Abstract
BACKGROUND
Maternal-fetal attachment, which forms as soon as pregnancy starts, is essential to an infant’s mental development.
OBJECTIVE
This study aimed to explore the effect of teaching attachment behaviors to pregnant women on infant mental health from birth to 3 months of age.
DESIGN
Randomized controlled trial.
SETTING
Hafiz Hospital, Shiraz University of Medical Sciences, Iran, from February to November 2014.
PATIENTS AND METHODS
The participants were randomly divided into an intervention and a control group at 28–34 weeks gestation. The participants in the intervention group attended six educational sessions each lasting for 60–90 minutes. After delivery, the infants of mothers in each group were compared in terms of mental health indexes (total mean scores and scores derived from a checklist of questions for infant mental health with results categorized as low, average and high). Maternal anxiety levels were also recorded at birth and at 3 months.
MAIN OUTCOME MEASURE(S)
Infant mental health index.
RESULTS
In 190 pregnant women (96 in the intervention group and 94 in the control group), the total mean (SD) scores for infant mental health at birth were 16.66 (1.51) in the intervention group and 16.07 (1.74) in the control group (P=.013). At 3 months, the total mental health scores infants were 31.05 (1.88) in the intervention group and 30.25 (2.10) in the control group (P=.007). Differences in checklist scores between the groups at 3 months were not statistically significant, except for crying intensity at 3 months (P=.021). Women in the control group had higher anxiety levels at 3 months (P=.01).
CONCLUSION
Teaching attachment skills to mothers increased the attachment between the mothers and their infants, and consequently, improved infant mental health. Thus, teaching attachment skills should be incorporated into routine prenatal care.
LIMITATIONS
Use of phone calls by the researcher to assess mental health.
Maternal-fetal attachment refers to the emotional attachment between the mother and fetus and is an indication of their health and the mother’s efficiency in the postnatal period.1 According to Robinson (2010), attachment does not form after delivery but develops in seven stages: planning for pregnancy, adapting to pregnancy, accepting pregnancy, feeling the fetal movements, recognizing the fetus as an individual, birth-giving, and seeing and touching the baby.2 Winkler et al (2000) studied 481 pregnant women and concluded that maternal-fetal attachment was an influential factor in infant physical development during and after pregnancy.3 Muller believes that attachment between the mother and fetus forms as soon as pregnancy begins and develops as pregnancy develops. In the second trimester, the attachment peaks and remains so until after delivery, playing an important role in mothers’ adaptation to pregnancy.4
Even though pregnancy is a natural phenomenon, it is often accompanied by fears that can result in stress and anxiety, which adversely affects the pregnant women’s attachment process.5 In the mental-social stress charts, the anxiety derived from the birth of the first child is classified as severe. Thus, women tend to experience depression, anxiety, and phobias during pregnancy, which adversely affect the baby’s development.6 Anxiety and bitterness on the part of the mother increases her plasma cortisol and, in turn, increases the secretion of hypothalamic-hypophyseal-adrenal axis in the fetus, directly affecting its personality traits.7,8 One study showed that the mother’s anxiety levels influenced the number and flexibility of fetal heartbeats, eventually leading to tachycardia.9 Also, mothers who experience high stress and anxiety levels during pregnancy are more likely to give birth to babies with kinesthetic or mental development disorders. Despite advances in prenatal care, the results are not satisfactory.10 Anxiety is one reason for failure and affects morbidity and mortality directly and indirectly. Non-medicinal treatments are among effective approaches in the relief of anxiety. Most non-medicinal interventions are based on mind-body medicine, where the emphasis is on the balance between the mind and body and its effects on health. In mind-body medicine, interventions are introduced through enhancing those capacities of the mind that influence the body. Such interventions include hypnotism, visual imagery, yoga, relaxation, and teaching attachment.6,11,12 It has been proved that children with behavioral and emotional disorders, incontinence, and educational failures belong to mothers who had no attachment to their babies during and after pregnancy. Not only does maternal-fetal attachment influence the mother’s attachment behaviors, but it acts like a nutritious substance for the baby and gives it the security and love that it needs to develop mentally and physically.13 Behavioral disorders that appear in childhood and persist in adulthood have undesirable consequences. Thus, it is important to study the factors that lead to such disorders. According to Farrant et al, the extent of attachment between the mother and her baby directly affects the baby’s emotions, feelings, and future behaviors.14 Moreover, Brumariu believed that individuals who had had poor emotional bonds with their mothers during their fetal period and early years were very likely to have personality, social, and intellectual disorders as adults.15 Likewise, Carter found out that children with behavioral and emotional disorders, incontinence, and educational failures had no emotional attachment with their mothers during their fetal stages and early years.16
Attachment between the mother and baby is related to the emotional aspect of their relationship and has a biological basis.17 According to Franc et al (2009), this relationship forms during pregnancy and is essential to the baby’s psychological development.18 Lee et al discovered that teaching attachment-based cognitive behavior to mothers directly affected the quality of their interaction with their babies as well as the babies’ mental health.19 Similarly, the study by Koniak et al revealed that enhanced attachment resulted in closeness and pleasant emotions that contributed to mother and infant mental health.20 In their study on the influence of maternal-fetal attachment on infant development, Alhusen et al (2012) investigated 166 pregnant women and concluded that a program to teach attachment behaviors to mothers and reduction of postnatal depression were two important factors in infant development in early years. In that study, women who had limited attachment with their babies during pregnancy and experienced greater postnatal depression gave birth to babies with developmental delays.21 The influence of mothers’ attachment behaviors on their babies’ mental health is a new area in medicine. Since only a limited number of studies have been conducted in this area, the present study aimed to explore the effect of teaching attachment behaviors to pregnant women on infant mental health from birth to three months of age.
