Abstract
BACKGROUND
Little attention has been paid to the problem of male osteopororsis in Saudi Arabia. In this prospective study we assessed the prevalence of male osteoporosis among Saudi Arabs.
SUBJECTS AND METHODS
We studied Saudi Arabian males > 50 years of age attending outpatient clinics at King Fahd Hospital of the University, Al-Khobar, between 1 May 2005 and 30 January 2006. We determined body mass index (BMI) and tests were done to rule out secondary osteoporosis. All subjects had a bone mineral density (BMD) measurement of the hip area and the lumbar spine using dual energy X-ray absorptiometry (DEXA). A T-score of ≤−2.5 SD that of young, healthy adults was taken as osteoporotic and scores between −1 to −2.5 SD were taken as osteopenic.
RESULTS
One hundred fifteen patients (mean age, 61.8±0.75 years; range, 50 to 76 years) had a mean BMI of 24.7±0.35 (range, 18.5 to 31). Based on hip scans, the prevalence of osteoporosis was 24.3%. Sixty-four percent were osteopenic. Based on scans of the lumbar spine, the prevalence of osteoporosis was 37.4% and 33.9% were osteopenic. Spinal osteoporosis was more common than hip osteoporosis.
CONCLUSIONS
Our study indicates that the prevalence of osteoporosis among Saudi Arabian males is higher than among Western males. More studies are needed to determine the national prevalence of male osteoporosis. It is recommended that serious measures to be undertaken to prevent male osteoporosis to stop any future epidemic of catastrophic osteoporosis-related fractures.
Osteoporosis is simply weakness in the bone due to an imbalance between bone formation and resorption. This leads to architectural failure on minimal trauma, causing a fracture. According to the World Health Organization, 55% of the people over the age of 50 years in the USA suffer from osteoporosis.1 Initial studies focused on postmenopausal women as the main group suffering from osteoporosis due to cessation of estrogen at menopause. Reports indicate an incidence of postmenopausal osteoporosis (PMO) of 30% to 40% with over 60% having some degree of osteopenia.2 In Saudi Arabian women the incidence of PMO is reportedly higher in comparison to women in Western countries.3–7 Early diagnosis and treatment of osteoporosis can prevent osteoporosis-related fractures (ORF), thus decreasing morbidity and mortality in those who suffer from osteoporosis. The prevalence of PMO among Saudi Arabian females was underestimated in the past. It took the arrival of the new millennium to accept the reality. The situation appears similar in studying the prevalence of osteoporosis among the male population of Saudi Arabia. In the midst of all the attention given to PMO and its related complications it was never envisaged that osteoporosis among males could become a future problem. The aim of this prospective study was to assess the prevalence of osteoporosis among Saudi Arabian males over the age of 50 years, using bone mineral density measurements.
