Abstract
BACKGROUND AND OBJECTIVES
No study has assessed psychiatric disorders among infertile men and women seeking fertility treatment in Saudi Arabia. Therefore, we sought to measure the rate of psychiatric disorders in this population.
DESIGN AND SETTINGS
This was a cross-sectional observational study among patients attending infertility clinics at three referral hospitals in Riyadh, Saudi Arabia, between January 2013 and September 2014.
PATIENTS AND METHODS
406 patients (206 women and 200 men) participated in the study. The approved Arabic version of the MINI tool was used to assess 18 common psychiatric illnesses.
RESULTS
The response rate was 81%. Of the men surveyed, only 4.5% self-reported having a psychiatric disorder. Of the women surveyed, only 10.2% reported having a psychiatric disorder. However, using the MINI scale, psychiatric illness was documented in 30% of males and 36.9% of females. The most common diagnoses for both genders were depression (21.7%) and anxiety (21.2%). Significantly more females than males exhibited suicidality and depression. In contrast, significantly more males than females had bipolar disorders and substance-related disorders. A low monthly income among male and female participants and polygamy among female participants were significantly associated with psychiatric disorders.
CONCLUSIONS
This study shows that a higher prevalence of psychiatric disorders, particularly depression and anxiety, among infertile men and women in Saudi Arabia is associated with lower income and polygamy. This study highlights the importance of integrated care for alleviating the psychological burden of this unfortunate population and improving outcomes and quality of life. This study also encourages follow-up studies that aim to further understand the complex relationship between fertility and psychological well-being.
The psychological impacts of involuntary childlessness are routinely and substantially overrated, 1 while the repercussions of both an unfulfilled desire for a child and medically assisted reproduction treatments are often underestimated.2 In western societies, fertility problems have a negative impact on affected individuals depending on patient age, gender, and infertility type.3,4 Although the prevalence of fertility problems is similar nationwide, the individual impact of having such a condition varies greatly, especially from a psychological prospective.4 The stigmatization of having difficulty conceiving a child or being childless is evident in nearly all societies, but some cultures subject infertile couples to more disgrace.5 Cultural perceptions of parenthood, role identity, and religious influence give infertility its significance; therefore, these factors can all determine the level of psychosocial strain.4 In the Arabic world, family unity and parenting continue to be a core value that is held in high esteem.6,7
The psychological aspect of infertility has been studied at multiple levels, including the initial and long-term impacts of the diagnosis,8 the assessment of quality of life and the marital relationship,9 concurrence and risk factors for psychiatric disorders in infertile couples, and the effect of infertility management outcomes on quality of life.10
Our study had three aims. The first was to examine the sociodemographic and psychiatric profile of attendees at infertility clinics in Saudi Arabia. The second was to examine the performance of the mini international neuropsychiatric interview (MINI) among the attendees. The third aim was to compare psychiatric disorders among male and female attendees. Very few studies have addressed this issue in both males and females, and while the vast majority of similar studies have applied self-rated scales to assess psychiatric disorders or psychological well-being, in our study, we applied a validated full MINI structured psychiatric interview that was conducted by trained physicians.
To our knowledge, only two previous studies used the same assessment tool. One prevalence study included women visiting an assisted reproduction clinic,11 and the other study was conducted to determine the sociodemographic correlates of psychological distress among males with infertility.12 One Saudi study was conducted in a single medical city in Riyadh to evaluate knowledge, attitudes, and practices related to infertility among Saudi couples.13 However, no similar prevalence psychiatric studies have been performed within the Saudi population.
METHODS
The current study was conducted in patients attending specialized infertility clinics in three hospitals in Riyadh, Saudi Arabia: King Khalid University Hospital (a governmental hospital), Dallah Hospital, and Dr. Sulaiman Al-Habib Arryan Hospital (both are private hospitals and provide care for insured patients). All adult infertile male and female patients above the age of 18 years who consented to the study and were sufficiently intact cognitively to tolerate a protracted psychiatric interview, were included in the study. The study was cross-sectional in design and was carried out between January 2013 and September 2014. Two trained clinicians evaluated all patients. The study obtained all required ethical approvals from the institutional review board at the Faculty of Medicine at King Saud University in Riyadh, Saudi Arabia.
Since our population was large but unknown, we used the formula n = [(z2 * p * q) + ME2]/(ME2) to determine sample size, where n=sample size, z=critical standard score, p=population proportion, q=is the standard score, and ME=margin of error. Using a margin of error of ±4, confidence level of 95%, we calculated the sample size of 237 patients, assuming that we have a population of at least 1000 patients for the year 2013–2014.
The study questionnaire was developed and administered to all participants. The questionnaire included socio-demographic characteristics and questions pertaining to the infertility and psychiatric history of the participants. The content of the study questionnaire was validated by experts in obstetrics and gynecology, psychiatry, and epidemiology. The questionnaire was then pilot-tested on a small number of participants (N=20) before widespread distribution. The contents of the questionnaire were modified based on the feedback from the pilot sample.
