Abstract
Introduction:
Approximately 5%–11% of neurologically normal population has extensor plantar response (EPR).
Method:
This study is aimed to identify differentiating features of EPR between physiological and pathological population.
Results:
A total of 43 patients with pyramidal lesions and 113 normal controls were recruited for this study. The pathological EPRs were more reproducible, with 89.4% having at least two positive Babinski responses and 91.5% having two positive Chaddock responses (vs. 14.3% and 4.8% in controls, P < 0.001). The pathological EPR was more sensitive to stimulation, in which 89.1% were elicited when the stimulation reached mid-lateral sole (vs. 11.9% in controls, P < 0.001). Most (93.6%) pathological cases had sustained big toe extension throughout stimulation (vs. 73.8% in controls, P < 0.001). As compared to those with brain lesion, the plantar responses in those with spinal lesion are less likely to have ankle dorsiflexion (5.3% vs. 25%, P < 0.05) more likely to have sustained extensor response with Babinski (94.7% vs. 71.4%, P < 0.05), Chaddock (89.5% vs. 64.3%, P < 0.05), and Schaefer (26.3% vs. 3.6%, P < 0.05) methods. A scoring system was computed using four variables, i.e., two consecutive positive Babinski or Chaddock responses, extensor response at mid-lateral sole, and sustained extension throughout stimulation. A score ≥3 is predictive of pathological origin, with sensitivity and specificity of 78.7% and 95.2%, respectively.
Conclusion:
The pathological EPR is more reproducible, sensitive to stimulation, and sustainable compared to physiological extensor response.
Keywords: Babinski, Chaddock, physiological plantar response, plantar response, reflex, Schaefer
INTRODUCTION
Joseph Babinski's discovery on plantar reflex was presented in 1896.[1] According to him, plantar stimulation by stroking the lateral sole of the foot to the base of 5th toe and arcing toward the base of the big toe produce a downward deflection (or plantar flexion) of the great toe in those with normal upper motor neuron function and upward deflexion (or dorsiflexion) of the great toe and fanning of the other toes in those with an upper motor neuron lesion (UMNL). Babinski's discovery was initially known as “phenomene des orteils” or “phenomenon of toes.” Five years later, he added a new feature: abduction of the toes after plantar stimulation, which is known as the “fan sign” and initially described by Dupre.[2] This response is now referred eponymously as the “Babinski sign” or descriptively as the extensor plantar response (EPR).[3] Babinski has established a clinical significance of the reflex as a positive Babinski's sign which indicates pathology in the upper motor neuron. The introduction of Babinski's concept on plantar responses has been widely practised as an essential component of a complete neurological examination.[4]
Little is known about the reliability and validity of Babinski's sign. Plantar responses can be inconsistent with differences in tools, strength, methods, and assessors. Isaza Jaramillo et al. has reported that Babinski sign has low sensitivity (50.8%, 95% confidence interval [CI] 41.5–60.1), but high specificity (99%, 95% CI 97.7–100) in identifying pyramidal tract dysfunction with a positive likelihood ratio of 51.8 (95% CI 16.6–161.2) and calculated interobserver variability of 0.73 (95% CI 0.598–0.858).[5] Deng et al. observed that dorsiflexion of the big toe without recruitment of the other toes is more common in patients with cortical pyramidal tract lesions, while in those with lesions lower than cortex (corona radiata to the spinal cord) movement of other toes in addition to the big toe is more common.[6] De Jong has noted that an EPR may occasionally occur in patients with no evidence of corticospinal tract lesion.[7] We conducted a study on the variability of plantar response in normal population which demonstrated positive Babinski's sign in 5%–11% of the normal population, including those with withdrawal response, consistent with previous studies.[7,8,9,10] Withdrawal responses induced by nociception and ticklish sensation are seen in about 5% of the normal population. These responses are mostly characterized by flexion of the big toe and other toes, knee, and hip flexion with dorsiflexion of the ankle.[10,11]
Hence, this study aimed to characterize the differences in EPR (positive Babinski's sign) elicited in normal and pathological population.
