on location they may have a variety of clinical presentations and even simulate malignant neoplasms. We report a case of a 58-year-old woman who presented with acute pelvic pain. An emergency sonogram detected a hyperechogenic mass in the left adnexal region, with no vascularization on Doppler. A computed tomography confirmed the hypothesis of a fat containing tumor with signals of torsion. The patient underwent laparoscopy which depicted a mass over the antimesenteric side of the sigmoid with signs of ischemia and twisted vascular pedicle. The lesion was resected, and the microscopy confirmed the diagnosis of lipoma. The multidisciplinary team in the emergency room must be aware of these possible complications in order to optimize patient care.
Keywords: Lipoma, Acute abdomen, Ischemia, Computed tomography
Introduction
Lipomas of the gastrointestinal tract (GIT) are uncommon benign tumors of mature adipocytes and may occur in any portion along the gut. The incidence of gastrointestinal lipomas varies; however, due to imaging and endoscopic examination, more cases are being detected [1]. Despite being a benign tumor, it has potential complications which are rare and related to morphology and location, including intussusception, ulceration, intestinal obstruction, and abdominal pain [1].
The majority of lipomas of GIT are solitary, submucosal, small, and located in the right colon [1]. Lipomas of mesentery, mesocolon, and antimesenteric side of intestine are extremely rare, they may reach larger dimensions and their incidence are limited to case reports. Torsion of an intra-abdominal lipoma is a rare cause of acute abdomen and most of them were described within the mesentery or omentum. The objectives of this study are to describe a case of torsion of a giant antimesenteric lipoma and to review the current literature.
Case report
A 58-year-old woman was admitted in the emergency room with acute pelvic pain that started 1 day before her admission. The patient had pelvic pain with rebound tenderness and the pain was described as worse when walking. She had been treated for breast cancer 8 years before with no evidence of disease and was in use of an aromatase inhibitor (exemestane). On physical examination, she had a blood pressure of 110/57 mmHg, a pulse rate of 104 beats per minute, a respiratory rate of 16 breaths per minute, oral temperature of 36.2 °C, and oxygen saturation of 98%. Physical examination was otherwise normal, and the laboratory tests were normal.
Transvaginal ultrasound was requested to further study the pelvic organs and it demonstrated a rounded hyperechogenic mass in the left adnexal region, displacing the ovary anteriorly, measuring 7.5 cm and with no vascularization on color Doppler (Fig. 1). A contrast-enhanced computed tomography (CT) of the abdomen and pelvis was subsequently requested to further evaluate the mass. CT showed a large fat-containing mass measuring 7.5 cm next to the sigmoid colon surrounded by fat stranding (Fig. 2A and B). Abdominal CT did not demonstrate any other relevant abnormality. CT performed 7 years before the admission were retrieved from our digital archive and the comparison demonstrated that the lesion increased in size, changed its orientation within the pelvis and appeared a thick capsule surrounding the lesion and internal septations (Fig. 2C). Considering the acute onset of pain and the imaging features, the most likely diagnosis suggested by radiologists was torsion of lipoma from sigmoid or, less likely, torsion of a fat-containing left ovarian mass.
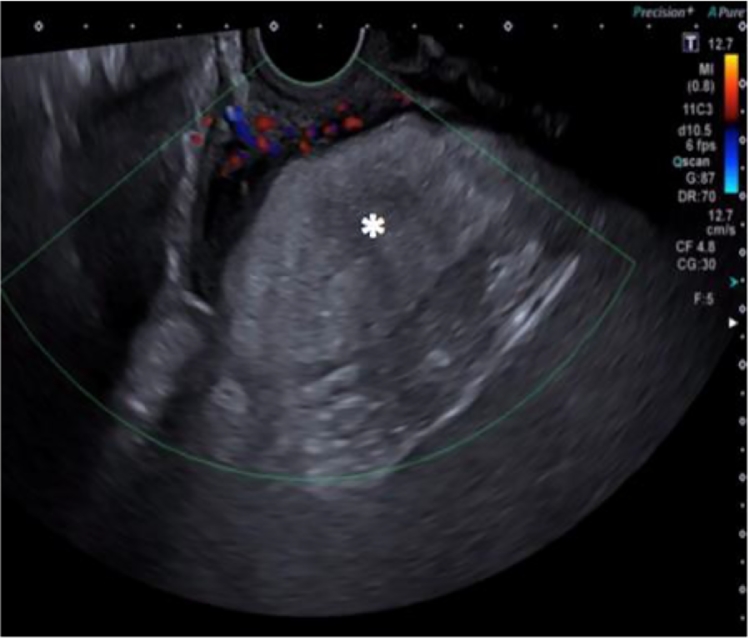
Fig. 1.
