Abstract
BACKGROUND
Reports describing the frequency and pattern of abnormal Pap smears in developing countries using the revised Bethesda system for Pap smear are few. We studied the pattern of cervical intraepithelial lesions and carcinoma detected in Pap smears of Saudi females in the western region of Saudi Arabia using the revised system.
METHODS
All cervical Pap smears reported in the Department of Pathology of King Abdulaziz Medical City, Jeddah, from 1 January 1998 to 31 August 2005 were reclassified according to the revised system with age ranges identified.
RESULTS
Of 5590 sufficient smears, 261 (5%) were identified as abnormal and were further classified as atypical squamous cells of undetermined significance (ASC-US) (103 cases, 40%), atypical squamous cells of high grade (6 cases, 2%), low-grade squamous intraepithelial lesions (LSIL) (56 cases, 22%), high-grade squamous intraepithelial lesions (HSIL) (31 cases, 12%), glandular cell abnormalities (30 cases, 11%) and invasive squamous cell carcinoma (21 cases, 9%). The ASC-US/SIL ratio was 1.9%. Invasive adenocarcinoma accounted for 14 cases (4%) with a similar age range as invasive squamous cell carcinoma.
CONCLUSION
Although this study showed a lower incidence and a wider age range of cervical epithelial cell abnormalities than others published internationally, the results emphasize the need for a well-organized cervical screening program supplemented by larger national studies on the pattern of cervical abnormalities in this country. The information provided in this study will encourage use of the Pap smear as a screening method for cervical cancer in developing countries.
Cervical cancer continues to be a major cause of morbidity and mortality among the female population worldwide, representing the second most common cancer in females with 500 000 news cases and 280 000 deaths each year.1–3 In underdeveloped countries such as Latin America and Southeast Asia it is considered the leading cause of cancer mortality in women.1–3 Since the introduction of the Pap smear in the 1940s, the incidence of cervical cancer has dropped dramatically, especially in countries with well-established cervical screening programs such as the USA where it is considered the sixth most common cancer in women with 13 000 cases of invasive carcinomas and 55 000 cases of carcinoma in situ diagnosed annually.4 In Saudi Arabia, cervical cancer ranks as the eighth most common cancer in females with a mean age of 53 years.5
Standardization of Pap smear reporting using the Bethesda system10 unified various overlapping terminologies and hence improved the diagnosis and management of these lesions. Reports describing the frequency and pattern of abnormal Pap smears in developing countries, particularly Saudi Arabia, using the revised Bethesda system are very few. For this reason the current study was conducted to explore the pattern of epithelial cell abnormalities detected in Pap smears in females of the western region of Saudi Arabia using the Bethesda system and to correlate the findings with published national and international data, in an effort to help improve the utilization of the Pap smear as a screening tool for cervical cancer in our region.
METHODS
We conducted a computerized data retrieval of all cervical Pap smears reported in the department of Pathology of King Abdulaziz Medical City, Jeddah, a large tertiary hospital and oncology referral centre in the western region of Saudi Arabia, in the period from the beginning of January 1998 to the end of August 2005. Adequate smears were first identified. A smear was considered adequate when all needed clinical information was present, including appropriate labeling of the slide, adequate sampling of the transformation zone and optimal preservation of the slide. All adequate cervical cytology smears were reviewed and reclassified according to the revised 2001 Bethesda system of Pap smear reporting (Table 1), into negative for intraepithelial lesions or malignancy or positive for epithelial abnormalities. Under the category of negative for intraepithelial lesions or malignancy the number and percentage of unremarkable (negative) smears and smears showing inflammatory/reactive smears were identified. Smears positive for epithelial cell abnormalities were identified and further classified following the 2001 Bethesda system. In cases of ambiguous diagnoses, the cytology slides were retrieved and reviewed on a multihead microscope by a senior cytotechnoogist and a cytopathologist especially assigned to review these cases using the above mentioned system. The total number and percentages of each abnormal Pap smear category were identified and correlated with the patient’s age.
