Abstract
BACKGROUND
Numerous studies have reported a decline in stroke-related mortality in developed countries.
OBJECTIVE
To assess trends in one-year mortality following a stroke diagnosis in Saudi Arabia.
DESIGN
Retrospective longitudinal cohort study.
SETTING
Single tertiary care center from 2010 through 2014.
PATIENTS
All patients admitted with a primary admitting diagnosis of stroke.
METHODS
Demographic data (age, gender, nationality), risk factor profile, stroke subtypes, in-hospital complications and mortality data as well as cause of death were collected for all patients. A multivariable logistic regression model was used to assess factors associated with one-year mortality following a stroke admission.
MAIN OUTCOME MEASURE(S)
One-year mortality.
RESULTS
In 548 patients with a mean age of 62.9 years (SD 16.9), the most frequent vascular risk factors were hypertension (90.6%), diabetes (65.5%), and hyperlipidemia (27.2%). Hemorrhagic stroke was diagnosed in 9.9%. The overall mortality risk was 26.9%. Non-Saudis had a significantly higher one-year mortality risk compared with Saudis (25% vs. 16.8%, respectively; P=.025). The most frequently reported causes of mortality were neurological and related to the underlying stroke (32%), sepsis (30%), and cardiac or other organ dysfunction-related (each 9%) in addition to other etiologies (collectively 9.5%) such as pulmonary embolism or an underlying malignancy. Significant predictors in the multivariate model were age (P<.0001), non-Saudi nationality (OR 1.8, CI 95 1.1 to 2.9; P=.019), and hospital length of stay (OR 1.01, CI 95 1 to 1.004; P=.001).
CONCLUSION
We observed no decline in stroke mortality in our center over the 5-year span. The establishment of stroke systems of care, use of thrombolytic agents, and opening of a stroke unit should play an important role in a decline in stroke mortality.
LIMITATIONS
Retrospective single center study. Mortality data were available only for patients who died in our hospital.
Stroke is a leading cause of death worldwide. Approximately 15 million people worldwide suffer from stroke each year according to the World Health Organization.1 Of these, 5 million die and another 5 million suffer permanent disabilities. In the United States (US), an estimated 700 000 cases of stroke are reported each year.2 In the Middle East, the incidence rates vary from 29.8 cases per 100 000 population in Saudi Arabia to 57 per 100 000 population in Bahrain; the 28-day case mortality rate ranges from 10% in Kuwait to 31.5% in Iran.3
Several reports show a declining trend in stroke mortality. 4–11 In the United Kingdom, the 56-day mortality after a first stroke declined by 43% between 1999 and 2008.10 In Australia, the age-standardized mortality rate for men fell by 71% between 1979 and 2010. A similar decline was observed among women over the same period.11 However, it is not known whether this trend is due to better acute stroke care or because strokes are becoming milder.12 The latter possibility is feasible for many reasons. First, advancement in neuroimaging, especially magnetic resonance imaging (MRI), resulted in higher detection of milder strokes that could have progressed to severe or even fatal strokes. Second, there are anecdotal reports suggesting that strokes are shifting towards small-vessel related strokes such as lacunar strokes.13,14 This is especially relevant in our country where a high prevalence of diabetes is reported. Third, it is possible that stroke is truly getting milder due to better recognition and management of stroke risk factors and thus mortality related to stroke is declining.
This study addressed these issues by assessing the trends in stroke mortality over a five-year period. Although there is declining overall mortality of strokes, it is not known whether that is true for all the stroke subtypes. 2–11 This study assessed trends in mortality in different stroke subtypes to help plan effective stroke care and prevention strategies.
METHODS
This was a retrospective longitudinal cohort of all stroke cases admitted to King Abdulaziz University Hospital, Jeddah, Saudi Arabia with a primary admitting diagnosis of ischemic or hemorrhagic stroke from January 2010 to December 2014. Patients were identified from the electronic medical record system using International Classification of Diseases codes (ICD-9 or ICD-10).16 The system does not capture patients who remained in the emergency department throughout their hospitalization.
