Abstract
Introduction
High healthcare costs make illness precarious for both patients and their families’ economic situation. Despite the recent focus on the interconnection between health and financial risk at the systemic level, the ethical conflict between concerns for potential health benefits and financial risk protection at the household level in a low-income setting is less understood.
Methods
Using a seven-step ethical analysis, we examine a real-life dilemma faced by families and health workers at the micro level in Ethiopia and analyse the acceptability of limiting treatment for an ill newborn to protect against financial risk. We assess available evidence and ethical issues at stake and discuss the dilemma with respect to three priority setting criteria: health maximisation, priority to the worse-off and financial risk protection.
Results
Giving priority to health maximisation and extra priority to the worse-off suggests, in this particular case, that limiting treatment is not acceptable even if the total well-being gain from reduced financial risk is taken into account. Our conclusion depends on the facts of the case and the relative weight assigned to these criteria. However, there are problematic aspects with the premise of this dilemma. The most affected parties—the newborn, family members and health worker—cannot make free choices about whether to limit treatment or not, and we thereby accept deprivations of people’s substantive freedoms.
Conclusion
In settings where healthcare is financed largely out-of-pocket, families and health workers face tragic trade-offs. As countries move towards universal health coverage, financial risk protection for high-priority services is necessary to promote fairness, improve health and reduce poverty.
Keywords: family, resource allocation, neonatology, distributive justice, decision-making
Introduction
Worldwide, neonatal mortality is decreasing, but still 2.6 million newborns die annually within their first month of life.1 Contributing to 8% of disability-adjusted life years (DALYs) lost globally every year, this largely avoidable burden mainly affect babies in low-income and middle-income countries.1 Seventy-one per cent of newborn deaths, mostly caused by prematurity, intrapartum complications and sepsis,1 could be prevented or treated with effective interventions.2 From a global perspective, one can argue that ill newborns are worse-off for different reasons. They have large and urgent immediate health needs and will suffer from the largest individual lifetime health loss if they die prematurely. Among ill newborns, some are worse-off than others, as there are inequalities in use of services across socioeconomic groups (figure 1), rural/urban location and gender.3
Figure 1.
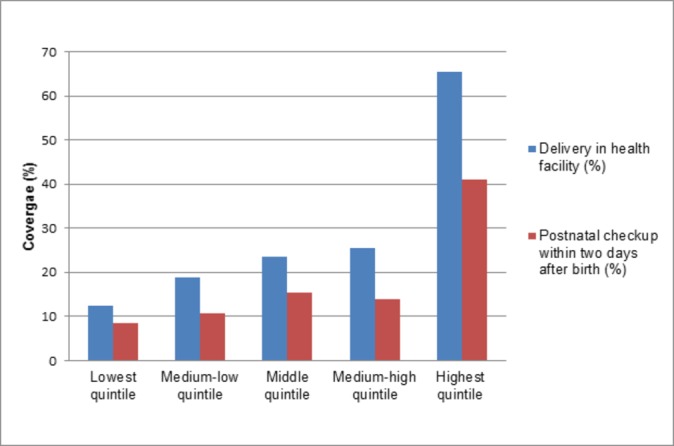
Coverage of newborn healthcare services per wealth quintile. Data source: Ethiopia Demographic and Health Survey 2016.18
Limited healthcare budgets challenge current initiatives to secure access to healthcare services for all neonates. In particular, in low-income countries, where public spending on health often is low,4 discussions about healthcare priority setting and newborn health become important.
