Abstract
Valgus extension overload syndrome (VEO) is the result of supraphysiologic stresses placed across the posterior elbow during pitching. Following failure of nonoperative measures, surgical options consist of arthroscopic or limited incision posteromedial decompression. Although technically challenging, arthroscopic treatment offers many advantages over open treatment, including improved joint visualization, decreased soft-tissue dissection, decreased postoperative pain, and quicker rehabilitation. Arthroscopic treatment of VEO consists of soft tissue and bony debridement, loose body removal, and osteophyte resection. This technique report details the steps of arthroscopic treatment of VEO in a patient with a subluxating ulnar nerve.
The supraphysiologic demands of pitching generate tensile stresses across the medial elbow. Over time, such repetitive stresses will compromise the integrity of the medial ulnar collateral ligament and lead to valgus instability. Valgus instability will trigger a cascade of pathology affecting the other compartments of the elbow.1 On the posterior side, shear stresses between the medial olecranon tip and olecranon fossa will lead to osteophytes and loose bodies, culminating in valgus extension overload syndrome (VEO).2, 3 Overhead athletes with VEO have a painful throwing motion and decreased throwing velocity. First-line treatment for VEO is nonoperative: rest from throwing, non-steroidal anti-inflammatory drugs, intra-articular steroid injections, assessment of pitching mechanics, and so on.
Following failure of nonoperative measures, surgical options include arthroscopic olecranon debridement or limited incision decompression. Among the benefits of arthroscopic (over open) treatment are limited morbidity to soft tissues and a more complete diagnostic evaluation of the elbow.4, 5, 6 The purpose of this technique is to describe the arthroscopic treatment of VEO in a patient with a subluxating ulnar nerve (Video 1).
Surgical Technique
Anesthesia and Patient Positioning
A preoperative elbow exam should be done on the day of surgery. Specifically, assessment should be done for a subluxating ulnar nerve. In addition, the resting position of the ulnar nerve relative to the medial epicondyle should be noted as this information can impact portal selection. General anesthesia is administered; regional anesthesia is avoided so that a complete neurologic exam can be performed immediately postoperatively. The patient is positioned in the lateral decubitus position on a bean bag. The nonoperative upper extremity is forward flexed, externally rotated, and placed on a padded arm board. A padded roll is placed under the patient's contralateral axilla, positioned between the patient and operating room table. The contralateral lower extremity is flexed slightly at the knee with all bony prominences padded and the peroneal nerve around the fibular neck unencumbered. The operative extremity is draped over an elbow arm holder such that the forearm is perpendicular to the floor. Prior to prepping and draping, the extremity is ranged through simulated operative positions to ensure no obstructions are present (Fig 1).
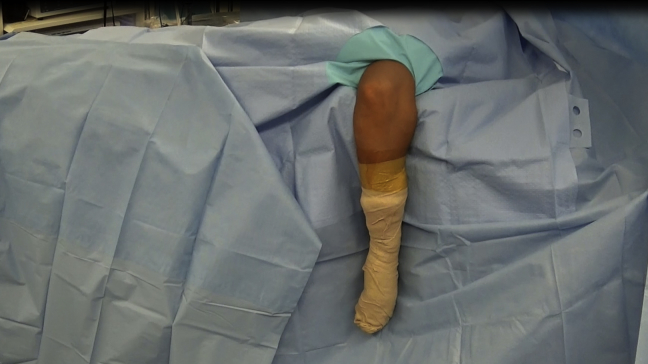
Fig 1.
The patient is placed in the lateral decubitus position with the right arm draped over an elbow arm holder such that the forearm is perpendicular to the floor. Although not visualized below the drapes in this figure, the nonoperative upper extremity is forward flexed, externally rotated, and placed on a padded arm board with a padded roll placed under the axilla. In addition, the contralateral lower extremity rests on the operating table, flexed slightly at the knee with all bony prominences padded and the peroneal nerve around the fibular neck unencumbered. Prior to prepping and draping, the surgeon must verify that adequate space is available to range the elbow as needed and to pass instruments. In addition, an exam under anesthesia is performed to confirm passive range of motion of the elbow.