Inclusion criteria were age of 18 years or more and stroke diagnosed clinically according to the World Health Organization definition of stroke (rapidly developing focal neurological deficit lasting more than 24 hours or longer or leading to death, with no apparent cause other than vascular origin).
Exclusion criteria were age less than 18 years old, sub-arachnoid hemorrhage, subdural hematoma or traumatic intracerebral bleeding, or transient ischemic attacks.
Medical records were reviewed to gather data on patient demographics (age, gender, ethnicity), vascular risk profile, stroke subtypes using TOAST criteria as described by Adams et al15 (i.e., large artery atherosclerotic, cardioembolic, small artery lacunar occlusion, stroke of other determined etiology and stroke of undetermined etiology), imaging and laboratory investigations, all in-hospital complications and discharge time, medications and destinations. The frequency and indication of readmission within 30 days were also collected. Finally, we followed all patients in our electronic system to capture mortality reports on all included patients until the end of December 2015 to allow for a minimum of a one-year follow up on patients who were admitted in December 2014.
Data on the demographics and vascular risk factors are described in absolute numbers and percentages. Measured variables are reported in means (and standard deviation, “SD”) or medians (and interquartile range, “IQR”), as appropriate. Continuous variables were compared using the t test or Mann Whitney U test, where appropriate. Categorical variables were compared using the chi-square test. A multivariable logistic regression model was used to assess factors associated with outcomes. Trends in one-year mortality after a stroke were compared across the study years. All testing was two-tailed and was measured at the 0.05 level of significance. Analyses were done using Stata 12 software (Stata Corp, College Station, TX).
RESULTS
Between January 2010 and December 2014, 548 patients were admitted with a primary admitting diagnosis of stroke. The mean age of the patients was 62.9 years (SD 16.9) and 42.1% of the cohort were females. Saudi patients represented 36.1% of all cases. Among the various vascular risk factors, hypertension was the most frequent (90.6%) followed by diabetes (65.5%). Hyperlipidemia was underreported (27.2%). Hemorrhagic stroke was diagnosed in 9.9%. Table 1 shows patients characteristics for each year.
Table 1.
Characteristics of the cohort by admission year.
| Admission Year | 2010 | 2011 | 2012 | 2013 | 2014 |
|---|---|---|---|---|---|
|
| |||||
| Mean age (years) | 65.6 | 65.1 | 62.7 | 60.1 | 62.3 |
| Female (%) | 42.2 | 52.7 | 36.3 | 41 | 40.3 |
| Saudi (%) | 28.1 | 30.6 | 29 | 46.2 | 42.6 |
| Hypertension (%) | 100 | 97.3 | 87.1 | 81.2 | 92.2 |
| Diabetes mellitus (%) | 65.6 | 62.5 | 61.8 | 69.2 | 68.8 |
| Hemorrhagic stroke (%) | 14.1 | 8.9 | 10.5 | 11.1 | 7 |
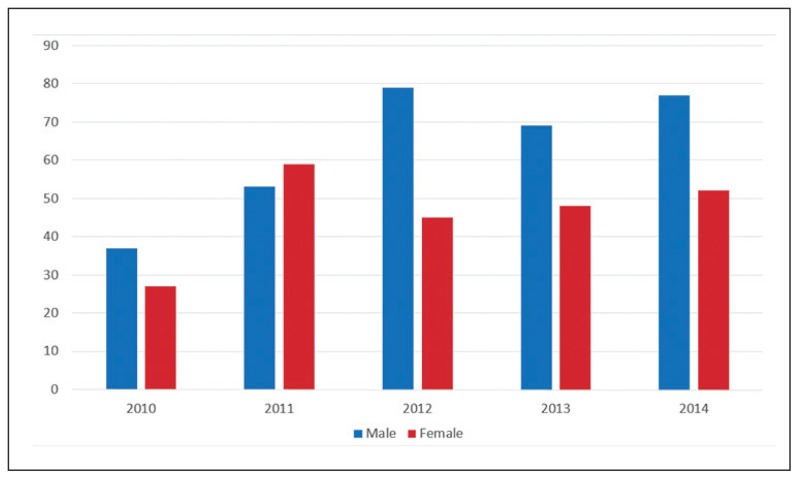
Figure 1 shows the total number of cases admitted each year according to sex. The median length of hospitalization was 9.7 days (interquartile range 16). Data relating to stroke mechanism was not always available given the variability of the stroke workup performed. On imaging findings, only 46 patients were found to have lacunar-like strokes on computed tomography or MRI. There were 111 (20.3%) patients who were discharged home on oral anticoagulation, indicating a cardioembolic stroke mechanism. In-hospital complications included bed sores in 21.5% and hospital-acquired infections in 13.8% (majority related to pneumonia). Readmission within 30 days of discharge was reported in 24.9%.
