Abstract
BACKGROUND
Malnutrition is highly prevalent among the elderly and is associated with poor clinical prognosis, decreased functional status, and increased morbidity and mortality.
OBJECTIVE
To estimate the prevalence of geriatric malnutrition among outpatients of a geriatric clinic and to determine factors associated with malnutrition.
DESIGN
Cross-sectional study.
SETTING
Geriatric outpatient clinic of the King Abdul Aziz University Hospital, Jeddah.
PATIENTS AND METHODS
All patients older than 60 years of age who attended the clinic during January 2016 were eligible for inclusion. Nutritional status was assessed using anthropometric data and by hemoglobin and albumin levels and lymphocyte count. The MNA was used to define malnutrition.
MAIN OUTCOME MEASURES
Anthropometric measures, biochemical tests, and the scores on the short version of the Mini Nutritional Assessment (MNA).
RESULTS
According to the MNA results, 8 (5.3%) of 152 elderly patients suffered overt malnutrition and 50 (32.9%) were at risk of malnutrition (71 males and 41 females; aged 72.4 [8.6] years). The prevalence of malnutrition was significantly higher among females (44.6%; 95% CI, 1.01–4.08; P=.044) than in males (28.3%). Malnourished patients were older than patients with normal nutritional status (mean 72.4 [8.6] years), and more common in patients who lived alone (62.5%). The malnourished patients had significantly smaller calf circumferences (63.4; 95% CI, 1.51–3.20; P=.001), and lower albumin and hemoglobin levels (P=.001). A significantly higher percentage of the malnourished patients compared with normal patients had experienced weight loss (37.9%; P<.001) and decreased food intake (56.9%; P<.001) during the previous three months. Binary logistic regression revealed that being female and living alone were significant predictors for being categorized as malnourished or at risk of malnutrition.
CONCLUSION
The prevalence of malnutrition is high among geriatric outpatients. Routine screening for malnutrition among geriatric patients would allow early diagnosis and prompt intervention.
LIMITATIONS
The heterogeneity of the study group (different diseases at different stages) could influence the generalizability of our findings. The relatively small number of patients (P=.002) is a potential limitation.
Malnutrition in the elderly is defined as “faulty or inadequate nutritional status (or) undernourishment characterized by insufficient dietary intake, poor appetite, muscle wasting and weight loss.” If overlooked, malnutrition leads to poor health and decreased quality of life.1 It is highly prevalent among geriatric outpatients, and is independently associated with defective functional status and poor quality of life.2
Worldwide, geriatric malnutrition is a substantial problem.3 The overall prevalence estimated from a pooled database was 22.8%.4 Persons aged 60 years and older are the fastest growing age group in the world.5 In 2014, the increase in the number of people in this group was triple that of the whole population.6 Between 1994 and 2014, the number of elderly doubled, with two thirds living in less developed regions of the world.7 By 2050, it is expected that the number of dependent adults in Saudi Arabia will equal the number of dependent children for the first time.5
Despite its high prevalence and well-documented adverse effects, malnutrition remains under-identified in this vulnerable group.8 Nutritional assessment is not a routine part of patient clinical evaluation at most Saudi hospitals. The current study aimed to investigate the prevalence of malnutrition among elderly patients who attended a geriatric outpatient clinic at King Abdulaziz University Hospital in Saudi Arabia and to determine factors associated with malnutrition.
PATIENTS AND METHODS
This cross-sectional study was carried out at King Abdulaziz University Hospital, which is an 845-bed teaching hospital with a specialized geriatric outpatient clinic. The study included geriatric patients (older than 60 years) in the clinic appointments list in January 2016 who agreed to participate in the study and gave informed consent.
Baseline demographic data were collected using a questionnaire that covered age, gender, marital status, living arrangement, income, chronic illness (diabetes, hypertension, cardiovascular diseases, bronchial asthma, renal diseases, chronic hepatic diseases and chronic neurological disorders), and education. Nutritional status was assessed using anthropometric data, including body mass index (BMI) and calf circumference. Weight was rounded to the nearest 0.1 kg, and measured while the patient was lightly clothed. Height was measured by the patient standing without shoes on a stadiometer, and rounded to the nearest 0.1 cm. Body mass index was calculated as the patient’s weight in kg divided by the square of the patient’s height in cm.9 When height or weight could not be measured precisely due to body abnormalities, the calf circumference was measured at its largest diameter to the nearest 0.1 cm and used as an indicator of nutritional status.10 Nutritional status was also assessed by hemoglobin and albumin levels, and lymphocyte count.