METHODOLOGY
A total of 156 subjects were recruited, including 43 patients with imaging-proven UMNL from Neurology Clinic and Wards, University Malaya Medical Centre, Kuala Lumpur, Malaysia. UMNL is defined in this study as a lesion in the pyramidal tract along the cortex, subcortical area, and spinal cord, identified in the neuroimaging. The etiologies of the patient enrolled include stroke, multiple sclerosis, and transverse myelitis. The remaining 113 out of 156 subjects were medical students without neurological deficit (control subjects). This study was approved by the Medical Ethics Committee of University Malaya Medical Center (MEC ID No: 20151-917). Written consent was obtained from all the participants.
Plantar examination procedure
All subjects were examined either in supine or seating position with their knees in extension. The subject was asked to relax and rotate their head to the opposite direction. Four different plantar examination methods, i.e., Babinski, Chaddock, Oppenheim, and Schaefer methods,[7] were performed thrice each on both lower limbs. All responses were videotaped for reassessment. The examiner (SFL and NKJ) first went through an intensive training to accustom themselves with methods of examination and documentation of findings, and their skills were evaluated by a neurologist (KSL) before the commencement of the research. Two assessors alternated in performing the examination of plantar reflexes on the subjects. Whenever there was no plantar response, Jendrassik maneuvre was performed.[7,12] Assessors were not blinded about the status (physiological/pathological), but the findings were documented by two separate assessors, and discrepancies were resolved through mutual consensus and by reviewing video recording of the assessment to minimize bias.
Observation in four aspects was made, including the movement of all joints in the lower limb, level of plantar stimulation inducing a response [Figure 1], movement of the contralateral leg, and the sequential movements of the big toe. The responses were recorded as follows: (a) first great toe movement as extension, flexion, or no movement; (b) other toe extension, flexion, or no movement; (c) toe abduction, adduction, or no movement; (d) ankle dorsiflexion, plantar flexion, or no movement; and (e) knee and hip flexion or no movement. Findings of big toe extension with abduction, flexion, or no movement of other toes were concluded as positive Babinski response. According to previous studies, withdrawal response is described as an extension of other toes with or without knee and hip flexion.[7]
Figure 1.
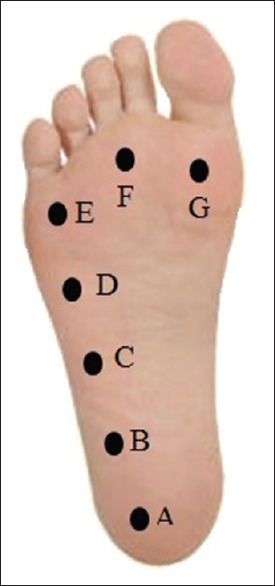
Level of the plantar stimulation at which a response was induced
The sensitivity to stimulation is determined by documenting the site of plantar stimulation inducing a response. Documentation was recorded as follows: (I) near the heel, (II) quarter-point, (III) midpoint, and (IV) three-quarter point along the lateral aspect of the sole between the heel and the base of the 5th toe, (V) base of the 5th toe, (VI) the 3rd toe, and (VII) the big toe [Figure 1]. The response of the contralateral leg was reported in a similar way.
Sustainability of the response was determined by documenting the sequential movement of the big toe in the following manner: (a) extension throughout, (b) flexion throughout, (c) extension followed by flexion, (d) flexion followed by extension, and (e) no movement.
Chaddock reflex was conducted by stroking the lateral aspect of the dorsum of the foot. Stroking begins from the inferior lateral malleolus and extending forward toward the 5th toe.[7] Oppenheim sign was examined by applying a great force by dragging the knuckle down from the inferior patella, along with the anteromedial surface of the tibia toward the ankle. Schaefer sign was elicited by application of deep pressure on the Achilles tendon.[7]
Statistical analysis
All analyses were performed using the statistical (IBM SPSS Statistics for Windows, IBM corp., Armonk, NY, USA), and significant level was set at a P < 0.05. Chi-square tests were used to determine the significance of differences between pathological and physiological EPR. A scoring system was computed from statistically significant variables, to differentiate pathological from physiological EPRs.