Diagnostic Arthroscopy
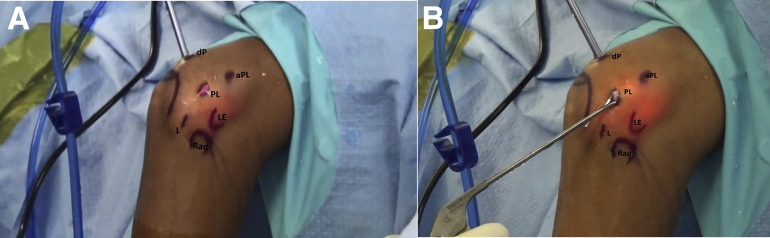
After draping, all relevant surface anatomy is marked, including bony landmarks, location of the fractured olecranon osteophyte, and potential portals to be used (Fig 2). One to two milligrams of 1% lidocaine with epinephrine is injected into each portal site for local anesthesia and local hemostasis. The markings are covered with a sponge, an Esmarch bandage is applied, and the extremity is exsanguinated. The elbow joint is insufflated with 15 mg of normal saline through the lateral soft spot portal formed between the lateral epicondyle, radial head, and olecranon.
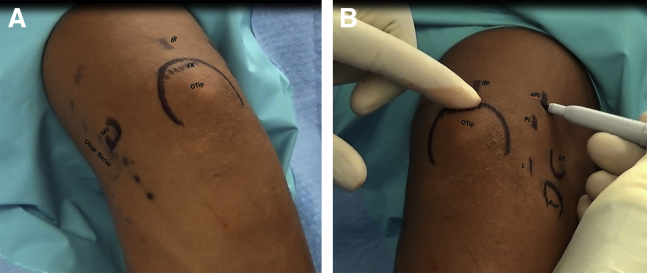
Fig 2.
(A) The bony and soft-tissue landmarks as well as potential portals to be used are marked after positioning in a lateral decubitus position and draping with the right arm bent over an arm holder. The view in the image is of the posteromedial elbow. Based on review of the preoperative imaging and palpation of anatomical landmarks, the location of the ulnar nerve with respect to the medial epicondyle (ME), the olecranon tip (OTip), and the associated fractured olecranon osteophyte (FX) are marked. Portals marked are the direct posterior (dP) portal 2 cm proximal to the olecranon tip, in the midline of the triceps tendon. The top of the photo is toward the shoulder, and the bottom edge of the photo is toward the hand, medial is to the left, and lateral is toward the right. (B) In a similar manner, on the posterolateral side of the right elbow, the relevant bony landmarks and potential portals are marked including the olecranon tip (OTip), lateral epicondyle (LE), and radial head (Rad). Potential portals to be used are the direct lateral (L) portal, which is the “soft spot” formed between the LE, Rad, and olecranon, the posterolateral (PL) portal approximately 1.5 cm from the proximal edge of the olecranon just lateral to the triceps tendon, and the accessory posterolateral (aPL) portal approximately 1.5 cm proximal to the LE and 1 cm anterior to the lateral intermuscular septum. This image is taken from the viewpoint of the surgeon looking down onto the posterior aspect of the elbow with the patient in the lateral decubitus position; the top of the photo is toward the shoulder, and the bottom of the photo is toward the hand, with lateral facing right and medial facing left.
