Abstract
BACKGROUND AND OBJECTIVES
Because there is no recent update on the state of diabetes and its concomitant complications in Saudi Arabia, we undertook a study of the prevalence of health complications in patients with type 2 diabetes mellitus admitted to our institution.
METHODS
We conducted a retrospective review of medical records of adult Saudi patients with type 2 diabetes who were seen in clinics or admitted to the Security Forces Hospital, Riyadh, Saudi Arabia, between January 1989 and January 2004.
RESULTS
Of 1952 patients, 943 (48.3%) were males. For the whole study population the mean age at enrollment was 58.4±14.2 years, the mean age at onset of diabetes was 48.1±12.8 years, the mean duration of diabetes was 10.4±7.5 years, and the mean duration of follow-up was 7.9±4.6 years. Nephropathy was the most prevalent complication, occurring in 626 patients (32.1%). Acute coronary syndrome occurred in 451 (23.1%), cataracts in 447 (22.9%), retinopathy in 326 (16.7%), and myocardial infarction in 279 (14.3%), Doubling of serum creatinine was seen in 250 (12.8%) and 79 (4.0%) went into dialysis. Hypertension was present in 1524 (78.1%) and dyslipidemia in 764 (39.1%). Overall mortality was 8.2%. Multiple complications were frequent. Males had higher prevalence of complications than females (P<.05). Mortality was significantly higher in males 92 (9.8%) than females 69 (6.8%) (P=.024). The prevalence of complications significantly increased with duration of diabetes and age (P<.05).
CONCLUSION
Among Saudis, the prevalence of concomitant diabetic complications is high, with cardiovascular and renal complications the most frequent. Many patients had multiple complications. Early and frequent screenings in the patients with type 2 diabetes are desirable to identify patients at high risk for concomitant complications and to prevent disabilities.
Patients with diabetes have an increased risk of complications of macrovascular (stroke, myocardial infarction, and coronary artery disease) and microvascular disease (retinopathy, nephropathy and neuropathy), which if undetected or left untreated can have a devastating impact on quality of life and a significant financial burden. A community-based national epidemiological health survey (1995–2000) reported a 23.7% prevalence of diabetes mellitus among Saudi adults between the ages of 30 to 70 years.1 A review of the literature indicates a rising trend in the incidence of diabetes mellitus in recent decades in Saudi Arabia.2–8
Complications due to long standing diabetes mellitus are a major public issue worldwide due to significantly higher morbidity and mortality rates associated with the disease. Furthermore, since optimization of treatment time has an impact on the outcome of life-threatening complications, frequent screenings are important. Prevalence reports from studies worldwide on microvascular and macrovascular complications of type 2 diabetes show varying rates. The prevalence of cataracts is 26% to 62%,9 retinopathy 17% to 50%, with 11% to 36% background retinopathy, and 1.7% to 3% proliferative retinopathy,9–12 blindness 3%,10 nephropathy 17% to 28%,13,14 cardiovascular complications 10% to 22.5%,15–19 stroke 6% to 12%,20,21 neuropathy 19% to 42%,17,20,22 and foot problems 5% to 23%.19 Mortality from all causes was reported as being between 14% to 40%.19 A 1992 study from Saudi Arabia showed that cataract was present in 42.7%, neuropathy in 35.9%, retinopathy in 31.5%, hypertension in 25%, nephropathy in 17.8%, ischemic heart disease in 41.3%, stroke in 9.4%, foot infections in 10.4% and amputations in 5.1% of patients with type 2 diabetes.23 However, this study reported complications for both types of diabetes. Studies on diabetic complications conducted in Saudi Arabia are very few and restricted. Furthermore, there is no recent update on the state of diabetes and its concomitant complications in Saudi Arabia, and therefore we undertook the present study to determine the prevalence of health complications in patients with type 2 diabetes in our institution.
METHODS
From the computer database of the Security Forces Hospital, all patients with the diagnosis of type 2 diabetes who were seen in clinics or admitted to the hospital, and followed between January 1989 and January 2004 were extracted. From these, only those with active follow-up visits within 6 months from the time of review were included in the analysis. Patients who were diagnosed with gestational diabetes, type 1 diabetes, recently diagnosed diabetics with <6 months follow-up and pediatric patients were excluded from the study. A retrospective review and collection of all pertinent data were conducted including baseline characteristics of age, gender, duration of diabetes, body mass index, blood pressure, and available laboratory results.
