Abstract
BACKGROUND AND OBJECTIVES
Primary percutaneous coronary intervention (pPCI) has been recognized as an effective management strategy for acute ST-segment–elevation myocardial infarction (STEMI). However, there is no first-hand information regarding the quality of pPCI procedures in the Arabian Gulf countries. This study aims to explore the quality of pPCI practice.
DESIGN AND SETTINGS
The Gulf Race II was designed as a prospective, multinational, multicentre registry of acute coronary events, focusing on the epidemiology, management practices, and outcomes of patients with acute coronary syndrome. The study recruited consecutive patients aged 18 years and above from 65 hospitals in 6 adjacent Middle Eastern countries (Bahrain, Saudi Arabia, Qatar, Oman, United Arab Emirates, and Yemen).
PATIENTS AND METHODS
We used data from the Gulf Registry of Acute Coronary Events (Gulf RACE 2). We analyzed data on patients who received pPCI to assess the guidelines-supported performance measure of door-to-balloon (D2B) ≤ 90 minutes and its impact on morbidity and mortality.
RESULTS
Of 3432 patients with STEMI, slightly more than half (53%, n=1832) were admitted to a hospital with a cardiac catheterization laboratory (Cath-Lab). Of these, only 1006 patients (55%) received reperfusion therapy, and pPCI was used in a small predominantly male subgroup (11% of the STEMI cohort admitted to hospitals with Cath-Lab, n=198). The median D2B time in the pPCI cohort was 85 minutes, and a D2B of ≤90 minutes was achieved in only 55%. Patients with timely pPCI (D2B ≤ 90 minutes) were less likely to have cardiogenic shock and require intra-aortic balloon pump. In-hospital, 1-month and 1-year mortality were not statistically in favor of timely pPCI.
CONCLUSION
Primary PCI was underused in the Gulf region with low rate of acute reperfusion and no timely pPCI and thus no mortality benefit.
ST-segment–elevation myocardial infarction (STEMI) is a common condition associated with high mortality.1 However, there has been a considerable decline in mortality as a consequence of improvements in initial therapy, including fibrinolysis and primary percutaneous coronary intervention (pPCI). Despite the improvement in overall management (fibrinolysis and pPCI) of STEMI, time is of paramount importance for initiating thrombolysis and performing pPCI in improving survival.2 The America College of Cardiology (ACC), American Heart Association (AHA), and the European Society of Cardiology (ESC) recommended that all STEMI patients should undergo rapid evaluation for reperfusion therapy and have reperfusion strategy implemented promptly after contact with the medical system.3,4
Based on available data from clinical trials, it is concluded that the state-of-the-art management for patients with STEMI is pPCI and is considered as a preferred method of reperfusion.5 Several trials have shown that time ≤90 minutes has been associated with smaller infarct sizes, fewer major adverse cardiovascular events, and better long-term survival.6–11 International guidelines in the management of patients with STEMI recommended several performance measures to monitor the quality of delivered patient care.12 Of particular interest are the door-to-balloon (D2B) time (arrival at hospital to pPCI) and overall health care system delay (first medical contact to reperfusion); both of these are acknowledged as valuable performance indicators.13–16 A previous study in the Arabian Gulf countries, where the prevalence of STEMI is considerably high, showed that about 30% of patients with STEMI arrived at hospital more than 12 hours from the onset of chest pain.17 In all, pPCI as a preferred reperfusion strategy in STEMI requires optimal systems of care and logistics to enable rapid treatment of all patients. In this study, we aim to explore the quality of pPCI practice and its impact on morbidity and mortality.