Subjects and Methods
This study was conducted at King Fahd Hospital of the University, Al-Khobar, Saudi Arabia between 1 May 2005 and 30 January 2006. Saudi Arabian males older than 50 years of age, attending outpatient orthopedic and internal medicine clinics, every second male patient over the age of 50 years was screened for osteoporosis by BMD measurement. After obtaining verbal consent to participation, a detailed history was recorded with emphasis on previous fractures, diseases and the present complaint for which the patient was attending the clinic. Weight and height was recorded to calculate the body mass index (BMI). Investigations to rule out secondary causes of osteoporosis included a complete blood picture and serum calcium, phosphorous, alkaline phosphatase, thyroid stimulating hormone (TSH), follicle stimulating hormone (FSH), leutinizing hormone (LH), testosterone and estrogen levels. The BMD of the hip and the lumbar spine was measured using dual energy x-ray absorptiometry (DEXA) (Hologic Inc., Waltham, MA, USA). The data were entered in the database and analyzed using the SPSS package. Patients with a T-score of ≤−2.5 standard deviations from the mean for healthy, young adults were taken as osteoporotic and those between −1 to −2.5 SD were taken as osteopenic for assessment of fracture risk.1
Results
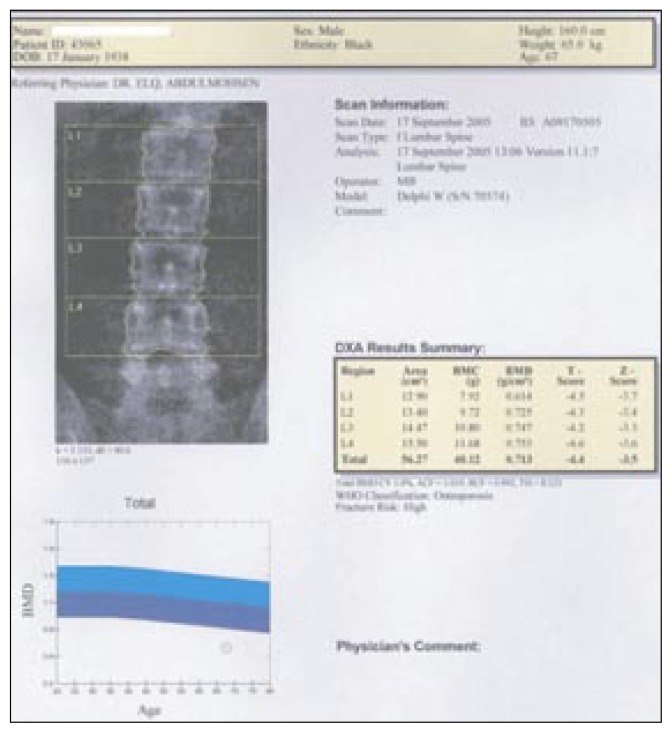
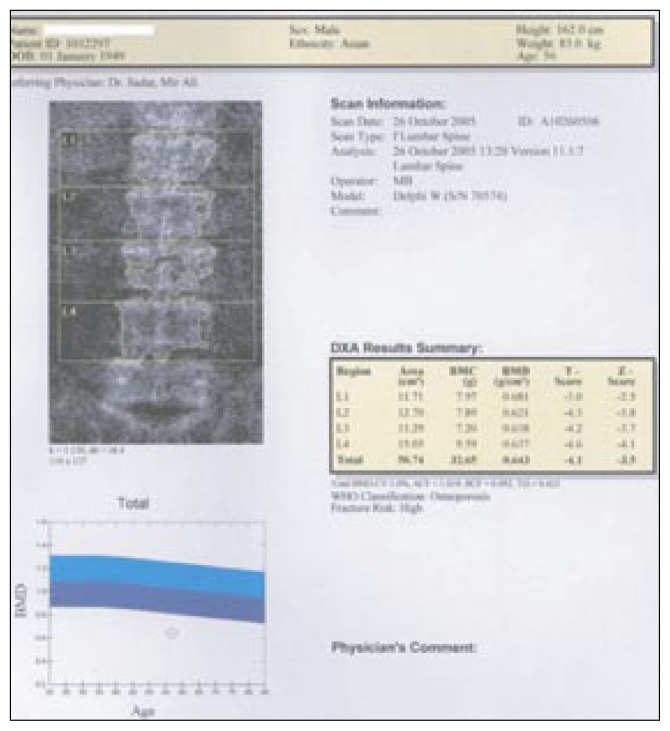
We were able to analyze the data of 115 patients, who had an average age of 61.8±0.75 years (range, 50 to 76 years) and a mean BMI of 24.7±0.35 (range, 18.5 to 31). Analysis of the scans of the hip revealed that 28 (24.3%) of the subjects were osteoporotic, with an average BMD of 0.786±0.01 g/cm2 (range, 0.724 to 0.0.821 g/cm2) and a mean T-score of −3.06±0.04 (−2.9 to −3.2). Sixty-four (55.6%) were osteopenic, with an average BMD of 0.922±0.012 g/cm2 (range, 0.836 to 1.051 g/cm2) and a mean T-score of −1.83±0.06 (range, −1.1 to −2.5) (Table 1). Analysis of BMD of the lumbar spine showed that 43 (37.4%) had osteoporosis, with a mean T-score of −3.45±0.28 (range, −2.7 to −5.1) and 39 (33.9%) were osteopenic with a T-score of −1.78±0.07 (−1.0 to −2.5) (Table 2). Spinal osteoporosis was more common than osteoporosis in the hip region (37.4% versus 24.3%). Figures 1 and 2 show two typical DEXA scans.