The presence of concomitant diabetic complications was determined by retrospective diagnosis, noting the date of onset, age at complication and other pertinent data associated with such complications. Hypertension was based on a preexisting history of hypertension and measurement of BP where systolic BP was considered an SBP >130 mm Hg and/or a DBP >80 mm Hg based on the seventh report of the Joint National Committee on the Prevention, Detection, Evaluation and Treatment of High Blood Pressure ( JNC 7). BP measurements from at least 4 readings per year were recorded as mean BP/year. Body mass index (BMI) was calculated from the formula weight (kg)/height (m2), with a value from 25 to >30 considered overweight and a value ≥30 considered obese. Cataract and retinopathy included findings of nuclear sclerosis for cataracts and the presence of retinal hemorrhages, exudates and macular edema for retinopathy. Neuropathy was considered if there was persistent numbness, paresthesia, loss of a tuning fork tested sense of vibration, or failure to elicit knee and/or ankle jerk reinforcement. Nephropathy was defined by the presence of positive persistent proteinuria by urinary dipstick with at least 3 readings per year and/or serum creatinine of more than 130 μmol/L or a glomerular filtration rate by Cockcroft-Gault of <60 mL/min. Data on microalbuminuria was not available. The presence of acute coronary syndrome (ACS) and myocardial infarction (MI) were based on clinical, electrocardiographic, biochemical and angiographic evidence of myocardial ischemia presenting as angina and/or MI. Stroke was supported by clinical or radiodiagnostic evidence (CT scan) of cerebrovascular accident. All values were taken at the initial visit, yearly and at a last visit and summarized as mean±standard deviation for yearly results.
Data management and analysis were conducted using Statistical Package for Social Sciences (SPSS) program 11.5 version. Continuous variables are presented as mean±SD whereas categorical variables are presented as numbers and percentages. The t test was used to compare means. The Chi-square test was used to compare categorical variables. A P value of <.05 was considered statistically significant.
RESULTS
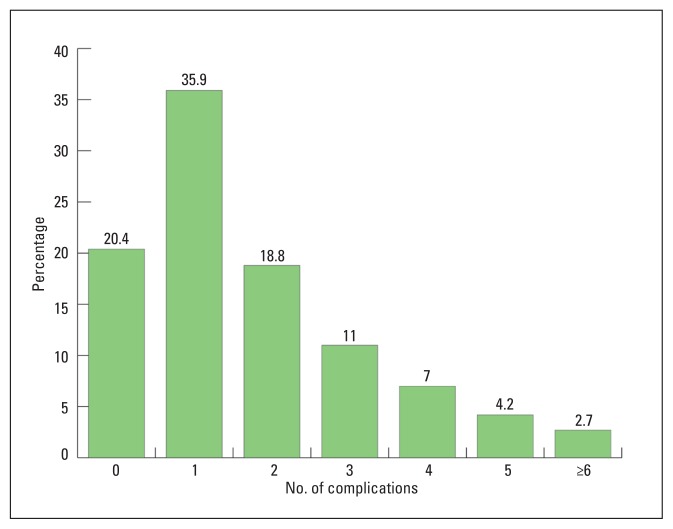
Of 1952 patients in the study population, 943 (48.3%) were males and 1009 (51.7%) females. Table 1 shows the general characteristics of the population, including age at time of enrollment, age at onset of diabetes, duration of diabetes, and duration of follow-up. A family history of diabetes was documented in 846 patients (43.3%). Most patients were overweight or obese. Table 2 shows the frequencies of diabetic complications. Hypertension, nephropathy and ACS were the most prevalent followed by cataracts, retinopathy, MI, neuropathy, and stroke. The mortality rate from all causes was 8.2%. The prevalence of multiple complications is shown in Figure 1. Advanced age and a long duration of diabetes were significantly associated with the prevalence of diabetes complications (Table 3). Regression analysis showed that duration of diabetes has a greater influence on the prevalence of complications than age or sex (Table 4). ACS and MI occurred as early as 30 years of age, but the prevalence of these complications was higher in older patients and in patients with a longer duration of diabetes (Table 3). Arrhythmia and atrial fibrillation appeared the earliest, at 10.1±7.2 years and 10.6±7.1 years, respectively, from the diagnosis of diabetes. Blindness was the last to appear, at 16.3±6.9 years from the onset of diabetes. Complications of diabetes occurred as early as 1 to 4 years from the diagnosis of diabetes. The prevalence of complications increased with duration of diabetes, becoming more prevalent when duration of diabetes was more than 20 years (Table 3).