Figure 1.
Stroke admissions during the study period.
Patients were tracked in the hospital system for a total of 1503 person-years. The one-year mortality risk was 22.1% while the thirty-day case fatality rate for stroke was 11.1%. The overall mortality risk in our cohort was 26.9%. Table 2 shows the age- and sex-specific one-year mortality rates. There was no difference in the overall mortality between males and females although there are suggestions that the age-specific mortality rates were less in females than males, but this did not reach statistical significance. However, non-Saudis had a significantly higher one-year mortality risk compared with Saudis (25% vs. 16.8%, respectively; P=.025).
Table 2.
Number of deaths in each year of stroke admission stratified by gender and age.
| Age group (years) | 2010 | 2011 | 2012 | 2103 | 2014 | Total | Age-specific mortality risk | Total sex-specific |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Males | ||||||||
| <60 (n=148) | 1 | 4 | 7 | 8 | 5 | 25 | 16.9% | |
| 60–69 (n=74) | 0 | 4 | 5 | 3 | 1 | 13 | 17.6% | |
| 70–79 (n=62) | 2 | 5 | 4 | 4 | 6 | 21 | 33.9% | |
| ≥80 (n=31) | 2 | 2 | 4 | 2 | 2 | 12 | 38.7% | |
| Total | 5 | 15 | 20 | 17 | 14 | 71 | 22.5% | |
| Females | ||||||||
| <60 (n=90) | 1 | 2 | 1 | 2 | 1 | 7 | 7.8% | |
| 60–69 (n=48) | 2 | 2 | 2 | 4 | 4 | 14 | 29.2% | |
| 70–79 (n=52) | 2 | 2 | 6 | 1 | 3 | 14 | 26.9% | |
| ≥80 (n=41) | 4 | 3 | 3 | 3 | 1 | 14 | 34.1% | |
| Total | 9 | 9 | 12 | 10 | 9 | 49 | 21.2% | |
The most frequently reported causes of mortality were neurological and related to the underlying stroke in 32%, followed by sepsis (30%), cardiac or other organ dysfunction-related (each 9%) in addition to other etiologies (collectively 9.5%) such as pulmonary embolism or an underlying malignancy.