RESULTS
There were 89 feet with big toe extension – 47 in patients with UMNL (pathological EPR) and 42 in controls (physiological EPR). The patient group was older (mean age 58.3 ± 13.5 years vs. 21.0 ± 1.5 years in controls, P < 0.001) and matched in gender with the control group (51.3% male vs. 63%, respectively). The causes for UMNL were mainly stroke (74.4%) followed by myelitis (25.6%).
Extensor response including withdrawal response was seen in 42 (18.6%) of 226 feet in the normal subgroup. Withdrawal response comprises of 20/42 (47.6%) of the extensor response, while the remaining 22/42 (52.4%) were concluded as positive Babinski response. The pathological plantar responses were more reproducible, with 89.4% having at least two positive Babinski responses (vs. 14.3% in normal subjects, P < 0.001); this is similar to the Chaddock method whereby 91.5% had at least two positive responses versus 4.8% in controls (P < 0.001) [Table 1]. The plantar examination using Oppenheim and Schaefer methods was less sensitive, in which only 27.7% and 42.5% had positive Oppenheim and Schaefer responses, respectively. More subjects in physiological group with EPR had ankle dorsiflexion (45%), knee flexion (36%), and hip flexion (36%), as compared to the pathological group (17%, 2.1%, and 2.1%, respectively, P < 0.05).
Table 1.
Differentiating big toe extension using different plantar reflexes between physiological (n=42) and pathological (n=47) population
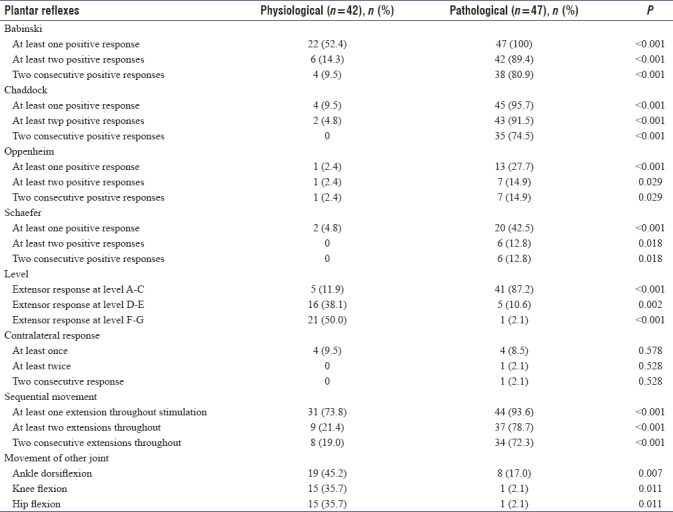
The pathological EPR was more sensitive to stimulation, in which 89.1% were elicited when the stimulation reached level III of plantar stimulation, which is at the midpoint along the lateral sole between the heel and the 5th toe, as compared to 11.9% in the normal controls (P < 0.001). Nearly 97.8% of pathological EPR was elicited by stroking the lateral sole. Majority of the physiological EPR occurred at level V and above, and 40.5% were elicited by stroking through the base of toes (level VII).
Contralateral response was not commonly found in both physiological and pathological plantar responses.
The pathological EPR was more sustainable, with most (93.6%) having sustained extension throughout stimulation, and only 6.4% had nonsustained extension followed by flexion. Controls experience much lower percentage (73.8%) of sustained extension throughout stimulation (P < 0.001).