A validated standard Arabic language version of the Mini International Neuropsychiatric Interview (MINI 6.0) was also administered as a psychiatric diagnostic instrument. The MINI was designed to meet the need for a short and precise structured psychiatric interview for clinical trials and epidemiology studies and to be used as a first step for outcome-tracking in clinical settings. The questionnaire requires approximately 15 minutes to administer and covers 17 common psychiatric disorders, including mood, anxiety, substance use, psychotic and eating disorders, in addition to a suicidality module. The instrument has been validated against the considerably longer Structured Clinical Interview for DSM diagnoses (SCID-P) in English and French and against the Composite International Diagnostic Interview for ICD-10 (CIDI) in English, French, and Arabic.14,15
Because it is nearly impossible to obtain a list of all patients serviced by all of the participating hospitals, we administered the questionnaire to patients attending infertility clinics at the time of the study (i.e., using convenience sampling). To minimize bias due to convenience sampling, we obtained a large sample from multiple medical centers with large, diverse, populations. The sample was collected at various days and times over 20-months duration. The questionnaire was distributed during the patients’ follow-up visits to the male/female infertility clinics, and samples were collected independently from the different male/female infertility clinics; thus, couples interviews were not necessary. Two trained clinicians conducted the interviews, and both were trained as specified by the MINI tool designers. Informed consent was obtained from all participants after providing an explanation of the study objectives. The participation rate was 81% of all contacted patients (406/500). Most of the patients who refused to participate gave the verbal excuse of being busy or not being interested in such a study.
Statistical analysis
The collected data were entered into the Statistical Package for Social Sciences (SPSS) version 18.1 (SPSS, IBM, Chicago, Illinois, USA). Continuous variables are expressed as the mean, range, and standard deviation. Categorical variables are expressed as percentages. Correlations of sociodemographic and marriage variables among participants who had psychiatric disorders and participants who did not have psychiatric disorders were identified using the chi-square test for categorical variables and the independent t-test for continuous variables. The chi-square test and the independent t-test were used to identify significant differences between the male and female groups. A stepwise logistic regression was done to determine the most significant factor associated with psychiatric disorders. A P value of less than .05 was considered statistically significant.
RESULTS
A total of 206 females and 200 males participated in the study. Females were significantly younger than males (Table 1). Most participants were Saudi and the majority came from the Central region of Saudi Arabia. Nearly two-thirds (70.4%) of the females were educated at the secondary or university level, whereas 166 of the males (83.0%) were educated at the secondary or university level (P=.212). Sixty-eight percent of the female participants were unemployed in comparison to the 86.0% employment rate among males (P<.001).
Table 1.
Demographic characteristics of the 406 infertile Saudi participants.
| Demographic characteristics | Males n (%) | Females n (%) | P value |
|---|---|---|---|
|
| |||
| Place of residence | .212 | ||
| Central region | 176 (88.0) | 185 (89.9) | |
| Western region | 4 (2.0) | 1 (0.5) | |
| Eastern region | 10 (5.0) | 12 (5.8) | |
| Northern region | 3 (1.5) | 6 (2.9) | |
| Southern region | 7 (3.5) | 2 (1.0) | |
| Educational qualification | .350 | ||
| Primary | 7 (3.5) | 13 (6.3) | |
| Intermediate | 11 (5.5) | 18 (8.7) | |
| Secondary | 65 (32.5) | 51 (24.8) | |
| University | 88 (44.0) | 94 (45.6) | |
| Masters | 11 (5.5) | 12 (5.8) | |
| Doctorate | 2 (1.0) | 2 (1.0) | |
| Uneducated | 3 (1.5) | 7 (3.4) | |
| No response | 13 (6.5) | 9 (4.4) | |
| Employment status | <.001 | ||
| Employed | 172 (86.0) | 66 (32.0) | |
| Unemployed | 28 (14.0) | 140 (68.0) | |
| Accommodation status | .659 | ||
| Lives in own house | 73 (36.5) | 84 (40.8) | |
| Renting a house | 110 (55.0) | 104 (50.5) | |
| Other | 5 (2.5) | 6 (2.9) | |
| No response | 12 (6.0) | 12 (5.8) | |
| Participant lives with: | .212 | ||
| Just with own family | 154 (77.0) | 151 (73.3) | |
| Living together with husband’s family | 34 (17.0) | 46 (22.3) | |
| No response | 12 (6.0) | 9 (4.4) | |
| Monthly income of the family (Saudi Riyals) | .002 | ||
| <5000 | 24 (12.0) | 44 (21.4) | |
| 5000–9999 | 67 (33.5) | 85 (41.3) | |
| 10 000–14 999 | 59 (29.5) | 50 (24.3) | |
| ≥15 000 | 31 (15.5) | 14 (6.8) | |
| No response | 19 (9.5) | 13 (6.3) | |
The female participants were married for a mean duration of 8.2 (6.6) years (range of 1–35 years), which was significantly longer than the male participants, who had a mean marriage duration of 6.8 [4.8] years (P=.017, 95% CI −2.51 to −0.248). The desire to have children (i.e., duration in years of desiring to have children) among female respondents was similar to that observed among male respondents (5.4 [4.3] years versus 5.4 [4.9] years, P=.984, 95% CI=−0.914 to 0.895).
More than two-thirds (67.5%) of the participants were not related maternally or paternally to the man or woman that they married (Table 2). Of the 200 men surveyed, 9 (4.5%) reported that they had been previously diagnosed with a psychiatric disorder; those men reported taking several psychotropic medications, primarily antidepressants, and/or undergoing psychotherapy. On the other hand, of the 206 women surveyed, 21 (10.2%) reported that they had been previously diagnosed with a psychiatric disorder; however, only 9 (42.8%) of those women reported taking psychotropic medications, primarily antidepressants, and/or undergoing psychotherapy.
Table 2.