Fairness in priority setting
In general, several criteria have been suggested to support the fair allocation of scarce resources. While there is disagreement on how to balance these, two principles form the basis for much of the discussion.5 The greater benefit principle can be understood as giving priority to interventions with greater health benefits. The worse-off principle is concerned with giving priority to those who are worse-off initially. These principles are often applied with a focus on direct health benefits, but some claim we should consider indirect or non-health benefits and burdens as well.6
The high economic burden of healthcare expenses makes it relevant to consider financial risk protection in priority setting at macro and meso levels.3 In health systems that largely depend on out-of-pocket (OOP) payments, healthcare costs put patients and their families at risk of poor health outcomes and impoverishment.3 Globally, 21% of total health expenditures are paid OOP, increasing up to 50% in low-income countries.7 As a part of the United Nations Sustainable Development Goals, all 193 member states have committed to achieving universal health coverage (UHC), which includes protection against financial risk when using healthcare services.8 As countries move towards achieving this goal, they will face priority setting dilemmas. The WHO framework, Making fair choices on the path to universal health coverage, suggests three substantive criteria to guide policy-makers in defining priority services.3 The health maximisation criterion gives priority to cost-effective interventions. The priority to the worse-off criterion prioritises interventions that benefit individuals or groups that are worse-off.i The financial risk protection criterion prefers interventions that protect against high OOP expenses. The criteria may all point in one direction, or concerns may conflict. If so, the WHO framework suggests that concerns should be carefully balanced. Decision-makers may disagree on how to evaluate lives saved versus poverty cases averted.3 Further, while priority setting discussions often focus on trade-offs at the policy and macro level,3 few have analysed diverging concerns for financial risk protection and health benefits at the micro level.9
Financial risk protection at the micro level
In previous studies of families’ and healthcare workers’ ethical dilemmas in Ethiopia, we found that concerns about financial risk protection were central in micro-level healthcare decision-making. In a setting without UHC, families with ill newborns struggled to pay OOP for healthcare; they had to borrow and sell their assets. Facing high costs, families and health workers made decisions that required balancing the needs of ill newborns versus other household needs. Families’ opportunities to seek care, obtain services and follow medical advice depended on their social and economic assets.10 11 Some families had no option but to delay care-seeking, which had tragic consequences. One father explained, “Since I didn’t have enough money, she died before I took her there (referral hospital).”10 When living on the margin, the families’ worry did not only concern the ill newborn but impacted the whole family. One mother was concerned about the future of her other children. “I had nothing, and I sold the only sheep I had to get treatment for my child. When the sheep is not there, what will I do in the future?”10
In an Ethiopian survey, 83% of physicians regularly withheld recommended treatment because patients could not afford services. They often protected patients against high costs by limiting prescription of drugs or diagnostics and compromised by offering suboptimal care.12 In their daily practice, physicians often had to choose between two evils, either poorer health outcomes for the patient or harmful economic consequences for the family.9
As these studies describe, families’ and health workers’ decisions on care-seeking often involve choices between diverging concerns for individual health and family welfare. Whereas priority setting trade-offs at macro level fortunately have received academic and policy attention,3 we find that there is a need to further scrutinise the common dilemma between financial risk and health benefits at micro level. By analysing a stylised case (box 1), our aim is to outline ethical concerns and normative implications of limiting treatment for an ill newborn to protect against financial risk. The micro-level dilemma in box 1 is discussed with reference to criteria for priority setting proposed in the WHO framework (health maximisation, priority to the worse-off, financial risk protection).3 Though this framework was developed for priority setting by policy-makers and technical advisors, we could not identify any other systematic framework that explicitly considers financial risk, which we found to be at the centre of families’ and health workers’ everyday dilemmas.9–11
Box 1. An ill newborn in a poor family in rural Ethiopia.
A mother and father have brought their 2-day-old newborn to a health centre in rural Ethiopia. Two days after a difficult 24-hour birth at home, the baby has still not taken breast. The health worker recognises that the newborn is in respiratory distress and suspects neonatal sepsis. From a medical perspective, the condition is severe, and the baby should be referred to the hospital, as the health centre does not offer intravenous treatment with antibiotics and supportive treatment. The father, who is a daily labourer, is in distress about the expenses for drugs and the hospital stay. He states, “How can we afford? We used everything we had and have no money. If I sell our seeds to pay for treatment, how will I get food for her brothers and sister? Can they go to school? Now, they will suffer”. The health worker is afraid the baby will not be taken to the hospital and may die. She asks herself, “Should I try to convince them to go? Will I force them into economic disaster? How should I negotiate?”
It should be noted that our discussion is grounded in the specific case from rural Ethiopia (box 1). We do not aim to provide a general conclusion on the inherent trade-off between health and welfare, which occurs in different settings and at multiple levels.
Methods
Drawing on earlier empirical work on micro-level priority setting in Ethiopia, we present an anonymised and stylised case in box 1.9–12 The micro-level dilemma was analysed using a modified version of Kymlica’s ethical case analysis as described by Miljeteig et al.13 In a seven-step analysis, we assess available evidence, clarify options for concerned parties, identify conflicts between interests and ethical principles, and suggest acceptable solutions (box 2). The analytic tool cannot offer guidance for how to reconcile competing interests of stakeholders involved or conclude on how to balance conflicting values and ethical principles. However, it is used to structure relevant information and ethical concerns at stake in the dilemma. This systematic approach supports a discussion on what matters most, the acceptability of the trade-off, and what are potential legitimate solutions.