Transvaginal ultrasound: demonstrated a rounded hyperechogenic mass in the left adnexal region (asterisk).
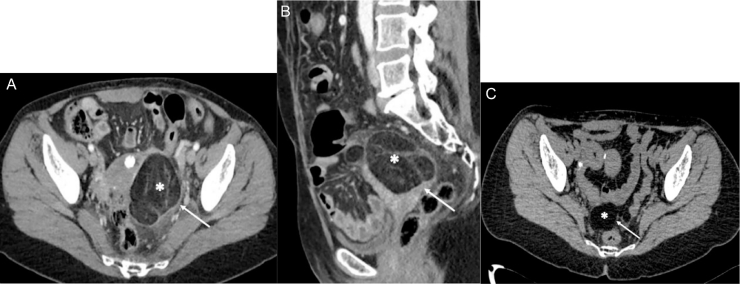
Fig. 2.
A and B. Contrast-enhanced CT of the abdomen and pelvis: showed a large fat-containing mass next to the sigmoid colon (asterisk) surrounded by fat stranding (arrow). C. Contrast-enhanced CT of the abdomen and pelvis: performed 7 years before the admission were retrieved from our digital archive and the comparison demonstrated that the lesion (asterisk) was smaller and located medial and posterior within the pelvis; and there was no fat stranding (arrow).
The patient underwent laparoscopy which depicted a nodular mass over the antimesenteric side of the sigmoid with signs of ischemia and twisted vascular pedicle (Fig. 3). The lesion was resected, and the microscopy confirmed the diagnosis of lipoma and showed areas of hemorrhage, vascular congestion and inflammatory infiltrate, suggestive of lipoma infarction (Fig. 4).
Fig. 3.
Intraoperative photograph: nodular mass (asterisks) over the antimesenteric side of the sigmoid with signs of ischemia.
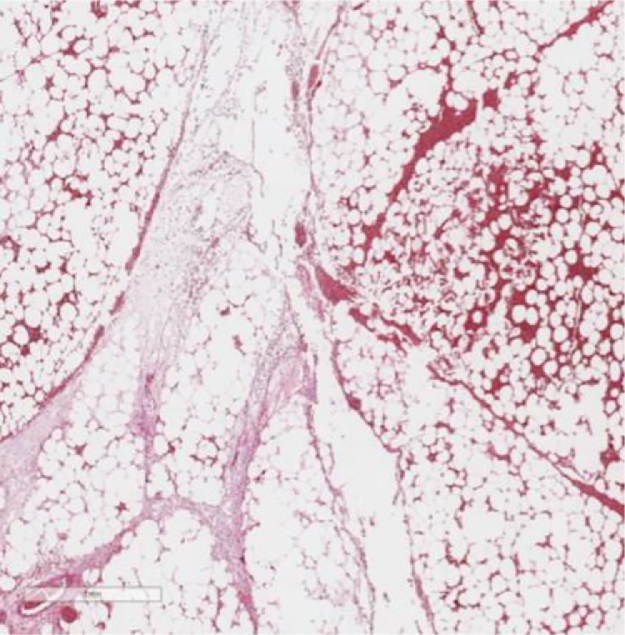
Fig. 4.
Microscopy evaluation: confirmed the diagnosis of lipoma and showed areas of hemorrhage, vascular congestion and inflammatory infiltrate, suggestive of infarction.
Discussion
Complications of lipomas of GIT are rare and related to morphology and location. If submucosal, they may be a leading point of an intussusception or may develop an ulceration and cause intestinal bleeding and/or iron deficiency anemia. If subserosal or located in the mesentery and mesocolon they can cause intestinal obstruction and abdominal pain [2]. With regard to antimesenteric lipomas of the intestine, we have found only one case in literature within the ileum [3]. There are few cases in the literature of torsion of GIT lipoma, most of them originating from mesentery or omentum. Herein, we report a rare case of torsion of an antimesenteric lipoma of the sigmoid. To our knowledge, such case has not been reported previously.
Locations of mesenteric lipomas include the mesentery, surrounding the jejunum and ileum, the mesocolon surrounding the colon, and in women, the peritoneum contained by the broad ligament. Lipomas generally are slow-growing fat-containing masses, with regular margin, which do not penetrate into surrounding organs [4]. Mesenteric lipomas have an equal incidence for both gender [4] and there is an increased incidence reported in adults with obesity, diabetes mellitus, hypercholesterolemia, trauma, radiation, family history, and certain chromosomal abnormalities [5].