Table 1.
General characteristics of 1952 type 2 diabetic patients from a tertiary care hospital in Saudi Arabia.
| Characteristic | |
|---|---|
| Age at time of enrollment (years) | 58.39±14.2 (15–100) |
| Duration of follow-up and range (years) | 7.88±4.57 (1–18) |
| Age of onset of diabetes and range (years) | 48.07±12.8 (13–95) |
| Duration of diabetes and range (years) | 10.41±7.45 (1–40) |
| Age of onset by decade (years) | |
| ≤30 | 171 (8.8%) |
| 31–40 | 394 (20.2%) |
| 41–50 | 562 (28.8%) |
| 51–60 | 493 (25.3%) |
| 61–70 | 244 (12.5%) |
| 71–80 | 78 (4.0%) |
| >80 | 10 (0.5%) |
| Positive family history of diabetes | 846 (43.3%) |
| Body mass index and range | |
| At initial visit | 29.89±5.03 (15.37–54.27) |
| At last visit | 29.33±4.85 (16.4–53.37) |
| BMI category at last visit | |
| Overweight | 762 (39.0%) |
| Obese | 874 (44.8%) |
| Normal | 306 (15.7%) |
| Underweight | 10 (0.5%) |
Data are mean and standard deviation, or numbers and percentages of patients.
Table 2.
Frequencies of diabetic complications and comorbidities among type 2 diabetics (n=1952).
| Complications and comorbidities | n (%) | Age of onset of diabetes | Age at onset of complication/comorbidity | Duration of diabetes at the time of complication |
|---|---|---|---|---|
| Hypertensiona | 1524 (78.07) | 49.1±12.4 (22–91) | 60.5±12.4 (22–95) | 11.6±7.4 (1–40) |
| Nephropathyb | 626 (32.1) | 51.6±12.3 (19–83) | 61.6±12.4 (22–95) | 12.6±6.8 (1–35) |
| Acute coronary syndromec | 451 (23.1) | 50.8±12.4 (20–86) | 62.6±12.4 (22–95) | 12±7.1 (1–37) |
| Cataract | 447 (22.9) | 51.0±11.1 (20–86) | 63.4±9.5 (33–96) | 12.4±6.5 (1–38) |
| Myocardial infarction | 279 (14.3) | 49.6±12.4 (20–86) | 63.3±12.5 (24–92) | 13.5±7.3 (1–39) |
| Peripheral neuropathyd | 268 (13.7) | 49.9±11.9 (19–79) | 58.6±12.1 (33–88) | 10.9±5.6 (1–27) |
| Background retinopathy | 223 (11.4) | 48.5±10.3 (19–78) | 62.8±9.5 (33–86) | 14.3±5.9 (1–38) |
| Strokee | 203 (10.4) | 50.3±12.0 (21–80) | 62.2±12.2 (24–95) | 12.0±6.8 (1–28) |
| Proliferative retinopathy | 103 (5.3) | 48.8±10.3 (26–83) | 64±8.8 (43–87) | 15.5±4.5 (4–28) |
| Foot infections | 83 (4.3) | 48.2±12.7 (19–72) | 60.8±9.2 (30–88) | 13.5±6.7 (1–28) |
| Amputations | 38 (1.9) | 46.1±11.6 (25–70) | 62.1±9.5 (33–95) | 15.5±6.2 (2–26) |
| Atrial fibrillation | 34 (1.7) | 55.6±15.0 (26–91) | 67.1±14.7 (31–97) | 10.6±7.1 (1–21) |
| Blindness | 23 (1.2) | 52.4±18.8 (22–91) | 70.3±12.6 (47–88) | 16.3±6.9 (5–28) |
| Arrhythmiaf | 18 (0.9) | 49.6±14.4 (21–67) | 59.5±18.8 (24–87) | 10.1±7.2 (1–20) |
| Death | 161 (8.2) | 53.1±12.2 (24–91) | 68.3±11.6 (34–97) | 15.3±8.3 (1–39) |
Data are mean±standard deviation and range in years.