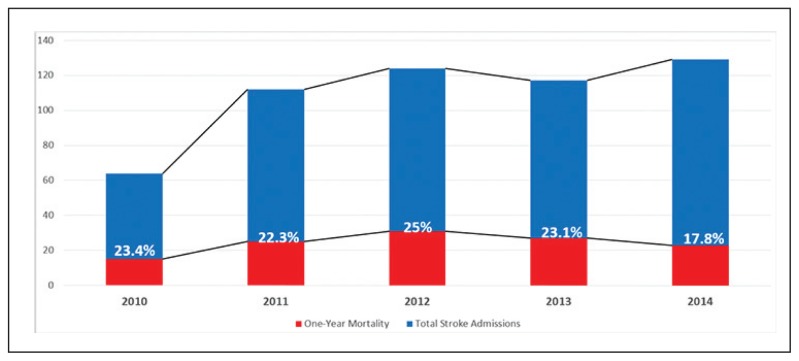
Figure 2 shows the trends in one-year mortality during the study period. Overall, there was no significant difference in the one-year stroke mortality over the study period (test of trend P=.34). In a multivariable logistic regression model, predictors of mortality included age (P=.0001), non-Saudi nationality (OR 1.8, 95% CI 1.1 to 2.9; P=.019), and hospital length of stay (OR 1.01, 95% CI 1 to 1.004; psuedo R2=0.0786 P=.001). Readmission within 30 days approached significance as a predictor of mortality (OR 1.6, 95 CI 0.99 to 2.6; P=.051). Neither stroke subtype (ischemic vs hemorrhagic) nor patient sex were significant predictors of one-year mortality.
Figure 2.
Total stroke admissions with one-year mortality.
DISCUSSION
Our analysis of the mortality trends in patients with a primary admitting diagnosis of ischemic or hemorrhagic stroke provides insights into stroke epidemiology in Saudi Arabia. Contrary to previous findings from the Western literature, we did not observe a decline in mortality. Several factors may explain this observation: (a) stroke risk factors are still not optimally managed in our community, and studies that showed a decrease in mortality had better risk factor control programs;16–18 (b) no stroke unit yet exists in our hospital or in the entire city of Jeddah. Stroke units have been shown to decrease stroke-related mortality by 30% and improve the functional outcome of stroke survivors;19 (c) the mixed population of Saudi and non-Saudi with very different health backgrounds may have diluted any influence on mortality related to genetic or ethnic factors. It is also possible that mortality is declining, but a larger sample or longer observation periods are needed to properly investigate the mortality trends in our patients. Studies from developed countries that showed a decline in stroke mortality observed such trends over a minimum of 10 years.20–23 In one report from the United States, for example, mortality due to stroke declined slowly throughout most of the 20th century, at a rate of approximately 0.5% per year.23 The rate of decline then accelerated to approximately 5% per year in the 1970s. In a more recent report from the United Kingdom,22 a substantial fall in stroke mortality was documented for the period 1979 to 2004. In the Oxford region, ischemic or hemorrhagic stroke was identified in 41% of all underlying cause stroke deaths in 1979. The rate fell to 33% in 1984, 20% in 1994, and then increased to 30% in 2004. Unfortunately, data on stroke mortality are lacking in the Middle East, and a single report projects that mortality due to stroke may nearly double by 2030 in the Middle East and North Africa.3
The most frequently reported causes of mortality were neurological and were related to the underlying stroke in about a third of all cases, followed by infections (30%). The distribution of mortality causes in our cohort is different from that found among 30-day survivors in other hospital-based studies: the initial stroke event accounted for 24.9% and pneumonia for 7.3% of deaths in a study conducted at a university hospital in Bern, Switzerland;24 infection, especially pneumonia, was the primary cause in 37.5% of the cases in a study performed at a local hospital in São Paulo, Brazil;25 and cardiac-related causes accounted for 26.2% and malignancies for 23.4% of deaths among stroke patients admitted to the Radboud University Nijmegen Medical Center in the Netherlands.26
The risk factor profile of our patients is similar to that of patients in other studies. In this study, hypertension was the most frequent vascular risk factor followed by diabetes while hyperlipidemia was underreported. Studies conducted in Malaysia,27 Ireland,28 and India29 showed that hypertension was the commonest risk factor for both stroke types. Diabetes mellitus ranked second, but only for ischemic stroke. Conversely, other investigators identified smoking as the major stroke risk factor, followed by hypertension and hyperlipidemia.30 Age has also been consistently reported as a risk factor for stroke and stroke mortality with evidence of its interaction with other stroke risk