The Mini Nutritional Assessment Short Form (MNASF)11 was used as a screening tool (Table 1).This form was introduced in 1994 to assess nutritional and functional status, and to predict mortality among the elderly. A simple, inexpensive tool, with 96% sensitivity and 98% specificity, it has been widely used in research and clinical practice.11 It was revised to include a “malnourished” category, which increased the applicability and rapid screening in clinical practice.12 The maximum score on the MNA is 14 points. Malnourished subjects are those who score less than 8. The at-risk group scores between 8 and 11, and the well-nourished group scores above 12.
Table 1.
The Mini-Nutritional Assessment Short Form (MNA-SF).
| Screening question | Answer score | |||
|---|---|---|---|---|
| 0 | 1 | 2 | 3 | |
|
| ||||
| (A) Has food intake declined over the past 3 months due to loss of appetite, digestive problems, chewing or swallowing difficulties? | severe decrease in food intake | moderate decrease in food intake | no decrease in food intake | ---------------- |
| (B) Weight loss during the last 3 months | weight loss greater than 3 kg (6.6 lbs) | does not know | weight loss between 1 and 3 kg (2.2 and 6.6 lbs) | no weight loss |
| (C) Mobility | bed or chair bound | able to get out of bed/chair but does not go out | goes out | ---------------- |
| (D) Has suffered psychological stress or acute disease in the past 3 months? | yes | ----------------- | no | ---------------- |
| (E) Neuropsychological problems | severe dementia or depression | mild dementia | no psychological problems | ---------------- |
| ± (F1) Body Mass Index (BMI) (weight in kg)/(height in m2) | BMI less than 19 | BMI 19 to less than 21 | BMI 21 to less than 23 | BMI 23 or greater |
| ± (F2) Calf circumference (CC) in cm | CC less than 31 | ----------------- | -------------------- | CC 31 or greater |
± IF BMI IS NOT AVAILABLE, REPLACE QUESTION F1 WITH QUESTION F2. DO NOT ANSWER QUESTION F2 IF QUESTION F1 IS ALREADY COMPLETED.
Screening scoring (max. 14 points) 12–14 points: Normal nutritional status, 8–11 points: At risk of malnutrition, 0–7 points: Malnourished
Normally distributed variables were expressed as means and standard deviation (SD). Categorical variables were expressed as a number and percentage. A chi-square test of association was used to examine the significance of categorical variables, and odds ratios were calculated to evaluate the magnitude of the impact of significant variables. A binary logistic regression was carried out to identify predictors of malnourishment, introducing significant factors from the chi-square test as the first step in the model and omitting non-significant factors afterwards. All results were analyzed using SPSS version 20 software, with statistical significance set at P<.05. This study was approved by the Unit of Biomedical Ethics Research Committee, Jeddah (No: HA-02-J-008).
RESULTS
Of 322 geriatric patients (older than 60 years) in the clinic appointments list in January 2016 152 agreed to participate in the study. Eighteen patients did not wish to participate in the study.
The age of the 152 participants ranged between 60 to 91 years (mean 70.2 [8.1] years). Almost two-thirds (60.5%) of the subjects were female (n=92). The patients were mostly married (85.5%) or widowed (13.8%). Ninety-four patients (61.8%) were illiterate. The great majority (83.6%) had a monthly income of <SR 3000 (US $800), and 10.5% reported that they were living alone. Most of the patients (81.6%) reported that they had been diagnosed previously with a chronic disease; these included 79 (52%) diabetics, 84 (55.3%) hypertensive patients, 34 (22.4%) with ischemic heart disease, and 46 (30.3%) with dyslipidemia.
