Abstract
Objective
To report voice outcome measures after injection laryngoplasty using the transnasal or transoral flexible endoscopic technique.
Methods
A retrospective review of all patients who underwent flexible endoscopic injection laryngoplasty between June 2010 and August 2016 was carried out. Only those patients who had pre- and post-injection voice outcome measures recorded were included. Voice outcome measures recorded included perceptual voice evaluation using GRBAS, Voice Handicap Index-10 (VHI-10), maximum phonation time (MPT) and closed quotient (CQ) before and after treatment.
Results
Forty-six patients were identified, of which 32 had pre- and post-injection voice outcome measures recorded. There were 19 males and 13 females. The mean age was 56.97 years (range 20–86 years) and the most common indication was unilateral vocal fold paralysis. Thirteen patients had a transnasal flexible endoscopic injection), while 19 patients were injected transorally. Following injection laryngoplasty, there was significant improvement in the mean grade of dysphonia (2.81 vs. 1.22, P < 0.01, roughness (2.44 vs. 1.34, P < 0.01), breathiness (2.72 vs. 1.13, P < 0.01), asthenia (2.78 vs. 1.06, P < 0.01), and strain (2.44 vs. 1.19, P < 0.01), MPT (3.85 s vs. 9.85 s, P < 0.01) and mean CQ (0.19 vs. 0.46, P < 0.01). There was also a decrease in the mean VHI-10 score (33.31 vs. 7.94, P < 0.01).
Conclusion
s: Patients achieved significant improvement in both subjective and objective voice measures after flexible endoscopic injection laryngoplasty via the nasal or transoral route. Voice outcomes were comparable to those reported for other approaches. This technique provides an alternative approach for the management of patients with vocal fold paralysis or glottal insufficiency.
Keywords: Injection, Laryngoplasty, Transnasal, Transoral, Flexible endoscopic, Vocal fold paralysis
Introduction
Injection laryngoplasty was initially described by Bruening in 1908 for the treatment of unilateral vocal fold paralysis.1 Since its inception, the indications for this technique have increased to include other etiologies of glottal insufficiency including vocal fold bowing, atrophy and paresis. With the goal of restoring the normal phonatory position of the vocal fold, various injection techniques have been described based on the clinical presentation and etiology of the glottal insufficiency. Both anatomic and technical considerations have been thoroughly discussed in the literature with emphasis on needle position and the type and amount of filler material used. In patients with unilateral vocal fold paralysis and an intact vibratory surface, the needle is usually inserted lateral to the vocal process, whereas in patients with vocal fold scarring or where there is tissue loss, the injection is usually placed more anterior and medial to restore the vibratory margin of the vocal fold.2
With the widespread performance of injection laryngoplasty in the office setting, various techniques and approaches have been described, all of which have shown promising results with significant improvement in both subjective and objective voice outcome measures.3, 4, 5, 6 The most commonly used approaches are the per-oral and percutaneous routes through the thyroid cartilage, thyrohyoid membrane, or cricothyroid membrane. The choice of approach is primarily determined by the surgeon's experience and preference, the patient's orofacial and neck anatomy, patient tolerance, and the availability of instrumentation.
Although the transnasal endoscopic approach has been previously reported for steroid injection as an alternative treatment for benign vocal fold lesions, only four articles in the literature have described the technique for vocal fold medialization.7, 8, 9, 10 Trask et al7 reported 20 patients who underwent vocal fold augmentation using a transnasal endoscope which was initially designed for in-office transnasal esophagoscopy. All patients except one tolerated the procedure and adequate medialization was achieved in all cases. In 2015, Hamdan et al9 reported subjective voice outcome measures using the transnasal approach in a group of patients with glottal insufficiency. There was significant subjective voice improvement and a reduction or complete closure of the glottal gap in all patients, though no objective voice measures were reported. More recently the transoral flexible endoscopic injection variation of the technique using the modified Guedel oral airway (Teleflex, Westmeath Ireland) has also been described.
The goal of this study is to report voice outcome measures after injection laryngoplasty using either the transnasal or transoral flexible endoscopic injection technique.
Methods
Subjects
After Institution Review Board approval was obtained, a retrospective chart review of all patients who underwent injection laryngoplasty under local anesthesia through the working channel of a flexible endoscope either transnasally or transorally between June 2010 and August 2016 was conducted. Only patients who had documentation of voice outcome measures before and after the procedure were included in the study. Not all voice outcome measures were recorded for all patients. All patients had perceptual voice evaluation preoperatively and post-operatively.
