Most basal cell carcinomas (BCC) occur on the sun-exposed skin of the head and neck regions. Arising from the sun-protected areas is uncommon and the nipple is an exceptionally rare primary site. Since the first full description by Robinson,1 only 25 cases have been reported in the literature. 2–5 There is no consensus about the treatment of BCCs of the nipple. Ten to 30 percent of BCCs are superficial and occur most frequently on the trunk and the limbs.6 We report the first case, to our knowledge, of a superficial type BCC in the nipple.
CASE
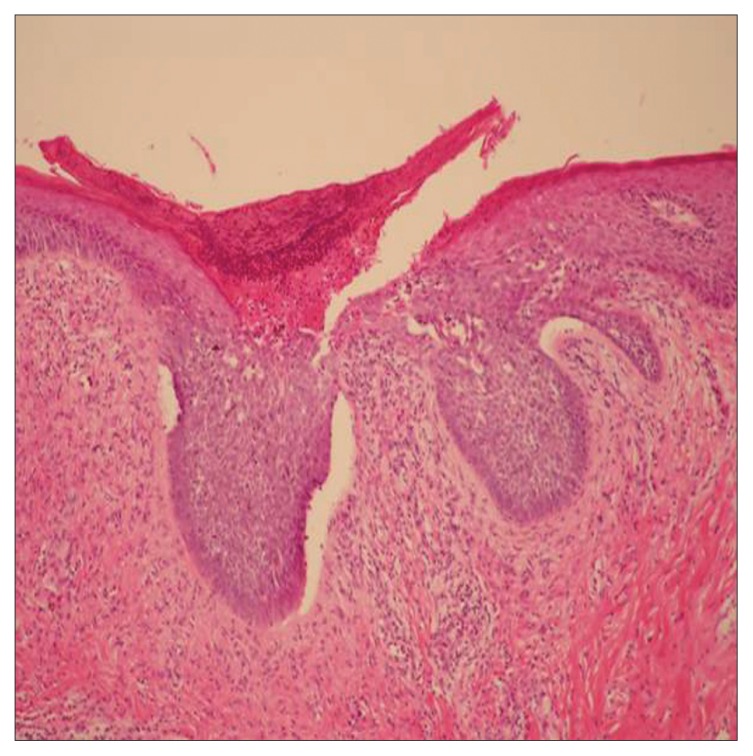
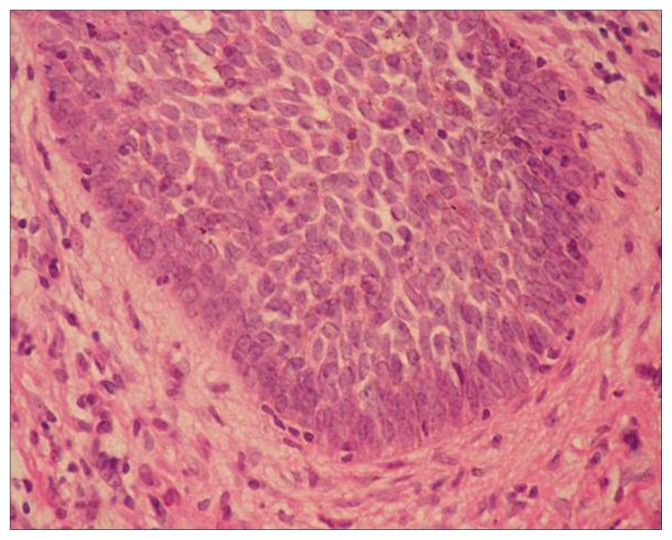
A 74-year-old female was referred for eczematous changes in the right nipple for several months. She also had no history of insult to the right breast. No pruritis, discharge, ulceration, or pain was noted. Physical examination revealed no axillary lymphadenopathy. Paget disease of the nipple was first considered and an excisional biopsy was performed. Gross examination of the surgical specimen disclosed an ellipse of skin that measured 1.6 × 0.9 × 0.9 cm with attached subcutaneous tissue. On light microscopic examination, the tumor consisted of several foci of superficial lobules of basaloid cells arising from the epidermis into the dermis (Figure 1). All these superficial lobules were confined to the papillary dermis. The tumor cells had round-to-oval nuclei with scanty cytoplasm. Characteristic peripheral palisading of the basal cells was also noted (Figure 2). The final diagnosis was superficial BCC. All the resection margins were free. The post operation course was smooth and uneventful. No adjuvant therapy was done.
Figure 1.
Skin of the nipple shows several superficial islands of basaloid cells arising from the epidermis into dermis. Note: all these superficial lobules are confined to the papillary dermis (H&E, ×100).
Figure 2.
