Since the first case report was published by Baur in 1906,1 primary malignant melanoma of the esophagus has been considered an extremely rare cancer. Among esophageal cancers, primary malignant melanoma accounts for 0.1%–0.2% of cases.2 We have used CT and positron emission tomography (PET) scans to evaluate metastasis. According to previous reports, the rate of metastasis is high when the tumor is first diagnosed.3 Use of PET obviously increases the accuracy of staging. Although primary malignant melanoma of the esophagus is now better understood, the 5-year survival rate is dismal and treatment remains challenging.
CASE
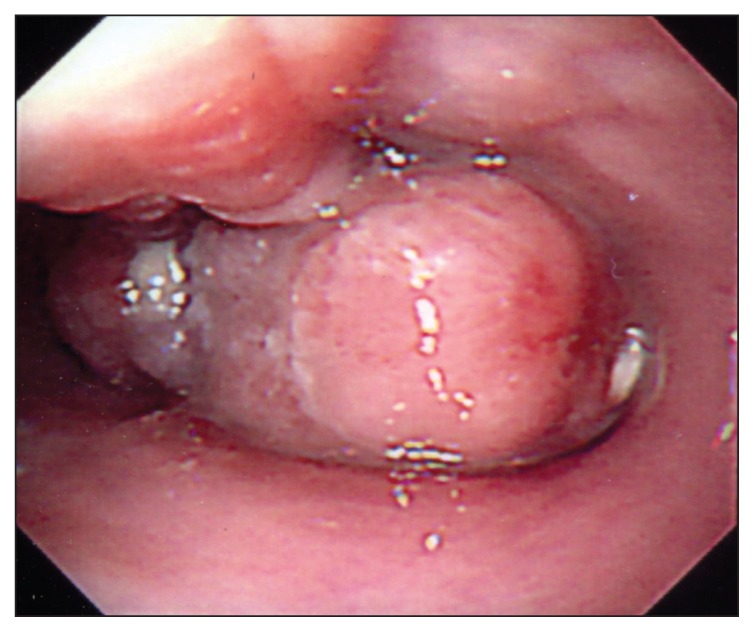
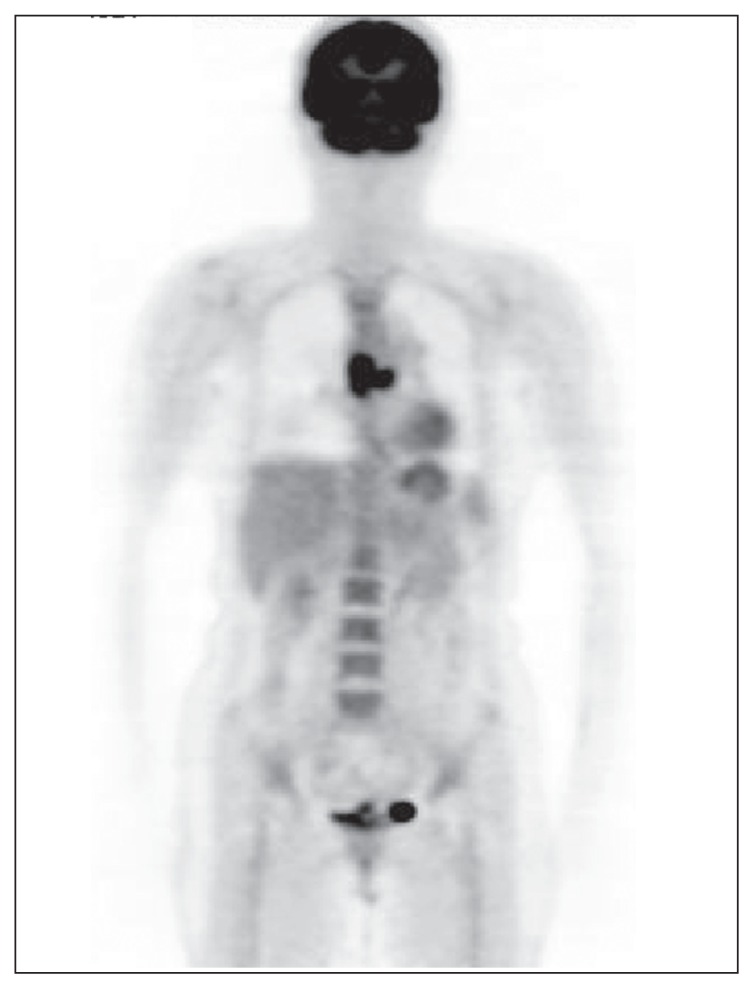
A 40-year-old woman with 3 months of dysphagia, myalgia over the subscapular region on the left side, and body weight loss (9 kg) was diagnosed with primary malignant melanoma of the esophagus by panendoscopy (PES) with biopsy (Figure 1). After the cancer was confirmed, CT, whole body bone scans and PET scans (Figure 2) were used to establish the clinical stage. An upper gastrointestinal (GI) series was also used to assess the axis of the esophagus and the mucosal lesion. The tumor was located about 25 to 30 cm from the incisors with a segmental filling defect and mucosal destruction evident in the upper GI series. Chest CT showed wall thickening and a soft-tissue lesion over the middle third of the esophagus, extending for more than 5 cm. Extratumoral extension and lymph node metastasis were considered. PET scans showed bifocal 2-[18F]-Fluoro-2-deoxy-D-glucose (FDG) uptake about the middle third of the esophagus and increased uptake in the right lower-neck region. Tumor markers including carcinoembryonic antigen and squamous cell carcinoma markers were negative.
Figure 1.
Panendoscopy finding: a fungating mass in the esophagus.
Figure 2.
PET scan image: FDG-avid tumor in the middle third of the esophagus, and another FDG-avid lesion localized in the right neck region, level 4.