Typically, our preference is to perform a diagnostic arthroscopy beginning in the anterior compartment. A proximal anteromedial portal would be created by incising only the skin within an 11-blade scalpel; a straight blunt clamp would be used to spread soft tissues down to capsule to avoid trauma to the medial antebrachial cutaneous nerve. A blunt trocar within an arthroscopic sheath is inserted with a trajectory toward the radiocapitellar joint; entry into the joint is confirmed by efflux of saline fluid. A standard 4.0-mm, 30° viewing arthroscope (Smith and Nephew, Andover, MA) is inserted. Specific anterior pathology to be evaluated in a patient with VEO would be osteochondral lesions and/or loose bodies involving the radiocapitellar joint, osteophytes of the coronoid tip and fossa, and chondral lesions of the trochlea. An 18-gauge spinal needle may be placed under direct visualization through the proximal anterolateral portal located 1 to 2 cm proximal to the lateral epicondyle and 1 cm anterior to the lateral intermuscular septum; the spinal needle serves as outflow to minimize intra-articular fluid pressures. If debridement within the anterior compartment is necessary, the spinal needle is removed and a formal skin incision is made for the proximal anterolateral portal. A series of sequentially larger dilators (Elbow Arthroscopy Set, Arthrex, Naples, FL) is inserted to expand the portal and facilitate passage of an arthroscopic probe, grasper, or shaver as needed. In the case illustrated (Video 1), a diagnostic arthroscopy of the anterior compartment was not indicated given symptoms, physical examination findings, and imaging localizing pathology to the posterior compartment only. Furthermore, the presence of a subluxating ulnar nerve lying anterior to the medial epicondyle makes anterior compartment arthroscopy risk prohibitive. Finally, although this patient had a subluxating ulnar nerve, he did not have symptoms or exam findings suggestive of an ulnar neuritis; therefore, concurrent ulnar nerve transposition was not indicated.
We proceeded with a posterior compartment arthroscopy. A posterolateral (PL) portal, located along the lateral border of the triceps tendon and 1 cm proximal to the olecranon tip, is established by incising skin and then bluntly spreading soft tissue down to capsule. A blunt trocar within an arthroscopic sheath is inserted with a trajectory toward the articulation of the olecranon. Although overgrowth of the olecranon tip can be appreciated, fibrous tissue overlying the olecranon fossa obscures complete visualization of the olecranon. The lateral gutter is inspected for loose bodies, and the radiocapitellar joint is visualized for articular cartilage damage. Next, a direct posterior (dP) portal is created 2 cm proximal to the olecranon tip, in the midline of the triceps tendon. An 18-gauge spinal needle is inserted at the site of portal creation and triangulated arthroscopically to confirm adequate localization. The dP portal is established by using an 11-blade scalpel to first incise skin only and subsequently penetrate deeper to incise the full thickness of the triceps tendon.
Posterior Compartment Debridement
With the PL portal being used as a visualization portal, an arthroscopic shaver (Smith and Nephew) is inserted into the dP portal. Fibrous tissue overlying the olecranon fossa and tip is debrided (Fig 3A). An arthroscopic electrocautery ablation device may also be used for debridement (Smith and Nephew; Fig 3B). When using a shaver, cautery, or suction device in the posteromedial gutter, consideration must be given to the ulnar nerve located immediately superficial to the capsule; an arthroscopic retractor placed through an accessory PL portal can elevate the capsule and nerve away from the working space. In this case, the ulnar nerve was subluxed anteriorly and therefore protected by the medial epicondyle. The goal of the debridement is to visualize the demarcation between olecranon osteophyte/loose body and normal olecranon bone. Irregular protrusions or “bumps” around the periphery of the olecranon tip suggest encased loose bodies.
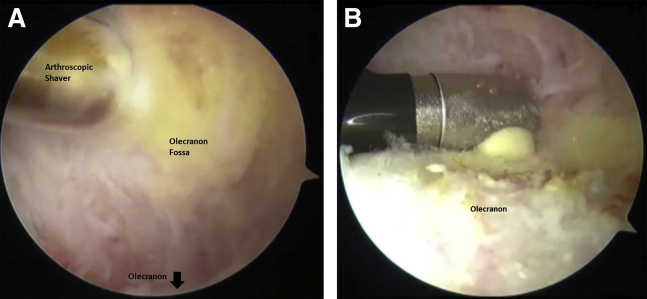
Fig 3.
(A) After completion of a diagnostic arthroscopy of the posterior compartment, the direct posterior (dP) portal is established in the right upper extremity under direct visualization following placement of an 18-gauge spinal needle and triangulation. To enhance visualization, the fibrous tissue in the olecranon fossa is debrided with an arthroscopic shaver by using the posterolateral (PL) portal for viewing and the dP portal for instrument passage. In the image, the contour of the olecranon fossa and the demarcation of the olecranon osteophyte are obscured by excessive overlying fibrous tissue. The image orientation is that proximal (i.e., humeral side) is toward the top of the image, distal (i.e., olecranon side) to the bottom, medial to the left, and lateral to the right. (B) For further debridement, an arthroscopic ablation device is used to debride soft tissue to expose the posterior surface of the olecranon by using the PL portal for viewing and the dP portal for instrument passage. The goal is to expose irregularities in the surface contour of the olecranon suggestive of an osteophyte, encased loose body, and/or fractured olecranon tip. The image orientation is that proximal (i.e., humeral side) is toward the top of the image, distal (i.e., olecranon side) is toward the bottom, medial is toward the left, and lateral is toward the right.