Table 1.
The revised Bethesda 2001 system (abridged) for cervical Pap smear reporting.12
| SPECIMEN ADEQUACY |
| Satisfactory for evaluation (note presence/absence of endocervical/transformation zone component) |
| Unsatisfactory for evaluation … (specify reason) |
| Specimen rejected/not processed (specify reason) |
| Specimen processed and examined, but unsatisfactory for evaluation of epithelial abnormality because of (specify reason) |
| GENERAL CATEGORIZATION (Optional) |
| Negative for intraepithelial lesion or malignancy |
| Epithelial cell abnormality |
| Other |
| INTERPRETATION/RESULT |
| Negative for Intraepithelial Lesion or Malignancy |
| Organisms |
| Trichomonas vaginalis |
| Fungal oganisms morphologically consistent with Candida species |
| Shift in flora suggestive of bacterial vaginosis |
| Bacteria morphologically consistent with Actinomyces species |
| Cellular changes consistent with herpes simplex virus |
| Other non-neoplastic findings (Optional to report; list not comprehensive) |
| Reactive cellular changes associated with inflammation (includes typical repair) |
| radiation |
| intrauterine contraceptive device |
| Glandular cells status posthysterectomy |
| Atrophy |
| Epithelial Cell Abnormalities |
| Squamous cell |
| Atypical squamous cells (ASC) |
| of undetermined significance (ASC-US) |
| cannot exclude HSIL (ASC-H) |
| Low-grade squamous intraepithelial lesion (LSIL) |
| encompassing: human papillomavirus/mild dysplasia/cervical |
| intraepithelial neoplasia (CIN) 1 |
| High-grade squamous intraepithelial lesion (HSIL) |
| encompassing: moderate and severe dysplasia, carcinoma in situ; |
| CIN 2 and CIN 3 |
| Squamous cell carcinoma |
| Glandular cell |
| Atypical glandular cells (AGO) (specify endocervical, endometrial, or not otherwise specified) |
| Atypical glandular cells, favor neoplastic (specify endocervical or not otherwise specified) |
| Endocervical adenocarcinoma in situ (AIS) |
| Adenocarcinoma |
| Other (List not comprehensive) |
| Endometrial cells in a woman ≥40 years of age |
| AUTOMATED REVIEW AND ANCILLARY TESTING (Include as appropriate) |
| EDUCATIONAL NOTES AND SUGGESTIONS (Optional) |
RESULTS
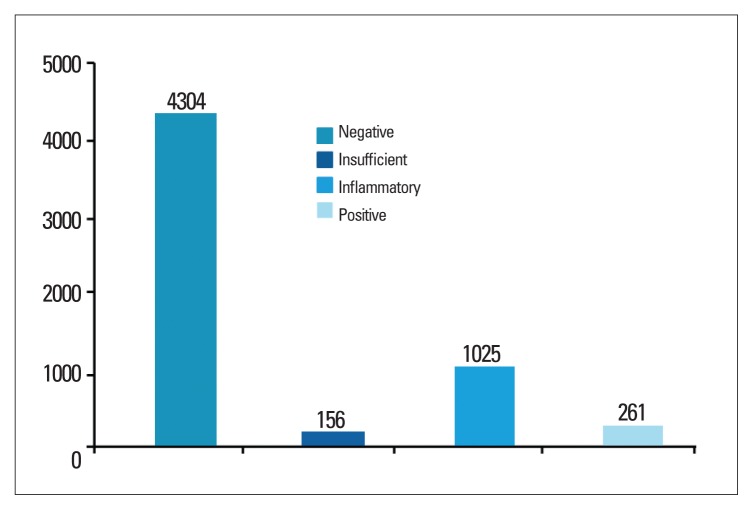
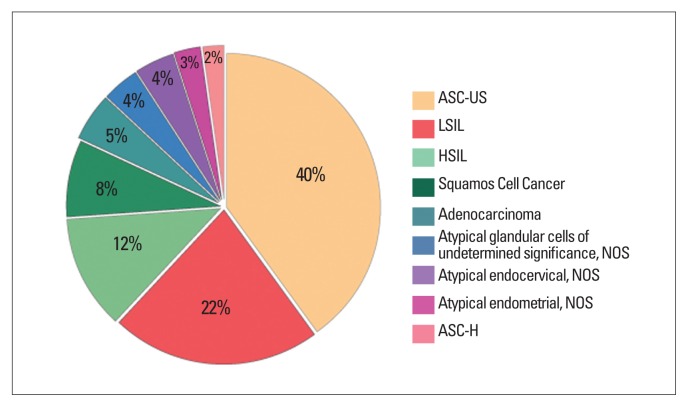
In the computer database we identified a total of 5746 cervical pap smears received and reported in the Department Of Pathology at King Abdulaziz Medical City (KAMC), Jeddah, in the period from January 1998 to August 2005. The study identified 5590 (97.2%) sufficient smears and 156 (2.8%) insufficient smears. The latter cases were excluded from this study. Of the 5590 sufficient smears, 4304 (77%) smears were reported as negative for squamous epithelial abnormalities while 1025 (18%) showed inflammatory/reactive changes (Figure 1). Two hundred sixty-one smears (5%) were diagnosed as positive for cervical epithelial abnormalities. The positive smears were further classified according to the revised 2001 Bethesda system as shown in Figure 2 and Table 2. No endocervical or endometrial cells, favor neoplastic or adenocarcinoma in situ were reported in this study.
Figure 1.