PATIENTS AND METHODS
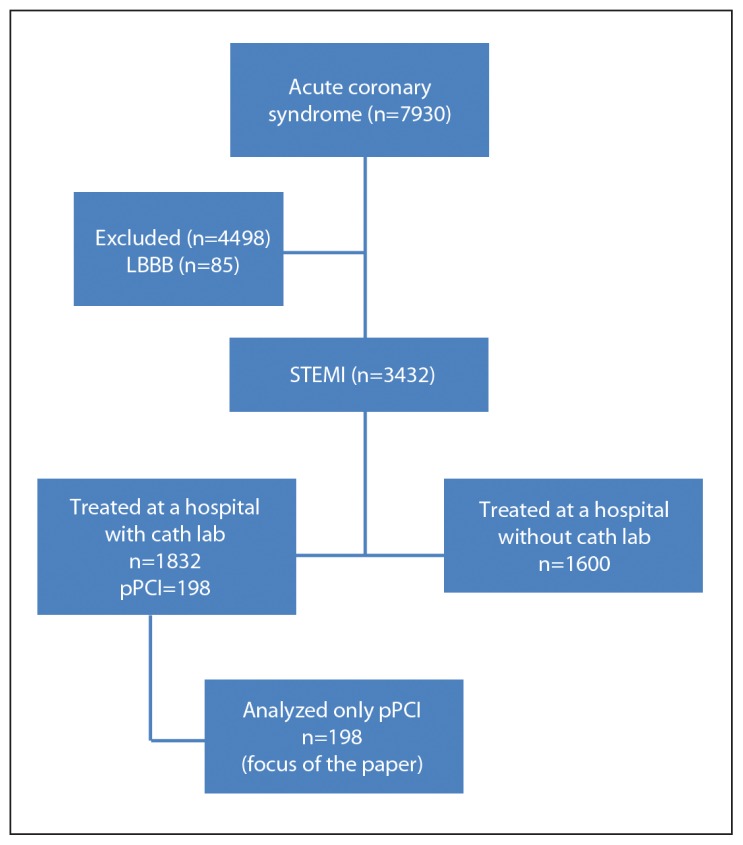
The Gulf Registry of Acute Coronary Events (Gulf RACE 2) study was conducted between October 2008 and June 2009 in 6 Arabian Gulf countries (Bahrain, Saudi Arabia, Qatar, Oman, UAE, and Yemen). The study protocols were approved by the institutional ethical review boards of all the participating hospitals. Details of the methodology have been previously described.18 Of the total STEMI patients, we extracted data for analysis from patients who have had pPCI, as indicated in Figure 1.
Figure 1.
Cohort patients with STEMI and analyzed sample size of pPCI from the Gulf RACE 2 registry.
Statistical analysis
All data were analyzed using SPSS, version 20.0 (SPSS, Inc., Chicago, IL USA). Descriptive summary measures were obtained. Chi-square test or Fischer exact test were used to compare between groups. Multivariate logistic regression analyses were used to identify independent predictors of morbidity and mortality. Statistical significance was set at a 0.05 level.
RESULTS
Among the 7930 patients with acute coronary syndrome in the GULF RACE 2 registry, 3432 were diagnosed with STEMI (based on electrocardiography [ECG] at presentation). Of these, 1832 were admitted to the surveyed hospitals with cardiac catheterization laboratory facilities. However, only 198 (10.8%) patients received pPCI. These patients had a mean age of 54.0 (11.8) years, were mostly males (87%), and often overweight or obese across all age groups. Our cohort pPCI patients had significant coronary risk factors: 40.8% dyslipidemia, 49.2% diabetes mellitus, 35.5% hypertension, and 54.5% smokers. A significant proportion also had a previous history of coronary artery disease who have had pPCI (12.6%), as shown in Table 1.
Table 1.
The clinical characteristics of patients with STEMI presenting to hospitals with catheterization laboratory, by type of therapy (n=1832).