A Freer elevator is inserted through the dP portal to probe for a plane between the loose body and normal olecranon (Fig 4A). For fractured osteophytes or encased loose bodies that would be difficult to extract through a portal incision, the Freer elevator should dislodge but not completely detach the bony fragment. By maintaining some fibrous attachments, the fractured osteophyte can remain in a relatively fixed position while a motorized shaver is used to debride it down in size (Fig 4B). Once the bony fragment is of sufficient size to be delivered from a portal incision, either a motorized shaver, ablation device, and/or Freer elevator can be used to free it of any and all fibrous attachments (Fig 4 C and D). To facilitate delivery of the osteophyte from the elbow joint, the arthroscope should be inserted into the dP portal and an arthroscopic grasper should be placed in the PL portal to retrieve the bony fragment (Fig 5 A and B). Delivering bony fragments through the PL portal is easier than through the dP portal because there are fewer layers of soft tissue between the elbow joint and skin to traverse. For example, when retrieving through a dP portal, a large bony fragment would need to maneuvered through the triceps tendon.
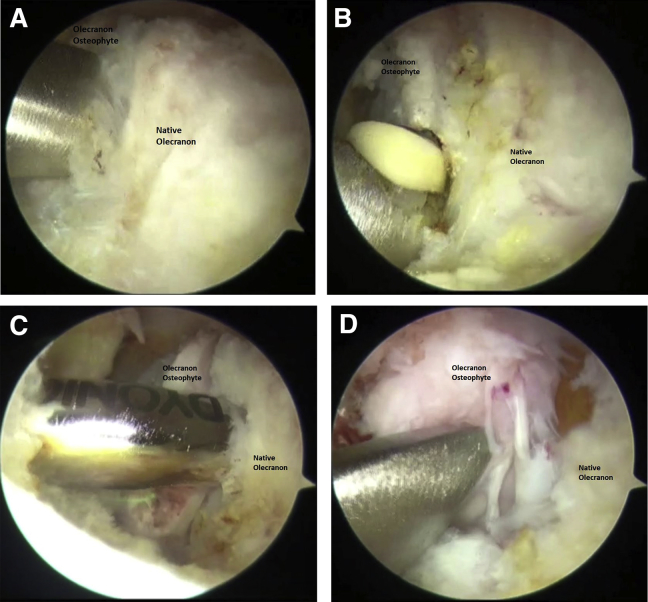
Fig 4.
(A) Using the posterolateral (PL) portal in the right upper extremity for viewing and the direct posterior (dP) portal for instrument passage, a Freer elevator is used to probe for the plane between the fractured olecranon osteophyte and the native olecranon. The Freer elevator is used to separate the fractured osteophyte from the native olecranon but not necessarily completely detach the osteophyte. Some fibrous attachments between the osteophyte and native olecranon should be left in place to assist in stabilization for further debridement. The image orientation is that proximal (i.e., toward the humeral side) is toward the top of the image, distal (i.e., toward the olecranon side) to the bottom, medial to the left, lateral to the right, and the Freer elevator is separating osteophyte on the left side from native olecranon on the right side. (B) Using the PL portal for viewing and the dP portal for instrument passage, an electrocautery ablation device can be used for further debridement of the soft tissue encasing and attaching the fractured osteophyte. Again, the image orientation is that proximal (i.e., toward the humeral side) is toward the top of the image, distal (i.e., toward the olecranon side) toward the bottom, medial toward the left, lateral toward the right, and the ablation device is separating osteophyte on the left side from native olecranon on the right side. (C) Using the PL portal for viewing and the dP portal for instrument passage, an arthroscopic motorized shaver can be used to debride surrounding soft tissue as well as debride the margins of the osteophyte to reduce its size. Reducing the size of the fractured osteophyte will assist in its eventual extraction. The image orientation is that proximal (i.e., toward the humeral side) is toward the top of the image, distal (i.e., toward the olecranon side) to the bottom, medial to the left (with the posterior aspect of the medial gutter being visualized toward the far left), lateral to the right, and the motorized shaver is separating osteophyte on the left side from native olecranon on the right side. (D) Using the PL portal for viewing and the dP portal for instrument passage, the osteophyte has been adequately freed of its attachments and is now ready for extraction from the elbow. A few fibrous attachments between the osteophyte and native olecranon are intentionally maintained to prevent escape of the osteophyte and transformation into a loose body. The image orientation is that proximal (i.e., toward the humeral side) is toward the top of the image, distal (i.e., toward olecranon side) to the bottom, medial to the left, lateral to the right, and the Freer elevator is separating osteophyte on the left side from native olecranon on the right side.