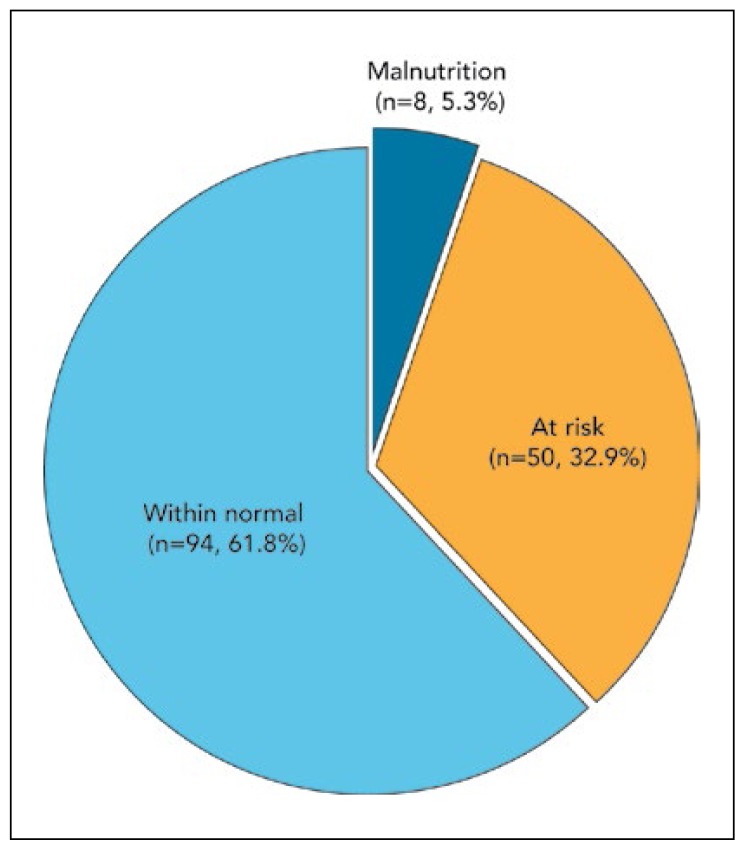
Based on categorization of the MNA score, only 8 (5.3%) had overt malnutrition (0–7 points). One-third (32.9%) were at risk of being malnourished (Figure 1). Table 2 shows that the prevalence of malnutrition was significantly higher among females (44.6%) than males (28.3%, P=.044), with an odds ratio (OR) of 2.0 and 95% confidence interval (CI) (1.01–4.08). The malnourished patients were significantly older (mean 72.4 years [8.6] years) than the subjects who were categorized as having normal nutritional status (68.8 years [7.5]) P=.007. Almost two thirds of those who were living alone (62.5%) were categorized as malnourished or at risk of malnutrition, which differed significantly from those who were living with others, among whom only one third was malnourished (35.3%; OR=3.1; 95% CI; 1.05–8.92, P=.034). Table 3 shows that the proportion of those who had a calf circumference less than 31 cm was significantly higher among malnourished patients (63.4%) than those who had a calf circumference greater than 31 cm (28.8%; OR=2.2; 95% CI; 1.51–3.20; P=.001); also, they had significantly lower mean (SD) albumin (29.6 mg/dL [7.1]) P=.002 and mean (SD) hemoglobin (10.8 g/dL [1.8], P=.001).
Figure 1.
Malnutrition among elderly patients by nutritional status (n=152).
Table 2.
Nutritional status of the geriatric patients according to their demographic characteristics (n=152).
| Variable | Normal nutrition (n=94) | Malnourished or at risk of malnutrition (n=58) | P |
|---|---|---|---|
|
| |||
| Demographic/social characteristics | |||
| Gender, n (%) | |||
| Males | 43 (71.1) | 17 (28.3) | |
| Females | 51 (55.4) | 41 (44.6) | .044 |
|
| |||
| Age, mean (SD) | 68.8 (7.5) | 72.4 (8.6) | .007 |
| Living arrangement, n (%) | |||
| Living with family/friends | 88 (64.7) | 48 (35.3) | |
| Living alone | 6 (37.5) | 10 (62.5) | .034 |
|
| |||
| Monthly income, n (%) | |||
| <US $800 | 78 (61.4) | 49 (38.6) | .808 |
| US $800+ | 16 (64.0) | 9 (36.0) | |
Chi-square test for categorical variables; the t test was used for age (malnourished females: 44.6%; 95% CI, 1.01–4.08; P=.044, living alone and malnourished 62.5%; 95% CI, 1.05–8.92; P=.034)
Table 3.