| Variables | No reperfusion (N=826) | Reperfusion (N=1006) | P value | |
|---|---|---|---|---|
| TT (n=808) | pPCI (n=198) | |||
| N (%) | N (%) | N (%) | ||
|
| ||||
| Age (y) | 0001 | |||
| Less than 30 | 12.0 (1.5) | 12.0 (1.5) | 2.0 (1.0) | |
| 30–39 | 70.0 (8.5) | 81.0(10.1) | 15.0 (7.6) | |
| 40–49 | 215.0 (26.0) | 278.0 (34.4) | 59.0 (29.8) | |
| 50–59 | 236.0 (28.6) | 263.0 (32.5) | 59.0 (29.8) | |
| 60–69 | 154.0 (18.6) | 121.0 (15.0) | 37.0 (18.7) | |
| 70–79 | 88.0 (10.7) | 45.0 (5.6) | 24.0 (12.1) | |
| 80+ | 51.0 (6.2) | 8.0 (1.0) | 2.0 (1.0) | |
| Gender | ||||
| Male | 708.0 (85.7) | 742(91.8) | 174 (87.9) | .0001 |
| BMI (kg/m2) | .052 | |||
| <18.5 | 23.0 (2.8) | 15.0 (1.9) | 2.0 (1.0) | |
| Normal 18.5–24.9 | 306.0 (37.1) | 289.0 (35.8) | 78.0 (39.6) | |
| Overweight 25–29.9 | 341.0 (41.3) | 364.0 (45.1) | 66.0 (33.5) | |
| Obese 30–34.9 | 115.0 (13.9) | 112.0 (13.9) | 38.0 (19.3) | |
| Morbid obesity 35–40 | 26.0 (3.2) | 17.0 (2.1) | 10.0 (5.1) | |
| ≥40 | 14.0 (1.7) | 10.0 (1.2) | 3.0 (1.5) | |
| WC (cm) | .256 | |||
| <88 | 205.0 (40.6) | 145.0 (35.0) | 19.0 (31.1) | |
| 88–102 | 213.0 (42.2) | 193.0 (46.6) | 33.0 (54.1) | |
| >102 | 87.0 (17.2) | 76.0 (18.4) | 9.0 (14..8) | |
| Past medical history | ||||
| CAD | 183.0 (22.5) | 161.0 (20.1) | 50.0 (25.5) | .204 |
| MI | 104.0 (13.0) | 77.0 (9.7) | 29.0 (14.8) | .044 |
| PCI | 31.0 (3.8) | 39.0 (4.8) | 25.0 (12.6) | .0001 |
| CABG | 8.0 (1.0) | 6.0 (0.7) | 3.0 (1.5) | .592 |
| HF | 13.0 (1.6) | 11.0 (1.4) | 6.0 (3.0) | .256 |
| VHD | 5.0 (0.6) | 0.0 (0.0) | 1.0 (0.5) | .089 |
| Stroke/TIA | 42.0 (5.1) | 14.0 (1.7) | 7.0 (3.5) | .001 |
| CKF | 14.0 (1.7) | 7.0 (0.9) | 2.0 (1.0) | .292 |
| PAD | 12.0 (1.5) | 6.0 (0.8) | 2.0 (1.0) | .365 |
| DM | 313.0 (38.7) | 243.0 (30.5) | 97.0 (49.2) | .000 |
| Hypertension | 310.0 (38.0) | 259.0 (32.5) | 70.0 (35.5) | .073 |
| Hyperlipidemia | 145.0 (20.6) | 150.0 (24.2) | 60.0 (40.8) | .0001 |
| Family history of PCAD | 67.0 (9.0) | 82.0 (11.5) | 32.0 (18.1) | .002 |
Key: pPCI: primary percutaneous coronary intervention: N: frequency; (%): percentage; TT: thrombolytic therapy; BMI: body mass index; WC: waist circumference; CAD: coronary artery disease; MI: myocardial Infarction; PCI: percutaneous coronary intervention; CABG: coronary artery bypass grafting; HF: heart failure; VHD: valvular heart disease; TIA: transient ischemic attack; CKF: chronic kidney failure; PAD: peripheral arterial disease; DM: diabetes mellitus; PCAD: premature coronary artery disease (family history).
Table 2 shows the characteristics of patients who received timely pPCI (D2B ≤ 90 minutes) versus delayed pPCI (D2B > 90 minutes). The use of ambulance services was substantially low (<30%) in both groups, but not significantly lower in delayed pPCI patients (27.7% vs. 16.6%; P=.06). Timely pPCI was seen more frequenty in the age group between 40 and 59 years. Majority of patients (91%) arrived at hospital within 12 hours from the onset of chest pain. We did not find significant differences between the groups (timely pPCI-D2B ≤90 minutes versus delayed pPCI-D2B >90 minutes) pertaining to age, body mass index, comorbid conditions, hospital arrival time (on/off working hours), STEMI type on ECG, and clinical vital signs. Table 3 shows no significant differences in medication and types of stents used in both groups, except for the loading dose of 600 mg clopidorgrel in favor of timely pPCI (68.5% vs. 48.9%; P=.02). Table 4 shows that unadjusted cardiogenic shock and Intra-aortic balloon pump (IABP) use were significantly higher in delayed pPCI.