Box 2. Seven-step ethical analysis13 .
Gather information. If insufficient, ask for more.
Step I: What is the ethical dilemma and alternative actions?
Step II: What do we know about the outcomes of alternatives?
Step III: What laws, rules or guidelines regulate the decision?
Step IV: Who are the involved stakeholders?
Step V: What are the stakeholders’ potential burdens and benefits?
Step VI: What interests are in conflict?
Step VII: What are the values and principles at stake?
Discuss what is most important in the case; clarify trade-offs and suggest acceptable solutions.
Ethical analysis
What is the ethical dilemma and alternative actions?
Is it ethically acceptable to limit treatmentii for the ill newborn, in this case to protect the family against financial risk? Alternative responses are yes, it is acceptable, or no, it is not acceptable.
What do we know about the outcomes of alternatives?
We evaluated evidence on the possible outcomes of both alternatives (limiting treatment for the newborn or not) and looked at health outcomes, costs and financial burden with and without treatment (table 1).
Table 1.
Potential outcomes of alternative actions
| Option I: Limit treatment to provide protection against financial risk | Option II: Provide treatment, which contributes to financial risk | |
| Medical prognosis of newborn* | ||
| Case fatality rate | 0.50 | 0.1 |
| Life expectancy | <1 month | <<65 years |
| Costs of treatment for family | ||
| Cost of treatment | ≈0 | US$64 (absolute) US$175 (PPP adjusted) (Additional costs for newborn with sequel) |
| Financial risk | ||
| Impact on available resources† | ≈0 | 3 months of spending (Additional impacts of spending on newborn with sequel) |
*Assuming that the newborn with severe neonatal sepsis has low chances without treatment.
†Assuming that the family lives below the poverty line (below US$1.90/day, 2011 PPP).
PPP, purchasing power parity.
Health outcomes
The burden of neonatal sepsis and infections contributes to 0.1%, and 2.9% of DALYs lost in high-income and low-income countries, respectively. In Ethiopia, neonatal sepsis and infections account for 3.1% of DALYs lost and 14 600 deaths annually.1
WHO guidelines for neonatal sepsis recommend antibiotic treatment (ampicillin and gentamicin).14 When skilled attendance is 0% and 100%, the case fatality rate is predicted to be 30% and 10%, respectively.15 In the ethical dilemma analysed, the health worker identified the ill newborn in need of inpatient care, and we conservatively assume the case fatality rate without treatment to be more than 50%.16 A Delphi consultation indicated that hospital-based management, including intravenous antibiotics and supportive care, could reduce sepsis-specific and pneumonia-specific mortality by 80% and 90%, respectively.15
Average life expectancy at birth in Ethiopia is 65 years.1 Even if the newborn survives from sepsis, a systematic review found that 49% of septic premature neonates developed long-term sequels.17 Though less is known about subsequent effects of sepsis in term babies, it is likely that some encounter physical, neurological and cognitive impairment.16 17 Thus, in this case, we assume that also if the newborn survives septicaemia, she is at increased risk of morbidity, increased health and welfare support, and lower life expectancy (<<65 yearsiii).
Being poor relate to poorer health outcomes, lower care-seeking and relatively higher burden of high healthcare costs.18 If the family falls into poverty due to high OOP expenses after paying for advanced treatment, household members may be of risk of worse health in the future. Current choices about healthcare-seeking hereby influence the future health (as well as welfare, see next paragraph) of the newborn and the family.
Costs
A facility-based study from Ethiopia found that the mean OOP cost of admission for severe pneumonia was US$64 per inpatient visit (0–59 months).19 While the relative burden of these costs may differ between poor and less well-off families, we—for simplicity—assume that the cost of treatment is similar for newborn sepsis. Bhutta et al estimated that a package of interventions to address stillbirth, neonatal and maternal deaths could be provided at US$60 per DALY averted.2 Since the 2015 gross domestic product (GDP) per capita in Ethiopia was US$619,20 treatment of the ill newborn can be considered highly cost-effective.
Financial burden
In the case analysed, the father expressed that costs of seeking healthcare are too high and was worried about the welfare and food supply for the family if he has to sell their seeds.