Marriage demographics and conditions pertaining to the marital lives of 406 infertile Saudi participants.
| Marriage variables | Males | Females | P value |
|---|---|---|---|
|
| |||
| The relationship of the participant to spouse | .009 | ||
| Paternal or maternal cousin | 36 (18.0) | 62 (30.1) | |
| No relationship | 161 (80.5) | 139 (67.5) | |
| Others | 3 (1.5) | 5 (2.4) | |
| Polygamy | .078 | ||
| Yes | 45 (22.5) | 32 (15.5) | |
| No | 155 (77.5) | 174 (84.5) | |
| Participant has been previously married to another spouse | .785 | ||
| Once | 35 (17.5) | 21 (10.2) | |
| More than once | 10 (5.0) | 7 (3.4) | |
| Delayed childbearing as a cause of failed marriage | 8 (4.0) | 3 (1.5) | .516 |
| Has children from current/previous marriage | <.001 | ||
| From current marriage | 24 (12.0) | 56 (27.2) | |
| From previous marriage | 8 (4.0) | 5 (2.4) | |
| Number of male children | .006 | ||
| One | 9 (4.5) | 22 (10.7) | |
| Two | 4 (2.0) | 10 (4.9) | |
| Three or more | 8 (4.0) | 6 (2.9) | |
| Number of female children | .049 | ||
| One | 12 (6.0) | 25 (12.1) | |
| Two | 3 (1.5) | 11 (5.3) | |
| Three or more | 6 (3) | 7 (3.4) | |
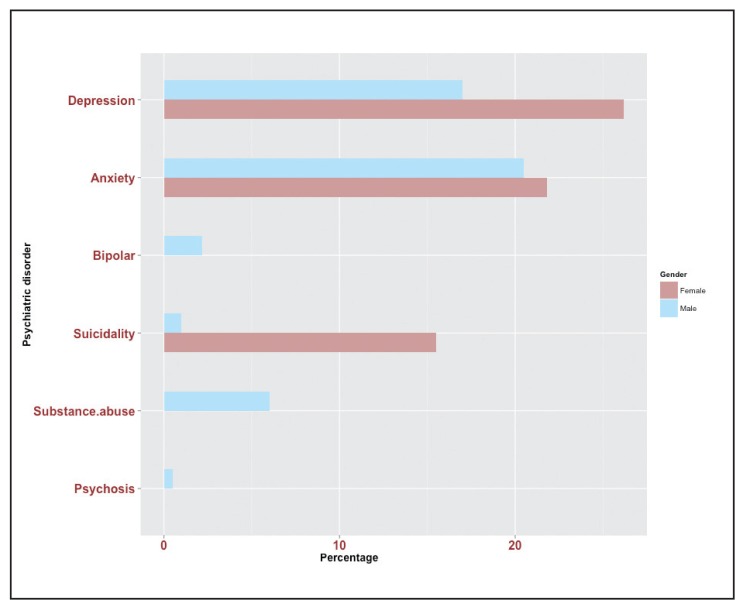
However, after interviewing the participants using the MINI scale, 60 (30%) men and 76 (36.9%) women were found to have psychiatric disorders (Table 3). The most common psychiatric disorder was depression in 88 (21.7%) patients, followed by anxiety in 86 (21.2%) patients. The least common disorder was psychosis, in 2 (0.5%) patients. Figure 1 illustrates the observed differences in the frequencies of psychiatric disorders between male and female patients. Significantly more females exhibited suicidality (n=32, 15.5% versus n=2, 1.0%, P<.001) and depression (n=54, 26.2% versus n=34, 17.0%, P=.024) in comparison to males. On the other hand, significantly more males than females had bipolar disorders and substance-related disorders (n=9, 2.2% versus n=0, 0%, P=.002 and n=12, 6.0% versus n=0, 0%, P<.001, respectively). No significant differences in the frequencies of psychotic disorders (0.5% versus 0%, P=.150) and anxiety (20.5% versus 21.8%, P=.740) were observed between males and females.
Table 3.
Psychiatric disorders diagnosed using the mini international neuropsychiatric interview (MINI) among 406 infertile Saudi participants.
| Psychiatric disorder | n | % |
|---|---|---|
|
| ||
| Depressive disorders | 88 | 21.7 |
| Anxiety disorders | 86 | 21.2 |
| Bipolar disorders | 9 | 2.2 |
| Suicidality | 34 | 8.4 |
| Substance-related disorders | 12 | 3.0 |
| Psychotic disorders | 2 | 0.5 |
Figure 1.
Percentage distribution of psychiatric disorders diagnosed using the mini international neuropsychiatric interview (MINI) among 406 infertile male and female Saudi participants.
The mean age of the female patients who had a psychiatric disorder was 32.0 (6.6) years, which was not significantly different than the mean age of patients (31.3 [5.6] years) who had no psychiatric disorders (P=.454). The number of years desiring to have children was significantly higher among female patients who had psychiatric disorders than among female patients with no psychiatric disorders (6.21 [5.5] years versus 4.84 [4.2] years, P=.048). No significant difference in the duration of delayed pregnancy was observed between female patients who had psychiatric disorders and female patients who had no psychiatric disorders (6.6 [5.2] years versus 5.3 [4.5] years, P=.052). In addition, no significant differences in the number of previous marriages, the numbers of male and female children, or the duration of marriage were observed between female patients who had psychiatric disorders and female patients who did not have psychiatric disorders (P=.239, P=.546, P=.149 and P=.314, respectively). Among male patients, the mean duration of marriage was significantly (P=.026) longer among men who had psychiatric disorders (7.85 [5.8] years) than among men who had no psychiatric disorders (6.24 [4.1] years). No significant differences in the mean age (35.72 [7.9] years versus 35.26 [8.8] years, P=.718) and the duration of delayed childbearing (6.0 [4.9] years versus 5.23 [3.9] years, P=.233) were observed between participants who had a psychiatric disorder and participants who did not have a psychiatric disorder. In addition, no significant differences in the number of previous marriages and the numbers of male and female children were observed between patients who had psychiatric disorders and patients who did not have psychiatric disorders (P=.150, P=.726, and P=.457, respectively). No significant differences in the mean duration of marriage or the number of years of desiring to have children were observed between male and female participants who had a psychiatric disorder (P=.314 and P=.521, respectively). Female patients who had a psychiatric disorder were significantly older than their male counterparts (P=.007).