PATIENT AND METHODS
Study design
In this clinical trial, the mental health of the infants in the intervention and control groups were compared after attachment behaviors were taught to the intervention group. The study sample consisted of the women who had registered for treatment at Hafiz Hospital from February to November 2014.
Sample size and randomization
Based on the study objectives and reported studies, considering a power=80%, a=0.05, 1-b=.80 sd=5, and loss rate of 10%, and using the following formula, a 198-subject sample size was determined for the study (99 participants in each group):22–24
The participants were selected through purposive sampling, a non-probability sampling technique that relies on the judgment of the researcher (http://goo.gl/6FXtW0). After selection, block randomization was used to divide participants into the control and intervention groups. The study could not be blinded in the education stage, but the researchers who evaluated the infant score of mental statues and analyzed the data were blinded to the assignment.
Subject population
The inclusion criteria of the study were willingness to participate in the study, signing written informed consent, being married, aged between 18 and 40 years, residency in Shiraz, with a planned pregnancy, singleton pregnancy, low-risk pregnancy, gestational age of 28–34 weeks, having at least a junior high-school education, and having mild or average anxiety levels based on Speilberger’s questionnaire. The exclusion criteria were missing more than one educational session, loss of pregnancy, high-risk pregnancy, preterm delivery, and congenital defects in the infant.
The women in the control group received routine care delivered by the staff midwife, including assessment of fetal heart rate and the measurement of uterine growth at each visit. Women in the control group took public classes in the form of lectures about prenatal care and breastfeeding. The mothers in the intervention group were trained on attachment skills in four 60–90-minute sessions held once a week. Training courses were held as lectures, question and response, open discussion, watching films and role playing. Topics included physiology of pregnancy and childbirth, awareness of the feelings and perceptions of the embryo, the concept of attachment, attachment behavior (the relationship with the fetus), attachment behavior (control of anxiety and negative thoughts) and patterns of proper sleep, exercise and nutrition during pregnancy.
The study data were collected using a personal information form (mother’s demographic characteristics, pregnancy characteristics, results of previous pregnancies, and others), Speilberger’s questionnaire, and the infant mental health evaluation at birth and at three months of age. Spielberger’s scale consists of 40 questions (20 items for trait anxiety and 20 for state anxiety) with the maximum score of 80. In this scale, scores of 0–19, 20–40, 41–60, and 61–80 represented normal, mild, average, and intense levels of anxiety, respectively25,26 conducted on 150 patients undergoing surgery in Iran in 2007, the reliability of this questionnaire was reported to be 97%. The reliability and validity indexes reported in that study were the basis of the present research.27
A list of questions designed to assess infant mental health at birth was based on the infant mental health indices in William’s books on developmental psychology, pregnancy, and delivery.28 Since infant mental health indices are not separable from their physical health at birth, the questions were designed to evaluate the main mental health indices.29,30 For infant mental health at birth, the mothers answered nine questions with scores of 0, 1, or 2. The scores were added for a total score from 0–18. Higher scores represent better mental health in the infant. In the study by Shayeghian et al,31 Chronbach’s alpha and split-half reliability of the checklist were 0.89 and 0.72, respectively. The content validity of the checklist (as calculated by 6 pediatricians) was 0.93. These measures were the basis of the current study.31 For infant mental health at 3 months of age, the mothers answered 17 questions with scores of 0, 1, or 2. The questions evaluated reflexes specific to this age, including sleep length, quietness, type of crying, breathing rate, and others.29,30 The scores were added for a total score from 0–34 with higher scores representing better mental health. According to the study conducted by Shayeghian et al, Chronbach’s alpha and split-half reliability of the questionnaire were 0.90 and 0.81, respectively. Its content validity was 0.95. The reliability and validity indexes were the basis of the present study.31
Data analysis
The primary endpoint was the difference in mean total scores for infant mental health between the intervention and control groups at birth and at 3 months. The secondary endpoint was differences in mental health scores of infants in the intervention and control groups at birth and at 3 months from the questions that assessed mental health in the infant, with results categorized as high, low and average. For the primary endpoint, the Mann-Whitney U test was used since the data were not normally distributed by Kolmogorov-Smirnov test. The chisquare or Fisher exact (when the expected frequency in a cell was less than 5) were used to compare proportions in the high, low and average categories (defined in footnotes to the tables). The chi-square test or Fisher exact test was used for comparison of demographic variables (employment of the mother, number of pregnancies, body mass index, level of education). The t test was used to compare ages and maternal anxiety levels. An alpha of .05 defined a statistically significant result.