Nutritional status of the geriatric patients according to anthropometric indicators and clinical characteristics (n=152).
| Variable | Normal nutrition, n=94 | Malnourished or at risk of malnutrition, n=58 | P |
|---|---|---|---|
|
| |||
| Anthropometric indicators | |||
| BMI categories, n (%) | |||
| Underweight | 0 (0.0) | 1 (100.0) | NA |
| Within normal | 16 (31.4) | 35 (68.6) | |
| Overweight | 33 (71.1) | 13 (28.3) | |
| Obese | 45 (83.3) | 9 (16.7) | |
| Calf circumference, n (%) | |||
| <31 cm | 15 (36.6) | 26 (63.4) | <.001 |
| 31+ cm | 79 (71.2) | 32 (28.8) | |
| Clinical characteristics | |||
| Chronic illnesses, n (%) | 75 (79.8) | 49 (84.5) | .468 |
| Albumin, mean (SD) | 33.2 (6.3) | 29.6 (7.1) | .002 |
| Hemoglobin, mean (SD) | 12.5 (1.5) | 10.8 (1.8) | <.001 |
| Lymphocytes mean (SD) | 2.0 (0.81) | 1.9 (0.97) | .730 |
Chi-square test for categorical variables; the t test was used for calf circumferences <31 cm (63.4; 95% CI, 1.51–3.20; P= .001).
As shown in Table 4, 56.9% of the malnourished patients reported that their food intake had decreased during the past three months, compared to 9.6% of the apparently normally nourished patients (P=.001). Similarly, the percentage of patients who reported that they could walk without assistance was significantly lower among malnourished patients (63.8%) than the apparently normal patients (81.9%) (P=.026). Moreover, a significantly higher percentage of the malnourished patients (37.9%) noted that they had lost weight in the past three months (P=.001) (Table 4). Binary logistic regression analysis indicated that being an elderly female and living alone were significant predictors for being malnourished or at risk of malnutrition (Table 5).
Table 4.
Nutritional status of the geriatric patients according to food intake and mobility (n=152).
| Variable | Normal nutrition, n=94 | Malnourished or at risk of malnutrition, n=58 | P |
|---|---|---|---|
|
| |||
| Food intake, n (%) | |||
| Decrease in food intake | 9 (9.6) | 33 (56.9) | <.001 |
| No decrease in food intake | 85 (90.4) | 25 (43.1) | |
| Mobility and walking ability, n (%) | |||
| Walk without assistance | 77 (81.9) | 37 (63.8) | |
| Walk with assistance | 10 (10.6) | 9 (15.5) | .026 |
| Using wheelchair or bed bound | 7 (7.4) | 12 (20.7) | |
| Weight loss in the past 3 months, n (%) | |||
| Yes | 6 (6.4) | 22 (37.9) | |
| No | 73 (77.6) | 11 (19.0) | <.001 |
| Don’t know | 15 (16.0) | 25 (43.1) | |
Chi-square test for all comparisons.
Table 5.
Predictors of malnutrition among geriatric inpatients.
| Variables | B | S.E. | Wald | df | P | Odds Ratio | 95% CI for Odds Ratio | |
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
|
| ||||||||
| Living arrangement | 1.081 | .573 | 3.556 | 1 | .059 | 2.948 | .958 | 9.066 |
| Sex | .844 | .380 | 4.944 | 1 | .026 | 2.327 | 1.105 | 4.897 |
| Age | .067 | .023 | 8.780 | 1 | .003 | .935 | .894 | .977 |
| Constant | −7.802 | 1.983 | 15.474 | 1 | .001 | |||
Cox and Snell R square: 0.106, Nagelkerke R square=0.145
DISCUSSION
In our study, almost two-thirds of the patients reported that they had decreased dietary intake, which may be due to loss of appetite and lower income among females. This is comparable to a report by Elmadbouly and Abdelhafez,13 who showed that 52.2% of the malnourished elderly had a severe decline in food intake. Similar results were observed by Oliveira et al who attributed decreased food intake to loss of appetite, digestive problems, or chewing or swallowing problems.14 In this age group, poverty and cognitive impairment may affect eating habits and food choices.15 Research in India pointed to the reciprocal relationship between reduced dietary intake and cognitive function in elderly patients.16 In the present study, females were more prone to loss of appetite than males. Other studies reported that females suffered more frequently from loss of appetite and were more prone to be underweight than males; this was also observed in our study, as the prevalence of malnutrition was significantly higher in females after controlling for other factors.17
In our study, 32.9% of the participants were at risk of malnutrition, which was lower than that detected at a teaching hospital in the Netherlands, where the prevalence among elderly outpatients was 56%.2 In a study conducted in the geriatric outpatient clinic of a university hospital in England, the prevalence of malnutrition was 30%. The discrepancy might be attributed to the use of a different assessment tool (Malnutrition Universal Screening Tool; MUST).18 In the current study, almost one third of our patients were either bedridden or could not move without assistance.