Fig 5.
(A) To facilitate delivery of the osteophyte from the elbow joint, the arthroscope should be inserted into the dP portal and an 11-blade should be used to extend the length of the PL portal incision. This image is taken from the viewpoint of the surgeon looking down onto the posterolateral aspect of the right elbow with the patient in the lateral decubitus position; the top of the photo is perpendicular to the posterior elbow, and the bottom of the photo is perpendicular to the longitudinal axis of the forearm/hand, with the right side of the photo toward the patient's head, and the left side of the photo toward the patient's torso. (B) To retrieve the osteophyte, the dP portal is used for visualization and an arthroscopic grasper is placed in the PL portal to retrieve the bony fragment. Delivering bony fragments through the PL portal is easier than through the dP portal because there are fewer layers of soft tissue to traverse between the elbow joint and skin (lateral epicondyle [LE], and radial head [Rad], direct lateral portal [L], posterolateral portal [PL], and accessory posterolateral portal [aPL]). As before, this image is taken from the viewpoint of the surgeon looking down onto the posterolateral aspect of the elbow with the patient in the lateral decubitus position; the top of the photo is perpendicular to the posterior elbow, the bottom is perpendicular to the longitudinal axis of the forearm, the right side is toward the patient's head, and the left side is toward the patient's torso.
The same process described above is repeated for any other osteophytes or encased loose bodies that may be present. In this case, bony fragments that had fractured from the osteophyte were retrieved with an arthroscopic grasper from the posteromedial gutter and the olecranon was contoured with a motorized shaver. We are very diligent to limit our olecranon resection to osteophyte/loose body removal only, avoiding resection of any normal olecranon bone. Multiple studies have reported that excessive resection of the olecranon during posteromedial decompression increases tensile forces across the medial ulnar collateral ligament during valgus stress and thus increases valgus instability.7, 8 If posterior impingement is present even after resecting all olecranon osteophytes, then inspect the humeral side for osteophytes and resect accordingly.9
Postoperative Protocol
All portal incisions are closed with 4-0 nylon sutures in a simple, interrupted manner. A soft compressive dressing is applied. In the postoperative recovery room, an upper extremity neurologic exam is done to assess for nerve injury. The patient is discharged home the same day with instructions to immediately start physical therapy to actively range the elbow. At the 2-week postoperative visit, sutures are removed and physical therapy is progressed to include flexor-pronator strengthening. At 6 weeks following surgery, a supervised throwing program is begun. The patient can expect to return to competitive throwing at 3 to 4 months postoperatively.
Discussion
VEO is the most common elbow pathology requiring surgical intervention in baseball players as well as other elite athletes requiring overhead throwing.10, 11 Arthroscopic treatment of this syndrome consists of posteromedial elbow decompression with resection of olecranon osteophytes and removal of loose bodies. Although no singular study has specifically evaluated the outcomes of arthroscopic treatment of VEO, many studies have reported outcomes on open and/or arthroscopic treatment of posterior elbow impingement in athletes.3, 10, 11, 12 Reddy et al.11 reported on 187 arthroscopic elbow procedures with the most common diagnoses being posterior impingement (51%), loose bodies (22%), and degenerative joint disease (22%). Eighty-seven percent of patients reported good to excellent outcomes, and 85% of baseball players were able to return to their preinjury level of competition.11
Among the benefits of arthroscopic treatment of VEO over limited incision decompression are improved joint visualization, decreased soft-tissue dissection, decreased postoperative pain, and quicker rehabilitation.4, 5, 6 Among the risks of arthroscopic treatment are injury to major neurovascular structures during portal creation and iatrogenic valgus instability during aggressive resection of olecranon osteophytes.4, 5, 6 The pearls and pitfalls of our surgical procedure are outlined in Table 1.