RESULTS
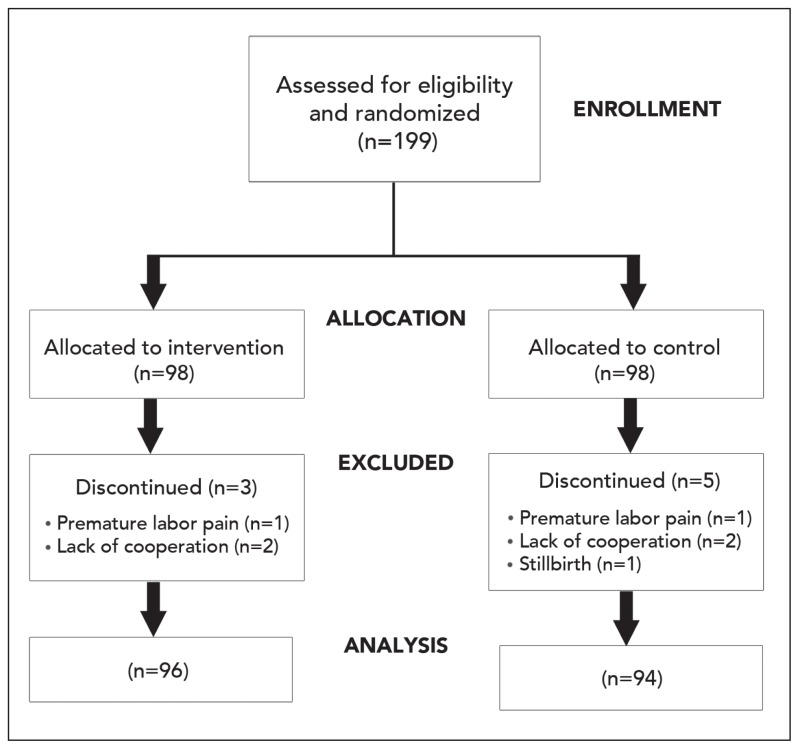
From an initial sample of 198 women (98 in each group) three were excluded in the intervention group and five in the control group (Figure 1) so that 94 patients in the intervention group and 96 in the control group were included in the analysis. In 190 pregnant women (96 in the intervention group and 94 in the control group), the mean age was 28.2 (6.0) in the intervention group and 27.7 (5.6) in the control group. Most participants were high-school graduates and undergraduates. The lowest and highest anxiety scores were 6 and 60 in the intervention group and 3.5 and 60 in the control group. There were no significant differences between the two groups in age (P=.59), education level (P=.80), occupation (P=.80), parity (P=.80) and anxiety level (P=.43). A significant difference was observed between the two groups in the total mean scores for infant mental health variables at birth (P=.013) (Table 1). Anxiety scores at 3 months were higher for women in the control group (29.70 [13.33] vs 24.51 [13.33] control vs. intervention; P=.01). At birth, infants in the intervention group had a higher frequency of ideal weight (P=.388), greater height (P=.366), higher Apgar scores (P=.681), non-cyanotic skin (P=.640), general skin conditions (P=.263), less crying (P=.021), better breathing (P=.403), and overall health (P=.859) compared with the control group, but the difference was only significant for the intensity of crying (Table 2). There was a significant difference between the two groups in total mean scores for infant mental health variables at three months of age (P=.007) (Table 1). At the age of three months, 13 variables were higher in the intervention group compared with the control group. However, the differences were not statistically significant. The highest scores in the intervention and control groups were related to light reflexes and overall skin conditions (92.6 versus 96.9), activity and breathing rate (88.3 versus 92.7), and the eye blink reflex (90.4 versus 91.7) (Table 3).
Figure 1.
Patient flow diagram.
Table 1.
Comparison of the total mean scores for mental health at birth and at three months of age and maternal anxiety scores between the intervention and control groups.
| Age | Groups | P | |
|---|---|---|---|
| Control Mean (SD) |
Intervention Mean (SD) |
||
|
| |||
| At birth | 16.07 (1.74) | 16.66 (1.51) | .013 |
| 3 months | 30.25 (2.10) | 31.05 (1.88) | .007 |
| Difference between scores at birth and after 3 months | 14.18 (2.61) | 14.38 (2.24) | .612 |
| Maternal anxiety score | 29.70 (13.33) | 24.51 (13.33) | .010 |
Values are mean (standard deviation)
Table 2.
Categorized scores for infant mental health variables at birth in the intervention and control groups.
| Index | Control (n=96) | Intervention (n=94) | Test | P | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| High (2) | Average (1) | Low (0) | High (2) | Average (1) | Low (0) | |||||||||
| % | n | % | n | % | n | % | n | % | n | % | n | |||
|
| ||||||||||||||
| Weight1 | 59.6 | 56 | 22.3 | 21 | 18.1 | 17 | 68.8 | 66 | 18.8 | 18 | 12.5 | 12 | C1 | .388 |
| Height2 | 96.8 | 91 | 3.2 | 3 | 0 | 0 | 99 | 95 | 1 | 1 | 0 | 0 | F2 | .366 |
| Head circumference3 | 86.2 | 81 | 13.8 | 13 | 0 | 0 | 81.2 | 78 | 18.7 | 18 | 0 | 0 | C | .359 |
| Apgar score4 | 96.8 | 91 | 3.2 | 3 | 0 | 0 | 97.9 | 94 | 2.1 | 2 | 0 | 0 | F | .681 |
| Skin color5 | 90.4 | 85 | 6.4 | 6 | 3.2 | 3 | 93.8 | 90 | 4.2 | 4 | 2.1 | 2 | F | .640 |
| Skin conditions6 | 68.1 | 64 | 22.3 | 21 | 9.6 | 9 | 78.1 | 75 | 16.7 | 16 | 5.2 | 5 | C | .263 |
| Crying status7 | 74.5 | 70 | 14.9 | 14 | 10.6 | 10 | 89.6 | 86 | 7.3 | 7 | 3.1 | 3 | C | .021 |
| Respiratory status8 | 87.2 | 82 | 7.4 | 7 | 5.3 | 5 | 87.5 | 84 | 10.4 | 10 | 2.1 | 2 | F | .403 |
| Health9 | 95.7 | 90 | 3.2 | 3 | 1.1 | 1 | 95.8 | 92 | 4.2 | 4 | 0 | 0 | F | .859 |
| Total number of each groups | 96 | |||||||||||||
Scores:
Less than 2500 grams=0, 2500–3000 grams=1, More than 3000 grams=2;
Less than 40 cm=0, 40–45 cm=1, More than 45 cm=2;
Less than 33 cm=0, 33–35 cm=1, More than 35 cm=2;
Less than 4=0, 4–7=1, More than 7=2;
Cyanosis=0, Pale=1, Pink and white (Normal)=2;
Acne and pimples=0, Dry=1, Smooth=2;
Intense=0, Typical=1, Calm=2;
Hard breathing=0, Rapid breathing=1, Typical breathing=2;
Unhealthy=0, With jaundice=1, Healthy=2.
