Celiac disease (gluten sensitive enteropathy) is an immune reaction to wheat gluten and related proteins in genetically predisposed individuals leading to malabsorption, intestinal and extraintestinal manifestations. Thromboembolic phenomena have been reported with celiac disease at times. Mesenteric vein thrombosis accounts for 5 to 15 percent of all mesenteric ischemia commonly secondary to a hypercoagulable state. We report on previously healthy woman with celiac disease that remained undiagnosed for many years and who presented with mesenteric vein thrombosis.
Case
A 30 year-old female presented with a 28-day history of severe epigastric pain radiating to the left upper quadrant that was colicky in nature. The pain had no relationship to food or position. There were no associated symptoms like vomiting, diarrhea or fever and no history of any similar attack. Her medical history was unremarkable apart from iron deficiency anemia for many years. Her hemoglobin ranged from 7–8 g/L. No clear cause had been established for anemia; she used to take intramuscular injection of Iron to improve her hemoglobin as there was no response to oral iron. There was no history of chronic diarrhea or abdominal pain but bloating occurred occasionally. There were no symptoms suggestive of thromboembolic, hematological or autoimmune disorder. She took no drugs including contraceptive pills. There was nothing significant in her family history.
Physical examination showed a well-looking young lady with a dark complexion but pale. She weighed 46.6 kg with a height 160 cm (BMI, 17). She was febrile, with a blood pressure of 107/77, a pulse rate of 91/min, and a regular respiratory rate of 20/min. The chest and cardiovascular system were normal, with mild epigastric tenderness and a palpable spleen tip. She had a white cell count of 2.3 × 109/L, hemoglobin 7.3 g/L and platelets of 518 × 1012/L, prothrombin time of 14 sec, partial thromboplastin time of 36 sec, and INR 1.2. Renal and liver function tests were normal. Antinuclear antibody was negative. Screening for hypercoagulable states including antithrombin III, protein C and S and the Ham Test were normal, anticardiolipin antibody, antiphospholipid antibody and activated protein C resistance were all negative. Serum iron was 3.6 μmol/L, TIBC 57 μmol/L, serum ferritin 20 μg/L, and the homocysteine level was mildly high at 10 units/L. A CT scan of the abdomen revealed extensive thrombosis involving the superior mesenteric vein and the splenic vein and portal vein, with collaterals seen; there was no evidence of bowel gangrene.
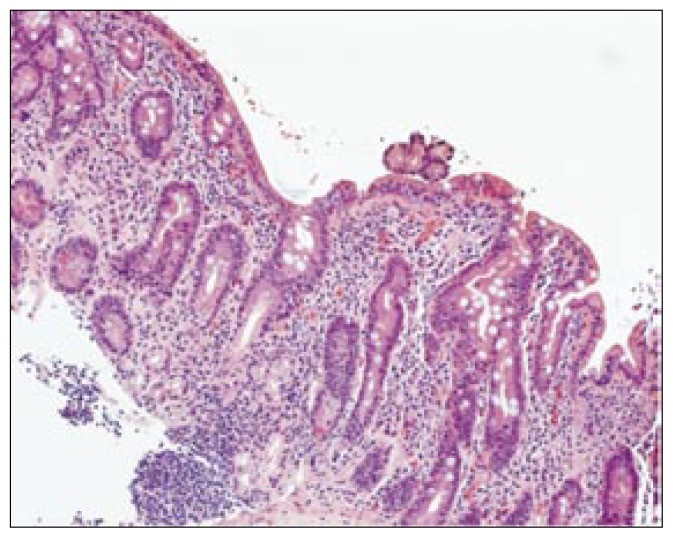
She was not considered for thrombolytic therapy as she presented to us 28 days after the acute event and there was no evidence of bowel ischemia. Thus she was started on heparin initially and then warfarin orally, targeting an INR of 2.5–3.5. An upper gastrointestinal endoscopy done for her iron deficiency anemia showed scalloping with loss of a normal mucosal fold in the duodenum, and biopsy showed severe villous atrophy associated with crypt hyperplasia and an increase in intraepithelial lymphocytes (Figure 1). Antiendomyseal antibody level was positive. Antitissue transglutamine IgA was high at 15.6 U (highest level is 20U). Both tests had a sensitivity and specificity of 97% in celiac disease which practically confirmed our clinical diagnosis of celiac disease. The patient was started on a gluten-free diet. She was discharged on warfarin and given advice regarding her diet. On clinical follow up six months later, she was asymptomatic with an increase in her weight and body mass index. Hemoglobin had increased to 113 g/L and follow-up antiendomyseal antibody was negative.
Figure 1.
H & E stained section showing total villous atrophy associated with crypt hyperplasia and an increased number of intraephithelial lymphocytes.
Discussion
Celiac disease is a malabsorption disorder, which most frequently occurs in childhood, but it can present at any age. A typical presentation of celiac disease is weight loss, steatorrhea and nutritional deficiencies, especially iron deficiency anemia. Celiac disease is the cause of 2% to 5% of iron deficiency anemia.1 Many patients with celiac sprue have minimal or no symptoms and consequently remain undiagnosed. Therefore the true prevalence of the disease is not known and consequently the prevalence of the disease is underestimated. The disease is rare in blacks2 but in Arabs is estimated to be 1:2800 live births.3 Presentation of the disease can be intestinal or extraintestinal. Thrombosis and the hypercoagulable state have been described in celiac disease as an extra-intestinal complication, which could be secondary to malabsorption leading to folate deficiency and acquired hyperhomocysteinaemia,4,5,6 but other causes like associated autoimmune disease could also be responsible.