Table 1.
Pearls and Pitfalls of Arthroscopic Treatment of Valgus Extension Overload
| Pearls and Pitfalls |
|---|
| • Preoperative upper extremity neurologic exam must be done to document subluxation of ulnar nerve and its resting position. |
| • Correlate patient symptoms, exam, and imaging findings to site of operative pathology. |
| • Simulation of elbow movements and instrument passage required during surgery should be done prior to prepping and draping to minimize positioning issues during the case. |
| • Suction should be avoided in the posteromedial gutter to minimize risk of injury to the adjacent ulnar nerve. |
| • Use a blunt instrument such as a Freer elevator to develop a plane to dislodge encased loose bodies. |
| • Extricate large loose bodies or osteophytes through the posterolateral portal. |
| • Do not resect native olecranon bone. |
| • If posterior impingement persists following olecranon osteophyte resection, then search for other sources of impingement: osteophytes on humeral side, loose bodies in posterior radiocapitellar joint. |
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
An overhead throwing athlete is diagnosed with valgus extension overload syndrome in the setting of a fractured olecranon osteophyte and an asymptomatic subluxating ulnar nerve. Plain x-rays and computed tomography scan images show a fractured osteophyte at the level of the proximal olecranon. The patient is indicated for surgical treatment with elbow arthroscopy, administered general anesthesia, and placed in the lateral decubitus position with the operative upper right extremity supported by an elbow arm holder. Prior to prepping and draping, the operative elbow is ranged through simulated intraoperative positions to ensure that no obstructions are present. After prepping and draping the operative extremity in standard sterile fashion, bony and soft-tissue landmarks as well as potential portals to be used are marked on the radial and ulnar sides of the elbow. A diagnostic arthroscopy of the elbow is initiated. Although our preference is to begin with an anterior compartment diagnostic arthroscopy, the presence of a subluxating ulnar nerve lying anterior to the medial epicondyle makes anterior compartment arthroscopy risk prohibitive. Given the exclusive presence of posterior compartment pathology, we proceeded with a posterior compartment diagnostic arthroscopy. The posterolateral portal is established first and then a direct posterior portal is established via triangulation. With the posterolateral portal being used for visualization and the direct posterior portal for instrumentation, debridement of the olecranon osteophyte begins by identifying the plane between the osteophyte and the native olecranon. A Freer elevator inserted through the direct posterior portal is used to probe the plane between the osteophyte and native olecranon and partially mobilize the osteophyte. Subsequently, a motorized shaver and ablation device are used to methodically free the osteophyte of fibrous attachments. To facilitate extraction of the osteophyte from the elbow joint, the direct posterior portal is used for visualization and the posterolateral portal for instrumentation and delivery. The posterolateral portal is preferred for delivery of the osteophyte as there is concern for the osteophyte becoming entrapped within the layers of the triceps tendon if extracted through the direct posterior portal.