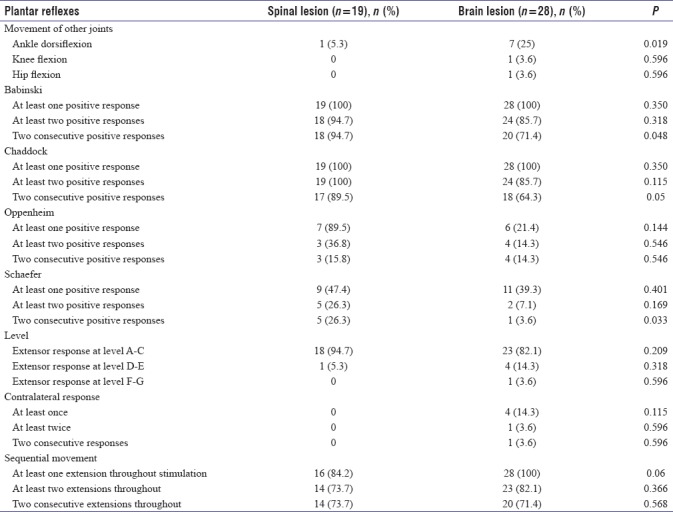
As compared to those with brain lesion, the plantar responses in those with spinal lesion are less likely to have ankle dorsiflexion (5.3% vs. 25%, P = 0.019) and more likely to have sustained extensor response with Babinski (94.7% vs. 71.4%, P < 0.05), Chaddock (89.5% vs. 64.3%, P = 0.05) and Schaefer (26.3% vs. 3.6%, P < 0.05) methods [Table 2].
Table 2.
Differentiating big toe extension using different plantar reflexes between those with spinal lesion (n=19) and brain lesion (n=28)
Jendrassik maneuver was not performed in the pathological group as the majority of the patients either had weakness or unable to comprehend command. In the physiological group with no EPR, 6% were found to have extensor big toe after Jendrassik maneuver.
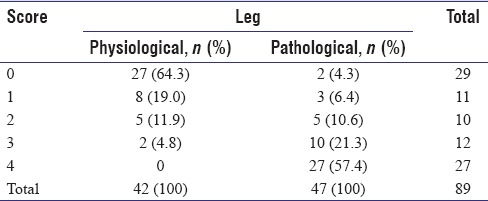
We had computed a scoring system using four variables with significant differences between the pathological and physiological EPR at P < 0.001, i.e., (a) two consecutive positive Babinski response, (b) two consecutive positive Chaddock responses, (c) EPR at level III of plantar stimulation, and (d) sequential movement with extension throughout stimulation. Each variable was given one mark if present and 0 if absent. As shown in Table 3, majority (78.7%) of the pathological EPR scored 3 and above, as compared to 4.8% in the physiological EPR. The sensitivity and specificity of using a score of 3 or more to predict whether the EPR is pathological were 78.7% and 95.2%, respectively
Table 3.
Scoring system to differentiate physiological and pathological population
DISCUSSION
EPR, also known as positive Babinski response, can be elicited in normal population. In this study, as high as 18.6% of controls had EPR, which is partially explained by withdrawal response. However, the physiological extensor response is characteristically different from pathological response, whereby the pathological EPR is more reproducible (with positive Babinski or Chaddock response in at least two attempts), sensitive to stimulation (with response induced with early stimulation at the lateral sole), and sustainable (with extension of big toe throughout stimulation), as compared to physiological EPR.
Van Gijn and Bonke investigated the biasing effect of other signs and symptoms on the interpretation of plantar reflex. They have found significant relation whereby physician interpretation on the direction of toe movement differed significantly, conforming to the history given.[13] This study has ensured that bias is minimized by two independent assessors whereby discrepancies were resolved through mutual consensus and by reviewing the video recording of the assessment.
We have shown that pathological EPR is more likely to be reproducible than those seen in the normal population. This is comparable with the previous study by Vin Gjin and Bonke which described the reproducibility of true Babinski's response, unlike voluntary withdrawal of the toes.[13] This was in contrast with De Jong's observation whereby repeated stimulation of the sole reduces extensor movement and finally disappear.[7]
We have shown that pathological EPR is sensitive. Babinski's method has two components, i.e., (a) stroking from the heel to the base of the 5th toe and (b) arcing medially toward the base of the big toe. However, the reason of performing the second component is not well stated by Babinski. In our study, stroking the lateral sole was able to elicit EPR in most cases in the patient group. This corresponds to De Jong's assertion whereby extensor movement of the great toe is quick, and response usually occurs by the time the stimulus reaches the midportion of the foot. In normal subjects, almost 40% of the EPRs were elicited after stroking the base of the toes. It has previously been reported by Grimby that stimulation of the sole of the foot in a normal subject may result in extensor activity on hallux stimulation,[14] possibly due to the direct stimulation of extensor halluces longus tendon. Thus, this study suggests that stroking the lateral sole is enough to elicit pathological EPR, and stroking through the base of the toes should best be avoided.