Impaired mobility was found in the present study to be associated with an increased risk of malnutrition. Like most geriatric problems, malnutrition is multifactorial and overlapping. Normal age-related changes in the neurological and musculoskeletal system are responsible for weakness i elderly individuals; this weakness is exacerbated by malnutrition.19
Other factors that contribute to malnutrition among the elderly are social isolation and financial deprivation.20 In our study, the percentage of malnourished geriatric patients was significantly higher in those who were living alone than in those who were living with others (62.5% OR 3.1; 95% CI; 1.05–8.92), which emphasizes the important role of social support for this age group, as they are often unable to serve themselves and have no support for preparing food.2
Serum proteins are used as markers of nutritional status.21 Although Nazemi et al found that the MNA detected risk of malnutrition in patients with normal albumin levels,13 the current study showed serum albumin levels were significantly lower among subjects with malnourishment detected by the MNA. In the current study, mean hemoglobin levels were significantly lower among patients who were either malnourished or at risk of malnutrition. Similarly, Sahin et al in Turkey stated that “malnutrition and malnutrition risk increased the incidence of anemia.”22
A limitation in the analysis is the heterogeneity of the study group with different diseases at different stages, which potentially could influence the generalizability of our findings. The relatively small number of patients available for the study is also a potential limitation.
In conclusion, the prevalence of malnutrition in elderly patients who attended the geriatric clinic of King Abdulaziz University Hospital was high. Routine screening for malnutrition is essential for early detection and prompt treatment, and should be an integral part of the regular follow-up for outpatients. The MNA-SF is a valuable tool to determine the type and causes of malnutrition in elderly individuals, and it can be integrated into the management of geriatric outpatients to increase the quality of care and optimize outcomes.
REFERENCES
- 1.Chen CC, Schilling LS, Lyder CH. A concept analysis of malnutrition in the elderly. Journal of advanced nursing. 2001;36(1):131–42. doi: 10.1046/j.1365-2648.2001.01950.x. [DOI] [PubMed] [Google Scholar]
- 2.van Bokhorst-de van der Schueren MA, Lonterman-Monasch S, de Vries OJ, Danner SA, Kramer MH, Muller M. Prevalence and determinants for malnutrition in geriatric outpatients. Clinical nutrition (Edinburgh, Scotland) 2013;32(6):1007–11. doi: 10.1016/j.clnu.2013.05.007. [DOI] [PubMed] [Google Scholar]
- 3.Harith S, Shahar S, Yusoff M, Kamaruzzaman B, Hua P. The magnitude of malnutrition among hospitalized elderly patients in university Malaya medical centre. Health Environ J. 2010;1:64–72. [Google Scholar]
- 4.Kaiser MJ, Bauer JM, Ramsch C, Uter W, Guigoz Y, Cederholm T, et al. Frequency of malnutrition in older adults: a multinational perspective using the mini nutritional assessment. Journal of the American Geriatrics Society. 2010;58(9):1734–8. doi: 10.1111/j.1532-5415.2010.03016.x. [DOI] [PubMed] [Google Scholar]
- 5.Economic UNDoI, Division SAP. World Population Ageing, 2013. 2013. [Google Scholar]
- 6.United Nations. Concise Report on the World Population Situation in 2014. Department of Economic and Social Affairs, Population Division; 2014. [Google Scholar]
- 7.Garcia de Lorenzo A, Rodriguez-Montes J. Elderly ICU patient: Nutritional and metabolic support. Nutr Hosp. 2011;4(3):61–6. [Google Scholar]
- 8.Correia MI, Campos AC. Prevalence of hospital malnutrition in Latin America: the multicenter ELAN study. Nutrition (Burbank, Los Angeles County, Calif) 2003;19(10):823–5. doi: 10.1016/s0899-9007(03)00168-0. [DOI] [PubMed] [Google Scholar]