Table 3.
Categorized scores for infant mental health variables at three months of age in the intervention and control groups.
| Index | Control (n=96) | Intervention (n=94) | Test | P | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| High (2) | Average (1) | Low (0) | High (2) | Average (1) | Low (0) | |||||||||
| % | n | % | n | % | n | % | n | % | n | % | n | |||
|
| ||||||||||||||
| Nutrition1 | 60.6 | 57 | 39.4 | 37 | 0 | 0 | 67.7 | 65 | 32.3 | 31 | 0 | 0 | C | .309 |
| Grasping reflex2 | 89.4 | 84 | 7.4 | 7 | 3.2 | 3 | 93.8 | 90 | 4.2 | 4 | 2.1 | 2 | F | .551 |
| Pupillary reflex3 | 92.6 | 87 | 5.3 | 5 | 2.1 | 2 | 96.9 | 93 | 3/1 | 3 | 0 | 0 | F | .274 |
| Eyelid reflex4 | 90.4 | 85 | 5.3 | 5 | 4.3 | 4 | 91.7 | 88 | 5.2 | 5 | 3.1 | 3 | F | .929 |
| The speed of sucking milk5 | 90.4 | 85 | 7.4 | 7 | 2.1 | 2 | 86.5 | 83 | 11.5 | 11 | 2.1 | 2 | F | .745 |
| Respiratory rate6 | 88.3 | 83 | 8.5 | 8 | 3.2 | 3 | 92.7 | 89 | 5.2 | 5 | 2.1 | 2 | F | .573 |
| Skin status7 | 92.6 | 87 | 4.3 | 4 | 3.2 | 3 | 96.9 | 93 | 3.1 | 3 | 0 | 0 | F | .231 |
| Hugging reactions8 | 70.2 | 66 | 25.5 | 24 | 4.3 | 4 | 75 | 72 | 21.9 | 21 | 3.1 | 3 | F | .750 |
| Reaction to mother leaving9 | 88.3 | 83 | 7.4 | 7 | 4.3 | 4 | 83.3 | 80 | 12.5 | 12 | 4.2 | 4 | F | .519 |
| The amount of sucking milk10 | 86.2 | 81 | 9.6 | 9 | 4.3 | 4 | 89.6 | 86 | 7.3 | 7 | 3.1 | 3 | F | .733 |
| Reaction during breastfeeding11 | 83 | 78 | 12.8 | 12 | 4.3 | 4 | 88.5 | 85 | 9.4 | 9 | 2.1 | 2 | F | .490 |
| The amount of sleep12 | 73.4 | 69 | 17 | 16 | 9.6 | 9 | 75 | 72 | 18.8 | 18 | 6.2 | 6 | C | .684 |
| Sleeping time13 | 59.6 | 56 | 31.9 | 30 | 8.5 | 8 | 67.7 | 65 | 26 | 25 | 6.2 | 6 | C | .499 |
| Activity14 | 88.3 | 83 | 9.6 | 9 | 2.1 | 2 | 92.7 | 89 | 6.2 | 6 | 1 | 1 | F | .513 |
| Breastfeeding status15 | 75.5 | 71 | 20.2 | 19 | 4.3 | 4 | 82.3 | 79 | 16.7 | 16 | 1 | 1 | F | .302 |
| Breastfeeding time16 | 74.5 | 70 | 25.5 | 24 | 0 | 0 | 82.3 | 79 | 17.7 | 17 | 0 | 0 | C | .190 |
| Distinguishing the baby’s hunger by the mother17 | 88.3 | 83 | 5.3 | 5 | 6.4 | 6 | 86.5 | 83 | 6.2 | 6 | 7.3 | 7 | C | .929 |
Scores: Infant formula=1, breast milk=2;
No reaction=0, Drawing back the hand=1, Taking the hand=2;
No reaction=0, Slow reaction=1, Quick reaction=2;
No reaction=0, Reactions to the object just in front=1, Follow the object with eyes=2;
Lethargic=0, Very fast=1, Normal=2;
Hard=0, Very fast=1, Normal=2;
Inflamed with acne=0, Abnormal and rough skin=1, Natural and smooth skin=2;
Mostly restless=0, Sometimes restless=1, Mostly relax=2;
Apathetic=0, Intense crying until the mother returned=1, Short cry=2;
Refusal to suck=0, Sucks little=1, Sucks enough=2;
Restless=0, Hiccups and vomiting=1, Calm down=2;
7–11 hours=0, 11–16 hours=1, 16–20 hours=2;
Too short=0, 1–2 hours=1, 3–4 hours=2;
Lethargic=0, Hyperactive=1, Normal=2;
Does not hug=0, Completely covered=1, Half-bare=2;
Appropriate time=0, Specified time=1, When baby is hungry=2;
No=0, Sometimes=1, Yes=2.
DISCUSSION
Infant mental health is a top priority among public health issues.33 Mental disorders at infancy can have long-term consequences for individuals, their families, and societies. 33 The results of the present study showed a significant difference between the intervention and control groups in the total mean scores for infant mental health variables at birth and at three months of age. Huizink et al (2002) studied the relationship between mothers’ temperament disorders and anxiety during pregnancy and their babies’ mental health and temperament traits. They collected data from 170 first-time mothers who were in their first few weeks of pregnancy and evaluated and analyzed their babies’ temperament traits at three and eight months of age through direct observation and parent reports. The results showed that anxiety during pregnancy led to a significant reduction in infant mental health at the ages of three months (P<.005) and eight months (P=.01).34 In the present study, teaching attachment behaviors to the mothers resulted in a .59-point and .80-point increase in infant mental health scores at birth and at three months of age, respectively.