Table 2.
Demographic and clinical characteristics of patients who received timely vs. delayed pPCI.
| Variable | Timely pPCI (≤90 min) [N=108] | Delayed pPCI (>90 min) [N=90] | P value |
|---|---|---|---|
|
| |||
| Age (y) | .027 | ||
| <30 | 1.0 (0.9) | 1.0 (1.1) | |
| 30–39 | 4.0 (3.7) | 11.0 (12.2) | |
| 40–49 | 36.0 (33.3) | 23.0 (25.6) | |
| 50–59 | 39.0 (36.1) | 20.0 (22.2) | |
| 60–69 | 15.0 (13.9) | 22.0 (24.4) | |
| 70–79 | 13.0 (12.0) | 11.0 (12.2) | |
| 80+ | 0.0 (0.0) | 2.0 (2.2) | |
| Age (mean±SD) | 53.4 (10.7) | 54.8 (12.9) | .41 |
| Gender | |||
| Male | 97.0 (89.8) | 77.0 (85.6) | .389 |
| BMI (kg/m2) | .718 | ||
| 18.5–24.9 | 44.0 (40.7) | 36.0 (40.4) | |
| 25–29.9 | 37.0 (34.3) | 29.0 (32.6) | |
| 30+ | 27.0 (25.0) | 24.0 (26.9) | |
| Clinical history | |||
| DM | 48.0 (44.4) | 49.0(55.1) | .154 |
| Hypertension | 40.0 (37.0) | 30.0 (33.7) | .656 |
| History of angina | 23.0 (21.7) | 27.0 (30) | .193 |
| History of MI | 15.0 (14.0) | 14.0 (15.7) | .840 |
| History of previous PCI | 13.0 (12.0) | 12.0 (13.3) | .832 |
| History of CABG | 1.0 (0.9) | 2.0 (2.2) | .592 |
| History of HF | 1.0 (0.9) | 5.0 (5.6) | .095 |
| Smoking | 63.0 (58.3) | 45.0 (50.0) | .255 |
| Mode of arrival to hospital | .063 | ||
| Ambulance | 30.0 (27.7) | 15.0 (16.6) | |
| Private | 78.0 (72.2) | 75.0 (83.3) | |
| Time since onset of chest pain | |||
| <12 h | 94.0 (90.7) | 87.0 (96.6) | .02 |
| <2 h | 42.0 (38.8) | 32.0 (35.5) | .66 |
| ECG findings | |||
| Anteroseptal | 52.0 (48.1) | 52.0 (57.8) | .192 |
| Inferior | 31.0 (28.7) | 23.0 (25.6) | .634 |
| Posteriolateral | 25.0 (23.1) | 15.0 (16.7) | .289 |
| Presenting characteristics | |||
| SBP>90 mmHg | 105.0 (95.4) | 84.0 (93.3) | .551 |
| Killip class I | 97.0 (89.8) | 75.0 (83.3) | .208 |
| Time of presentation | .669 | ||
| 8:00 AM to 5:00 PM | 53.0 (49.1) | 41.0 (45.6) | |
| Off clinic hours | 55.0 (50.9) | 49 (54.4) | |
| D2B in min Mean (SD) |
57 (19) | 175 (143) | .0001 |
| Median (minimum-maximum) | 60 (13–89) | 121 (90–1248) | |
| All countries | 108.0 (54.5) | 90.0 (47.2) | .00001 |
| Bahrain | 43.0 (76.8) | 13.0 (23.2) | |
| UAE | 15.0 (71.4) | 6.0 (28.6) | |
| Qatar | 10.0 (62.5) | 6.0 (37.5) | |
| Saudi Arabia | 38.0 (40.9) | 55.0 (59.1) | |
| Yemen | 2.0 (22.2) | 7.0 (77.8) | |
| Oman | 0.0 (0.0) | 3.0 (100.0) | |
Key: pPCI: Primary percutaneous coronary intervention; N: frequency; BMI: Body mass index; DM: diabetes mellitus; MI: myocardial infarction; CABG: coronary angio bypass grafting; HF: heart failure; ECG: electrocardiogram; SBP: systolic blood pressure; Killip class I: includes individuals with no clinical signs of heart failure; AM: Morning; PM: evening.