The patients’ age and gender, indication for injection, material injected, site of injection and amount injected were recorded. Voice outcome measures collected included the Voice Handicap Index-10 (VHI-10)11, perceptual evaluation using the GRBAS grading system12, maximum phonation time, and the closed quotient. The closed quotient was defined as the number of closed frames/the total number of frames (open + closed) on videostroboscopy.13
Technique
With the patient awake in the sitting position, the pharynx was sprayed with 2% lidocaine. The nasal cavity was decongested and anesthetized using pledgets soaked in 1% lidocaine with epinephrine 1:100,000 mixed with oxymetazoline hydrochloride 0.1%. After several minutes, the flexible fiberoptic laryngoscope with a working channel (Karl Storz Model 11001UD1; El Segundo, CA) was introduced through either the nasal cavity or through the modified Guedel oral airway. The transoral approach was used when nasal obstruction would not allow transnasal insertion, or when the patient was on anticoagulants. Four percent lidocaine gel was applied to the dorsum and base of tongue prior to placement of the oral airway. Next, using a 1.8 mm Teflon catheter (BTC Medical Europe Srl, Valeggio sul Mincio, Italy)passed through the working channel, 2 ml of 2% lidocaine were applied above the palate, at the epiglottis and at the vocal folds while the patient is asked to phonate. Once the endolarynx was adequately anesthetized, a 19-gauge flexible endoscopic needle (BTC Medical Europe Srl, Valeggio sul Mincio, Italy) was passed through the working channel of the endoscope and inserted either lateral to the vocal process in cases of unilateral vocal fold paralysis, or in the mid-portion of the vocal fold lateral to the vocal ligament in cases of vocal fold atrophy or volume loss, and hyaluronic acid (Restylane®, Galderma SA Lausanne, Switzerland)injected via a 3 ml syringe. The patient was asked to phonate during the injection until the desired voice outcome was achieved.
Statistics
Means and standard deviations were reported for continuous variables, whereas frequencies and percentages were reported for categorical variables. A paired Student t-test was used to compare means. Results were considered significant at P < 0.05. Data was analyzed using SPSS version 23.0 (SPSS Inc, Chicago, Ill).
Results
Demographic data
Forty-six patients who underwent awake injection laryngoplasty in the office using the flexible endoscope transnasally or transorally were identified. Of these, 32 had documented voice outcome measures before and after the procedure, and met the selection criteria for this study. The mean age was 56.97 years (range 20–86 years). There were 19 males and 13 females. Thirteen patients (41%) were injected using the transnasal route and 19 patients (59%) using the transoral approach. Hyaluronic acid (Restylane® Galderma SA Lausanne, Switzerland) 0.20–0.80 ml (mean = 0.51 ml) was injected. The indication, side of injection, material and amount injected are summarized in Table 1.
Table 1.
Patient information.
| Total subjects | 32 |
|---|---|
| Gender | |
| Male | 19 |
| Female | 13 |
| Diagnosis | |
| Vocal cord paralysis | 27 |
| S/p cordectomy | 3 |
| Vocal fold atrophy/bowing | 2 |
| Material injected | |
| Restylane®a | 32 (39) |
| Side of injection | |
| Right | 8 |
| Left | 17 |
| Bilateral | 7 |
| Age (years)b | 56.97 ± 19.39 (20.00–86.00) |
| Amount injected (ml)b | 0.51 ± 0.17 (0.20–0.80) |
Number of injections.
Mean ± SD (Range).