At last visit 1437 (73.6%) patients were receiving anti-hypertensive medication.
250 patients (39.9%) had a doubling of serum creatinine, 95 (15.2%) developed end-stage renal disease, and 79 (12.6%) were on dialysis.
14 patients (77.8%) had a positive stress test; in 12 patients (66.7%) an acute coronary syndrome was the initial event.
Foot ulcers developed in 43 (16%) after duration of diabetes of 20.5±4.5 years or 8 or 9 years after start of neuropathy; 28 (10.4%) had a limb amputation 20.8±5.8 years from onset of diabetes or 1–2 years (median, 1.5 years) from appearance of foot ulcers and foot infections.
165 (81.3%) thrombotic-ischemic, 35 (17.2%) hemorrhagic, 3 (1.5%) due to infection; 181 (58.1%) single episode, 17 (8.4%) 2 episodes, 3 (1.5%) 3 episodes, 2 (1.0%) 4 episodes. There were 62 (66.7%) reported deaths due to stroke.
239 patients (53%) developed MI approximately 1–1.5 years from onset of chest pain.
Figure 1.
Number of complications among patients with type 2 diabetes (including nephropathy, background retinopathy, proliferative retinopathy, acute coronary syndrome, diabetic foot, neuropathy, stroke and hypertension).
Table 3.
Frequencies of diabetic complications according to duration of diabetes among type 2 diabetics (n=1952).
| Complications | n (%) | Duration of diabetes in years | |||||
|---|---|---|---|---|---|---|---|
| 1–4 (n=521) (26.7%) |
>4–8 (n=426) (21.8%) |
>8–12 (n=337) (17.3%) |
>12–16 (n=237) (12.1%) |
>16–20 (n=213) (10.9%) |
>20 (n=218) (11.2%) |
||
|
| |||||||
| Mean(±SD) age of patients at diagnosis of diabetes (range) | 1952 | 47.5±14.3 (18–83) |
49.2±13.8 (18–95) |
50.6±12.7 (18–85) |
49.1±10.7 (20–77) |
46.5±10.4 (21–75) |
43.9±10.0 (19–70) |
|
| |||||||
| Mean (±SD) age of patients at enrollment (range) | 1952 | 50.0±14.4 (19–86) |
55.4±13.8 (24–100) |
60.8±12.7 (28–95) |
63.5±10.6 (33–90) |
65.1±10.7 (32–95) |
68.6±9.4 (46–96) |
|
| |||||||
| Cataract | 447 (22.9) | 46 (8.83) | 41(9.6) | 60 (17.8) | 85 (35.86) | 102 (47.89) | 113 (51.83) |
|
| |||||||
| Background retinopathy | 223 (11.4) | 13 (2.5) | 6 (1.41) | 21 (6.23) | 46 (19.41) | 55 (25.82) | 82 (37.61) |
|
| |||||||
| Proliferative retinopathy | 103 (5.3) | 2 (0.38) | 5 (1.17) | 6 (1.78) | 15 (6.33) | 21 (9.86) | 54 (24.77) |
|
| |||||||
| Blindness | 23 (1.2) | - | 3 (0.7) | 2 (0.59) | 2 (0.84) | 5 (2.35) | 11 (5.05) |
|
| |||||||
| Persistent proteinuria | 450 (23.1) | 22 (4.22) | 46 (10.8) | 73 (21.66) | 83 (35.02) | 97 (45.54) | 129 (59.17) |
|
| |||||||
| Acute coronary syndrome | 451 (23.1) | 46 (8.8) | 71 (16.67) | 73 (21.66) | 81 (34.18) | 85 (39.91) | 95 (43.58) |
|
| |||||||
| Myocardial infarction | 279 (14.3) | 20 (3.84) | 31 (7.28) | 40 (11.87) | 47 (19.83) | 63 (29.58) | 78 (35.78) |
|
| |||||||
| Neuropathy | 268 (13.7) | 18 (3.45) | 27 (6.34) | 32 (9.5) | 53 (22.36) | 59 (27.7) | 79 (36.24) |
|
| |||||||
| Stroke | 203 (10.4) | 21 (4.03) | 18 (4.23) | 39 (11.57) | 42 (17.72) | 35 (16.43) | 48 (22.02) |
|
| |||||||
| Death | 161 (8.2) | 21 (4.03) | 18 (4.23) | 23 (6.82) | 23 (9.7) | 32 (15.02) | 44 (20.18) |
Table 4.