Table 3.
Medications on admission (home), during hospitalization and at discharge from hospital.
| Variable | Timely PCI (<90 min) (N=108) | Delayed PCI (> 90 min) (N=90) | P value |
|---|---|---|---|
|
| |||
| First 24 h of admission | |||
| Aspirin | 107.0 (99.1) | 88.0 (97.8) | .432 |
| Clopidogrel | 107.0 (99.1) | 88.0 (97.8) | .432 |
| Loading 600 mg | 74.0 (68.5) | 44.0 (48.9) | .025 |
| Beta-blocker | 89.0 (82.4) | 73.0 (81.1) | .478 |
| ACEi/ARB | 81.0 (75.0) | 70.0 (77.8) | .387 |
| Statin | 107.0 (99.1) | 87.0 (96.7) | .231 |
| Prior to PCI | |||
| Anticoagulation | 101.0 (93.5) | 79.0 (87.7) | .162 |
| GPIIbIIIa inhibitor | 68.0 (55.7) | .0 | .389 |
| Type of stents: | |||
| BMS | 57.0 (54.3) | 40.0 (50.0) | .738 |
| At discharge: | |||
| Aspirin | 103.0 (95.3) | 82.0 (91.1) | .260 |
| Clopidogrel | 103.0 (95.3) | 82.0 (91.1) | 260 |
| Beta-blocker | 98.0 (90.7) | 76.0 (85.4) | .271 |
| ACEi/ARB | 83.0 (76.9) | 73.0 (82.0) | .385 |
| Statin | 104.0 (96.3) | 80.0 (89.9) | .085 |
Key: ACEi: Angiotensin-converting enzyme inhibitors; ARB: angiotensin receptor blocker; GIIbIIIa: glycoprotein 2b-3a inhibitor.
Table 4.
Clinical outcomes, type of reperfusion therapy.
| Outcome | Timely PCI (<90 min) [N = 108] | Delayed PCI (>90 min) [N = 90] | P value |
|---|---|---|---|
|
| |||
| In hospital complications | |||
| Recurrent ischemia/Re-infarction | 16.0 (14.8) | 9.0 (10.0) | .392 |
| HF | 12.0 (11.1) | 12.0 (13.3) | .633 |
| Ventilation | 6.0 (5.6) | 11.0 (12.2) | .095 |
| IABP | 4.0 (3.7) | 10.0 (11.1) | .043 |
| Inotrope | 14.0 (12.9) | 17.0 (8.8) | .326 |
| Cardiogenic shock | 7.0 (8.5) | 15.0 (16.6) | .023 |
| VT/VF | 5.0 (4.6) | 9.0 (10.0) | .17 |
| Stroke | 0.0 (0.0) | 2.0 (2.2) | .201 |
| Mortality | |||
| In-hospital | 3.0 (2.8) | 7.0 (7.8) | .19 |
| 1 mo | 4.0 (3.7) | 8.0 (8.8) | .14 |
| 1 y | 8.0 (7.4) | 14.0 (15.5) | .11 |
Key: N: Frequency; HF: heart failure; IABP: intra-aortic balloon pump; VT/VF: ventricular tachycardia/ventricular fibrillation.
DISCUSSION
Despite strong recommendations for reperfusion therapy (thrombolysis or pPCI), only 55% of STEMI patients presented to our catheterization laboratory (Cath-Lab) capable hospitals received reperfusion therapy (mainly pharmacological [80%]). Reasons for missing any means of reperfusion have been reported to be multifactorial; in particular, advanced age, comorbid conditions, hypertension, and stroke, as in our cohort of patients. Many strategies to increase the use of appropriate life-saving therapies have been recommended, which include community and physician awareness programs, among other things.19–22
Of particular focus, however, is the significant small proportion of 198 (10.8%) STEMI patients who received mechanical reperfusion as pPCI. Although the reasons for these findings were not very clear, the majority of patients were males, often overweight or obese. In addition, patients who received pPCI have had a significant history of myocardial infarction, dyslipidemia, diabetes mellitus, and previous PCI.