Voice outcome measures
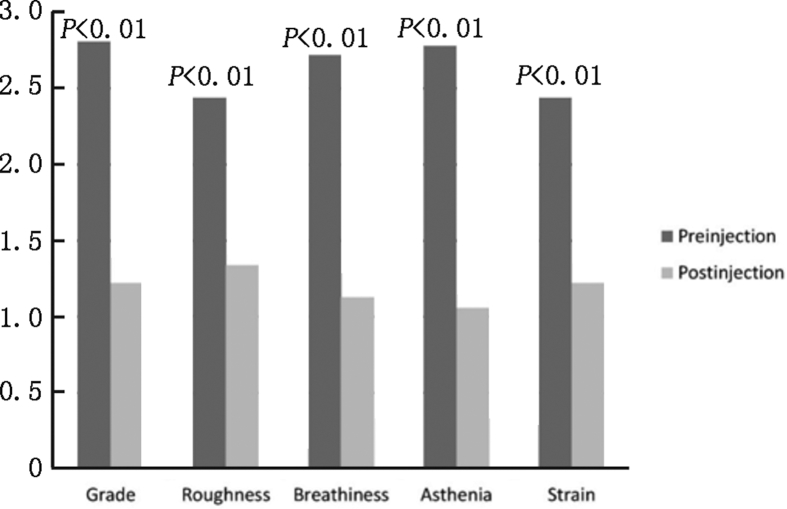
There was a decrease in the Voice Handicap Index-10 after injection for all subjects with a significant difference in the mean before and after injection laryngoplasty for the entire group (33.31 vs. 7.94, P < 0.01). Perceptually, the overall grade of dysphonia decreased from 2.81 to 1.22 (P < 0.01), roughness from 2.44 to 1.34 (P < 0.01), breathiness from 2.72 to 1.13 (P < 0.01), asthenia from 2.78 to 1.06 (P < 0.01), and strain from 2.44 to 1.19 (P < 0.01), see Fig. 1. All patients had a decrease in the grade of dysphonia. Twenty-eight patients (88%) had a decrease in roughness, 29 patients (91%)in breathiness, 30 patients (94%) in asthenia, and 27 patients (84%) in strain. There was a significant increase in the MPT in all subjects with a significant difference in the mean MPT before and after injection (3.85 s vs. 9.85 s, P < 0.01) for the entire group. There was also a significant increase in the closed quotient in 23 out of 24 patients (96%), with a significant difference in the mean before and after (0.19 vs. 0.46, P < 0.01) for the entire group (Table 2).
Fig. 1.
Perceptual evaluation before and after injection laryngoplasty.
Table 2.
Voice outcome measures before and after injection laryngoplasty.
| Voice outcome measures | Mean ± St.dev (Before) | Mean ± St.dev (After) | P-value |
|---|---|---|---|
| Maximum phonation time (s) (n = 20) | 3.85 ± 1.00 | 9.85 ± 2.62 | <0.01 |
| Closed quotient (n = 24) | 0.19 ± 0.15 | 0.46 ± 0.09 | <0.01 |
| Voice Handicap Index-10 (n = 16) | 33.31 ± 3.82 | 7.94 ± 2.84 | <0.01 |
Complications
Three patients (9%) developed inflammatory reactions at the injection site that were treated with systemic steroids and resolved.
Discussion
Numerous reports in the literature have described the transoral and percutaneous approaches for injection laryngoplasty.14, 15, 16, 17 Most of these have reported favorable voice outcomes with few complications. Amin18 has reported the tolerance rate and quality of life survey results in 10 patients who underwent injection laryngoplasty using the thyrohyoid approach. His findings support the usefulness of this approach for vocal fold augmentation. Lee et al19 has similarly reported favorable voice outcomes in patients undergoing injection laryngoplasty percutaneously using Polyacrylomide Hydrogel. In his report of 34 patients, there was significant improvement in the perceptual parameters, acoustic measures, mucosal wave, and glottic closure post-operatively. Chandran et al20 reported the Australian experience of 34 injections performed under either local or general anesthesia with improvement in the VHI-10, all perceptual parameters except asthenia, and a less than 10% complication rate. Barbu et al21 in their investigation on the feasibility of bed side injection laryngoplasty using the transoral approach in the immediate post-operative period have reported advancement in oral intake in 70 percent of patients, thus supporting the importance of early intervention. Mohammed et al22 reported their experience in the UK with 21 patients undergoing injection laryngoplasty using the thyrohyoid approach, and have similarly demonstrated improvement in the VHI-10 score 3 and 6 months after injection. Similar results were reported by other groups also highlighting improvement in the median Voice Performance Questionnaire (VPQ) score and all perceptual vocal parameters following the injection.23
In contrast, there have been few reports describing the flexible endoscopic injection technique for vocal fold augmentation.7, 9, 10 The transnasal flexible endoscopic approach for injection laryngoplasty was initially described in 2005 by Trask et al7 in their report of 20 patients with glottal insufficiency. The procedure was performed in the outpatient clinic setting thus eliminating the additional cost of using the operating room. It was of particular value for those patients with difficult laryngeal exposure or at high risk for general anesthesia.7 In 2015, Hamdan et al9 reported voice outcome measures in 16 patients with glottal insufficiency who underwent transnasal injection laryngoplasty. This included a significant decrease in the mean score for perceptual parameters, and a marked reduction or closure of the glottal gap in all subjects. More recently, the transoral flexible endoscopic injection technique as a variant to the transnasal approach using the same flexible endoscope with a working channel has been described by the same group.10
In the current study, we report the voice outcome measures for injection laryngoplasty using the flexible endoscope passed through the nose or oral cavity. There was significant improvement noted in the mean grade of dysphonia, roughness, breathiness, asthenia and strain. There was also a significant improvement in all other voice outcome measures including VHI-10, MPT and closed quotient. These results are similar with those published for the percutaneous and transoral approaches.