Regression analysis showing the contribution of age and duration of diabetes on some concomitant complications.
| Diabetic complications | n | Age | Duration of diabetes | ||
|---|---|---|---|---|---|
| Beta | P value | Beta | P value | ||
|
| |||||
| Background retinopathy | 223 | .05 | .03 | .352 | <.0001 |
|
| |||||
| Cataract | 447 | .17 | <.0001 | .304 | <.0001 |
|
| |||||
| Proliferative retinopathy | 103 | .039 | .111 | .27 | <.0001 |
|
| |||||
| Myocardial infarction | 279 | .087 | <.0001 | .277 | <.0001 |
|
| |||||
| Stroke | 203 | .084 | .001 | .167 | <.0001 |
|
| |||||
| Diabetic nephropathy | 626 | 0.161 | <.0001 | 0.02 | .312 |
|
| |||||
| Neuropathy | 268 | 0.073 | .005 | 0.253 | <.0001 |
There were significant differences in the prevalence of some concomitant diabetic complications between male and female patients. Mean age at onset of complications was significantly earlier among males than females (46.9±13.1 years vs 49.2±12.4 years, P<.0001) Overall, females were less prone to diabetic complications. More males than females had cataracts, background retinopathy, and neuropathy, while more females had hypertension (Table 5). Patient survival was better among females: 92 (9.76%) males died compared with 69 (6.84%) females (P=.024). Duration of diabetes between males (10.7±7.5 years) and females (10.2±7.4 years) was not significantly different (P=.138). Mean age at the onset of diabetes was significantly earlier among females (P<.0001). Male patients developed the complications of diabetes sooner than females; cataract occurred after 11.6±6.7 years of onset of diabetes in males and 13.4±6.2 years after the onset of diabetes in the females (P=.002). Nephropathy appeared significantly earlier among males than females (12.2±6.8 years vs. 14.0±6.8 years, respectively, P=.005), but amputation occurred later (17.9±5.2 years in males vs. 11.6±5.8 years in females, P=.0011). Onset of other complications was not significantly different between males and females.
Table 5.
Frequency of diabetic complications for males and females.
| Complications (%) | All patients | Males | Females | P value |
|---|---|---|---|---|
| Number | 1952 | 943 (48.3) | 1009 (51.7) | |
| Complications | ||||
| Cataract | 447 (22.9) | 243 (25.8) | 204 (20.2) | .004* |
| Background retinopathy | 223 (11.4) | 125 (13.3) | 98 (9.5) | .017* |
| Proliferative retinopathy | 103 (5.3) | 56 (5.94) | 47 (4.66) | .245 |
| Blindness | 23 (1.2) | 12 (1.27) | 11 (1.09) | .8703 |
| Acute coronary syndrome | 451 (23.1) | 236 (25.0) | 215 (21.3) | .058 |
| Myocardial Infarction | 279 (14.3) | 148 (15.7) | 131 (12.98) | .100 |
| Atrial Fibrillation | 34 (1.7) | 14 (1.48) | 20 (1.98) | .507 |
| Arrhythmia | 18 (0.9) | 9 (0.95) | 9 (0.89) | .926 |
| Neuropathy | 268 (13.7) | 156 (16.5) | 112 (11.1) | .001* |
| Foot infections | 83 (4.3) | 46 (4.88) | 37 (3.67) | .225 |
| Amputations | 38 (1.9) | 23 (2.44) | 15 (1.49) | .174 |
| Nephropathy | 626 (32.1) | 294 (31.1) | 332 (32.9) | .2750 |
| Stroke | 203 (10.4) | 110 (11.6) | 93 (9.2) | .898 |
| Death | 161 (8.2) | 92 (9.76) | 69 (6.84) | .024* |
| Co-morbidities | ||||
| Obesity | 1629 (83.45) | 729 (77.3) | 900 (89.2) | <.0001* |
| Dyslipidemiaa | 764 (39.14) | 356 (37.8) | 408 (40.4) | .2247 |
| Hypertensive | 1524 (78.07) | 759 (80.5) | 765 (75.8) | .0127* |
Statistically significant (t-test).