Table 1.
Demographic data and BMD of the hip for 115 Saudi males.
| Normal (Group A) | Osteopenic (Group B) | Osteoporotic (Group C) | P value | |
|---|---|---|---|---|
| Number of subjects (%) | 23 (20.1) | 64 (55.6) | 28 (24.3) | |
| Age | 60.6±4.3 (55 to 70) | 60.2±6.5 (51 to 70) | 65.2±8.8 (50 to 76) | NS |
| BMI | 27.1±4.2 (20 to 30.9) | 24.3±3.4 (18.5 to 34.5) | 23.6±3.4 (18.4 to 28.9) | Between Group A and B: P<0.01 Group A and C: P<0.001 |
| Screened area in centimeters | 36.6±2.6 (33.3 to 40.6) | 34.3±3.1 (26.7 to 41.8) | 38.2±9.9 (26.7 to 61.3) | NS |
| BMC g/cm | 38.2±5.8 (31.2 to 50.5) | 32.4±2.9 (21.9 to 39.4) | 32.9±6.1 (18.2 to 50.1) | Between Group A and B: P<0.01. Group A and C: P<0.001 |
| BMD g/cm2 | 1.052±0.107 (0.927 to 1.326 | 0.936±0.050 (0.863 to 1.065) | 0.837±0.040 (0.697 to 0.936) | Between Group A and B: P<0.01. Group B and C: P<0.001 |
| T-score | 0.43±0.66 (−1.0 to 0.8) | −1.6±0.36 (−1.1- to 2.5) | −2.8±0.27 (−2.5 to −3.4) | Not tested |
| Z-score | 0.53±1.02 (−0.9 to 2.8) | −0.65±0.62 (0.9 to −2.3) | −1.2±0.63 (−1 to −2.3) | Not tested |
Values are mean±standard deviation and range. BMI = body mass index, BMC = bone mineral content, BMD = bone mineral density
Table 2.
Demographic data and BMD of the spine for 115 Saudi males.
| Normal (Group A) | Osteopenic (Group B) | Osteoporotic (Group C) | P value | |
|---|---|---|---|---|
| Number of subjects (%) | 26 (20.5) | 47 (37) | 54 (42.5) | |
| Age | 60.0±4.06 (55 to 70) | 59.9±6.82 (51 to 72) | 63.2±8.2 (50 to 76) | NS |
| BMI | 27.4±3.1 (20.5 to 31.5) | 25.3±3.6 (19.5 to 35.5) | 22.7±3.0 (18.4 to 28.9) | Between Group A and B: P was NS Group A and C: P<0.001 |
| Area screened In centimeters | 65.9±4.1 (60.4 to 75.0) | 61.5±6.0 (49.3 to 71.5) | 57.5±5.6 (47.1 to 67.7) | NS |
| BMC g/cm | 69.4±5.1 (61.1 to 76.9) | 59.0±2.9 (41.5 to 72.9) | 44.7±9.2 (29.9 to 56.8) | Between Group A and B: P<0.01. Group A and C: P<0.001 |
| BMD g/cm2 | 1.063±0.040 (1.006 to 1.123) | 0.956±0.050 (0.862 to 1.050) | 0.765±0.10 (0.527 to 0.931) | Between Group A and B: P<0.01. Group B and C: P<0.001 |
| T-score | −0.4±0.52 (0.3 to −1) | −1.9±0.33 (−1.3 to −2.5) | −3.4±0.74 (−2.7 to −5.1) | Not tested |
| Z-score | 0.45±0.48 (−0.2 to −1) | −1.04±0.34 (−03 to −1.6) | −2.14±0.89 (−1.5 to −4.8) | Not tested |
Values are mean±standard deviation and range. BMI = body mass index, BMC = bone mineral content, BMD = bone mineral density
Figure 1.
DEXA scan of a 67-year-old Saudi male with osteoporosis.
Figure 2.
DEXA Scan of a 56-year-old Saudi male with osteoporosis.