Health systems that largely depend on OOP payments rather than prepayments expose households for great financial risk and poor health.3 In Ethiopia, 48% of healthcare costs for children are covered OOP payments.21 We assume that neonatal sepsis and infections account for 20% of all deaths from respiratory infections.1 Extrapolating from Verguet et al’s study on the burden of medical impoverishment in Ethiopia, we estimate that neonatal pneumonia and sepsis cause 11 800 poverty cases per year.22
Thirty-four per cent of the Ethiopian population lives on less than US$1.90 a day (2011 PPP).20 When we adjust the cost of treatment for purchasing power, the OOP expenditure of US$64 equals about US$175 (current international purchasing power parities (PPPs)).19 The family in the case is likely to live below the poverty line, and we estimate the relative impact of treatment to be close to 3 months’ spending (US$175/US$1.90=92 days).20 These estimates indicate that the consequences for family welfare are severe. The financial well-being of the household is likely to influence the future of the family and the newborn. Yet, the monetary value in our estimates may not fully reflect the real loss for the family. If they sell their seeds, there will be an immediate loss as well as an impact on future sources of food and income. This may influence other family members, where the newborn and other children may get less food, can no longer go to school, or the parents must find additional sources of income.
What laws, rules or guidelines regulate the decision?
Ethiopia ratified the United Nations Convention on the Rights of the Child in 1991. The Convention recognises the right of children to have the highest attainable standard of health and the obligation of the state to pursue implementation.23
For this analysis, two strategies by the Federal Ministry of Health are of particular relevance. The National Strategy for Newborn and Child Survival in Ethiopia focuses on goals and plans to ensure coverage of high-impact neonatal interventions with an emphasis on marginalised populations.24 In the Health Sector Transformation Plan V, Ethiopia has committed to move towards UHC, where necessary services are to be made accessible for everyone while providing protection against financial risk.21 However, there is limited guidance on how to incorporate concerns about financial risk in priority setting and decision-making.
WHO guidelines and national treatment guidelines on neonatal illness and sepsis clearly state that the newborn - in this case - should be treated.14
Who are the involved stakeholders?
The most-affected parties are the ill newborn, the parents, other children in the family, the healthcare worker, other ill newborns, community members, society, policy-makers and international stakeholders.
What are the stakeholders’ potential burdens and benefits?
We consider benefits and burdens of affected parties if treatment for the ill newborn is withheld to protect against financial risk (table 2).
Table 2.
Benefits and burdens of limiting treatment to protect against financial risk
| Benefits | Burden | |
| The ill newborn | No direct benefit | The chance of survival decreases, and the newborn is likely to die |
| The parents | Avoid selling their harvest/seeds Avoid risk of catastrophic health expenditures More resources for food and other necessities |
Emotional burden of losing a baby Future productive loss of losing a child Immediate funeral costs, etc. Long-term lost income if the child lived |
| The other children | More resources for other children: improved nourishment, opportunity to go to school, improved health | Emotional and productive burden of losing a sibling |
| The health worker | Protecting the family against high costs and financial risk | Moral distress of not providing treatment to the ill newborn Professional stress when not following medical guidelines |
| Other ill newborns | Indirect: More physcial room and public resources for other ill newborns in the hospital | Indirect: Shape perceptions and practices of (not) seeking treatment for ill newborns |
| Community members | Friends and neighbours have to lend money to family with ill newborn | Loss of a new child Fear that high costs of treatment might delay care-seeking for others |
| Society | Avoid further poverty | Loss of one citizen |
| Policy-makers | Less families experiencing high OOP payments Success in financial risk protection outcomes |
Higher newborn mortality rate Lack of success in newborn mortality |
| International stakeholders | Less poverty cases due to high OOP payments Success in financial risk protection outcomes |
Higher newborn mortality rate Lack of success of newborn health programmes or funding |
OOP, out of pocket.
The largest benefits will be for other family members. By restricting treatment, the family avoids devastating costs for their already-vulnerable economic situation. The costs of treatment may push them into the vicious circle of poverty and ill health. The most severe burden will be on the ill newborn, who will lose out on better survival chances when not receiving medical treatment. Health workers might experience moral and professional stress if the newborn is not treated.
If it is perceived as acceptable to give priority to household needs over newborn health in the community, this might delay seeking care for other ill newborns.11 Although policy-makers and international stakeholders will not be directly affected by one additional newborn death or one additional poverty case, general trends in newborn mortality and OOP expenses are relevant for their work.
What interests are in conflict?
The direct interests of the newborn, the parents and other children of the family are in conflict. Without treatment, the newborn’s chances of survival are lower, and the newborn may die. It is in the economic interest of the parents and siblings to not sell their assets, in this case, their seeds, to avoid financial ruin. At the same time, the loss of a newborn is an emotional burden and a future productivity loss for the family.