502 (25.7%) taking statins
One hundred sixty-one (8.2 %) patients died in the hospital, including 92 (57.1%) males and 69 (42.8%) females. Cardiovascular-related death was documented in 97 (60.3%) patients, fatal infections in 7 (4.3%) patients, respiratory disease in 12 (7.4%) cancer in 31 (19.3%) and deaths due to miscellaneous reasons in 14 patients (8.7%).
At the last visit, 1077 (55.2%) patients were taking oral hypoglycemic agents alone, 206 (10.6%) were taking insulin alone, 647 (33.1%) patients were taking oral hypoglycemic agents plus insulin and 22 (1.1%) were not taking antidiabetic medication.
DISCUSSION
This study is a comprehensive review of type 2 diabetes complications in a hospital setting in an Arab country. The study reveals that most of the complications of diabetes developed between 10 and 13 years from the onset of diabetes, similar to the findings of Kim et al9 and Chuang.13 Complications were identified as early as 1 to 4 years from diagnosing diabetes, as the onset probably preceded the time of diagnosis by years in many cases. The incidence of complications continued to rise with age and duration of diabetes. Among female Saudi patients, onset of diabetes was significantly earlier than males, but the prevalence of complications was higher among males than females. ACS (seen in 23.1% of our patients) and MI (seen in 14.3%), were higher than in reports from Western countries,14–19 which may be attributed to the relatively sedentary lifestyle of our population, the lack of awareness of the complications of high blood sugar, high blood pressure, dyslipidemia, and a lack of awareness of how to control these diseases. Hypertension was higher in our study compared to the 25% reported by Famuyiwa23 and the 34% by Al-Nozha, but our study population was different from their populations.1 The prevalence of cataracts in our study was lower than in other countries with the same type 2 diabetic population.9–12 Similarly, neuropathy (13.7%) was lower than in other reports, which indicated a prevalence of neuropathy up to 75%.16,18,19 This could be in part due to late screening after the disease is obviously manifested and lack of proper assessment for neuropathy. Our 10.4% prevalence of stroke was relatively high compared to reports from Asia (6%) and Europe (6.3%),16,19,20 but was similar to reports from the UK (2.8%–12.0%).16,18,20 The prevalence of stroke increased to 10.4% in the present study compared to 9.4% reported by Famuyiwa in 1992.23 Nephropathy (32.1% in our study) was almost similar to the 30.4% to 54.3% of Huraib,8 but higher than Famuyiwa.23 Cataract and retinopathy was lower than in Famuyiwa’s report.23
Mortality was low in the present study compared to other studies since we reported only those deaths that occurred in the hospital. Our study reflects that diabetes and its complications have progressed in Saudi Arabia. Not only has the prevalence rate of each complication risen, but multiple complications were also frequent. As many as six or more complications appeared in a single individual in the present study, which should alert physicians to look to other complications as well. A multidisciplinary management covering all comorbidities is desired. Improper diet, minimal physical exercise, sedentary lifestyle and the established cultural belief in consanguinity in the population, over and above a genetic predisposition may have influenced these rising figures. Despite rapid modernization, very few Saudis openly enroll in health and fitness clubs. Another factor is that obesity is very common among Saudi nationals. The ethnic factor should also be considered in the analysis of this problem. There is an urgent need to readdress diabetes and the development of its complications not only through early referral and aggressive management, but also through making people aware that controlling blood sugar, blood pressure, and lipids together with regular exercise can save a person from the dreaded complications of type 2 diabetes mellitus.