For infertile females, monthly income and a polygamous husband were the two variables that were significantly associated with a psychiatric disorder (Table 4). Of the 76 female participants who had a psychiatric disorder, 22 (28.9%) had a monthly income of less than 5 000 riyals per month, 31 (40.8%) had a monthly income between 5 000 and 10 000 riyals per month, and 20 (26.3%) had a monthly income between 10 000 and 15,000 per month. In contrast, among the 130 female participants who did not have a psychiatric disorder, only 22 (16.9%) had a monthly income of less than 5 000 riyals per month, and 44 (33.8%) had a monthly income of 10 000 riyals or more per month (P=.046). A significant difference in the frequency of psychiatric conditions was also observed between women who had a polygamous husband and women who did not have a polygamous husband. The prevalence of women with a polygamous husband was 23.7% (n=18/76) among female participants who had a psychiatric disorder in comparison to a prevalence of 10.8% (n=14/130) among female participants who had no psychiatric disorders (P=.014).
Table 4.
Correlations of sociodemographic and marriage variables with the frequency of psychiatric disorders diagnosed using the mini international neuropsychiatric interview (MINI) among 200 males and 206 females infertile Saudi participants.
| Sociodemographic and marriage variables | Correlation coefficient (P value) | |
|---|---|---|
| Females | Males | |
|
| ||
| Age of the participant | 15.62 (.945) | 0.03 (.718) |
| Educational qualification | 9.61 (.212) | −0.09 (.245) |
| Nationality | 0.82 (.364) | 0.04 (.950) |
| Place of residence | 6.65 (.155) | 0.12 (.091) |
| Presence of job | 0.17 (.676) | 0.04 (.556) |
| Type of accommodation | 0.59 (.900) | 0.04 (.620) |
| With whom the participant lives | 1.18 (.554) | 0.03 (.643) |
| Monthly income | 9.67 (.046) | −0.14 (.069) |
| Relationship with husband/wife | 1.79 (.408) | 0.02 (.791) |
| Polygamy | 6.09 (.014) | 0.10 (.502) |
| Husband has children from another marriage | 0.73 (.392) | −0.27 (.188) |
| Previous marriage | 0.07 (.797) | −0.08 (.746) |
| Number of previous marriages | 1.52 (.469) | |
| Failed marriage | 0.92 (.632) | |
| Has children | 0.49 (.482) | |
| Number of male children | 1.74 (.629) | 0.09 (.726) |
| Number of female children | 2.63 (.622) | 1.72 (.457) |
| Had premature children | 26.15 (.294) | |
For infertile males, only monthly income was significantly associated with having a psychiatric disorder (Table 4). Of the 60 male participants who had a psychiatric disorder, 38 (63.3%) had a monthly income of less than 10 000 riyals per month (P=.009). In contrast, among the 140 participants who did not have a psychiatric disorder, 57.3% had a monthly income of more than 10 000 SR per month, and only 42.7% had a monthly income of less than 10 000 SR per month. No significant difference in the frequency of psychiatric conditions was observed between educated and non-educated men (P=.282). In addition, the frequency of psychiatric conditions did not vary according to place of residence (P=.482), employment status (P=.431), owning a house (P=.918), living with other members of the family (P=0.686), the relationship between the couple (P=.566), previous marriage (P=.859), being polygamous (P=.700), and having children from a previous wife or previous marriage (P=.360).
Among females, depression was significantly positively correlated with having a polygamous husband (r=0.141, P=.044). Anxiety disorders were significantly correlated with the place of residence (r=0.150, P=.031), having a polygamous husband (r=0.227, P=.001), a long duration of desire to have children (r=0.201, P=.004), and a long duration of delayed childbirth (r=0.167, P=.017). Suicidality was significantly correlated with the place of residence (r=0.174, P=.012). Among males, depression was significantly correlated with polygamy (r=0.419, P=.004), and anxiety disorders were significantly positively correlated with the number of clinic visits (r=0.147, P=.044). Significant positive correlations were observed between the frequency of psychiatric disorders in males and females and both the level of education and monthly income (r=17.77 P=.007 and r=10.647 P=.014, respectively) (Table 5). Using a stepwise logistic regression analysis on the significant factors, monthly income was the only significant predictor of psychiatric disorder (beta −0.159, t=−3.053, P=.002, 95%CI=−0.135 to −0.029)
Table 5.