Prehospital delays may account for up to 75% of time to treatment delays.23 The majority of our patients arrived at hospital within 12 hours from the onset of chest pain. The mean and median delay were 4.4 hours and 2.1 hours, respectively; only 37% of them presented within 2 hours of onset of ischemic symptoms, as similar studies have reported.24–27
Although it is class 1 recommendation for patients with symptoms suggestive of a possible STEMI to seek medical attention promptly by activating the emergency response system, only 22.7% of our pPCI cohort patients used ambulance. Most patients either drove themselves or had a friend or family member drive them to hospital. The underuse of emergency services was also reported in well-established health care system.28 It has been shown that direct ambulance transport of STEMI patients to the Cath-Lab can significantly reduce D2B time and subsequently improve the delivery of pPCI and clinical outcomes.2,29 Such benefits persist regardless of time from the onset of chest pain and baseline risk of mortality.2,12
In our study cohort, we found that more patients with timely pPCI were transported by ambulance. Nonetheless, patients with STEMI frequently present during off hours (6.00 pm–8.00 am and weekends), and many of our health care facilities were challenged to maintain the availability of pPCI around the clock. This had no effect on patients receiving timely pPCI and hence no effect on outcome. Other studies reported similar findings of pPCI during off hours, partly.30,31
We have observed that patients who received timely pPCI were mainly among the age group 40 to 59 years. Comparing the countries, the highest proportion of timely pPCI was achieved in Bahrain (77%), perhaps due to the single-center nature of pPCI program in Bahrain. Such information may be useful for the effective education of particular patient populations and to identify cultural, language, political, and/or financial barriers that may exist to access and/or use care.
Consistent with recent recommendations, there were more use of higher loading dose of 600 mg clopidogrel in all pPCI patients but more significantly in those who received timely pPCI, as this also was shown to contribute to a better outcome.32
Regarding in-hospital clinical outcomes, we have noticed that unadjusted cardiogenic shock and IABP use were significantly lower in timely pPCI. However, after adjusting for all patients’ covariates, the differences were attenuated and remained weakly significant. There were no significant differences in other morbidity and mortality components between the groups perhaps due to the small sample size and hospital variability across the participating countries.
Taken all together, the findings highlighted that the majority of hospitals in the Arabian Gulf countries do not meet the required international guidelines on the management of pPCI. Accomplishing a high performance level is an organizational challenge. Recent regional efforts are drawing attention to the importance of D2B time as a key indicator of quality of care for patients with STEMI treated with pPCI. Delays in D2B time have been consistently associated with poorer outcomes in many studies. More importantly, it provides an open, vibrant community for hospitals to share their findings to save lives by reducing the D2B times in hospitals performing pPCI. Thus, a coordinated effort among clinicians, administrators, other health care professionals, emergency units, across all hospitals (within country), may provide a better diagnosis and treatment approaches for STEMI patients. The provision of pPCI Cath-Lab program, where absent, and intensive training for Cardiac Intensive Care Unit (CICU) physicians, nurses, radiology technicians, and other paramedical staff should be considered as priority to effective reduction in D2B time across the 6 adjacent Gulf countries. Also, improved emergency services and mass patient education programs may improve the use of ambulance services. A particular focus should be given to improving regional awareness in facilitating the adoption of evidence-based practices.
Limitations
Our study has several limitations. First, as with most other registries, the study results may not be representative of clinical practice in all hospitals in the region. However, the wide geographic distribution of several hospitals from different health care sectors in our study provides a reasonable overall representation of pPCI care. Second, there is an inherent selection bias because of the observational nature of the study design and the possibility of missing unmeasured important co-variables. Third, the sample size was small in subgroups. Nevertheless, the ongoing Gulf RACE 3 may provide-up-to-date data about emergency medical services for acute STEMI patients in the Gulf.
In summary, our data shows that only a small number of patients with STEMI were treated with pPCI, partly due to the lack of pPCI Cath-Lab program and an ineffective ambulance services use. The D2B time (timely PCI) is suboptimal across almost all participating countries. If patients were treated within an appropriate reperfusion strategy according to their clinical risk, arrival time may have no influence on mortality. There is a pressing need for coordinated efforts among the Gulf countries to achieve improved prehospital and in-hospital patient care to meet international guidelines for pPCI treatment among patients with STEMI.