Pap smear diagnosis for 5590 smears from the records of King Abdulaziz Medical City Hospital from 1 January 1998 to 31 August 2005.
Figure 2.
Pattern of epithelial abnormalities in 261 positive Pap smears.
Table 2.
Numbers and percentages of epithelial abnormalities out of the total number of smears (5590) and total number of positive smears (261), including age range and average age using the revised 2001 Bethesda System.
| Type of epithelial abnormality | Number of epithelial abnormalities | % of total number of smears (n=5590) | % of positive Pap smears (n=261) | Age range (years) | Average age (years) |
|---|---|---|---|---|---|
| ASC-US | 103 | 1.84 | 40 | 19–65 | 42 |
| ASC-H | 6 | 0.1 | 2 | 36–70 | 53 |
| LSIL | 56 | 1 | 22 | 29–47 | 38 |
| HSIL | 31 | 0.55 | 12 | 18–67 | 42.5 |
| Squamous cell carcinoma | 21 | 0.37 | 9 | 30–88 | 59 |
| Atypical endocervical cells, NOS | 10 | 0.17 | 4 | 25–75 | 50 |
| Atypical endometrial cells, NOS | 9 | 0.16 | 3 | 22–80 | 51 |
| Atypical glandular cells, NOS | 11 | 0.19 | 4 | 26–89 | 57.5 |
| Adenocarcinoma (endocervical, endometrial) | 14 | 0.25 | 4 | 27–78 | 52.5 |
| Total | 261 | 4.63 | 100 |
NOS: Not otherwise specified
DISCUSSION
In Saudi Arabia, cervical carcinoma ranks as the eighth most common cancer accounting for 3.6% of all cancers in females, with a mean age of 53 years.5 Although many risk factors has been studied as etiologic factors leading to cervical cancer, recently published international epidemiologic and molecular studies confirm beyond a doubt the strong casual relationship between human papilloma virus (HPV) and cervical intraepithelial lesions and carcinoma independent of other risk factors.6 The WHO has concluded that there is sufficient evidence to consider HPV as the cause of cervical cancer.7 Over 100 HPV types have been isolated with more than 15 considered oncogenic (such as type 16, 18, 31, 33, 35, and others) based on their association with malignant lesions.8
Over the years, the original Pap smear classification system has gone through many modifications in response to our growing knowledge of cervical carcinoma precursors and our understanding of the rule of HPV cervical carcinogenesis. These overlapping classifications contain several vague terminologies. Poorly defined abnormal smear findings have pushed the medical societies to try to unify different reporting systems. 9 In 1988, the National Cancer Institute adopted the Bethesda system for cervical smear reporting10 in an attempt to overcome this problem. This system underwent further updates later in 1991.11 In the year 2001, a revised Bethesda system was introduced12 to include new technologies such as HPV DNA studies and liquid base cytology. The adequate but limited category in the adequacy component was cancelled and the atypical squamous cells of undetermined significance (ASCUS) category is divided into either atypical squamous cells of undetermined significance (ASC-US) or atypical squamous cells where high grade cannot be ruled out (ASC-H). 12 The United Atates and many other countries use the revised Bethesda classification for both squamous and glandular lesions.