References
- 1.Paulino F.E., Villacis D.C., Ahmad C.S. Valgus extension overload in baseball players. Am J Orthop (Belle Mead NJ) 2016;45:144–151. [PubMed] [Google Scholar]
- 2.Fleisig G.S., Barrentine S.W., Escamilla R.F., Andrews J.R. Biomechanics of overhand throwing with implications for injuries. Sports Med. 1996;21:421–437. doi: 10.2165/00007256-199621060-00004. [DOI] [PubMed] [Google Scholar]
- 3.Wilson F.D., Andrews J.R., Blackburn T.A., McCluskey G. Valgus extension overload in the pitching elbow. Am J Sports Med. 1983;11:83–88. doi: 10.1177/036354658301100206. [DOI] [PubMed] [Google Scholar]
- 4.Kelly E.W., Morrey B.F., O'Driscoll S.W. Complications of elbow arthroscopy. J Bone Joint Surg Am. 2001;83:25–34. doi: 10.2106/00004623-200101000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Nelson G.N., Wu T., Galatz L.M., Yamaguchi K., Keener J.D. Elbow arthroscopy: Early complications and associated risk factors. J Shoulder Elbow Surg. 2014;23:273–278. doi: 10.1016/j.jse.2013.09.026. [DOI] [PubMed] [Google Scholar]
- 6.O'Driscoll S.W., Morrey B.F. Arthroscopy of the elbow. Diagnostic and therapeutic benefits and hazards. J Bone Joint Surg Am. 1992;74:84–94. [PubMed] [Google Scholar]
- 7.Kamineni S., Hirahara H., Pomianowski S. Partial posteromedial olecranon resection: A kinematic study. J Bone Joint Surg Am. 2003;85:1005–1011. doi: 10.2106/00004623-200306000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Kamineni S., ElAttrache N.S., O'Driscoll S.W. Medial collateral ligament strain with partial posteromedial olecranon resection. A biomechanical study. J Bone Joint Surg Am. 2004;86:2424–2430. doi: 10.2106/00004623-200411000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Byram I.R., Kim H.M., Levine W.N., Ahmad C.S. Elbow arthroscopic surgery update for sports medicine conditions. Am J Sports Med. 2013;41:2191–2202. doi: 10.1177/0363546513482106. [DOI] [PubMed] [Google Scholar]
- 10.Andrews J.R., Timmerman L.A. Outcome of elbow surgery in professional baseball players. Am J Sports Med. 1995;23:407–413. doi: 10.1177/036354659502300406. [DOI] [PubMed] [Google Scholar]
- 11.Reddy A.S., Kvitne R.S., Yocum L.A., Elattrache N.S., Glousman R.E., Jobe F.W. Arthroscopy of the elbow: A long-term clinical review. Arthroscopy. 2000;16:588–594. doi: 10.1053/jars.2000.8953. [DOI] [PubMed] [Google Scholar]
- 12.Andrews J.R., Carson W.G. Arthroscopy of the elbow. Arthroscopy. 1985;1:97–107. doi: 10.1016/s0749-8063(85)80038-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
An overhead throwing athlete is diagnosed with valgus extension overload syndrome in the setting of a fractured olecranon osteophyte and an asymptomatic subluxating ulnar nerve. Plain x-rays and computed tomography scan images show a fractured osteophyte at the level of the proximal olecranon. The patient is indicated for surgical treatment with elbow arthroscopy, administered general anesthesia, and placed in the lateral decubitus position with the operative upper right extremity supported by an elbow arm holder. Prior to prepping and draping, the operative elbow is ranged through simulated intraoperative positions to ensure that no obstructions are present. After prepping and draping the operative extremity in standard sterile fashion, bony and soft-tissue landmarks as well as potential portals to be used are marked on the radial and ulnar sides of the elbow. A diagnostic arthroscopy of the elbow is initiated. Although our preference is to begin with an anterior compartment diagnostic arthroscopy, the presence of a subluxating ulnar nerve lying anterior to the medial epicondyle makes anterior compartment arthroscopy risk prohibitive. Given the exclusive presence of posterior compartment pathology, we proceeded with a posterior compartment diagnostic arthroscopy. The posterolateral portal is established first and then a direct posterior portal is established via triangulation. With the posterolateral portal being used for visualization and the direct posterior portal for instrumentation, debridement of the olecranon osteophyte begins by identifying the plane between the osteophyte and the native olecranon. A Freer elevator inserted through the direct posterior portal is used to probe the plane between the osteophyte and native olecranon and partially mobilize the osteophyte. Subsequently, a motorized shaver and ablation device are used to methodically free the osteophyte of fibrous attachments. To facilitate extraction of the osteophyte from the elbow joint, the direct posterior portal is used for visualization and the posterolateral portal for instrumentation and delivery. The posterolateral portal is preferred for delivery of the osteophyte as there is concern for the osteophyte becoming entrapped within the layers of the triceps tendon if extracted through the direct posterior portal.