In a prospective study which lasted for 14 years, O’Donnell et al studied the relationship between mothers’ temperamental disorders and anxiety during pregnancy and incidence of behavioral and mental disorders in their children between the ages of 4 and 13 years. They concluded that pregnancy anxiety and stress had caused mental, emotional, and behavioral disorders in the children and that pregnancy anxiety doubled the risk of such disorders in children (12.31% versus 6.83%).35 The research population in the present study was composed of pregnant women with normal, mild, and average anxiety levels (the women with high anxiety levels were referred to counselors). Thus, the effectiveness of the educational classes can be attributed to the subjects’ mental-emotional preparation. Bornstein believed that mothers who had insufficient knowledge of their babies’ developmental processes suffered from more mental issues which could have an effect on infant mental and physical functions.36 Accordingly, in two educational sessions in the present study, the subjects were informed about the physical changes women undergo during pregnancy, effective ways to adapt with unpleasant changes, and important facts about nutrition, exercise, rest, work, travelling, vaccination, and having sex during pregnancy. They were also informed about the formation and development of the fetus, movements of the fetus, hearing the heartbeat of the fetus, and the importance of sonography. Studies have indicated that mothers prefer skin touch with their babies to the common care methods. In this way, the baby is very close to the mother, resulting in more verbal and tactile contacts. It also facilitates and completes the care of the baby.37–39
Bowlby stressed intimate and continuous relationship between the mother and baby and deemed it essential to the baby’s mental health and emotional development as well as to the mother’s new identity as a mother.40 According to Laxton et al (2002) and Pollock et al (1999), low levels of maternal-fetal attachment could prove detrimental to the fetus.41,42 Continuous anxiety on the part of the mother, on the other hand, results in fetal restlessness and future anxiety and depression.
In a prospective study that lasted 30 years, the relationship between maternal attachment behavior and mental health of children was evaluated. Significant associations were found between how mothers and newborn babies communicated and newborn mental health (P=.026). This relationship was not observed in adulthood. After removal of confounding factors, the change in the mental health in children whose mothers behavior was were not supportive was present at 8 months. The investigators concluded that infants who did not experience attachment with their mothers are at increased risk for behavioral and emotional problems, and in the future would have fewer mental health problems.43
Another study showed that good attachment during pregnancy led to better fetal development compared with babies deprived of this communication as fetuses.44
Reduced maternal attachment during pregnancy may also affect the mental health of the mother.45–48 This maternal behavior can damage neonatal and developmental outcomes. Educational programs during pregnancy for maternal psychological well-being,49 and postpartum home visits, improve child health and development.50,51
In two educational sessions in the present study, the subjects were informed about maternal-fetal attachment, the effects of such attachment on the mother, fetus, and baby, and ways to enhance such attachment through group discussion and role playing. Actions such as speaking to the fetus, looking at and caressing the stomach, giving the fetus a name, encouraging other family members to talk to the fetus, visualizing the face of the fetus, visualizing breastfeeding, and hugging the baby, were stressed as techniques to enhance maternal-fetal attachment. Hence, the better mental health of infants in the intervention group might have resulted from the education about attachment. Studies have shown that interaction between the mother and fetus increases the attachment.52 Feeling the movements of the fetus also contributed to attachment behaviors.53 Once the fetus moves, it feels more real to the mother and mothers with higher levels of attachment feel more movements.54 Moreover, counting the movements of the fetus involves the mother in actions that stimulate her emotions and results in greater interaction with the fetus. It should be noted that fetal movement and heartbeat is associated with the pregnancy stage and development of the nervous system.55
According to Carter et al, there is reliable evidence that maternal-fetal attachment is reflected in the mother’s behaviours. Investigating the effects of interventions during pregnancy on postnatal attachment behaviors, they noticed that the mothers who had caressed their stomachs and talked to the fetus had greater interest in their babies after birth.16 Fearon (2010) also maintained that mothers who were less attached to their babies were more likely to have babies with mental disorders. Although this correlation was not strong in that study, it was statistically significant.56
The relationship between attachment behaviors and infant mental peace can be explained according to studies on animal wombs, which have shown that the womb is a noisy environment. The noises from the mother’s cardiac, gastrointestinal, and vocal systems are among the noises heard by the fetus.57 Changes in the mother’s heartbeat, blood pressure, and gastrointestinal movements act as auditory stimuli to the baby and make it react to its environment. The reactions of the fetus to maternal anxiety include reduced cardiac flexibility, tachycardia, and limited movement. On the other hand, anxiety-reducing interventions have been reported to be correlated with greater cardiac flexibility and less rigidity in the umbilical artery.58 Thus, interventions that reduce maternal anxiety during pregnancy lower both the mother’s and her baby’s heart rate. In fact, evidence has demonstrated that maternal and fetal heart rates are related.50 An increase in beat-to-beat variability of fetal heart rate is a major factor in reducing anxiety and mental peace after birth. It appears that teaching attachment behaviors results in a reduction in maternal anxiety and enhancement of the infant’s mental health.
A limitation of our study might be that although the occurrence of stressful and shocking events in the mothers’ lives was taken into account, it was not possible to measure the influence of everyday worries. Yet, by randomly assigning the subjects to the two groups, the researchers tried to minimize the influence of personal differences. Another limitation and problem was the means of infant mental health assessment at three months postpartum; the mothers were followed by means of phone calls by the researcher. We suggest that future activities include training fathers on attachment skills to improve understanding of the effects on infant mental health. We also suggest studies on neonatal mental health in the delivery room, including training of the delivery team.
Research should address:
Training fathers on attachment skills for paternal participant promotion in pregnancy.
Training the fathers on attachment skills as they relate to infant mental health.
Prevalence of neonatal mental health issues in the delivery room.