- 9.Santos JL, Albala C, Lera L, Garcia C, Arroyo P, Perez-Bravo F, et al. Anthropometric measurements in the elderly population of Santiago, Chile. Nutrition (Burbank, Los Angeles County, Calif) 2004;20(5):452–7. doi: 10.1016/j.nut.2004.01.010. [DOI] [PubMed] [Google Scholar]
- 10.Alhamdan AA, Alsaif AA. The nutritional, glutathione and oxidant status of elderly subjects admitted to a university hospital. Saudi journal of gastroenterology : official journal of the Saudi Gastroenterology Association. 2011;17(1):58–63. doi: 10.4103/1319-3767.74474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rubenstein LZ, Harker JO, Salva A, Guigoz Y, Vellas B. Screening for undernutrition in geriatric practice: developing the short-form mini-nutritional assessment (MNASF) The journals of gerontology Series A, Biological sciences and medical sciences. 2001;56(6):M366–72. doi: 10.1093/gerona/56.6.m366. [DOI] [PubMed] [Google Scholar]
- 12.Kaiser MJ, Bauer JM, Ramsch C, Uter W, Guigoz Y, Cederholm T, et al. Validation of the Mini Nutritional Assessment short-form (MNA-SF): a practical tool for identification of nutritional status. The journal of nutrition, health & aging. 2009;13(9):782–8. doi: 10.1007/s12603-009-0214-7. [DOI] [PubMed] [Google Scholar]
- 13.Nazemi L, Skoog I, Karlsson I, Hosseini S, Mohammadi MR, Hosseini M, et al. Malnutrition, Prevalence and Relation to Some Risk Factors among Elderly Residents of Nursing Homes in Tehran, Iran. Iranian journal of public health. 2015;44(2):218–27. [PMC free article] [PubMed] [Google Scholar]
- 14.Oliveira MR, Fogaca KC, Leandro-Merhi VA. Nutritional status and functional capacity of hospitalized elderly. Nutrition journal. 2009;8:54. doi: 10.1186/1475-2891-8-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Culross B. Nutrition: Meeting the Needs of the elderly. ARN Network. 2008 [Google Scholar]
- 16.Agarwal A, Chauhan K, Shinglot K. Anthropometric indices and dietary intake: prospective determinants of geriatric cognitive impairment? Nutrition and health. 2013;22(2):157–67. doi: 10.1177/0260106014563448. [DOI] [PubMed] [Google Scholar]
- 17.Reijnierse EM, Trappenburg MC, Leter MJ, Blauw GJ, de van der Schueren MA, Meskers CG, et al. The Association between Parameters of Malnutrition and Diagnostic Measures of Sarcopenia in Geriatric Outpatients. PloS one. 2015;10(8):e0135933. doi: 10.1371/journal.pone.0135933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stratton RJ, Hackston A, Longmore D, Dixon R, Price S, Stroud M, et al. Malnutrition in hospital outpatients and inpatients: prevalence, concurrent validity and ease of use of the ‘malnutrition universal screening tool’ (‘MUST’) for adults. The British journal of nutrition. 2004;92(5):799–808. doi: 10.1079/bjn20041258. [DOI] [PubMed] [Google Scholar]
- 19.Ha L, Hauge T, Spenning AB, Iversen PO. Individual, nutritional support prevents undernutrition, increases muscle strength and improves QoL among elderly at nutritional risk hospitalized for acute stroke: a randomized, controlled trial. Clinical nutrition (Edinburgh, Scotland) 2010;29(5):567–73. doi: 10.1016/j.clnu.2010.01.011. [DOI] [PubMed] [Google Scholar]
- 20.Pearson JM, Schlettwein-Gsell D, Brzozowska A, van Staveren WA, Bjornsbo K. Life style characteristics associated with nutritional risk in elderly subjects aged 80–85 years. The journal of nutrition, health & aging. 2001;5(4):278–83. [PubMed] [Google Scholar]
- 21.Heizer W, Holcombe B. Approach to the patient requiring nutritional supplementation. Textbook of Gastroenterology. 1995:1044–90. [Google Scholar]
- 22.Sahin S, Tasar PT, Simsek H, Cicek Z, Eskiizmirli H, Aykar FS, et al. Prevalence of anemia and malnutrition and their association in elderly nursing home residents. Aging clinical and experimental research. 2015 doi: 10.1007/s40520-015-0490-5. [DOI] [PubMed] [Google Scholar]