Correlations of sociodemographic and marriage variables with the frequency of psychiatric disorders diagnosed using the mini international neuropsychiatric interview (MINI) among 406 infertile Saudi participants.
| Sociodemographic and marriage variables | Correlation coefficient | P value |
|---|---|---|
|
| ||
| Gender | 3.245 | .072 |
| Age of the participant | 24.236 | .969 |
| Educational qualification | 17.77 | .007 |
| Nationality | 0.379 | .538 |
| Place of residence | 6.719 | .152 |
| Presence of job | 2.310 | .679 |
| Type of accommodation | 0.371 | .831 |
| With whom the participant lives | 0.225 | .635 |
| Monthly income | 10.647 | .014 |
| Polygamy | 1.660 | .198 |
| Number of previous marriages | 0.960 | .327 |
| Has children from previous marriage | 0.098 | .755 |
| Number of male children | 6.944 | .139 |
| Number of female children | 1.130 | .889 |
DISCUSSION
To our knowledge, this study is the first in Saudi Arabia to evaluate the prevalence of psychiatric disorders among infertile patients. The majority of the participants were of Saudi nationality and were from the Central province of Saudi Arabia. The mean age of the female participants was 31.5 years in comparison to a mean age of 35.4 years in the male group; these values reflect a nearly 4- to 7-year delay in parenthood compared to the general Saudi population, for which the mean age of childbearing was 28.6 years in 2014.16 That age is similar to the childbearing age in developed countries, which ranges from 24 to 28 years.17 Females exhibited higher rates of unemployment (68%) compared to males (14%); these rates are higher than the unemployment rates for both genders in the general population (32.8% for females and 5.9% for males).18 Although the number of years of marriage was significantly greater among females (8.2 [6.6] years) than among males (6.8 [4.8] years), both genders are equal in terms of the number of years longing for children (approximately 5.4 years) and are close to the figures reported in a Chinese study.19 However, in both developed and less developed countries, 56% of couples with delayed fertility will seek medical advice after the first year.20
The prevalence of self-reported psychiatric illnesses in this cohort was as low as 4.5% in males and 10.2% in females. However, when conducting the MINI neuropsychiatric interview, the results showed that 30% of the men and 36.9% of the women had current psychiatric disorders; this finding may reflect the fact that subjects suffering from infertility either tend to minimize their psychological distress or receive inadequate psychological care from their primary physicians. A similarly wide gap between self-reported psychological distress and the actual frequency determined by a valid scale was reported in a previous gastroenterology study of a Saudi population that evaluated help-seeking behavior and its association with psychiatric comorbidity. In this study, only 6% of the participants reported having psychiatric disorders; however, strikingly, after applying the PHQ-9 and GAD-7 scales, 40% were found to have symptoms of depression or anxiety disorders.21 In contrast, in developed countries, women with fertility problems were more likely to report depression and/or anxiety than fertile women.8 In addition, another study found that infertile females who scored high on self-rating scales (i.e., the zung depression scale and the zung anxiety scale) had previously indicated their need for psychological support.22
Our study shows that 21.7% of the study population met the criteria for depression; this value was significantly higher in females than males (26.2% vs. 17%, respectively), while anxiety symptoms were relatively comparable in the two genders (20.5% in males and 21.8% in females). Despite using different assessment tools, these figures are comparable to those reported in a local study in a primary care setting (24% and 20% for anxiety and depression, respectively).23 However, another study that used the same tool to screen for depression in the same primary care setting showed more than double this percentage (49.9%). Moreover, the female gender had higher depression rates.24 On the other hand, anxiety appeared to be more frequent among the male population.25,26 Regional studies addressing psychiatric comorbidities in infertile populations are lacking, but a study that was conducted in the United Arab Emirates highlighted increased life stress among infertile women, with an abundance of mood-related complaints.27 The mode of assessing the psychological burden varies greatly among infertility studies. Furthermore, the vast majority of such research focuses on females;28 hence, it has been nearly impossible to standardize outcomes and difficult to compare data. In a study comparing infertile Iranian women with a group of fertile controls using the SCL-90-R, an increased occurrence of psychiatric disorders (44%) was found among infertile women compared to controls (28.7%); in particular, depression had higher scores.29 Data from another developing nation that assessed both males and females are consistent with our study, not only in terms of the predominance of females among patients displaying psychiatric symptoms but also in terms of the increased frequency of depression among females. However, anxiety symptoms were more frequent in males than females.30
Nonetheless, studies conducted in more developed countries reported comparable results. In an Italian study that addressed psychiatric morbidity among infertile couples, only females in the study group showed a significant increase in psychiatric disorders in comparison to the female correspondents in the control group (12% vs. 8%, 12% vs. 8% and 28% vs. 3% for generalized anxiety, adjustment disorder with depressive features and adjustment disorder with mixed depression, and anxiety, respectively). However, male subjects did show a slightly higher frequency of generalized anxiety (7% vs. 3%) and adjustment disorder with mixed depression and anxiety (4% versus 1%) than control males.31 In addition, using the Beck Depression Inventory and the Beck Anxiety Inventory, a Polish study revealed that the risk factors for depression and infertility include the following factors: female sex, age over 30 years, a lower level of education, a lack of occupational activity, diagnosed male infertility, and an infertility disorder duration of 3–6 years.32
Our study revealed a significant difference in the rate of bipolar disorders and substance-related psychiatric disorders between the two genders (2.2% versus 0% and 6.0% versus 0%, respectively). A recent Danish study highlighted a 17% increased chance of hospitalization among females with unsuccessful fertility outcomes compared to females who achieved motherhood after the initial evaluation. The main reasons for admission were substance- and alcohol-related disorders (2-fold) and psychosis (50% increment). Surprisingly, mood disorders showed a 10% decrease, which could be explained either by chance or by multiple births in the comparison group, which is by itself a risk factor for depression.33
Among females who displayed psychiatric disorders in our study, financial stress and a polygamous husband were significantly correlated with the presence of psychiatric disorders. There is a positive association between depression and polygamy, which is considered to be an absolute stressor in our society.34 Anxiety disorders were significantly correlated with the place of residence in which the majority of our sample is living, with having a polygamous husband, and with having a long duration of desire to have children or a long duration of delayed childbirth, which is associated with the progression of age and a decreased chance of childbearing. 35 Suicidal risk was significantly correlated with the place of residence due to the sample allocation. Among males, depression was significantly correlated with polygamy; this finding may be explained by the financial burden that results in a lower economic status36 or the community pressure to have a second wife without a personal interest to do so.37 Anxiety disorders were significantly positively correlated with the number of clinic visits made to seek help for delayed conception. Furthermore, positive correlations were observed between both the level of education and monthly income and the frequency of psychiatric disorders in both genders.