Discussion
Osteoporosis is a major health care problem in developed and developing countries. Western nations spend billions of dollars on the complications of postmenopausal osteoporosis. The focus until now has been on postmenopausal women without realization that males can also develop osteoporosis to the extent that fractures occur.8–10 Looker and his associates11 assessed the incidence of osteoporosis in men and reported that men suffer from osteoporosis in the range of 3% to 6% and osteopenia up to 47%. In this study we found that 27.6% of Saudi Arabian men with an average age of 60 years suffered from osteoporosis and 57.5% were osteopenic, which is significantly higher in comparison to their counterparts in the Western world. In 2004, the Osteoporosis Working Group at King Faisal Specialist Hospital and Research Center recommended that once osteoporosis is diagnosed in men, secondary causes need to be excluded.12 Our study population might appear to be a selective hospital group of patients, but every attempt was made to exclude secondary osteoporosis by means of a detailed history, clinical examination and relevant investigations.
The objective of early diagnosis and treatment of osteoporosis is to prevent low trauma fractures. It is estimated that the lifetime risk of fracture at 50 years is 17% to 22.5% in women and 6% to 11% in men,13–14 with higher rates of hospitalization and institutionalization after osteoporotic fractures in men than in women.15 It has been projected that the incidence of hip fractures by 2050 will range between 7 to 21.3 million and men will have more fractures than women.16 Poor and his associates17 found that inactivity and obesity increase the risk of fractures in men many-fold, and Kanis and colleagues, after the MEDOS study, reported that low exposure to sunlight and decreased physical activity were the highest attributable risk factors for fractures.18 At present, the incidence of ORF is low in men but the 12-month mortality in men after ORF is twice that of women.19–20 Thus, it appears that the risk of osteoporosis in women got more attention and that the risk of osteoporosis in men has been neglected, even though the morbidity and mortality in men remains higher.
In Saudi Arabia the problem of postmenopausal osteoporosis took over a decade and a half to be acknowledged, as Sadat-Ali et al21 suggested in 1992 that there was a high prevalence of osteoporosis in postmenopausal women and a high incidence of ORF. This clinical study is probably the first study to report on osteoporosis in men of older than 50 years, showing the reluctance of physicians in Saudi Arabia to study male osteoporosis in Saudi Arabia. The population in Saudi Arabia is aging and in the coming decades the percentage of elderly men and women will increase thereby increasing the population at risk for developing osteoporosis and ORFs.
In conclusion, we believe that the prevalence of osteoporosis in Saudi men is higher than in men in the Western world. More needs to be done in advocating prevention by avoiding risk factors like sedentary lifestyle, non-exposure to sunlight, and cigarette smoking. Patients who are already osteoporotic and osteopenic should be adequately treated to reduce or prevent osteoporosis-related fractures.
References
- 1.National Osteoporosis Foundation. America’s Bone Health: The State of Osteoporosis and Low Bone Mass in Our Nation. Washington DC: National Osteoporosis Foundation; 2002. [Google Scholar]
- 2.Ullom-Minnich P. Prevention of osteoporosis and fractures. Am Fam Physician. 1999;60:194–202. [PubMed] [Google Scholar]
- 3.Sadat-Ali M, Al-Habdan I, Al-Mulhim FA, El-Hassan AY. Effect of parity on bone mineral density among postmenopausal Saudi Arabian women. Saudi Med J. 2005;26:1588–90. [PubMed] [Google Scholar]