Reviewing the literature, we found 7 case reports in which patients with celiac disease developed thromboembolic disease, most likely secondary to celiac disease. These included a patient with deep venous thrombosis,7,8,9,10 Budd-Chiari syndrome,11,12 pulmonary embolism5 and a patient with splenic thrombosis.13 Our patient is the first case of celiac disease with mesenteric vein thrombosis. She remained undiagnosed for a long time and celiac disease was confirmed based on laboratory, serology and histological tests. Villous atrophy is not specific to celiac disease and can be seen in chronic intestinal ischemia, refractory or unclassified sprue, other protein allergies, and lymphocytic enterocolitis, but the symptoms of bloating, anemia, positive celiac antibodies, and total villous atrophy and crypt hyperplasia histologically established the diagnosis of celiac disease in this patient.
Celiac disease prevalence in Saudi Arabia has not been reported, but one centre in Riyadh reported a celiac disease incidence of 21% as the etiology in 48 children with chronic diarrhea.14 Our case is challenging in view of the absence of classical abdominal symptoms of celiac disease in a dark-colored woman in an area of low prevalence of the disease. Such complications could have been prevented if she was suspected and thus diagnosed earlier. In a patient with unexplained anemia and thromboembolism with a negative hypercoagulable screen, celiac disease should be considered.
References
- 1.Gorazza GR, Valentini RA, Andreani ML. subclinical Celiac disease id frequent case of Iron deficiency scand. J Gastroenterology. 1995;30:153–156. doi: 10.3109/00365529509093254. [DOI] [PubMed] [Google Scholar]
- 2.Misra RC, Kastheri PI. Adult Celiac disease in tropical. Br Med J. 1966;2:1230. doi: 10.1136/bmj.2.5524.1230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rawashdeh MO, Khalil B, Raweily E. Celiac disease in Arabs. J Pediatr Gastroenterol Nutr. 1996;23(4):415–8. doi: 10.1097/00005176-199611000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Rozen R. molecular genetic aspect of hyperhomocystenemia and its relation to folic acid. Clin Invest Med. 1996 Jun;19(3):171–8. [PubMed] [Google Scholar]
- 5.Welch GN, Loscalzo J. Homocystein and atherothrombosis. N Eng J Med. 1998 Apr 9;338(15):1042–50. doi: 10.1056/NEJM199804093381507. [DOI] [PubMed] [Google Scholar]
- 6.Gabrielli M, Santoliquido A, Gasbarrini G, Pola P, Gasbarrini A. Latent coelic disease, hyperhomocysteinemia and pulmonary thrombolism: a close link? Thrombosis & Haemostasis. 2003 Jan;89(1):203–4. UI 12561813. [PubMed] [Google Scholar]
- 7.Casella G, Perego D, Baldini V, Monti C, Crippa S, Buda CA. A rare association between ulcerative colitis (UC), Celiac disease (CD), membranous glomerulonephritis, leg venous thrombosis, and heterozygosity for factor V Leiden. Journal of Gastroenterology. 2002;37(9):761–2. doi: 10.1007/s005350200126. UI:12375154. [DOI] [PubMed] [Google Scholar]
- 8.Durlach J. [Celiac disease, magnesium deficiency and venous thrombosis]. Presse Medicale. 2001 May 19;30(18):904. [French] [Letter] UI: 11413850. [PubMed] [Google Scholar]
- 9.Grigg AP. Deep venous thrombosis as the presenting feature in a patient with coelic disease and homocysteinaemia. Australian and New Zealand Journal of Medicine. 1999 Aug;29(4):566–7. doi: 10.1111/j.1445-5994.1999.tb00764.x. UI 10868541. [DOI] [PubMed] [Google Scholar]
- 10.Hida M, Erreimi N, Ettair S, Mouane N, Bouctha F. [Associated celiac disease and venous thrombosis]. Archives de pediatrie. 2000 Feb;7(2):215–6. doi: 10.1016/s0929-693x(00)88097-5. [French] UI: 10701071. [DOI] [PubMed] [Google Scholar]
- 11.El Younsi S, Nassif T, Kouch V, Boytchev I, Pelletier G, Buffet C. [Associated of Budd-Chiari syndrome and celiac disease]. Gastroenterologie Clinique et Biologique. 2003 Feb;27(2):236–7. [French] Ui 12658136. [PubMed] [Google Scholar]
- 12.Aguirrebarrena G, Pulcineli S, Giovannoni AG, Gidekel L. [Celiac disease and Budd-Chiari syndrome:infrequent association]. Revista Espanola de Enfermedades Digestivas. 2001 Sep;93(9):611–2. [Spanish] [PubMed] [Google Scholar]
- 13.Andres E, Pflumio F, Knab MC, Muller M, Ott C, Ubrich M, Baumann R, Geisler F. [Splenic thrombosis and celiac disease: a fortuitous association?]. Presse Medicale. 2000 Nov 18;29(35):1933–4. [French] UI: 11244621. [PubMed] [Google Scholar]
- 14.Abdullah AM. Aetiology of chronic diarrhea in children :experience at King Khalid University Hospital, Riyadh. Ann Trop Paediater. 1994;14(2):111–7. doi: 10.1080/02724936.1994.11747702. [DOI] [PubMed] [Google Scholar]