Few reports are present from our region studying the prevalence of cervical cancer and its precursors using the newly revised 2001 Bethesda system. In this study, all abnormal Pap smears received and reported by the pathology department in King Abdulaziz Medical City, Jeddah were retrieved and reclassified following the Bethesda system. Smears studied in this report are of Saudi females since our centre is a strict military and referral hospital for local citizens only. Our results are in agreement with previously published studies from this country,13–16 showing a lower incidence of abnormal cervical lesions and a wider age range when compared with those from other countries.17–19 In a previous study from the same hospital,13 97 of 3088 Pap smears were reported as abnormal over a period of 7 years. In that study, the findings were as follows: ASC-US (0.45%), LSIL (0.93%), HSIL (0.55%), invasive squamous cell carcinoma (0.13%), AGUS (0.13%), and adenocarcinoma (0.03%).
The percentages of low SIL, High SIL and AGUS categories in the present as well as the above mentioned study from the same hospital were similar, except for a decrease in the percentage in the ASC category (1.84% for ASC-US and 0.1% for ASC-H) and an increase in the incidence of both invasive squamous cell carcinoma (0.37% in the present study) and adenocarcinoma (0.25% in the present study).
Although it may be due to the natural progression of this disease, the increase in the total number of Pap smears with an increased incidence in certain categories and a decreased incidence in borderline categories such as ASC-US is most likely due to the increased rate of referred cancer cases to the recently opened oncology referral centre (opened in the year 2000), the increased awareness of Saudi females of the importance of cervical cancer screening and abidance of cytotechnoogists and cytopathologists to more stringent criteria when submitting diagnoses such as ASC-US.
Edelman et al17 studied Pap smears from 29 295 females over a period of one year and the Pap smear abnormalities were as follows: 9.9% ASC-US, 2.5% LSIL, 0.6% HSIL and 0.2% invasive cancer. In the same study adolescents with an age range of 13–22 years had a significantly higher rate of LGSIL (low-grade squamous intraepithelial lesion). The compared to the present study, a comparable number of HGSIL (high-grade squamous intraepithelial lesion) and low number of invasive carcinoma could be related to early detection of abnormal cervical lesions by well established cervical screening programs. In another study from Brazil 18 22 441 Pap smears were examined over a period of 5 years (October 1997–October 2002) and results showed that low-grade lesions were more common in women aged 15–30 years while high-grade lesions were more common in women aged 25–45 years. Patients older than 40 years had the greatest incidence of invasive cancer. Although a similar age range difference between low-and high-grade lesions is seen in the present study confirming the well-established natural history of cervical carcinogenesis, all grades of abnormal cervical lesions were seen in slightly older age groups when compared to the two previous studies, most likely due to late detection of such lesions, usually as a part of either post partum follow up or investigation of a gynecologic complaint.