Higher magnification demonstrating the characteristic peripheral palisading of basal cells. (H&E, ×400)
DISCUSSION
BCCs arising from the nipple are encountered extremely rarely. Our case was probably the first case of a superficial type BCC reported in the literature. Several variants of BCC have been described, including the superficial type, which occurs mainly on the trunk. Superficial BCC arises as a multifocal proliferation of tumor nests attached to the epidermis, with the characteristic feature of peripheral nuclei palisading.
The exact etiology of BCCs arising from the nipple is still obscure. Of the 25 previously reported cases, 16 were reported in men.2–5 It has been postulated that the male predominance may be due to a higher amount of sun exposure in this area.7 All cases are sporadic and no familial aggregation has been observed.
The clinical appearance of BCCs in the nipple is various and differentiating BCC from Paget disease of the nipple, Bowen disease, or other benign breast disease is considerably hard for the clinician. Microscopic examination is usually diagnostic and straightforward without much difficulty.
Calcification was reported as present in BCCs of the nipple,8 which may cause diagnostic difficulty because calcification in breast cancer is a well-known phenomenon. Therefore, accurate diagnosis can be difficult based solely on radiological observation. A histological examination is required to make the precise diagnosis.
BCC is a locally destructive tumor that is rarely metastatic. Treatment methods include surgical excision with clear margins, local destruction with radiotherapy, cryotherapy, photodynamic therapy, intralesional interferon treatment, fluorouracil, or imiquinod.9 Among the 25 cases reported in the literature, 3 patients had axillary lymph node metastasis. The metastatic rate for primary BCCs in the nipple is 12% (3/25), which is much higher compared to a less than 1% metastatic rate from other common sites for BCCs.10 Due to this increasing rate of metastasis, more aggressive treatment may be needed for the BCCs in the nipple. Wide excision with safe resection margins is required. When axillary lymph nodes are clinically palpable, sentinel lymph node biopsy or axillary lymph node dissection may be considered. Pathologic features of our case revealed a superficial type BCC with a clean resection margin and no obvious axillary lymphadenopathy; therefore, no more aggressive treatment was given but the case was followed up closely.
In conclusion, BCCs of the nipple are an extremely rare neoplasm with more aggressive behavior compared to those that occur outside the nipple. Accurate pathological diagnosis and appropriate treatment modalities with close long-term follow-up are highly recommended in these rarely encountered patients.
REFERENCES
- 1.Robinson H. Rodent ulcer of the male breast. Trans Pathol Soc Lond. 1893;44:147–148. [Google Scholar]
- 2.Rosen N, Muhn CY, Bernstein SC. A common tumor, an uncommon location: basal cell carcinoma of the nipple and areola in a 49-year-old woman. Dermatol Surg. 2005;31:480–483. doi: 10.1111/j.1524-4725.2005.31120. [DOI] [PubMed] [Google Scholar]
- 3.Nouri K, Ballard CJ, Bouzari N, Saghari S. Basal cell carcinoma of the areola in a man. J Drugs Dermatol. 2005;4:352–354. [PubMed] [Google Scholar]
- 4.Huang CW, Pan CK, Shih TF, Tsai CC, Juan CC, Ker CG. Basal cell carcinoma of the nipple-areola complex: a case report. Kaohsiung J Med Sci. 2005;21:480–483. doi: 10.1016/S1607-551X(09)70155-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gupta C, Sheth D, Snower DP. Primary basal cell carcinoma of the nipple. Arch Pathol Lab Med. 2004;128:792–793. doi: 10.5858/2004-128-792-PBCCOT. [DOI] [PubMed] [Google Scholar]
- 6.LeBoit PE, Burg G, Weedon D, Sarasain A, editors. World Health Organization Classification of Tumours: Pathology and Genetics of Skin Tumors. Lyon: IARC Press; 2006. pp. 15–16. [Google Scholar]
- 7.Cain RJ, Sau P, Benson PM. Basal cell carcinoma of the nipple. J Am Acad Dermatol. 1990;22:207–210. doi: 10.1016/0190-9622(90)70025-d. [DOI] [PubMed] [Google Scholar]
- 8.Cooper RA, Eilers DB. Mammographic findings in basal cell carcinoma of the male nipple. AJR. 2000;175:1065–1066. doi: 10.2214/ajr.175.4.1751065. [DOI] [PubMed] [Google Scholar]
- 9.Bath-Hextall F, Bong J, Perkins W, Williams H. Interventions for basal cell carcinoma of the skin: systemic review. BMJ. 2004;329:705–709. doi: 10.1136/bmj.38219.515266.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Farmer ER, Helwig EB. Metastatic basal cell carcinoma: a clinicopathologic study of seventeen cases. Cancer. 1980;46:748–757. doi: 10.1002/1097-0142(19800815)46:4<748::aid-cncr2820460419>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]