factors. According to one report,27 if only patients older than 70 years were analyzed, the prevalence of hyperlipidemia was significantly higher in patients with ischemic stroke. On the contrary, other authors reported a significant relationship between hypercholesterolemia and stroke only in patients under 45 years old.31 Collins et al32 found that the risk factor associated with the highest hazard for a 30-day mortality was advanced age (≥ 75 years). A similar finding was reported by de Jong et al,33 who found that advanced age, along with diabetes and stroke subtype, was an independent predictor of 30-day case fatality. In a more recent study of 469 older patients (mean age of 80 years), the authors demonstrated that 30-day mortality was associated with age, congestive heart failure, and altered level of consciousness. 34 While we did not identify risk factors by stroke type, it is worth noting that in contrast to other vascular diseases, risk factors associated with stroke as well as short- and long-term prognosis vary according to the subtype of stroke, making it hard to acquire reliable data about factors associated with an increased risk of mortality that are valid for all stroke patients. In addition, severity of stroke (which has been incorporated in models for risk prediction)35–37 could not be ascertained since the description of the clinical examination findings were not always documented and the standard measure of stroke severity (National Institutes of Health Stroke Scale score) was not formally performed.
Our study has limitations that need to be taken into consideration. First, mortality data were available only for patients who died in our hospital. While this may result in an underestimation of the mortality rate, it is more likely for patients who were admitted to our center once to return to this hospital to seek future medical care. Thus, the impact of missing any outside-hospital mortality is thought to be small. Second, our prognostic model did not include relevant characteristics that were not documented in the medical records, such as stroke severity as measured by the National Institute of Health Stroke Scale score; or funcational outcome as measured by the modified Rankin scale or Barthel Index. The magnitude of this factor is hard to predict since prior studies38,39 demonstrated that a model that incorporated stroke severity may overestimate or underestimate mortality at 30 days or 1 year after stroke. Third, socioeconomic status and the cause of stroke, which are potentially important variables, were not routinely collected and thus could not be included in our mortality prediction model. Socio-economic data would have been particularly instructive as it may explain differences in mortality between Saudi and non-Saudi patients. Despite these limitations, this study is among the first to report on mortality associated with stroke in recent years in a Saudi center. It should stimulate prospective data collection from multiple centers to provide valid records of all important variables to quantify their direct effect and influence on stroke mortality.
Overall, we observed no decline in stroke mortality and, based on the trends, we cannot determine whether stroke mortality will decrease in the future at our healthcare center. Nevertheless, the parameters selected in this study are reasonable considerations as factors that influence stroke mortality and represent key components of stroke prevention. Other factors, such as systems of care, use of antithrombotic agents, smoking cessation, exercise, and atrial fibrillation may play a role in stroke deaths, but additional studies conducted over longer periods and with larger samples are needed to determine the impact of these factors on stroke deaths.
ACKNOWLEDGMENTS
The author would like to thank Princila Mukoko, Trisha Dane Cuajao, and Shaik Sajeed for their assistance with the data collection and manuscript preparation.
Footnotes
Source(s) of support
This work was funded by the Deanship of Sceintific Research (DSR), King Abdulaziz University, Jeddah, under gran No. (D1435-523-140). The author, therefore, acknowledge with thanks DSR technical and financial support.