Training the maternity care team (doctors, midwives and nurses) on the criteria for diagnosis of mental health of newborns at birth and a few months later.
In conclusion, educating mothers on attachment skills enhanced the attachment between the mothers and their babies and reduced anxiety in the babies which, in turn, improved their mental health at birth and at the age of three months. We suggest that educational programs on attachment skills for pregnant women to be incorporated into routine prenatal care.
Acknowledgments
The present article was extracted from the thesis of Akran Dokuhaki, (thesis number: 92-6857, IRCT: 2014042217393N1). The authors would like to thank the Research Vice-chancellor of Shiraz University of Medical Sciences for financially supporting the study. The authors would like to thank Dr. Nasrin Shokrpour at Center for Development of Clinical Research of Nemazee Hospital for editorial assistance.
Footnotes
Clinical trial registration
Registered in the International Centre for Iranian Registry of Clinical Trials.
Conflict of interests
None declared.
REFERENCES
- 1.Zolfaghari Motlagh M, Jazayeri AR, Khoshabi K, Mazaheri MA, Karimlou M. Effectiveness of attachment based therapy on reduction of symptoms in separation anxiety disorder. Iranian journal of psychiatry and clinical psychology. 2009;14(4):380–8. (persian) [Google Scholar]
- 2.Robinson LB, Nackerud Larry, Margaret The relationship of attachment theory and perinatal loss. Death studies. 1999;23(3):257–70. doi: 10.1080/074811899201073. [DOI] [PubMed] [Google Scholar]
- 3.Winkler J, Hrdinová J, Kukla L. [Maternal bonding and a healthy life style during pregnancy]. Cas Lek Cesk. 2000 Feb 16;139(3):71–3.4. [PubMed] [Google Scholar]
- 4.Muller ME. Development of the Prenatal Attachment Inventory. Western journal of nursing research. 1993 Apr;15(2):199–211. doi: 10.1177/019394599301500205. [DOI] [PubMed] [Google Scholar]
- 5.Dunkel Schetter C, Tanner L. Anxiety, depression and stress in pregnancy: implications for mothers, children, research, and practice. Current opinion in psychiatry. 2012 Mar;25(2):141–8. doi: 10.1097/YCO.0b013e3283503680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Akbarzadeh M, Rafiee B, Asadi N, Zare N. Comparison of two Methods of Relaxation and Maternal- Fetal attachment on the Fetal Heart pattern. NAUTILUS. 2014;128(1):104–12. [Google Scholar]
- 7.Oates MR. Adverse effects of maternal antenatal anxiety on children: causal effect or developmental continuum? Br J Psychiatry. 2002 Jun;180:478–9. doi: 10.1192/bjp.180.6.478. [DOI] [PubMed] [Google Scholar]
- 8.Punamaki RL, Repokari L, Vilska S, Poikkeus P, Tiitinen A, Sinkkonen J, et al. Maternal mental health and medical predictors of infant developmental and health problems from pregnancy to one year: does former infertility matter? Infant behavior & development. 2006 Apr;29(2):230–42. doi: 10.1016/j.infbeh.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 9.Sjöström K, Valentin L, Thelin T, Marsál K. Maternal anxiety in late pregnancy: effect on fetal movements and fetal heart rate. Early human development. 2002 Apr;67(1):87–100. doi: 10.1016/s0378-3782(01)00256-0. [DOI] [PubMed] [Google Scholar]
- 10.Woolery A, Myers H, Sternlieb B, Zeltzer L. A yoga intervention for young adults with elevated symptoms of depression. Alternative therapies in health and medicine. 2004 Mar-Apr;10(2):60–3. [PubMed] [Google Scholar]
- 11.Khalsa SBS. Treatment of chronic insomnia with yoga: A preliminary study with sleep–wake diaries. Appl Psychophysiol Biofeedback. 2004 Dec;29(4):269–78. doi: 10.1007/s10484-004-0387-0. [DOI] [PubMed] [Google Scholar]
- 12.Toosi M, Akbarzadeh M, Sharif F, Zare N. The Reduction of Anxiety and Improved Maternal Attachment to Fetuses and Neonates by Relaxation Training in Primigravida Women. Women’s Health Bulletin. 2014;April(1):e18968. [Google Scholar]
- 13.Toosi M, akbarzadeh M, Zare N, sharif F. Comparison of the effects of attachment behavior and relaxation training on maternal fetal attachment and infant in prime pregnant women. Journal of Fundamentals of Mental Health. 2014 Summer;2(62):142–9. (persian) [Google Scholar]
- 14.Farrant BM, Maybery MT, Fletcher J. Maternal Attachment Status, Mother-Child Emotion Talk, Emotion Understanding, and Child Conduct Problems. Child Development Research. 2013;2013 [Google Scholar]
- 15.Brumariu LE, Kerns KA, Seibert A. Mother–child attachment, emotion regulation, and anxiety symptoms in middle childhood. Personal Relationships. 2012 Sep;19(3):569–85. [Google Scholar]
- 16.Carter-Jessop L. Promoting maternal attachment through prenatal intervention. MCN: The American Journal of Maternal/Child Nursing. 1981 Mar-Apr;6(2):107–12. doi: 10.1097/00005721-198103000-00009. [DOI] [PubMed] [Google Scholar]
- 17.Burgess KB, Marshall PJ, Rubin KH, Fox NA. Infant attachment and temperament as predictors of subsequent externalizing problems and cardiac physiology. J Child Psychol Psychiatry. 2003 Sep;44(6):819–31. doi: 10.1111/1469-7610.00167. [DOI] [PubMed] [Google Scholar]
