Abstract
Association of dengue fever with transverse myelitis is a rare phenomenon; involvement of a long segment is even rarer. We describe a middle-aged female who presented with weakness of bilateral lower limbs and urinary retention 4 days after recovery from dengue fever. She, in addition, had a sensory level up to the level of nipples. Magnetic resonance imaging confirmed the diagnosis of longitudinally extensive transverse myelitis. Besides, the patient had spontaneous subarachnoid hemorrhage (SAH) in the absence of dengue hemorrhagic fever. The patient was started on steroids along with rehabilitation. Our case highlights the extensive involvement of spinal cord in the postinfectious phase of dengue and inclusion of this arboviral disease in the differential diagnoses of myelitis as well as an etiology of SAH.
Keywords: Dengue, subarachnoid hemorrhage, transverse myelitis
INTRODUCTION
Dengue fever affects 100 million cases per year. The virus has been reported in nearly every country between the Tropic of Capricorn and the Tropic of Cancer putting 2.5 billion people at risk. Both overcrowding and increasing travel have been attributed to resurgence of Aedes aegypti – the vector of this arbovirus.[1,2]
The neurotropic effects are rare in uncomplicated dengue infection and have been recently recognized. Neurologic involvement during the acute phase manifests as encephalitis, myelitis, and meningitis – a consequence of direct invasion of central nervous system by the virus.[3]
The postinfectious phase may be associated with acute disseminated encephalomyelitis, neuromyelitis optica, optic neuritis, Guillain–Barré syndrome, myelitis, oculomotor palsy, and phrenic neuropathy. Among all, encephalitis is the most common neurologic manifestation. Spinal cord affliction in the postinfectious phase of dengue fever is rare. Moreover, if the spinal cord is affected in this phase, then the most frequent manifestation is transverse myelitis. Involvement of a long segment of the spinal cord, known as longitudinally extensive transverse myelitis (LETM), is far rarer.[4]
Hemorrhagic manifestations of dengue hemorrhagic fever (DHF) are a common occurrence. In the absence of DHF, bleeding has seldom been reported in dengue. Subarachnoid hemorrhage (SAH) in dengue fever with transient thrombocytopenia is an example of the latter.[5]
In the present case, we describe LETM and SAH in the postinfectious phase of dengue fever in a 55-year-old patient.
CASE REPORT
A 55-year-old female patient presented with a history of high-grade fever with chills 20 days back that lasted for 3 days. She, in addition, complained of myalgia and low backache. There was no history of headache, vomiting, cough, sore throat, and petechial rash.
Four days after the fever subsided, she developed acute-onset bilateral lower limb weakness with urinary retention. Besides, there was impairment of pain and touch sensation in both lower limbs and abdomen. However, there was no bowel involvement. There was no history of bleeding tendency or any unusual medical history.
Her general examination was unremarkable. Neurologic examination revealed flaccid paralysis of bilateral lower limbs with grade 0/5 power at both ankles, knees, and hips. Deep tendon reflexes were absent in both lower extremities. Abdominal reflexes were absent, and bilateral plantar reflexes were mute. She had a deficit in pain and touch perception that extended from bilateral lower limbs to the level of nipples. Neurologic examination of both upper limbs and cranial nerves was normal.
Laboratory investigations depicted hemoglobin of 10.2 g/dL, leukocyte count of 5 × 103/μL, and platelet count of 1.1 × 103/μL. Cerebrospinal fluid analysis showed absence of cells, glucose of 40 mg/dL (normal: 40–70 mg/dL), and protein of 74 mg/dL (normal: 15–45 mg/dL). Antinuclear antibody (by enzyme-linked immunosorbent assay) was negative. She, however, tested positive for dengue IgM antibody (single-step immunochromatographic assay).
Magnetic resonance imaging (MRI) of spine revealed a long-segment T2 and STIR hyperintense signal involving the central cord and extending from C2 to D4 [Figures 1 and 2]. Brain screening revealed FLAIR (fluid-attenuated inversion recovery) hyperintense signal in the frontal and occipital lobe sulci. A noncontrast computed tomography (CT) head confirmed these to be foci of SAH [Figure 3]. Hemogram at this stage showed platelet count to be 1.0 × 103 /μL with normal hematocrit.
Figure 1.
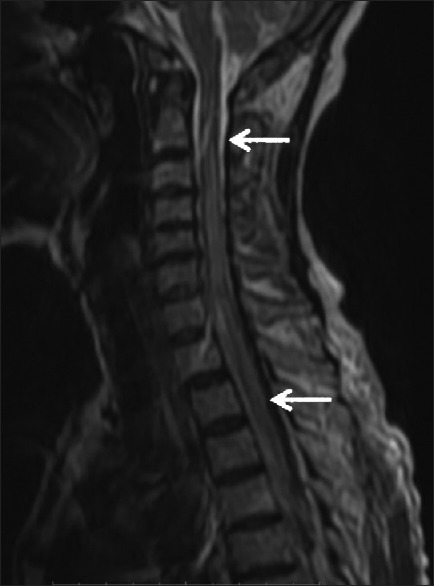
Sagittal T2-weighted image shows hyperintense signal within the cord extending from third cervical vertebrae to second thoracic vertebra
Figure 2.
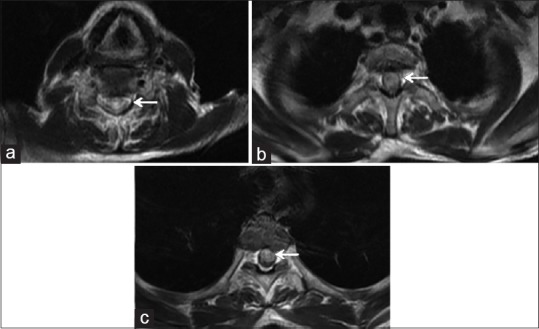
Axial sections at cervical (C7 in 2a) and thoracic (D1 in 2b; D3 in 2c) depict T2 hyperintense signal in the spinal cord
Figure 3.