The prevalence of concomitant complications of diabetes is high among Saudis. Cardiovascular and renal complications are most frequent. Many patients had multiple complications. Advanced age, longer duration of diabetes, and male gender were the most significant risk factors for diabetes complications. Earlier and frequent screenings in patients with type 2 diabetes are desirable to identify patients at high risk of health complications and to prevent disabilities. Despite the retrospective nature of this study, the lack of data on microalbuminuria to document nephropathy and the hospital-based data collection which could have biased the results, we were able to document the macrovascular and microvascular complications of type 2 diabetes in a large population from a single setting which could jump-start and serve as a reference for future larger scale studies.
REFERENCES
- 1.Al-Nozha MM, Al-Maatouq MA, Al-Mazrou YY, Al-Harthi SS, Arafah MR, Khalil MZ, et al. Diabetes Mellitus in Saudi Arabia. Saudi Med J. 2004;25(11):1603–10. [PubMed] [Google Scholar]
- 2.Al-Nuaim AR, Al-Mazrou Y, Al-Attas O, et al. National Chronic Metabolic Diseases Survey Part I. Ministry of Health and King Saud University; Riyadh, Kingdom of Saudi Arabia: 1995. p. 63. [Google Scholar]
- 3.AlWakeel JS, Mitwalli AH, Abu-Aisha H, Tarif N, Memon N, Sulimani F, et al. Single center experience with pre-dialysis patients. Saudi J Kidney Dis Tranplant. 2002;13(3):363–70. [PubMed] [Google Scholar]
- 4.El-Hazmi MA, Al-Swailem A, Warsy AS, Al-Sudairy F, Sulimani R, Al-Swailem A, et al. Prevalence of diabetes mellitus and impaired glucose tolerance in the population of Riyadh. Ann Saudi Med. 1995;15(6):598–601. doi: 10.5144/0256-4947.1995.598. [DOI] [PubMed] [Google Scholar]
- 5.Warsy AS, El-Hazmi MA. Diabetes mellitus, hypertension and obesity-related common multifactorial disorders in Saudis. East Mediterr Health J. 1999;5(6):1236–42. [PubMed] [Google Scholar]
- 6.Karim A, Ogbeide DO, Siddiqui S, Al-Khalifa IM. Prevalence of diabetes mellitus in a Saudi community. Saudi Med J. 2000;21(5):438–42. [PubMed] [Google Scholar]
- 7.Mohsen A, El-Hazmi F, Warsy AS, Al-Swailem AR, Al-Swailem AM, Sulaimani R. Diabetes mellitus as a health problem in Saudi Arabia. Euro Med Health J. 1998;4(1):58–67. [Google Scholar]
- 8.Huraib S, Abu-Aisha H, Sulimani R, Famuyiwa OO, Alwakeel JS, Askar A, et al. Pattern of Diabetic Nephropathy among Saudi patients with non-insulin dependent diabetes mellitus. Ann Saudi Med. 1995;15(2):120. doi: 10.5144/0256-4947.1995.120. [DOI] [PubMed] [Google Scholar]
- 9.Kim SI, Kim SJ. Prevalence and risk factors for cataracts in persons with type 2 diabetes. Kor J Ophthal. 2006;20:201–4. doi: 10.3341/kjo.2006.20.4.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Al-Till MI, Al-Bdour MD, Ajlouni KM. Prevalence of blindness and visual impairment among Jordanian diabetics. Eur J Ophthal. 2005;15:62–8. doi: 10.1177/112067210501500110. [DOI] [PubMed] [Google Scholar]
- 11.Janghorbani M, Amini M. Cataract in type 2 diabetes mellitus in Isfahan, Iran: incidence and risk factors. Ophthalmic Epidemiol. 2004;11:347–58. doi: 10.1080/09286580490888753. [DOI] [PubMed] [Google Scholar]