Mesenteric lipomas are usually asymptomatic, but larger lipomas can twist around their vascular pedicle, leading to ischemia and infarction. In case of torsion, patient refers an acute onset of pain and imaging may show inflammatory changes, such as edema and fat stranding [6]. There are 4 cases of mesenteric lipomas complicated with torsion described in the literature [3], [5], [6], [7]. Table 1 summarizes those case reports. In the literature, all cases occurred in men, the mean age was 38.5 years (range, 6-9), 2 lipomas were located within the mesentery of ileum, 1 in the antimesenteric border of ileum and 1 in the transverse mesocolon, the mean size was 11.8 cm (range, 8.3-15.0 cm) and all of them were treated with surgical resection.
Table 1.
Summary of cases of torsion of lipoma in the mesentery or mesocolon described in the literature.
| Author, Year | Gender | Age (years) | Location | Size on largest axis (cm) | Treatment |
|---|---|---|---|---|---|
| Yang et al., 2017 | Male | 67 | Antimesenteric border of the ileum | 12.0 | Surgical resection of the ileum and tumor mass |
| Watt et al., 2015 | Male | 72 | Mesentery of the ileum | Not described | Surgical resection of 30 cm of small bowel and ileostomy* |
| Laguna et al., 2014 | Male | 6 | Transverse mesocolon | 8.3 | Surgical resection of the lesion |
| Wolko et al., 2003 | Male | 9 | Mesentery of ileum | 15.0 | Surgical resection of the lesion |
This patient also had intestinal perforation.
The main differential diagnosis of fat-containing mass of the GIT are liposarcoma and teratoma. The differentiation between lipoma and malignant fat-containing tumors can be challenging and, eventually, the histopathological correlation is needed [6]. Increase in size and development of new enhancing septations and a thickened capsule may suggest liposarcoma; however, in a patient with acute clinical presentation these changes may be due to torsion, as demonstrated in our case. Furthermore, change in lesion orientation and presence of adjacent inflammatory changes on CT favor the hypothesis of torsion.
Lipomas of the GIT are benign lesions; however, they may present complications that can result in acute abdomen, including torsion. The multidisciplinary team in the emergency room must be aware of these possible complications in order to optimize patient care.
Footnotes
Declarations of Interest: None.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.radcr.2018.06.011.
Appendix. Supplementary materials
References
- 1.Yaman I, Derici H, Demirpolat G. Giant colon lipoma. Turkish J Surg [Internet] 2015;31(2):102–104. doi: 10.5152/UCD.2013.15. http://www.ulusalcerrahidergisi.org/eng/abstract/1310/eng Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vagholkar K, Bendre M. Lipomas of the colon: a surgical challenge. Int J Clin Med. 2014;5:309–313. [Google Scholar]
- 3.Yang TW, Tsuei YW, Kao CC, Kuo WH, Chen YL, Lin YY. Torsion of a giant antimesenteric lipoma of the ileum: a rare cause of acute abdominal pain. Am J Case Rep. 2017;18:589–592. doi: 10.12659/AJCR.903574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cha JM, Lee JI, Joo KR, Choe JW, Jung SW, Shin HP. Giant mesenteric lipoma as an unusual cause of abdominal pain: a case report and a review of the literature. J Korean Med Sci [Internet] 2009;24(2):333–336. doi: 10.3346/jkms.2009.24.2.333. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=19399281 Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wolko JD, Rosenfeld DL, Lazar MJ, Underberg-Davis SJ. Torsion of a giant mesenteric lipoma. Pediatr Radiol. 2003;33(1):34–36. doi: 10.1007/s00247-002-0810-8. [DOI] [PubMed] [Google Scholar]
- 6.Laguna BA, Iyer RS, Rudzinski ER, Roybal JL, Stanescu AL. Torsion of a giant mesocolic lipoma in a child with Bannayan-Riley-Ruvalcaba syndrome. Pediatr Radiol. 2015;45(3):449–452. doi: 10.1007/s00247-014-3083-0. [DOI] [PubMed] [Google Scholar]
- 7.Watt DG, Sanjay P, Walsh S V, Young JA, Alijani A. Mesenteric lipoma causing small bowel perforation: a case report and review of literature. Scott Med J [Internet] 2012;57(4):247. doi: 10.1258/smj.2012.012109. http://www.ncbi.nlm.nih.gov/pubmed/23002156 Available from: [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.