The patient received subtotal esophagectomy and lymph node dissection after a series of studies. Reconstruction of the esophagus with a gastric tube (substernal route) with cervical esophagogastrostomy was performed after the first step of the operation. A solid fixed lymph node about 3.5×2 cm was noted and dissected. The resected esophageal specimen was 10.5 cm in length and a fungating mass about 4×3.5×2.5 cm was evident in the specimen (Figure 3). The final pathology report indicated that the mass was a malignant melanoma invading to the submucosal layer and characterized by vesicular hyperchromatic nuclei with prominent eosinophilic nucleoli and frequent mitosis. Immunohistochemical stains for HMB-45 antigen and S-100 protein were positive. The surgical margins were free of tumor invasion, but lymph nodes were noted to contain tumor emboli. We took a biopsy of the cervical lymph node on the basis of the PET findings and, unfortunately, a metastasis was found.
Figure 3.
Operative finding and specimen.
DISCUSSION
Primary malignant melanoma of the esophagus is a rare and aggressive tumor with a poor prognosis. Only 15% of all melanomas are encountered in noncutaneous sites,4 with 0.5% of these arising in the esophagus.5 Primary malignant melanoma of the esophagus was widely accepted after de la Pava et al demonstrated the presence of melanocytes in normal esophageal mucosa in 1963.6 In 1953, Allen and Spitz developed histological criteria for primary esophageal malignant melanoma, which emphasized the presence of junctional epithelial changes in the overlying or juxtaposed epithelium near the tumors.7 No more than 300 cases have been reported worldwide since 1906, most of which were in individual case reports. The symptoms included dysphagia (79.8%), weight loss (37.5%), substernal or epigastric discomfort or pain (33.1%) and melena (7%). Some patients were asymptomatic. The mean duration of symptoms was 3.2 months. It has been shown that esophageal melanocytosis is mostly located in the middle and lower thirds of the esophagus and most of malignant melanomas are located over this area.8 Endoscopic biopsy yields diagnostic specimens only 50% of the time.4 The histopathological diagnosis is not established until after resection is performed.