Despite the widespread use of the percutaneous and transoral approaches, a major limitation of these approaches is the need for an assistant to handle the endoscope and allow concurrent visualization of the vocal folds during the injection. In the transoral approach, the patient's gag reflex may lead the procedure to be aborted.14 The cricothyroid approach is limited by difficulty in visualizing the tip of the needle during the procedure.15 In the thyrohyoid approach, access to the most anterior and posterior portion of the vocal folds is often restricted, and insertion of the needle can be further challenged in patients with obscure neck landmarks.24
The flexible endoscopic approaches provide a viable alternative for injection laryngoplasty which obviates the need for an assistant. The flexible endoscopic transoral approach in addition, is particularly useful in cases where nasal anatomy limits scope insertion, or when concurrent anticoagulation increases the risk of iatrogenic epistaxis with the transnasal approach. Constraints of the flexible endoscopic technique include the offset working channel which makes right side injection challenging in some, the additional cost of the endoscopic needle, and the unavoidable loss of injectable material in the long flexible endoscopic needle which can be partially circumvented by injecting saline to flush through the injectate.
Limitations of this study include the relatively small number of patients and the lack of all voice outcome measures for all patients. In addition, no data on patient tolerance of the procedure was available, although no cases were aborted. Nonetheless, this study adds to the growing body of literature on available techniques for awake injection laryngoplasty, their voice outcomes, and as such augments the laryngologist's armamentarium.
Conclusion
The flexible endoscopic approach via the nasal or oral route is a viable option for injection laryngoplasty. Both allow for completion of the procedure without the need of an assistant. The transoral route is useful for patients with narrow nasal passages or who are anticoagulated. Voice outcome measures are comparable to those reported for other approaches. Familiarity with multiple injection approaches empowers the laryngologist managing patients with vocal fold paralysis or glottal insufficiency.
Edited by Jie Gao
Footnotes
Peer review under responsibility of Chinese Medical Association.
References
- 1.Lewy R.B. Experience with vocal cord injection. Ann Otol Rhinol Laryngol. 1976;85:440–450. doi: 10.1177/000348947608500404. [DOI] [PubMed] [Google Scholar]
- 2.Courey M.S. Injection laryngoplasty. Otolaryngol Clin N Am. 2004;37:121–138. doi: 10.1016/j.otc.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 3.Upton D.C., Johnson M., Zelazny S.K., Dailey S.H. Prospective evaluation of office-based injection laryngoplasty with hyaluronic acid gel. Ann Otol Rhinol Laryngol. 2013;122:541–546. doi: 10.1177/000348941312200901. [DOI] [PubMed] [Google Scholar]
- 4.Reiter R., Rudolf R., Brosch S., Sibylle B. Laryngoplasty with hyaluronic acid in patients with unilateral vocal fold paralysis. J Voice. 2012;26:785–791. doi: 10.1016/j.jvoice.2011.11.007. [DOI] [PubMed] [Google Scholar]
- 5.Damrose E.J. Percutaneous injection laryngoplasty in the management of acute vocal fold paralysis. Laryngoscope. 2010;120:1582–1590. doi: 10.1002/lary.21028. [DOI] [PubMed] [Google Scholar]
- 6.Birkent H., Sardesai M., Hu A., Merati A.L. Prospective study of voice outcomes and patient tolerance of in-office percutaneous injection laryngoplasty. Laryngoscope. 2013;123:1759–1762. doi: 10.1002/lary.24010. [DOI] [PubMed] [Google Scholar]
- 7.Trask D.K., Shellenberger D.L., Hoffman H.T. Transnasal, endoscopic vocal fold augmentation. Laryngoscope. 2005;115:2262–2265. doi: 10.1097/01.mlg.0000184316.51516.83. [DOI] [PubMed] [Google Scholar]
- 8.Wang C.T., Lai M.S., Liao L.J., Lo W.C., Cheng P.W. Transnasal endoscopic steroid injection: a practical and effective alternative treatment for benign vocal fold disorders. Laryngoscope. 2013;123:1464–1468. doi: 10.1002/lary.23715. [DOI] [PubMed] [Google Scholar]