REFERENCES
- 1.Mackay J, Mensah GA. The Atlas of Heart Disease and Stroke. Geneva: World Health Organization; 2004. Available at: http://www.who.int/cardiovascular_diseases/resources/atlas/en. [Google Scholar]
- 2.Goldstein LB, Adams R, Alberts MJ, Appel LJ, Brass LM, Bushnell CD, et al. Primary prevention of ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council: cosponsored by the Atherosclerotic Peripheral Vascular Disease Interdisciplinary Working Group; Cardiovascular Nursing Council; Clinical Cardiology Council; Nutrition, Physical Activity, and Metabolism Council; and the Quality of Care and Outcomes Research Interdisciplinary Working Group. Circulation. 2006;113(24):e873–923. doi: 10.1161/01.STR.0000223048.70103.F1. [DOI] [PubMed] [Google Scholar]
- 3.Tran J, Mirzaei M, Anderson L, Leeder SR. The epidemiology of stroke in the Middle East and North Africa. J Neurol Sci. 2010 Aug 15;295(1–2):38–40. doi: 10.1016/j.jns.2010.05.016. [DOI] [PubMed] [Google Scholar]
- 4.Sarti C, Rastenyte D. International Trends in Mortality from Stroke, 1968 to 1994. Stroke. 2000;31:1588–1601. doi: 10.1161/01.str.31.7.1588. [DOI] [PubMed] [Google Scholar]
- 5.Hu G, Sarti C. The Impact of History of Hypertension and Type 2 Diabetes at Baseline on the Incidence of Stroke and Stroke Mortality. Stroke. 2005;36:2538–2543. doi: 10.1161/01.STR.0000190894.30964.75. [DOI] [PubMed] [Google Scholar]
- 6.Benatru I, Rouaud O. Stable Stroke Incidence Rates but Improved Case-Fatality in Dijon, France, From 1985 to 2004. Stroke. 2006;37:1674–1679. doi: 10.1161/01.STR.0000226979.56456.a8. [DOI] [PubMed] [Google Scholar]
- 7.Kunst AE, Amiri M, Janssen F. The decline in stroke mortality: exploration of future trends in 7 Western European countries. Stroke. 2011;42(8):2126–30. doi: 10.1161/STROKEAHA.110.599712. [DOI] [PubMed] [Google Scholar]
- 8.Teuschl Y, Brainin M, Matz K, Dachenhausen A, Ferrari J, Seyfang L, Lang W Austrian Stroke Unit Registry Collaborators. Time trends in patient characteristics treated on acute stroke-units: results from the Austrian Stroke Unit Registry 2003–2011. Stroke. 2013;44(4):1070–4. doi: 10.1161/STROKEAHA.111.676114. [DOI] [PubMed] [Google Scholar]
- 9.Vaartjes I, O’Flaherty M, Capewell S, Kappelle J, Bots M. Remarkable decline in ischemic stroke mortality is not matched by changes in incidence. Stroke. 2013;44(3):591–7. doi: 10.1161/STROKEAHA.112.677724. [DOI] [PubMed] [Google Scholar]
- 10.Lee S, Shafe AC, Cowie MR. UK stroke incidence, mortality and cardiovascular risk management 1999–2008: time-trend analysis from the General Practice Research Database. BMJ Open. 2011;1(2):e000269. doi: 10.1136/bmjopen-2011-000269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Australian Institute of Health and Welfare. Stroke and its Management in Australia: an update. [Accessed on January 30, 2016]. Available from: http://www.aihw.gov.au/WorkArea/DownloadAsset.aspx?id=60129543611.