Despite our growing understanding of this malignant disease, the prognosis of esophageal melanoma remains poor, with a 5-year survival rate after surgery of 4.2%.8 This is most likely because of the advanced state of these tumors at the time of diagnosis, with metastases commonly seen. The common sites of metastases are the liver (31%), the mediastinum and mediastinal lymph nodes (29%), the lung (17.7%) and the brain (13.2%).3 For lymph node metastasis, FDG PET detected 100% of metastases ≥10 mm, 83% of metastases 6–10 mm, and 23% of metastases <5 mm. Moreover, FDG PET has high sensitivity (≥93%) only for metastases with more than 50% lymph node involvement or with capsular infiltration.2 The choice of treatment for this condition is mainly dependent on the patient’s functional status and the presence and extent of metastatic disease at the time of diagnosis.10 Surgical resection with total esophagectomy remains the main component of management, even in cases of recurrence. Although radiotherapy and chemotherapy have not proven to be beneficial, they play a palliative role after surgical consideration.11 Our case demonstrates the importance of PET, which is helpful in finding metastasis to the cervical node. In our opinion, PET should be used in those who are diagnosed with primary malignant melanoma of the esophagus that may increase the accuracy of staging.
REFERENCES
- 1.Baur EH. Ein fall von primärem melanom des oesophagus. Arb Geb Pathol Anat Inst Tübingen. 1906;5:343–354. [Google Scholar]
- 2.Joob AW, Haines GK, 3rd, Kies MS, Shields TW. Primary malignant melanoma of the esophagus. Ann Thorac Surg. 1995;60:217–22. [PubMed] [Google Scholar]
- 3.Chalkiadakis G, Wihlm JM, Morand G, et al. Primary malignant melanoma of the esophagus. Ann Thorac Surg. 1985;39:472–475. doi: 10.1016/s0003-4975(10)61963-7. [DOI] [PubMed] [Google Scholar]
- 4.Mills SE, Cooper PH. Malignant melanoma of the digestive system. Pathol Annu. 1983;18:1–26. [PubMed] [Google Scholar]
- 5.Scotto J, Fraumeni JF, Jr, Lee JAH. Melanomas of the eye and other noncutaneous sites: Epidemiologic aspects. J Nat Cancer Inst. 1976;56:489–491. doi: 10.1093/jnci/56.3.489. [DOI] [PubMed] [Google Scholar]
- 6.de la Pava, Nigogosyan G, Pickven JW, Cabrera A. Melanosis of the esophagus. Cancer. 1963;16:48–50. doi: 10.1002/1097-0142(196301)16:1<48::aid-cncr2820160107>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 7.Allen AC, Spitz S. Malignant melanoma: a clinicopathological analysis of the criteria for diagnosis and prognosis. Cancer. 1953;6:1–45. doi: 10.1002/1097-0142(195301)6:1<1::aid-cncr2820060102>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 8.Dematos P, Wolfe WG, Shea CR, Prieto VG, Seigler HF. Primary malignant melanoma of the esophagus. J Surg Oncol. 1997;66:201–6. doi: 10.1002/(sici)1096-9098(199711)66:3<201::aid-jso9>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 9.Suzuki H, Nagayo T. Primary tumor of the esophagus other than squamous cell carcinoma: histologic classification and statistics in the surgical and autopsied materials in Japan. Int Adv Surg Onc. 1980;3:73. [PubMed] [Google Scholar]
- 10.Jawalekar K, Tretter P. Primary malignant melanoma of the esophagus. J Surg Oncol. 1979;12:19–25. doi: 10.1002/jso.2930120104. [DOI] [PubMed] [Google Scholar]
- 11.Crippa F, Leutner M, Belli F, et al. Which kinds of lymph node metastases can FDG PET detect? A clinical study in melanoma. J Nucl Med. 2000;41:1491–1494. [PubMed] [Google Scholar]