Indirectly, the interests at stake and conflict between the newborn and the family’s interests affect the health worker. From a professional view, the health worker’s obligations concern the patient. However, in handling the dilemma, the physician is likely to be challenged by concerns for family welfare.9
What are the values and principles at stake?
There are several values and principles at stake in this dilemma, such as respecting patient autonomy, the healthcare worker’s duty to care and the principles to do good (beneficence) and do no harm (non-maleficence).25 Following a non-consequentialist approach, the healthcare worker’s duty to provide a life-saving treatment may very well override all other concerns for the well-being of other family members. Yet, the purpose of our analysis was to discuss the ethical acceptability of prioritising health versus welfare, which we discuss with regards to the criteria in the WHO framework. In our discussion of justice and fairness, we pay particular attention to health maximisation, priority to the worse-off and financial risk protection.3
Maximising health
The newborn, if treated, can expect to live up. Though she has an increased risk of long-term complications,16 17 the most likely outcome is survival without sequels. Limiting highly cost-effective treatment would not maximise health.2 The newborn will most likely die.
Priority to the worse-off
The WHO framework identifies the worse-off in terms of health as those with the largest individual disease burden.3 26 iv The ill newborn is worse-off in terms of potential lifetime health loss, and benefits to the newborn should therefore have extra weight. Even if we include non-health outcomes, no other person in the family is as badly off as the ill newborn, although the total well-being loss to the family due to the financial burden may be larger. Thus, the weight assigned to the worst-off, in this case the newborn, will affect the aggregated sum of benefits and burdens under the two alternatives.
Protecting against financial risk
At the micro level, concerns for financial risk protection for all family members may favour limiting treatment for the newborn. Some may argue that improved well-being outcomes for the parents and older children, taken together, are more important than the improved health outcome for the newborn. We grant that the unweighted sum of well-being for the family, in this case, may be greater than the burden for the newborn if left to die. Yet, the well-being gain for each member of the family is, in this case, substantially smaller than the burden imposed on the newborn. The key question is whether these smaller benefits for many outweigh the larger loss for the one newborn.
Altogether, when we assess the total burdens and benefits for all family members compared with the well-being loss and gain for the newborn, the latter outweighs the former when additional weight is assigned to the health benefits for the worse-off. This is a judgement made by the authors—we attach a large weight to the substantial benefit of survival for the newborn—and we acknowledge that others, including the mother and father in this case, may reach a different conclusion.
Discussion
Health benefits or financial risk protection?
The stakes are high in the micro-level dilemmas families and health workers face in settings without UHC. The empirically derived case is constructed, but we have reason to believe that patients, next of kins and healthcare professionals face similar choices in settings where healthcare is largely financed OOP. The ethical dilemma concerns what to do when family members or health workers cannot both improve health and protect against financial risk. For the father and mother: should they sell their seeds to pay for treatment, or not? For the health worker: should she advise the parents to seek care at the hospital, or not? At worst, their choices can cause newborn death, economic disaster or both.
Central in this dilemma is the value judgement on whether to take well-being beyond health outcomes into account or not.6 27 Should we consider only direct health benefits or include non-health and indirect benefits? Brock has argued that "different activities have different distinct purposes".27 The purposes of these activities, such as healthcare services to improve health, should determine their "proper sphere", and goods and resources should be distributed based on the activities they produce.27 While the argument to separate allocation of health and non-health benefits may hold in an ideal world, the pragmatic reality seen in the real-life dilemmas illustrated in our case shows how spheres are not separated at household level. As long as patients pay OOP for healthcare services, families’ decisions are constrained by one budget, and both health and non-health concerns are taken into account in intra-household decisions. Persad and du Toit argue that relying on separate spheres through "tunnel-vision approaches" in health policies is a mistake.6
We agree and accept that well-being beyond health is relevant, and that health maximisation, priority to the worse-off and financial risk protection are ethically relevant criteria for priority setting. However, it is not clear what to do when these concerns conflict.3 Depending on which outcome one values most, and for whom, one may conclude that it is either acceptable or unacceptable to limit treatment. Though limiting treatment can secure 3 months of daily expenses and thus secure a total well-being gain for the whole household, the baby has a high chance if dying and is clearly worse-off than the others (table 1). In our all-things-considered judgement, where gains to the worse-off are given additional weight, we incline towards the option that limiting treatment is not acceptable.