- 9.Hamdan A.L., Ziade G., Jaffal H., Skaff G. Transnasal injection laryngoplasty. Ann Otol Rhinol Laryngol. 2015;124:474–479. doi: 10.1177/0003489414567936. [DOI] [PubMed] [Google Scholar]
- 10.Hamdan Al, Rizk M., Ayoub C., Ziade G. Injection laryngoplasty through a transoral approach using the Guedel oral airway. Acta Otorhinolaryngol Ital. 2017;37:444–446. doi: 10.14639/0392-100X-1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rosen C.A., Lee A.S., Osborne J., Zullo T., Murry T. Development and validation of the voice handicap index-10. Laryngoscope. 2004;114:1549–1556. doi: 10.1097/00005537-200409000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Hirano M., editor. Psycho-acoustic Evaluation of Voice: GRBAS Scale for Evaluating the Hoarse Voice. Clinical Examination of Voice. Springer-Verlag; New York: 1981. pp. 81–84. [Google Scholar]
- 13.Carroll T.L., Wu Y.H., McRay M., Gherson S. Frame by frame analysis of glottic insufficiency using laryngovideostroboscopy. J Voice. 2012;26:220–225. doi: 10.1016/j.jvoice.2011.01.008. [DOI] [PubMed] [Google Scholar]
- 14.Andrade F.P.A., Carrau R.L., Buckmire R.A. Safety and cost-effectiveness of intra-office flexible videolaryngoscopy with transoral vocal fold injection in dysphagic patients. Am J Otolaryngol. 2006;27:319–322. doi: 10.1016/j.amjoto.2006.01.009. [DOI] [PubMed] [Google Scholar]
- 15.Jin S.M., Park C.Y., Lee J.K., Ban J.H., Lee S.H., Lee K.C. Transcutaneous injection laryngoplasty through the cricothyroid space in the sitting position: anatomical information and technique. Eur Arch Otorhinolaryngol. 2008;265:313–319. doi: 10.1007/s00405-007-0450-6. [DOI] [PubMed] [Google Scholar]
- 16.Lee S.W., Kim J.W., Koh Y.W., Shim S.S., Son Y.I. Comparative analysis of efficiency of injection laryngoplasty technique for with or without neck treatment patients: a transcartilaginous approach versus the cricothyroid approach. Clin Exp Otorhinolaryngol. 2010;3:37–41. doi: 10.3342/ceo.2010.3.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Getz A.E., Scharf J., Amin M.R. Thyrohyoid approach to cidofovir injection: a case study. J Voice. 2005;19:501–503. doi: 10.1016/j.jvoice.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 18.Amin M.R. Thyrohyoid approach for vocal fold augmentation. Ann Otol Rhinol Laryngol. 2006;115:699–702. doi: 10.1177/000348940611500909. [DOI] [PubMed] [Google Scholar]
- 19.Lee S.W., Son Y.I., Kim C.H., Lee J.Y., Kim S.C., Koh Y.W. Voice outcomes of polyacrylamide hydrogel injection laryngoplasty. Laryngoscope. 2007;117:1871–1875. doi: 10.1097/MLG.0b013e3180caa1b1. [DOI] [PubMed] [Google Scholar]
- 20.Chandran D., Woods C., Ullah S., Ooi E., Athanasiadis T. A comparative study of voice outcomes and complication rates in patients undergoing injection laryngoplasty performed under local versus general anaesthesia: an Adelaide voice specialist's experience. J Laryngol Otol. 2017;131:S41–S46. doi: 10.1017/S0022215116009221. [DOI] [PubMed] [Google Scholar]
- 21.Barbu A.M., Gniady J.P., Vivero R.J., Friedman A.D., Burns J.A. Bedside injection medialization laryngoplasty in immediate postoperative patients. Otolaryngol Head Neck Surg. 2015;153:1007–1012. doi: 10.1177/0194599815601393. [DOI] [PubMed] [Google Scholar]
- 22.Mohammed H., Masterson L., Gendy S., Nassif R. Outpatient-based injection laryngoplasty for the management of unilateral vocal fold paralysis – clinical outcomes from a UK centre. Clin Otolaryngol. 2016;41:341–346. doi: 10.1111/coa.12516. [DOI] [PubMed] [Google Scholar]
- 23.Powell J., Carding P., Birdi R., Wilson J.A. Injection laryngoplasty in the outpatient clinic under local anaesthetic: a case series of sixty-eight patients. Clin Otolaryngol. 2014;39:224–227. doi: 10.1111/coa.12274. [DOI] [PubMed] [Google Scholar]
- 24.Clary M.S., Milam B.M., Courey M.S. Office-based vocal fold injection with the laryngeal introducer technique. Laryngoscope. 2014;124:2114–2117. doi: 10.1002/lary.24659. [DOI] [PubMed] [Google Scholar]