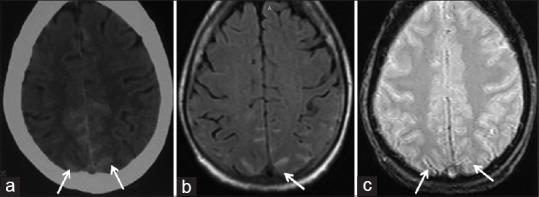
Axial sections of the brain reveal hyperdensity (a, computed tomography), hyperintensity on fluid-attenuated inversion recovery (b, MRI) along parafalcine sulci. (c) depicts corresponding susceptibility-weighted image. These findings confirm the presence of subarachnoid hemorrhage
The patient was catheterized and started on intravenous methylprednisolone pulse therapy (1 g/day for 5 days) along with physical therapy. Her platelet count returned to baseline without transfusion. On a 1-month follow-up, there was no significant improvement in her motor weakness.
DISCUSSION
Neurologic manifestations associated with dengue fever have been receiving an increased recognition due to their impact on overall prognosis. Dengue-associated transverse myelitis has been sparingly reported. The association between dengue infection and LETM is even rarer.[4]
Our patient had weakness of both lower limbs, urinary retention, and a sensory level extending up to the level of nipples. These deficits appeared 4 days after the fever subsided. Further, she tested positive for dengue IgM antibody. This thus established recent dengue infection (in the postinfectious phase) as the likely cause of LETM. Dengue-associated myelitis may develop more commonly in the acute infectious[6,7] phase or sometimes in postinfectious phase.[8,9] The pathogenesis of myelitis in our case was likely immune-mediated neural injury. However, the exact mechanism is not clear. LETM runs a poor prognosis. A review of literature reveals partial-to-complete resolution of symptoms with methylprednisolone.[8,9] In a case reported by Larik et al.,[4] the patient showed improvement after treatment with intravenous immunoglobulins. However, our patient did not show any improvement except for relief of backache after pulse therapy of methylprednisolone.
Further, our patient revealed SAH. Hemorrhagic complications are a common occurrence in DHF characterized by leakage of plasma and thrombocytopenia. Bleeding in the absence of DHF has been sparingly reported in dengue and has been called dengue fever with hemorrhage (DF hem).[5] DF hem may be associated with transient thrombocytopenia. Patey et al.[10] and Jensenius et al.[5] described SAH in dengue fever with transient thrombocytopenia. The cause of bleeding is postulated to be activation of platelets.[5]
CONCLUSION
Transverse myelitis is a rare neurologic manifestation of dengue infection; LETM in dengue is even rarer. It is vital that clinicians look for this arbovirus as a cause of LETM or other inflammatory neurologic manifestations in patients residing in dengue prevalent zones. Early recognition of this treatable entity, in both para- and post-infectious phases, can help reduce morbidity. Further, it should be borne in mind that hemorrhagic complications such as SAH may occur in dengue fever in the absence of features of DHF.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Solomon T, Dung NM, Vaughn DW, Kneen R, Thao LT, Raengsakulrach B, et al. Neurological manifestations of dengue infection. Lancet. 2000;355:1053–9. doi: 10.1016/S0140-6736(00)02036-5. [DOI] [PubMed] [Google Scholar]
- 2.Halstead SB. Dengue. Lancet. 2007;370:1644–52. doi: 10.1016/S0140-6736(07)61687-0. [DOI] [PubMed] [Google Scholar]
- 3.Murthy JM. Neurological complication of dengue infection. Neurol India. 2010;58:581–4. doi: 10.4103/0028-3886.68654. [DOI] [PubMed] [Google Scholar]
- 4.Larik A, Chiong Y, Lee LC, Ng YS. Longitudinally extensive transverse myelitis associated with dengue fever. BMJ Case Rep 2012. 2012:pii: bcr1220115378. doi: 10.1136/bcr.12.2011.5378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jensenius M, Berild D, Ormaasen V, Maehlen J, Lindegren G, Falk KI, et al. Fatal subarachnoidal haemorrhage in a Norwegian traveller with dengue virus infection. Scand J Infect Dis. 2007;39:272–4. doi: 10.1080/00365540600891307. [DOI] [PubMed] [Google Scholar]
- 6.Leão RN, Oikawa T, Rosa ES, Yamaki JT, Rodrigues SG, Vasconcelos HB, et al. Isolation of dengue 2 virus from a patient with central nervous system involvement (transverse myelitis) Rev Soc Bras Med Trop. 2002;35:401–4. doi: 10.1590/s0037-86822002000400018. [DOI] [PubMed] [Google Scholar]
- 7.Renganathan A, Keong W, Tin Tan C. Transverse myelitis in association with dengue infection. Neurol Asia. 1996;1:61–3. [Google Scholar]
- 8.de Sousa AM, Alvarenga MP, Alvarenga RM. A cluster of transverse myelitis following dengue virus infection in the Brazilian Aamazon region. Trop Med Health. 2014;42:115–20. doi: 10.2149/tmh.2014-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Seet RC, Lim EC, Wilder-Smith EP. Acute transverse myelitis following dengue virus infection. J Clin Virol. 2006;35:310–2. doi: 10.1016/j.jcv.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 10.Patey O, Ollivaud L, Breuil J, Lafaix C. Unusual neurologic manifestations occurring during dengue fever infection. Am J Trop Med Hyg. 1993;48:793–802. doi: 10.4269/ajtmh.1993.48.793. [DOI] [PubMed] [Google Scholar]