In our study, The ASC-US category accounted for 40% of all abnormal smears, ASC-H for 2% of all abnormal cases and the atypical glandular cell diagnosis (AGC) including AGUS, NOS as well as atypical endocervical and endometrial cells (NOS) for a total of 11% which compares favorably with other local13–16 and international figures.19,20
In the last decade several new techniques have been developed such as thin-layer cytological preparations and hybrid capture testing for HPV DNA.21,22 Thin prep cytology, approved by the FDA in 1996, is based on collection of the cervical cell sample in a vial containing a special liquid media. Several studies22 showed that the thin prep method of sampling results in a significant increase in cytological diagnosis of cervical smear precursors and in an increased percentage of adequate smears as compared with the conventional method of Pap smearing. Although clear recommendations for the use of HPV DNA testing in cervical cancer screening are still not available and data is still insufficient to justify the use of HPV DNA testing as a primary method of cervical cancer screening, the cost effectiveness as well as ability to incorporate the value of a positive HPV test into the management of the screened patient should be studied.21 In one study by Kaufman et al23 1128 women with two readings of either LGSIL or ASCUS on Pap smear received colposcopy, biopsy and HPV DNA testing. The detection of high-risk DNA HPV poorly predicted the likelihood of finding CIN 2 or 3 on biopsy. The sensitivity of HPV testing was only 28% for women with ASCUS and only 58% for women with LGSIL.
In June 2006, the FDA 24 approved Gardasil, a vaccine targeted against HPV type 6 and 11 which accounts for 90% of genital warts and HPV type 16 and 18, which accounts for 70% of cervical cancer. Whether the vaccine can be used effectively in prevention of cervical cancer in this country is yet to be determined. More research is needed to unmask the definite etiological factors for cervical cancer and whether a cause-effect relationship between HPV and cervical intraepithelial lesions and cancer can be established in our country.
Based on the data regarding the incidence of abnormal cervical lesions outlined in the present as well as the previously published local studies and reports,13–16 health and social organizations in this country should cooperate to build a well-organized national cervical screening program. Key elements for the establishment and success of such a program include increased public awareness, especially in young females about the importance of cervical screening in prevention of cervical cancer, the availability of financial coverage as well as standardization of protocols used in diagnosis and management of these lesions by health professionals. It is recommended that different parties including gynecologists, family physicians and midwives as well active community members initiate such programs. These parties should be aware and work hard to overcome several obstacles that may be faced during the implementation of such programs such as poor education among females from rural areas and small villages as well as the presence of some cultural restraints in those places which prohibit full access to the target groups of the population.
REFERENCES
- 1.Morris M, Tortolero-Luna G. Cervical intraepithelial neoplasia and cervical carcinoma. Obstet Gynecol Clin North Am. 1996;23:347–401. [PubMed] [Google Scholar]
- 2.Coleman M, Esteve J, Damieck P. Trends in cancer incidence and mortality Cervix uteri. 121. Lyon France: IARC Scientific Publication; 1993. p. 433. [DOI] [PubMed] [Google Scholar]
- 3.Bridging the gaps. Geneva: World Health Organization; 1995. The World Health Report 1995. [Google Scholar]
- 4.Cancer statistics. CA cancer. J Clinicians. 1999;49:54–6. [Google Scholar]