On the other hand, in several studies that assessed risk factors that contribute to a negative psychological experience among men, ambiguous results from the infertility evaluation,10 male factor infertility,28 first infertility evaluation, and a temporary career22 were associated with depression10 and stressful emotions,28 although males react less stressfully in response to missing fatherhood.28
To date, the literature has been inconsistent on the relationship between mental disorders and infertility, although a bidirectional relationship is assumed.38 Among women, the failure to achieve conception following each trial leads to more vulnerability to depression,10 while anxiety is related to the initiation of each treatment cycle.11 Advanced age, a longer infertility period, and a female source of infertility exhibited close associations with anxiety and/or depression.27 On the contrary, other studies showed no associations of age, length of infertility, education, income, or previous treatment history with psychiatric outcomes.11 In a study conducted in Turkey, the lack of husband and/or significant other support resulted in an increased chance of anxiety and depression among infertile women. Depression, anxiety and self-esteem improved as age and the duration of infertility increased.39 In 2011, a meta-analysis found that pretreatment emotional distress was not associated with treatment outcome after a cycle of assisted reproductive technology.40 Among infertile males, a systematic review found that stress alone may reduce testosterone levels and spermatogenesis. 41 Moreover, a more recent prospective study of 501 couples found that higher levels of stress as measured by salivary alpha-amylase are associated with a longer time-to-pregnancy (TTP) and an increased risk of infertility. 42 Nevertheless, a recent systemic review and meta-analysis of 39 studies (total n=2746 men and women) suggested that psychosocial interventions for couples undergoing treatment for infertility could be helpful both in reducing psychological distress and in improving clinical pregnancy rates.43
Consistent with our results and for similar reasons, polygamy seems to correlate with negative psychological consequences.27 Nevertheless, the psychological state of one spouse was found to influence the other; for example, having an anxious male partner increases the rate of depression and anxiety in the female partner and vice versa.22
Our study has the advantage of applying an objective assessment tool (the MINI psychiatric interview), although this study could be prone to reporting bias, false positive cases and the tool does not cover all psychiatric disorders. This limitation was overcome by assigning two trained physicians, including one physician who was a psychiatrist, to conduct the interviews. Another limitation of our study is the cross-sectional design, which makes it difficult to relate causal factors. In addition, the results may be subject to prevalence incidence bias. The lack of available information on the prevalence of psychiatric disorders in Saudi Arabia may lead to the over- or under-estimation of the actual impact of infertility. Because of the use of convenience sampling, our results should be cautiously generalized and not be considered as representative to all patients in Riyadh, Saudi Arabia.
In conclusion, this study reports a higher prevalence of psychiatric disorders, particularly depression and anxiety, among infertile Saudi men and women, especially those with a lower income and those practicing polygamy. This study also sheds light on the importance of integrated care for alleviating the psychological burden of this unfortunate population and improving their outcomes and quality of life. The study also encourages follow-up research that aims to further understand the complex relationship between fertility and psychological well-being.
Acknowledgments
We would like to extend our sincere appreciation to the Deanship of Scientific Research at King Saud University, Riyadh, Saudi Arabia for its funding of this research group No. (RG–1435-087). Furthermore, we would like to express gratitude to Ms. Fatima Jama for her help in data entry and Dr. Isnani Arthur for his assistance in data analysis.
Footnotes
Conflict of interest
The authors have no competing interests.