De Jong described the nature of plantar response may vary whereby initial extension may be followed by flexion and less often brief flexion precedes extension.[7] In the present study, sequential movement, i.e., an extension of the big toe followed by flexion, was uncommon (6.4%) in those with pathological extensor response. Thus, observation of sustained extensor response throughout stimulation is another useful feature to differentiate pathological from physiological extensor response.
A scoring system is computed in this study, which demonstrated high sensitivity and specificity, whereby a cumulative score of 3 and above are more inclined toward the pathological response.
The Babinski and Chaddock reflex are complementary, and each can occur without the other, although both usually present in UMNL. It has been reported that Babinski and Chaddock reflex may be positive equally.[7,15] Chaddock's sign may appear before Babinski sign and may disappear later, and may be positive bilaterally in the unilateral lesion. However, the sensitivity of Chaddock, Oppenheim, and Schaefer methods in evoking an EPR was not previously reported, to the best of our knowledge. This study showed that Chaddock method is as sensitive as Babinski's method in evoking an extensor response in up to 95.7%, followed by 42.5% using Schaefer method and 27.7% using Oppenheim method.
As compared to those with brain lesion, the plantar responses in those with spinal lesion are less likely to have ankle dorsiflexion and more likely to have prominent and more sustained extensor response with Babinski, Chaddock, and Schaeffer response. Deng et al. has reported similar observation whereby dorsiflexion of the big toe is more commonly seen in patients with cortical pyramidal tract lesion than those lesions lower than the cortex.[6]
We postulated that those with UMNL could have contralateral response, similar to cross adductor response. However, our study reported contralateral response in about 10% of the cases, but there was no significant difference between the pathological and physiological groups. This may be due to the flexor reflex synergy which appears when the polysynaptic flexor response is active.[16]
Sherrington called it flexion reflex synergy because activation of all muscles results in shortening of the limb which forms the toe extension. During the 1st year of life, Babinski sign is a normal occurrence due to flexion synergy.[17] However, as the nervous system matures, flexion synergy is inhibited to facilitate ambulation. With upper motor neuron dysfunction, it is disinhibited, thereby resulting in reflex flexion withdrawal.[18,19] Controls with EPR could have a problem with inhibition of flexor reflex synergy. In the physiological group without extensor plantar reflex, Jendrassik maneuver results in 6% of EPR, possibly because Jendrassik maneuver disrupted the inhibition of flexor reflex synergy. However, this postulation requires further exploration.
Tickle-induced withdrawal can cause dorsiflexion of the great toe in a pattern similar to the Babinski sign, which can be reduced by self-stimulation. It is postulated that this inhibition takes place in the cerebellum.[20] Self-stimulation shall be considered in future study.