- 5.National cancer registry. Cancer incidence report, 1997–1998. [Google Scholar]
- 6.Bosch FX, Manos MM. Prevalence of human papilloma virus in cervical cancer: a worldwide perspective. J Natl Cancer Inst. 1995;87:796–802. doi: 10.1093/jnci/87.11.796. [DOI] [PubMed] [Google Scholar]
- 7.Sherman ME, Kurman RJ. Intraepithelial carcinoma of cervix: reflections on half a century of progress. Cancer. 1998;83:2243–6. doi: 10.1002/(sici)1097-0142(19981201)83:11<2243::aid-cncr1>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 8.Lorinz AT, Reid R. Human papilloma virus infection of cervix: relative risk association of 15 common anogenital types. Obstet Gynecol. 1992;79:328–37. doi: 10.1097/00006250-199203000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Jordan LB, Monaghan H. Pathology of the cervix: recent developments. Clinical Oncology. 2004;16:248–254. doi: 10.1016/j.clon.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 10.NCI workshop. The 1988 Bethesda system for reporting cervical/vaginal cytological diagnosis. AMA. 1989;262:931–4. [PubMed] [Google Scholar]
- 11.National Cancer Institute. The Bethesda system for reporting of cervical/vaginal diagnosis: revised after the sehincond national cancer institute workshop on April 29–30 1991. Acta Cytol. 1993;37:115–124. [PubMed] [Google Scholar]
- 12.Solomon D, Davey D, Kurman R The forum group members. The Bethesda 2001 workshop. The 2001 Bethesda system: terminology for reporting results of cervical cytology. JAMA. 2002;287:2114–2119. doi: 10.1001/jama.287.16.2114. [DOI] [PubMed] [Google Scholar]
- 13.Altaf F. Pattern of cervical smear cytology in the western region of Saudi Arabia. Ann Saudi Med. 2001;21:94–96. [PubMed] [Google Scholar]
- 14.Abduljabbar H. Abnormal cervical cytology: a preliminary report on 21372 women from the western region of Saudi Arabia. SaudiMed J. 1990;11(5):372–375. [Google Scholar]
- 15.Jamal A, AlMaghrabi J. Profile of Pap smear cytology in the western region of Saudi Arabia. SaudiMed J. 2003;24(11):1225–1229. [PubMed] [Google Scholar]
- 16.Elhakeem H, Algamdi A, AlMagrabi J. Cytopathological pattern of cervical Pap smear according to the Bethesda system in southwestern Saudi Arabia. 2005 Apr;26(4):588–92. [PubMed] [Google Scholar]
- 17.Edelman M, Fox A. Cervical Papanicolaou smear abnormalities in inner bronx adolescents: prevalence, progresion and immune modifiers. Cancer (cancer cytopathology) 1999;87(4):184–189. [PubMed] [Google Scholar]
- 18.Bleggi TLF, Werner B. Cervical cancer screening program of Parana: cost-effective model in a developing country. Diagn Cytopathol. 2003 Jul;29(1):49–54. doi: 10.1002/dc.10269. [DOI] [PubMed] [Google Scholar]
- 19.Karateke A, Gurbuz A, Kabaca C. Atypical squamous cells: improvement in cytohistological correlation by the 2001 Bethesda system. European J Gynecol Oncol. 2004;25(5):615–618. [PubMed] [Google Scholar]
- 20.Parellanda CI. Atypical glandular cells on cervical smears. Int J Gynecol Obstet. 2002 Sep;78(3):227–34. doi: 10.1016/s0020-7292(02)00194-7. [DOI] [PubMed] [Google Scholar]
- 21.Lee KR, Ashfaq R, Birdsong GG. Comparison of conventional Papanicolaou smears and a fluid-based, thin layer system for cervical cancer screening. Obstet Gynecol. 1997;90:278–83. doi: 10.1016/S0029-7844(97)00228-7. [DOI] [PubMed] [Google Scholar]
- 22.Wright TC, Jr, Massad LS, Twiggs LB. ASCCP-sponsored consensus conference. 2001 consensus guidelines for the management of women with cervical cytological abnormalities. JAMA. 2002;287:2120–2129. doi: 10.1001/jama.287.16.2120. [DOI] [PubMed] [Google Scholar]
- 23.Kaufman RH, Adam E, Icenogle J. Relevance of human pappilomavirus in management of cervical intraepithelial neoplasia. Am J Obstet Gynecol. 1997;176:87–92. doi: 10.1016/s0002-9378(97)80017-8. [DOI] [PubMed] [Google Scholar]
- 24.FDA documentation of Gardasil approval. http://www.fda.gov/cber/products/hpvmer060806.htm.