REFERENCES
- 1.Wischmann TH. Psychogenic infertility--myths and facts. J Assist Reprod Genet. 2003;20:485–94. doi: 10.1023/B:JARG.0000013648.74404.9d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Domar A, Gordon K, Garcia-Velasco J, La Marca A, Barriere P, Beligotti F. Understanding the perceptions of and emotional barriers to infertility treatment: a survey in four European countries. Hum Reprod. 2012;27:1073–9. doi: 10.1093/humrep/des016. [DOI] [PubMed] [Google Scholar]
- 3.Morreale M, Balon R, Tancer M, Diamond M. The impact of stress and psychosocial interventions on assisted reproductive technology outcome. J Sex Marital Ther. 2011;37:56–69. doi: 10.1080/0092623X.2011.533584. [DOI] [PubMed] [Google Scholar]
- 4.Cousineau TM, Domar AD. Psychological impact of infertility. Best Pract Res Clin Obstet Gynaecol. 2007;21:293–308. doi: 10.1016/j.bpobgyn.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 5.Lykeridou K, Gourounti K, Sarantaki A, Roupa Z, Iatrakis G, Zervoudis S, et al. What kind of care and support do infertile women undergoing fertility treatment in Greece expect? A questionnaire survey. Clin Exp Obstet Gynecol. 2010;37:201–8. [PubMed] [Google Scholar]
- 6.Hassane S, McClam T, Woodside M. The Status of Women and Its Influence on Human Service Education in a Non-Western Culture. Hum Serv Educ. 2009;29:25–34. [Google Scholar]
- 7.Renzaho AMN, McCabe M, Sainsbury WJ. Parenting, role reversals and the preservation of cultural values among Arabic speaking migrant families in Melbourne, Australia. Int J Intercult Relations. 2011;35:416–424. [Google Scholar]
- 8.Herbert DL, Lucke JC, Dobson AJ. Depression: an emotional obstacle to seeking medical advice for infertility. Fertil Steril. 2010;94:1817–21. doi: 10.1016/j.fertnstert.2009.10.062. [DOI] [PubMed] [Google Scholar]
- 9.Onat G, Kizilkaya Beji N. Effects of infertility on gender differences in marital relationship and quality of life: a case-control study of Turkish couples. Eur J Obstet Gynecol Reprod Biol. 2012;165:243–8. doi: 10.1016/j.ejogrb.2012.07.033. [DOI] [PubMed] [Google Scholar]
- 10.Volgsten H, Skoog Svanberg A, Ekselius L, Lundkvist O, Sundstrom Poromaa I. Risk factors for psychiatric disorders in infertile women and men undergoing in vitro fertilization treatment. Fertil Steril. 2010;93:1088–96. doi: 10.1016/j.fertnstert.2008.11.008. [DOI] [PubMed] [Google Scholar]
- 11.Chen TH, Chang SP, Tsai CF, Juang KD. Prevalence of depressive and anxiety disorders in an assisted reproductive technique clinic. Hum Reprod. 2004;19:2313–2318. doi: 10.1093/humrep/deh414. [DOI] [PubMed] [Google Scholar]
- 12.Yusuf AJ, Maitama HY, Amedu MA, Ahmed M, Mbibu HN. Socio-demographic correlates of psychological distress among male patients with infertility in Zaria, Nigeria. African J Urol. 2012;18:170–174. [Google Scholar]
- 13.Abolfotouh MA, Alabdrabalnabi AA, Albacker RB, Al-Jughaiman UA, Hassan SN. Knowledge, attitude, and practices of infertility among Saudi couples. Int J Gen Med. 2013;6:563–73. doi: 10.2147/IJGM.S46884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 2):22–33. quiz 34–57. [PubMed] [Google Scholar]
- 15.Sadek A. Mini international neuropsychiatric interview (MINI): the Arabic translation. Psychiatry Updat Inst Psychiatry. 2000;2:23–31. [Google Scholar]
- 16.Central Department of Statistics and Information. Indicator of Fertility. [accessed 9 Apr 2015]. http://www.cdsi.gov.sa/english/index.php?option=com_docman&Itemid=164.
- 17.Mathews TJ, Hamilton BE. Mean age of mother, 1970–2000. Natl Vital Stat Rep. 2002;51:1–13. [PubMed] [Google Scholar]
- 18.Central Department of Statistics and Information. Labour Force survey 2014 Round 2 - Labour Force surveys - Social Statistics - statistics and information tables. [accessed 22 May 2015]. http://www.cdsi.gov.sa/english/index.php?option=com_docman&task=cat_view&gid=243&Itemid=162.
- 19.Lok IH, Lee DTS, Cheung LP, Chung WS, Lo WK, Haines CJ. Psychiatric morbidity amongst infertile Chinese women undergoing treatment with assisted reproductive technology and the impact of treatment failure. Gynecol Obstet Invest. 2002;53:195–199. doi: 10.1159/000064560. [DOI] [PubMed] [Google Scholar]
- 20.Boivin J, Bunting L, Collins JA, Nygren KG. International estimates of infertility prevalence and treatment-seeking: potential need and demand for infertility medical care. Hum Reprod. 2007;22:1506–12. doi: 10.1093/humrep/dem046. [DOI] [PubMed] [Google Scholar]
- 21.Alosaimi FD, Al-Sultan O, Alghamdi Q, Almohaimeed I, Alqannas S. Association of help-seeking behavior with depression and anxiety disorders among gastroenterological patients in Saudi Arabia. Saudi J Gastroenterol. 20:233–40. doi: 10.4103/1319-3767.136977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chiaffarino F, Baldini MP, Scarduelli C, Bommarito F, Ambrosio S, D’Orsi C, et al. Prevalence and incidence of depressive and anxious symptoms in couples undergoing assisted reproductive treatment in an Italian infertility department. Eur J Obstet Gynecol Reprod Biol. 2011;158:235–41. doi: 10.1016/j.ejogrb.2011.04.032. [DOI] [PubMed] [Google Scholar]