Does this mean that we accept the real-life implications of this position? It may suggest that it is wrong for the family to withhold treatment from the newborn, and that the health professional should attempt to persuade them to borrow money or sell their seeds to afford treatment. Although we, as authors, make this judgement, we accept that the family may come to a different conclusion based on their balancing of expected gains and burdens. Health professionals can help clarify this choice and provide relevant arguments, but in this particular context the family will and should make the final decision.
Unacceptable real-life dilemmas
Our case highlights a real-life dilemma between promoting health benefits and reducing financial risk that plays out in healthcare systems worldwide.28 However, from a normative perspective, there are problematic consequences of accepting this situation and treating it merely as a dilemma where an ethically acceptable solution can be found. As a society, we should not accept that the worst-off newborn dies from a disease that could have been easily avoided with cost-effective interventions or that the family falls into financial ruin. The unfair choices imposed on the family and health worker is caused by priorities and choices made at health system level.
In their reflections on distributive justice, it is relevant to consider how people’s preferences, beliefs and choices are shaped by underlying conditions.29 30 Following Sen’s capabilities approach, being poor and ill—as seen in the case analysed—can be understood as deprivations of freedoms.29 Both as means and ends, poverty and ill health may restrict people’s capabilities to ‘live the kind of life they have reason to value’.29Conceptualised as adaptive preferences, Sen and Nussbaum discuss how individuals adjust their preferences based on the choices that are available to them.31 32 In the dilemma analysed, the most-affected parties—the newborn, family members and health worker—cannot make free choices about whether to limit treatment or not. There is reason to believe that they would value treating the newborn without ending in financial ruin, but without money, this is not a real option.10 We argue that the situation in which the ethical dilemma plays out is unacceptable and unfair. Worldwide, healthcare is often financed by patients and their families, and opportunities to survive and enjoy lives without poverty often depend on economic factors. Our discussion demonstrates that the resource-constraints settings in which these dilemmas occur compromise people’s substantive freedoms and could have been avoided by pooling resources for high-priority health services.
Micro-dilemmas and macro-decisions
Policy-level questions on UHC typically centre on which services to include, to whom they should be provided and how to protect against financial hardship.3 Organisation and implementation of health and welfare systems, closely connected to macro-decisions, influence micro-level practices and opportunities. Dilemmas faced by families and health workers (box 1) are shaped by policy choices at higher levels of the system. In Ethiopia, life expectancy increased by 9 years between 2005 and 2015,1 and in 2013, total health spending was 4.7% of GDP.7 An essential healthcare package is being implemented, and advanced medical treatments such as renal transplants and cancer care are about to be implemented in selected hospitals.21 Although these new services seem promising, expanding access to low-priority and medium-priority services when larger parts of the population cannot access or afford high-priority services is problematic.3 33 From a fairness perspective, reducing OOP payments for essential services, such as antibiotic treatment for neonatal infections, is more important than ensuring access to expensive and less-effective services, such as advanced cancer treatment.21 If basic newborn healthcare services were provided at no or low cost, the unacceptable ethical dilemma analysed in this study would not be present. Trade-offs between health and welfare may always be present, but examples such as the case analysed are particularly problematic. For cost-effective services for a group that is worse-off in terms of health and well-being, lower-level decision-makers should not be left to choose between health benefits and financial risk protection. Progressive realisation of UHC can make care-seeking without falling into poverty a reality, which may intrinsically and instrumentally enhance people’s capabilities.3 Ethiopia’s roll-out of community-based and social health insurance represents promising steps away from financing models based on OOP payments and voluntary mechanisms. Yet, to progressively realise UHC here and in countries worldwide, it is urgent to make high-priority services affordable.
Methodological concerns
A better understanding of real-life dilemmas is relevant for health policies and for normative discussions to illuminate what justice—and injustice—means. As far as we know, this is one of the first attempts to explicitly analyse a micro-level ethical dilemma where concerns for health benefits and financial risk protection diverge. Some important methodological considerations should be noted. We chose the WHO framework for our analysis, which included financial risk, a criterion that has received little attention in the medical ethics literature. However, it did not take bedside rationing considerations, such as health professionals’ duty to care, into account.9 12 While this may have left out relevant principles or values, it was a deliberate choice on our part as we aimed to focus on financial risk. Further discussion of the health–welfare trade-off, whether these concerns are incommensurable, and the role of professional duties, are of great interest but beyond the aim of this study.