- 18.Franc N, Maury M, Purper-Ouakil D. [ADHD and attachment processes: are they related?]. Encephale. 2009 Jun;35(3):256–61. doi: 10.1016/j.encep.2008.04.007. [DOI] [PubMed] [Google Scholar]
- 19.Lee G, McCreary L, Breitmayer B, Kim MJ, Yang S. Promoting mother-infant interaction and infant mental health in low-income Korean families: attachment-based cognitive behavioral approach. Journal for specialists in pediatric nursing : JSPN. 2013 Oct;18(4):265–76. doi: 10.1111/jspn.12034. [DOI] [PubMed] [Google Scholar]
- 20.Koniak-griffin D. The relationship between social support, self-esteem, and maternal-fetal attachment in adolescents. Res Nurs Health. 1988 Aug;11(4):269–78. doi: 10.1002/nur.4770110408. [DOI] [PubMed] [Google Scholar]
- 21.Alhusen JL, Hayat MJ, Gross D. A longitudinal study of maternal attachment and infant developmental outcomes. Archives of women’s mental health. 2013 Dec;16(6):521–9. doi: 10.1007/s00737-013-0357-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Uguz F, Gezginc K, Kayhan F, Sari S, Buyukoz D. Is pregnancy associated with mood and anxiety disorders? A cross-sectional study. General hospital psychiatry. 2010 Mar-Apr;32(2):213–15. doi: 10.1016/j.genhosppsych.2009.11.002. [DOI] [PubMed] [Google Scholar]
- 23.Vythilingum B. Anxiety disorders in pregnancy. Current psychiatry reports. 2008 Aug;10(4):331–5. doi: 10.1007/s11920-008-0053-y. [DOI] [PubMed] [Google Scholar]
- 24.Moradi Zahra, Akbarzadeh Marzieh, Moradi Parvin, Toosi Monieh, Hadianfard Mohammad Javad. The Effect of Acupressure at GB-21 and SP-6 Acupoints on Anxiety Level and Maternal-Fetal Attachment in Primiparous Women: a Randomized Controlled Clinical Trial. Nurs midwifery stud. 2014;3(3):e19948. doi: 10.17795/nmsjournal19948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Akbarzadeh F, Ranjbar Kouchaksaraei F, Bagheri Z, Ghezel M. Effect of preoperative informative information and reassurance in decreasing anxiety of patients who are candidate for coronary artery bypass graft surgery. J Cardovasc Thorac Res. 2009;1(2):25–8. [Google Scholar]
- 26.Lee MK, Chang SB, Lee HS, Kim HS. Effects of San-Yin-Jiao (Sp6) acupressure on anxiety, pulse and neonatal status in women during labor. Korean J Women Health Nurs. 2003;9(2):138–151. [Google Scholar]
- 27.Aghamohammadi Kalkhoran M, Karimollahi M. Religiousness and preoperative anxiety: a correlational study. Ann Gen Psychiatry. 2007 Jun 29;6:17. doi: 10.1186/1744-859X-6-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cunninngham FG, Gant NF, Leveno KJ, Gilstrap Lc, Hauth JC, Wenstrom KD. Williams Obstetrics and Gynecology. 23st ed. Michigan: Mc Gepw-hill; 2010. [Google Scholar]
- 29.Kalkhoran MA, Karimollahi M. Religiousness and preoperative anxiety: a correlational study. Annals of General Psychiatry. 2007 Jun;6(1):1744–859. doi: 10.1186/1744-859X-6-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nejati H. Developmental psychology. Tehran: Mehshad Publications; 1992. (persian) [Google Scholar]
- 31.Shayeghian Z, Rasolzadeh Tabatabaey SK. Effect of Maternal Anxiety during Third Trimester on Pregnancy Outcomes and Infants’ Mental Health. Hayat. 2009;14(4):57–65. (-persian) [Google Scholar]
- 32.World Health O. Caring for children and adolescents with mental disorders: setting WHO directions. 2003. [Google Scholar]
- 33.World Health O. Mental health: Strengthening our response (Fact sheet No. 220) Geneva, Switzerland: Author; 2010. [Google Scholar]
- 34.Huizink AC, Robles de Medina PG, Mulder EJ, Visser GH, Buitelaar JK. Psychological measures of prenatal stress as predictors of infant temperament. Journal of the American Academy of Child & Adolescent Psychiatry. 2002 Sep;41(9):1078–1085. doi: 10.1097/00004583-200209000-00008. [DOI] [PubMed] [Google Scholar]
- 35.O’Donnell KJ, Glover V, Barker ED, O’Connor TG. The persisting effect of maternal mood in pregnancy on childhood psychopathology. Dev Psychopathol. 2014 May;26(2):393–403. doi: 10.1017/S0954579414000029. [DOI] [PubMed] [Google Scholar]
- 36.Bornstein MH, Cote LR. “Who is sitting across from me?” Immigrant mothers’ knowledge of parenting and children’s development. Pediatrics. 2004 Nov;114(5):e557–e64. doi: 10.1542/peds.2004-0713. [DOI] [PubMed] [Google Scholar]
- 37.Carfoot S, Williamson P, Dickson R. A randomised controlled trial in the north of England examining the effects of skin-to-skin care on breast feeding. Midwifery. 2005 Mar;21(1):71–9. doi: 10.1016/j.midw.2004.09.002. [DOI] [PubMed] [Google Scholar]
- 38.Crenshaw J. Care practice# 6: No separation of mother and baby, with unlimited opportunities for breastfeeding. J Perinat Educ. 2007 Summer;16(3):39–43. doi: 10.1624/105812407X217147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Velandia M, Matthisen AS, Uvnäs-Moberg K, Nissen E. Onset of Vocal Interaction Between Parents and Newborns in Skin to Skin Contact Immediately After Elective Cesarean Section. See comment in PubMed Commons below Birth. 2010 Sep;37(3):192–201. doi: 10.1111/j.1523-536X.2010.00406.x. [DOI] [PubMed] [Google Scholar]