- 4.Sadat-Ali M, Al-Habdan I, Al-Mulhim FA, El-Hassan AY. Bone mineral density among postmenopausal Saudi women. Saudi Med J. 2004;25:1623–25. [PubMed] [Google Scholar]
- 5.El-Desouki M. Osteoporosis in postmenopausal Saudi women using dual x-ray bone densitometry. Saudi Med J. 2003;24(9):953–56. [PubMed] [Google Scholar]
- 6.Sadat-Ali M, Al-Habdan I, Marwah S. Bone mineral density measurement of distal radius in Saudi Arabian females. Ann Saudi Med. 1996;16:414–16. doi: 10.5144/0256-4947.1996.414. [DOI] [PubMed] [Google Scholar]
- 7.El-Desouki M. Bone mineral density of the spine and femur in the normal Saudi population. Saudi Med J. 1995;16:30–35. [PubMed] [Google Scholar]
- 8.Bilezikian JP. Osteoporosis in men. J Clin Endocrinol Metab. 1999;84:3431–34. doi: 10.1210/jcem.84.10.6060. [DOI] [PubMed] [Google Scholar]
- 9.Seeman E. Osteoporosis in men. Osteoporosis Int. 1999;(9 suppl2):S97–S110. doi: 10.1007/pl00004168. [DOI] [PubMed] [Google Scholar]
- 10.Orwoll ES. Osteoporosis in men. Endocrinol Metab Clin North Am. 1998;27:349–67. doi: 10.1016/s0889-8529(05)70009-8. [DOI] [PubMed] [Google Scholar]
- 11.Looker AC, Orwoll ES, Johnston CC, Jr, Lindsay RL, Wahner HW, Dunn WL, et al. Prevalence of low femoral bone density in older US adults from NHANES III. J Bone Miner Res. 1997;12(11):1769–71. doi: 10.1359/jbmr.1997.12.11.1761. [DOI] [PubMed] [Google Scholar]
- 12.Raef H, Frayha HH, El-Shaker M, Al-Humaidan A, Conca W, Sieck U, et al. Recommendations for the diagnosis and management of osteoporosis: A local Perspective. Ann Saudi Med. 2004;24(4):242–52. doi: 10.5144/0256-4947.2004.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Melton LJ, Kan SH, Wahner HW, Riggs BL. Lifetime fracture risk: An approach to hip fracture risk assessment based on bone mineral density and age. J Clin Epidemiol. 1988;41(10):985–94. doi: 10.1016/0895-4356(88)90036-4. [DOI] [PubMed] [Google Scholar]
- 14.Oden A, Dawson A, Dere W, Johnell O, Jonsson B, Kanis JA. Lifetime risk of hip fractures is underestimated. Osteoporosis Int. 1998;8(6):599–603. doi: 10.1007/s001980050105. [DOI] [PubMed] [Google Scholar]
- 15.Reginster JY, Gillet P, Ben Sedrine W, Brands G, Ethgen O, de Froidmont C, et al. Direct costs of hip fractures in patients over 60 years of age in Belgium. Pharmacoeconomics. 1999;15:507–14. doi: 10.2165/00019053-199915050-00008. [DOI] [PubMed] [Google Scholar]
- 16.Gullberg B, Johnell O, Kanis J. World-wide projections for hip fracture. Osteoporosis Int. 1997;7:407–13. doi: 10.1007/pl00004148. [DOI] [PubMed] [Google Scholar]
- 17.Poor G, Atkinson EJ, O’Fallon WM, Melton LJ., III Prediction of hip fractures in elderly men. J Bone Miner Res. 1995;10:1900–7. doi: 10.1002/jbmr.5650101209. [DOI] [PubMed] [Google Scholar]
- 18.Kanis J, Johnell O, Gullberg B, Elfforts L, Allander E, Ranstam J, et al. Risk factors of hip fracture in men from Southern Europe: the MEDOS study. Osteoporosis Int. 1999;9:45–54. doi: 10.1007/s001980050115. [DOI] [PubMed] [Google Scholar]
- 19.Kaufman JM, Johnell O, Abadie E, Adami S, Audran M, Avounac B, et al. Background for studies on the treatment of male osteoporosis: State of the art. Ann Rheum Dis. 2000;59(10):765–72. doi: 10.1136/ard.59.10.765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jacobsen SJ, Goldberg J, Miles TP, Brody JA, Steirs W, Rimm AA. Race and sex differences in mortality following fracture of the hip. Am J Public Health. 1992;82(8):1147–50. doi: 10.2105/ajph.82.8.1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sadat-Ali M, El-Hassan AY, Ibrahim EM, Al-Frehi H, Al-Mohanna F. Postmenopausal osteoporosis in Saudi women. A pilot screening with 2-year follow up. Proceedings of the 1st World G.C.C. Orthopaedic Conference; 1992; January 18–23rd; Oman, Muscat. [Google Scholar]