The strength of evidence on outcomes can be questioned. In the analysis, we simply assumed that the baby suffered from neonatal sepsis and could be saved. In real life, health outcomes may depend on additional factors such as quality of treatment, appropriate care and the aetiology of illness.16 17 This may also hold for our assumptions on financial risk, where data are even more limited. To address these challenges and research gaps, further empirical studies on financial burden and indirect costs and benefits,19 22 and normative discussion on how to weigh health and non-health concerns are needed.6
Studies show that healthcare financing in low-income countries is particularly dependent on OOP payments.4 7 Though our analysis deliberately focused on one case from Ethiopia, it is likely that similar tragic dilemmas are seen in other settings, and especially in underfinanced healthcare systems. While essential newborn health services are very effective, analysis of other services for other less severe diseases may influence the balance in the health–welfare trade-off towards a different conclusion. Though context always matters, we still believe the ethical issues highlighted are relevant for discussions on fairness and financial risk protection.
Concluding remarks
By analysing an ethical dilemma in a resource-constrained setting, we have seen that non-health factors challenge our views about which principles matter in priority setting and how conflicting concerns should be balanced. Families’ and health workers’ choices about health benefits or protection against financial ruin play out at micro level, but are influenced by macro-level decisions and priorities. If we neglect the fact that non-health factors affect real-life priority setting, in particular the health and welfare of the poor, this neglect may perpetuate and reinforce inattention to underlying structural issues that shape health and development.
Acknowledgments
We thank colleagues in the Global Health Priorities research group and two anonymous reviewers for their helpful feedback.
Footnotes
In the WHO framework, the worse-off in terms of health is understood as those with the largest individual disease burden.3
Limiting treatment is understood as not receiving recommended antibiotics and supportive treatment at the referral hospital.
Data on long-term outcomes of sepsis in term newborns in resource-constrained settings are limited.16 17
The literature on badness of death discusses other ways to assess when it is worst to die.26
Contributors: The project idea and analysis was developed by KHO, IM and OFN. KHO wrote the first draft of the manuscript and incorporated critical feedback from IM and OFN. All authors read and approved the final manuscript.
Funding: The study was funded by the Norwegian Research Council (Global Health Priorities 2020 project, no. 218694/H10).
Competing interests: None declared.
Patient consent: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: The study did not include use of primary data.
References
- 1.Institute for Health Metrics and Evaluation. GBD results tool. 2017. http://ghdx.healthdata.org/gbd-results-tool (accessed 12 Apr 2017).
- 2. Bhutta ZA, Das JK, Bahl R, et al. . Can available interventions end preventable deaths in mothers, newborn babies, and stillbirths, and at what cost? Lancet 2014;384:347–70. 10.1016/S0140-6736(14)60792-3 [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Making fair choices on the path to universal health coverage: final report of the WHO Consultative Group on Equity and Universal Health Coverage. Geneva: World Health Organization, 2014. [Google Scholar]
- 4. Stenberg K, Hanssen O, Edejer TT, et al. . Financing transformative health systems towards achievement of the health Sustainable Development Goals: a model for projected resource needs in 67 low-income and middle-income countries. Lancet Glob Health 2017;5:e875–e887. 10.1016/S2214-109X(17)30263-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ottersen T. Lifetime QALY prioritarianism in priority setting. J Med Ethics 2013;39:175–80. 10.1136/medethics-2012-100740 [DOI] [PubMed] [Google Scholar]
- 6. Persad G, du Toit J. The case for valuing non-health and indirect benefits : Emanuel EJ, Verguet S, Jamison D, Global health priority-setting: beyond cost-effectiveness. Oxford: Oxford University Press; (forthcoming). [Google Scholar]
- 7. Dieleman JL, Templin T, Sadat N, et al. . National spending on health by source for 184 countries between 2013 and 2040. Lancet 2016;387:2521–35. 10.1016/S0140-6736(16)30167-2 [DOI] [PubMed] [Google Scholar]
- 8. Nations U. Transforming our world: the 2030 agenda for sustainable development. New York: United Nations, 2015. [Google Scholar]