- 40.Bowlby J. Attachment And Loss. Vol. 2: Separation: Anxiety And An: Evt. Penguin books; 1973. [Google Scholar]
- 41.Laxton-Kane M, Slade P. The role of maternal prenatal attachment in a woman’s experience of pregnancy and implications for the process of care. Journal of Reproductive and Infant Psychology. 2002 Agu;20(4):253–66. [Google Scholar]
- 42.Pollock PH, Percy A. Maternal antenatal attachment style and potential fetal abuse. Child Abuse Negl. 1999 Dec;23(12):1345–57. doi: 10.1016/s0145-2134(99)00101-5. [DOI] [PubMed] [Google Scholar]
- 43.Fan AP, Buka SL, Kosik RO, Chen Y-S, Wang S-J, Su T-P, et al. Association between maternal behavior in infancy and adult mental health: A 30-year prospective study. Comprehensive psychiatry. 2014 Feb;55(2):283–9. doi: 10.1016/j.comppsych.2013.08.024. [DOI] [PubMed] [Google Scholar]
- 44.Alhusen JL, Hayat MJ, Gross D. A longitudinal study of maternal attachment and infant developmental outcomes. Archives of women’s mental health. 2013 Dec;16(6):521–9. doi: 10.1007/s00737-013-0357-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Alhusen JL, Gross D, Hayat MJ, Rose L, Sharps P. The role of mental health on maternal-fetal attachment in low-income women. J Obstet Gynecol Neonatal Nurs. 2012 Nov;41(6):E71–E81. doi: 10.1111/j.1552-6909.2012.01385.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Alhusen JL, Gross D, Hayat MJ, Woods AB, Sharps PW. The influence of maternal-fetal attachment and health practices on neonatal outcomes in low-income, urban women. Res Nurs Health. 2012 Apr;35(2):112–20. doi: 10.1002/nur.21464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Brandon AR, Trivedi MH, Hynan LS, Miltenberger PD, Labat DB, Rifkin JB, et al. Prenatal depression in women hospitalized for obstetric risk. J Clin Psychiatry. 2008 Apr;69(4):635–43. doi: 10.4088/jcp.v69n0417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.McFarland J, Salisbury AL, Battle CL, Hawes K, Halloran K, Lester BM. Major depressive disorder during pregnancy and emotional attachment to the fetus. Arch Womens Ment Health. 2011 Oct;14(5):425–34. doi: 10.1007/s00737-011-0237-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kingston D, Tough S, Whitfield H. Prenatal and postpartum maternal psychological distress and infant development: A systematic review. Child Psychiatry Hum Dev. 2012 Oct;43(5):683–714. doi: 10.1007/s10578-012-0291-4. [DOI] [PubMed] [Google Scholar]
- 50.Olds DL, Robinson J, O’Brien R, Luckey DW, Pettitt LM, Henderson CR, et al. Home visiting by paraprofessionals and by nurses: A randomized, controlled trial. Pediatrics. 2002 Sep;110(3):486–96. doi: 10.1542/peds.110.3.486. [DOI] [PubMed] [Google Scholar]
- 51.Olds DL, Kitzman HJ, Cole RE, Hanks CA, Arcoleo KJ, Anson EA, et al. Enduring effects of prenatal and infancy home visiting by nurses on maternal life course and government spending: follow-up of a randomized trial among children at age 12 years. Arch Pediatr Adolesc Med. 2010 May;164(5):419–24. doi: 10.1001/archpediatrics.2010.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Maeda K, Morokuma S, Yoshida S, Ito T, Pooh RK, Serizawa M. Fetal behavior analyzed by ultrasonic actocardiogram in cases with central nervous system lesions. J Perinat Med. 2006;34(5):398–403. doi: 10.1515/JPM.2006.079. [DOI] [PubMed] [Google Scholar]
- 53.van Dixhoorn J, White A. Relaxation therapy for rehabilitation and prevention in ischaemic heart disease: a systematic review and meta-analysis. Eur J Cardiovasc Prev Rehabil. 2005 Jun;12(3):193–202. doi: 10.1097/00149831-200506000-00002. [DOI] [PubMed] [Google Scholar]
- 54.Cunningham G, Leveno J, Bloom S. Williams OBSTETRICS. 23. Tehran: Golban; 2010. [Google Scholar]
- 55.Velazquez MD, Rayburn WF. Antenatal evaluation of the fetus using fetal movement monitoring. Clinical obstetrics and gynecology. 2002;45(4):993–1004. doi: 10.1097/00003081-200212000-00006. [DOI] [PubMed] [Google Scholar]
- 56.Fearon R, Bakermans-Kranenburg MJ, Van IJzendoorn MH, Lapsley Am, Roisman GI. The Significance of Insecure Attachment and Disorganization in the Development of Children’s Externalizing Behavior: A Meta-Analytic Study. Child Dev. 2010 Mar-Apr;81(2):435–56. doi: 10.1111/j.1467-8624.2009.01405.x. [DOI] [PubMed] [Google Scholar]
- 57.Galen Buckwalter J, Stanczyk ZF, Mc-Cleary AC, Bluestein WB, Buckwalter KD, Rankin PK, et al. Pregnancy, the postpartum, and steroid hormones: effects on cognition and mood. doi: 10.1016/s0306-4530(98)00044-4. [DOI] [PubMed] [Google Scholar]
- 58.DiPietro JA, Costigan KA, Nelson P, Gurewitsch ED, Laudenslager ML. Fetal responses to induced maternal relaxation during pregnancy. Biol Psychol. 2008 Jan;77(1):11–19. doi: 10.1016/j.biopsycho.2007.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]