- 12.Sarti C, Stegmayr B, Tolonen H, Mähönen M, Tuomilehto J, Asplund K WHO MONICA Project. Are changes in mortality from stroke caused by changes in stroke event rates or case fatality? Results from the WHO MONICA Project. Stroke. 2003;34(8):1833–40. doi: 10.1161/01.STR.0000081224.15480.52. [DOI] [PubMed] [Google Scholar]
- 13.The Canadian Collaborative Study Group of Stroke Hospitalizations. Hospitalization and Case Fatality Rates for Stroke in Canada From 1982 Through 1991. Stroke. 1996;27:1215–1220. doi: 10.1161/01.str.27.7.1215. [DOI] [PubMed] [Google Scholar]
- 14.Yang Q, Botto LD, Erickson JD, Berry RJ, Sambell C, Johansen H, et al. Improvement in stroke mortality in Canada and the United States, 1990 to 2002. Circulation. 2006;113(10):1335–43. doi: 10.1161/CIRCULATIONAHA.105.570846. [DOI] [PubMed] [Google Scholar]
- 15.Adams HP, Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993;24(1):35–41. doi: 10.1161/01.str.24.1.35. [DOI] [PubMed] [Google Scholar]
- 16.Colquhoun DM. Lipid lowering agents: how important are they in secondary prevention of coronary heart disease? Aust Fam Physician. 2002;31(1):25–6. 29–30. [PubMed] [Google Scholar]
- 17.Scherr C, Cunha AB, Magalhães CK, Abitibol RA, Barros M, Cordovil I. Life-habit intervention in a public institution. Arq Bras Cardiol. 2010;94(6):730–7. doi: 10.1590/s0066-782x2010005000058. [DOI] [PubMed] [Google Scholar]
- 18.Stamler J, Stamler R, Neaton JD, Wentworth D, Daviglus ML, Garside D, et al. Low risk-factor profile and long-term cardiovascular and noncardiovascular mortality and life expectancy: findings for 5 large cohorts of young adult and middle-aged men and women. JAMA. 1999;282(21):2012–8. doi: 10.1001/jama.282.21.2012. [DOI] [PubMed] [Google Scholar]
- 19.Indredavik B, Bakke F, Slørdahl SA, Rokseth R, Håheim LL. Stroke unit treatment 10-year follow-up. Stroke. 1999;30(8):1524–7. doi: 10.1161/01.str.30.8.1524. [DOI] [PubMed] [Google Scholar]
- 20.Peltonen M, Asplund K. Age-periodcohort effects on stroke mortality in Sweden 1969–1993 and forecasts up to the year 2003. Stroke. 1996;27(11):1981–5. doi: 10.1161/01.str.27.11.1981. [DOI] [PubMed] [Google Scholar]
- 21.Islam MS, Anderson CS, Hankey GJ, Hardie K, Carter K, Broadhurst R, et al. Trends in incidence and outcome of stroke in Perth, Western Australia during 1989 to 2001: the Perth Community Stroke Study. Stroke. 2008;39(3):776–82. doi: 10.1161/STROKEAHA.107.493643. [DOI] [PubMed] [Google Scholar]
- 22.Goldacre MJ, Duncan M, Griffith M, Rothwell PM. Mortality rates for stroke in England from 1979 to 2004: trends, diagnostic precision, and artifacts. Stroke. 2008;39(8):2197–203. doi: 10.1161/STROKEAHA.107.509695. [DOI] [PubMed] [Google Scholar]
- 23.Lackland DT, Roccella EJ, Deutsch AF, Fornage M, George MG, Howard G, et al. Factors influencing the decline in stroke mortality: a statement from the American Heart Association/American Stroke Association. Stroke. 2014;45(1):315–53. doi: 10.1161/01.str.0000437068.30550.cf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nedeltchev K, Renz N, Karameshev A, Haefeli T, Brekenfeld C, Meier N, et al. Predictors of early mortality after acute ischaemic stroke. Swiss Med Wkly. 2010;140(17–18):254–9. doi: 10.4414/smw.2010.12919. [DOI] [PubMed] [Google Scholar]
- 25.Machado MF, Brucki SM, Nogueira CF, Rocha MS. Infectious disease is the most common cause of death among stroke patients: two-years of follow-up. Arq Neuropsiquiatr. 2013;71(6):371–5. doi: 10.1590/0004-282X20130041. [DOI] [PubMed] [Google Scholar]