- 9. Defaye FB, Danis M, Desalegn D, et al. ; Financial risk protection at the bedside: how Ethiopian physicians try to minimize out-of-pocket health expenditures (forthcoming). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Onarheim KH, Sisay MM, Gizaw M, et al. . Selling my sheep to pay for medicines—household priorities and coping strategies in a setting without universal health coverage. BMC health services research. 2018. 18(1): 153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Onarheim KH, Sisay MM, Gizaw M, et al. . What if the baby doesn’t survive? Health-care decision making for ill newborns in Ethiopia. Soc Sci Med 2017;195(Suppl C):123–30. 10.1016/j.socscimed.2017.11.003 [DOI] [PubMed] [Google Scholar]
- 12. Defaye FB, Desalegn D, Danis M, et al. . A survey of Ethiopian physicians' experiences of bedside rationing: extensive resource scarcity, tough decisions and adverse consequences. BMC Health Serv Res 2015;15:467 10.1186/s12913-015-1131-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Miljeteig I, Johansson KA, Sayeed SA, et al. . End-of-life decisions as bedside rationing. An ethical analysis of life support restrictions in an Indian neonatal unit. J Med Ethics 2010;36:473–8. 10.1136/jme.2010.035535 [DOI] [PubMed] [Google Scholar]
- 14.World Health Organization. Compilation of WHO recommendations on maternal, newborn, child and adolescent health: recommendations on newborn health. Geneva: World Health Organization, 2013. [Google Scholar]
- 15. Zaidi AK, Ganatra HA, Syed S, et al. . Effect of case management on neonatal mortality due to sepsis and pneumonia. BMC Public Health 2011;11(Suppl 3):S13 10.1186/1471-2458-11-S3-S13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Seale AC, Blencowe H, Zaidi A, et al. . Neonatal severe bacterial infection impairment estimates in South Asia, sub-Saharan Africa, and Latin America for 2010. Pediatr Res 2013;74(Suppl 1):73–85. 10.1038/pr.2013.207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mwaniki MK, Atieno M, Lawn JE, et al. . Long-term neurodevelopmental outcomes after intrauterine and neonatal insults: a systematic review. Lancet 2012;379:445–52. 10.1016/S0140-6736(11)61577-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia Demographic and Health Survey 2016: Key Indicators Report. Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA and ICF, 2016. [Google Scholar]
- 19. Memirie ST, Metaferia ZS, Norheim OF, et al. . Household expenditures on pneumonia and diarrhoea treatment in Ethiopia: a facility-based study. BMJ Glob Health 2017;2:e000166 10.1136/bmjgh-2016-000166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.World Bank. World Bank Open Data. 2017. http://data.worldbank.org/ (accessed 10 Aug 2017).
- 21.Federal Democratic Republic of Ethiopia Ministry of Health. Health Sector Development Programme V. Addis Ababa, Ethiopia: Federal Democratic Republic of Ethiopia Ministry of Health, 2015. [Google Scholar]
- 22. Verguet S, Memirie ST, Norheim OF. Assessing the burden of medical impoverishment by cause: a systematic breakdown by disease in Ethiopia. BMC Med 2016;14:164 10.1186/s12916-016-0697-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.United Nations General Assembly. Convention on the rights of the child. United Nations, 1989. [Google Scholar]
- 24.Federal Democratic Republic of Ethiopia Ministry of Health. National newborn and child survival strategy document brief summary: 2015/16–2019/20: Federal Democratic Republic of Ethiopia Ministry of Health, 2015. [Google Scholar]
- 25. Beauchamp T, Childress J. Principles of biomedical ethics. 6th edn New York: Oxford University Press, 2009. [Google Scholar]
- 26. Solberg CT, Gamlund E. The badness of death and priorities in health. BMC Med Ethics 2016;17:21 10.1186/s12910-016-0104-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Brock DW. Separate spheres and indirect benefits. Cost Eff Resour Alloc 2003;1:4 10.1186/1478-7547-1-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Norheim OF, Emanuel EJ, Millum J, Global health priority-setting: beyond cost-effectiveness. Oxford: Oxford University Press; (forthcoming). [Google Scholar]
- 29. Sen A. Development as freedom. 1st ed New York: Oxford University Press, 1999. [Google Scholar]
- 30. Nussbaum MC. Women and human development: the capabilities approach. Cambridge; New York: Cambridge University Press, 2000. [Google Scholar]
- 31. Sen A. Rights and capabilities. Resources, values and development. Harvard University Press, 1984. [Google Scholar]
- 32. Nussbaum MC. Adaptive preferences and women’s options. Women and human development: the capabilities approach. Cambridge, New York: Cambridge University Press, 2000:312. [Google Scholar]
- 33. Norheim OF. Ethical perspective: five unacceptable trade-offs on the path to universal health coverage. Int J Health Policy Manag 2015;4:711–4. 10.15171/ijhpm.2015.184 [DOI] [PMC free article] [PubMed] [Google Scholar]