- 23.Becker S, Al Zaid K, Al Faris E. Screening for somatization and depression in Saudi Arabia: a validation study of the PHQ in primary care. Int J Psychiatry Med. 2002;32:271–83. doi: 10.2190/XTDD-8L18-P9E0-JYRV. [DOI] [PubMed] [Google Scholar]
- 24.Al-Qadhi W, Ur Rahman S, Ferwana MS, Abdulmajeed IA. Adult depression screening in Saudi primary care: prevalence, instrument and cost. BMC Psychiatry. 2014;14:190. doi: 10.1186/1471-244X-14-190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alibrahim OA, Al-Sadat N, Elawad NAM. Gender and risk of depression in Saudi Arabia, a systematic review and meta-analysis. J Public Health Africa. 2010;1:2010–1:e7. doi: 10.4081/jphia.2010.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.El-Rufaie OEFA, Albar AA, Al-Dabal BK. Identifying anxiety and depressive disorders among primary care patients: A pilot study. Acta Psychiatr Scand. 1988;77:280–282. doi: 10.1111/j.1600-0447.1988.tb05121.x. [DOI] [PubMed] [Google Scholar]
- 27.Khayata GM, Rizk DEE, Hasan MY, Ghazal-Aswad S, Asaad MaN. Factors influencing the quality of life of infertile women in United Arab Emirates. Int J Gynecol Obstet. 2003;80:183–188. doi: 10.1016/s0020-7292(02)00387-9. [DOI] [PubMed] [Google Scholar]
- 28.Fisher JRW, Hammarberg K. Psychological and social aspects of infertility in men: an overview of the evidence and implications for psychologically informed clinical care and future research. Asian J Androl. 2012;14:121–9. doi: 10.1038/aja.2011.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Noorbala AA, Ramezanzadeh F, Abedinia N, Naghizadeh MM. Psychiatric disorders among infertile and fertile women. Soc Psychiatry Psychiatr Epidemiol. 2009;44:587–91. doi: 10.1007/s00127-008-0467-1. [DOI] [PubMed] [Google Scholar]
- 30.Tuzer V, Tuncel A, Goka S, Bulut SD, Yuksel FV, Atan A, et al. Marital adjustment and emotional symptoms in infertile couples: gender differences. 2010;40:229–237. [Google Scholar]
- 31.Sbaragli C, Morgante G, Goracci A, Hofkens T, De Leo V, Castrogiovanni P. Infertility and psychiatric morbidity. Fertil Steril. 2008;90:2107–11. doi: 10.1016/j.fertnstert.2007.10.045. [DOI] [PubMed] [Google Scholar]
- 32.Drosdzol A, Skrzypulec V. Depression and anxiety among Polish infertile couples--an evaluative prevalence study. J Psychosom Obstet Gynaecol. 2009;30:11–20. doi: 10.1080/01674820902830276. [DOI] [PubMed] [Google Scholar]
- 33.Baldur-Felskov B, Kjaer SK, Albieri V, Steding-Jessen M, Kjaer T, Johansen C, et al. Psychiatric disorders in women with fertility problems: results from a large Danish register-based cohort study. Hum Reprod. 2013;28:683–90. doi: 10.1093/humrep/des422. [DOI] [PubMed] [Google Scholar]
- 34.Chaleby K. Traditional Arabian marriages and mental health in a group of outpatient Saudis. Acta Psychiatr Scand. 1988;77:139–142. doi: 10.1111/j.1600-0447.1988.tb05090.x. [DOI] [PubMed] [Google Scholar]
- 35.Leridon H. Can assisted reproduction technology compensate for the natural decline in fertility with age? A model assessment. Hum Reprod. 2004;19:1548–1553. doi: 10.1093/humrep/deh304. [DOI] [PubMed] [Google Scholar]
- 36.Al-Krenawi A, Graham JR, Slonim-Nevo V. Mental health aspects of Arab-Israeli adolescents from polygamous versus monogamous families. J Soc Psychol. 2002;142:446–60. doi: 10.1080/00224540209603911. [DOI] [PubMed] [Google Scholar]
- 37.Elbedour S, Onwuegbuzie AJ, Caridine C, Abu-Saad H. The Effect of Polygamous Marital Structure on Behavioral, Emotional, and Academic Adjustment in Children: A Comprehensive Review of the Literature. Clin Child Fam Psychol Rev. 5:255–271. doi: 10.1023/a:1020925123016. [DOI] [PubMed] [Google Scholar]
- 38.Schweiger U, Wischmann T, Strowitzki T. [Mental disorders and female infertility]. Nervenarzt. 2012;83:1442–7. doi: 10.1007/s00115-012-3662-y. [DOI] [PubMed] [Google Scholar]
- 39.Guz H, Ozkan A, Sarisoy G, Yanik F, Yanik A. Psychiatric symptoms in Turkish infertile women. J Psychosom Obstet Gynaecol. 2003 doi: 10.3109/01674820309074691. [DOI] [PubMed] [Google Scholar]
- 40.Boivin J, Griffiths E, Venetis CA. Emotional distress in infertile women and failure of assisted reproductive technologies: meta-analysis of prospective psychosocial studies. BMJ. 2011;342:d223. doi: 10.1136/bmj.d223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hall E, Burt VK. Male fertility: psychiatric considerations. Fertil Steril. 2012;97:434–9. doi: 10.1016/j.fertnstert.2011.11.027. [DOI] [PubMed] [Google Scholar]
- 42.Lynch CD, Sundaram R, Maisog JM, Sweeney AM, Buck Louis GM. Preconception stress increases the risk of infertility: results from a couple-based prospective cohort study--the LIFE study. Hum Reprod. 2014;29:1067–75. doi: 10.1093/humrep/deu032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Frederiksen Y, Farver-Vestergaard I, Skovgard NG, Ingerslev HJ, Zachariae R. Efficacy of psychosocial interventions for psychological and pregnancy outcomes in infertile women and men: A systematic review and meta-analysis. BMJ Open. 2015;5:e006592. doi: 10.1136/bmjopen-2014-006592. [DOI] [PMC free article] [PubMed] [Google Scholar]