- 26.Brown DL, Al-Senani F, Lisabeth LD, Farnie MA, Colletti LA, Langa KM, et al. Defining cause of death in stroke patients: The Brain Attack Surveillance in Corpus Christi Project. Am J Epidemiol. 2007;165(5):591–6. doi: 10.1093/aje/kwk042. [DOI] [PubMed] [Google Scholar]
- 27.Ong TZ, Raymond AA. Risk factors for stroke and predictors of one-month mortality. Singapore Med J. 2002;43(10):517–21. [PubMed] [Google Scholar]
- 28.McDonnell R, Fan CW, Johnson Z, Crowe M. Prevalence of risk factors for ischaemic stroke and their treatment among a cohort of stroke patients in Dublin. Ir J Med Sci. 2000;169:253–7. doi: 10.1007/BF03173526. [DOI] [PubMed] [Google Scholar]
- 29.Kaul S, Venketswamy P, Meena AK, Sahay R, Murthy JM. Frequency, clinical features and risk factors of lacunar infarction (data from a stroke registry in South India) Neurol India. 2000;48(2):116–9. [PubMed] [Google Scholar]
- 30.Bak S, Bak L, Sorense JS. Prevalence of risk factors in cerebral ischemia. Ugeskr Laeger. 1995;157:444–6. [PubMed] [Google Scholar]
- 31.Qizilbash N, Lewington S, Duffy S, Peto R. Cholesterol, diastolic blood pressure and stroke: 13,000 strokes in 450,000 people in 45 prospective cohorts. Prospective Studies Collaboration. Lancet. 1995;346:1647–52. [PubMed] [Google Scholar]
- 32.Collins TC, Petersen NJ, Menke TJ, Souchek J, Foster W, Ashton CM. Shortterm, intermediate-term, and long-term mortality in patients hospitalized for stroke. J Clin Epidemiol. 2003;56:81–75. doi: 10.1016/s0895-4356(02)00570-x. [DOI] [PubMed] [Google Scholar]
- 33.de Jong G, van Raak L, Kessels F, Lodder J. Stroke subtype and mortality. a follow-up study in 998 patients with a first cerebral infarct. J Clin Epidemiol. 2003;56:262–8. doi: 10.1016/s0895-4356(02)00572-3. [DOI] [PubMed] [Google Scholar]
- 34.Zuliani G, Cherubini A, Ranzini M, Ruggiero C, Atti AR, Fellin R. Risk factors for short-term mortality in older subjects with acute ischemic stroke. Gerontology. 2006;52:231–6. doi: 10.1159/000093655. [DOI] [PubMed] [Google Scholar]
- 35.Smith EE, Shobha N, Dai D, Olson DM, Reeves MJ, Saver JL, et al. Risk score for in-hospital ischemic stroke mortality derived and validated within the Get With the Guidelines–Stroke Program. Circulation. 2010;122:1496–1504. doi: 10.1161/CIRCULATIONAHA.109.932822. [DOI] [PubMed] [Google Scholar]
- 36.Konig IR, Ziegler A, Bluhmki E, Hacke W, Bath PM, Sacco RL, et al. Predicting long-term outcome after acute ischemic stroke: a simple index works in patients from controlled clinical trials. Stroke. 2008;39:1821–1826. doi: 10.1161/STROKEAHA.107.505867. [DOI] [PubMed] [Google Scholar]
- 37.Saposnik G, Kapral MK, Liu Y, Hall R, O’Donnell M, Raptis S, et al. IScore: a risk score to predict death early after hospitalization for an acute ischemic stroke. Circulation. 2011;123(7):739–49. doi: 10.1161/CIRCULATIONAHA.110.983353. [DOI] [PubMed] [Google Scholar]
- 38.Williams GR, Jiang JG. Development of an ischemic stroke survival score. Stroke. 2000;31:2414–2420. doi: 10.1161/01.str.31.10.2414. [DOI] [PubMed] [Google Scholar]
- 39.Goldie FC, Fulton RL, Frank B, Lees KR VISTA Collaboration. Interdependence of stroke outcome scales: reliable estimates from the Virtual International Stroke Trials Archive (VISTA) Int J Stroke. 2014 Apr;9(3):328–32. doi: 10.1111/ijs.12178. [DOI] [PubMed] [Google Scholar]