- 12.Rotimi C, et al. Prevalence and determinants of diabetic retinopathy and cataracts in West African type 2 diabetics. Eth Dis. 2003;13:S110–7. [PubMed] [Google Scholar]
- 13.Chuang LM, Tsai ST, Huang BY, Tai TY. Diabcare (Taiwan Study Group) Diabetes Res Clin Pract. 2001;54:S55–65. doi: 10.1016/s0168-8227(01)00310-2. [DOI] [PubMed] [Google Scholar]
- 14.Al-Hamrany MA, Abdulmoneim I. Significance of proteinuria in type 2 Diabetic patients treated at a primary health care in Abha City, Saudi Arabia. West Afr J Med. 2004;23(3):211–4. doi: 10.4314/wajm.v23i3.28123. [DOI] [PubMed] [Google Scholar]
- 15.Lahoz-Rallo B. Cardiovascular disease risk in subjects with type 2 diabetes mellitus in a population in southern Spain. Diab Res Clin Pract. 2007;76:436–44. doi: 10.1016/j.diabres.2006.09.028. [DOI] [PubMed] [Google Scholar]
- 16.Soto-Pedre E, Hernaez-Ortega MC, Pinies JA. Duration of diabetes and screening coverage for retinopathy among patients with type 2 diabetes. Ophthalmic Epidemiol. 2007;14:76–9. doi: 10.1080/09286580600879032. [DOI] [PubMed] [Google Scholar]
- 17.Adler AI, Stratton IM, Neil HA, et al. Association of systolic blood pressure with macrovascular complications of type 2 diabetes (UKPDS 36): prospective observational study. BMJ. 2000;321:412–19. doi: 10.1136/bmj.321.7258.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Akbar DH, Ahmed MM, Algamdi AA. Cardiovascular risk factors in Saudi Arabian and Non-Saudi Arabian diabetic patients in Saudi Arabia. East Mediterr Health J. 2003;9(5–6):884–92. [PubMed] [Google Scholar]
- 19.Stratton IM, Adler AI, Neil HA, Matthews DR, Mansley SE, Cull CA, et al. Association of glycemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational studies. BMJ. 2000;12(321):405–12. doi: 10.1136/bmj.321.7258.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Giorda CB, Avogaro A, Maggini M, Lombardo F, Mannucci E, Turco S, et al. Incidence and risk factors for stroke in type 2 diabetic patients: the DAI study. Stroke. 2007;38(4):1154–60. doi: 10.1161/01.STR.0000260100.71665.2f. [DOI] [PubMed] [Google Scholar]
- 21.Mulnier HE, Seaman HE, Raleigh VS, Soedamah-Muthu SS, Colhoun HM, Lawrenson RA, et al. Risk of stroke in people with type 2 diabetes in the UK: a study using the General Practice Research Database. Diabetologia. 2006;49:2859–65. doi: 10.1007/s00125-006-0493-z. [DOI] [PubMed] [Google Scholar]
- 22.Janghorbani M, Rezvanian H, Kachooei A, Ghorbani A, Chitsaz A, Izadi F, et al. Peripheral neuropathy in type 2 diabetes mellitus in Isfarhan, Iran: prevalence and risk factors. Acta Neurol Scand. 2006;114:384–91. doi: 10.1111/j.1600-0404.2006.00716.x. [DOI] [PubMed] [Google Scholar]
- 23.Famuyiwa FO, Sulimani RR, Laajam MA, Al-Jasser J, Mekki MO. Diabetes mellitus in Saudi Arabia - the clinical pattern and complications in 1000 patients. Ann Saudi Med. 1992;12:140–51. doi: 10.5144/0256-4947.1992.140. [DOI] [PubMed] [Google Scholar]
- 24.Virgolici B, Popescu L. Risk factors in cataract. Oftalmologia. 2006;50(2):3–9. [PubMed] [Google Scholar]; Ueda H, Ishimura E, Miki T, Shimada N, Nixhizawa Y. Analysis of factors for progression of diabetic renal failure in elderly people. Nippon Ronen Igakkai Zasshi. 2005;42(5):553–6. doi: 10.3143/geriatrics.42.553. [DOI] [PubMed] [Google Scholar]