CONCLUSION
The pathological EPR is more reproducible, sensitive to stimulation, and sustainable compared to physiological extensor response.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Rehman HU. Babinski sign. Neurologist. 2002;8:316–8. doi: 10.1097/00127893-200209000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Van Gijn J. The Plantar Reflex: A Historical, Clinical and Electromyographic Study. Krips Repro, Meppel. 1977 [Google Scholar]
- 3.Morrow MJ, Mary MR. 'The babinski sign'. Br J Hosp Med. 2011;72:157–8. doi: 10.12968/hmed.2011.72.sup10.m157. [DOI] [PubMed] [Google Scholar]
- 4.Miller TM, Johnston SC. Should the babinski sign be part of the routine neurologic examination? Neurology. 2005;65:1165–8. doi: 10.1212/01.wnl.0000180608.76190.10. [DOI] [PubMed] [Google Scholar]
- 5.Isaza Jaramillo SP, Uribe Uribe CS, García Jimenez FA, Cornejo-Ochoa W, Alvarez Restrepo JF, Román GC, et al. Accuracy of the babinski sign in the identification of pyramidal tract dysfunction. J Neurol Sci. 2014;343:66–8. doi: 10.1016/j.jns.2014.05.028. [DOI] [PubMed] [Google Scholar]
- 6.Deng T, Jia JP, Zhang T, Guo D, Yang L. Cortical versus non-cortical lesions affect expression of babinski sign. Neurol Sci. 2013;34:855–9. doi: 10.1007/s10072-012-1132-8. [DOI] [PubMed] [Google Scholar]
- 7.Campbell WW. Dejong's the Neurologic Examination. 6th ed. United States of America: Lippincott Williams & Wilkings; 2005. [Google Scholar]
- 8.Kaye JA, Oken BS, Howieson DB, Howieson J, Holm LA, Dennison K, et al. Neurologic evaluation of the optimally healthy oldest old. Arch Neurol. 1994;51:1205–11. doi: 10.1001/archneur.1994.00540240049015. [DOI] [PubMed] [Google Scholar]
- 9.Maranhão-Filho P, Dib E, Ribeiro RG. Babinski and chaddock signs without apparent pyramidal disfunction. Arq Neuropsiquiatr. 2005;63:484–7. doi: 10.1590/s0004-282x2005000300022. [DOI] [PubMed] [Google Scholar]
- 10.Lee RA, Tay LL, Lim KS, Tan CT. Variability of plantar response in normal population. Neurol Asia. 2011;16:143–7. [Google Scholar]
- 11.Chew KS, Oon LK, Lim KS, Tan CT. Withdrawal response in healthy adult. Neurol Asia. 2010;15:159–65. [Google Scholar]
- 12.Nardone A, Schieppati M. Inhibitory effect of the Jendrassik maneuver on the stretch reflex. Neuroscience. 2008;156:607–17. doi: 10.1016/j.neuroscience.2008.07.039. [DOI] [PubMed] [Google Scholar]
- 13.Van Gijn J, Bonke B. Interpretation of plantar reflexes: Biasing effect of other signs and symptoms. J Neurol Neurosurg Psychiatry. 1977;40:787–9. doi: 10.1136/jnnp.40.8.787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grimby L. Pathological plantar response. II. Loss of significance of stimulus site. J Neurol Neurosurg Psychiatry. 1965;28:476–81. doi: 10.1136/jnnp.28.6.476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ghosh D, Pradhan S. “Extensor toe sign” by various methods in spastic children with cerebral palsy. J Child Neurol. 1998;13:216–20. doi: 10.1177/088307389801300504. [DOI] [PubMed] [Google Scholar]
- 16.Singerman J, Lee L. Consistency of the babinski reflex and its variants. Eur J Neurol. 2008;15:960–4. doi: 10.1111/j.1468-1331.2008.02219.x. [DOI] [PubMed] [Google Scholar]
- 17.Duysens J, De Groote F, Jonkers I. The flexion synergy, mother of all synergies and father of new models of gait. Front Comput Neurosci. 2013;7:14. doi: 10.3389/fncom.2013.00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bruno E, Horacio SM, Yolanda E, Guillermo GR. The articles of babinski on his sign and the paper of 1898. Neurol India. 2007;55:328–32. doi: 10.4103/0028-3886.37090. [DOI] [PubMed] [Google Scholar]
- 19.Kuruvilla A, Wattamwar PR. Kinaesthetic ipsilateral and crossed extensor plantar response: A new way to elicit upgoing toe sign (babinski response)? Ann Indian Acad Neurol. 2011;14:198–9. doi: 10.4103/0972-2327.85894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sohrab SA, Gelb D. Value of self-induced plantar reflex in distinguishing babinski from withdrawal. Neurology. 2016;86:977. doi: 10.1212/WNL.0000000000002454. [DOI] [PubMed] [Google Scholar]