Acknowledgments and funding
Gulf RACE is a Gulf Heart Association (GHA) project and was financially supported by the GHA, Sanofi Aventis, and the College of Medicine Research Center at King Khalid University Hospital, King Saud University, Riyadh, Saudi Arabia. The sponsors had no role in the study design, data collection, data analysis, writing of the report, or submission of the manuscript.
Footnotes
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the research, authorship, or publication of this article.
REFERENCES
- 1.Wood FO1, Leonowicz NA, Vanhecke TE, et al. Mortality in patients with ST-segment elevation myocardial infarction who do not undergo reperfusion. Am J Cardiol. 2012;110(4):509–14. doi: 10.1016/j.amjcard.2012.04.019. [DOI] [PubMed] [Google Scholar]
- 2.McNamara RL, Wang Y, Herrin J, et al. NRMI Investigators. Effect of door-to-balloon time on mortality in patients with ST-segment elevation myocardial infarction. J Am CollCardiol. 2006;47(11):2180–6. doi: 10.1016/j.jacc.2005.12.072. [DOI] [PubMed] [Google Scholar]
- 3.Steg PG, James SK, Gersh BJ. ESC STEMI guidelines and reperfusion therapy: Evidencebased recommendations, ensuring optimal patient management. Heart. 2013;99(16):1156–7. doi: 10.1136/heartjnl-2013-304498. [DOI] [PubMed] [Google Scholar]
- 4.Fox KA1, Goodman SG, Klein W, et al. Management of acute coronary syndromes. Variations in practice and outcome; findings from the Global Registry of Acute Coronary Events (GRACE) Eur Heart J. 2002;23(15):1177–89. doi: 10.1053/euhj.2001.3081. [DOI] [PubMed] [Google Scholar]
- 5.Wailoo AJ, Goodacre S, Sampson F, et al. Primary angioplasty versus thrombolysis for acute ST-elevation myocardial infarction: an economic analysis of the National Infarct Angioplasty Project. Heart. 2010;96(9):668–72. doi: 10.1136/hrt.2009.167130. [DOI] [PubMed] [Google Scholar]
- 6.Keeley EC, Boura JA, Grines CL. Comparison of primary and facilitated percutaneous coronary interventions for ST-elevation myocardial infarction: quantitative review of randomised trials. Lancet. 2006;367(9510):579–88. doi: 10.1016/S0140-6736(06)68148-8. [DOI] [PubMed] [Google Scholar]
- 7.Dryja T1, Kornacewicz-Jach Z, Goracy J, et al. Treatment of acute ST-segment elevation myocardial infarction in West Pomerania province of Poland. Comparison between primary coronary intervention and thrombolytic therapy. Kardiol Pol. 2006;64(6):591. [PubMed] [Google Scholar]
- 8.Brodie BR, Hansen C, Stuckey TD, et al. Doorto-balloon time with primary percutaneous coronary intervention for acute myocardial infarction impacts late cardiac mortality in high-risk patients and patients presenting early after the onset of symptoms. J Am Coll Cardiol. 2006;47(2):289–95. doi: 10.1016/j.jacc.2005.08.065. [DOI] [PubMed] [Google Scholar]
- 9.Cannon CP, Gibson CM, Lambrew CT, et al. Relationship of symptom-onset-to-balloon time an door-to-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA. 2000;283(22):2941–7. doi: 10.1001/jama.283.22.2941. [DOI] [PubMed] [Google Scholar]
- 10.Kumbhani DJ1, Cannon CP, Fonarow GC, et al. Get With the Guidelines Steering Committee and Investigators. Association of hospital primary angioplasty volume in ST-segment elevation myocardial infarction with quality and outcomes. JAMA. 2009;302(20):2207–13. doi: 10.1001/jama.2009.1715. [DOI] [PubMed] [Google Scholar]
- 11.Estevez-Loureiro R, Lopez-Sainz A, Perez de Prado A, et al. Timely reperfusion for STsegment elevation myocardial infarction: Effect of direct transfer to primary angioplasty on time delays and clinical outcomes. World J Cardiol. 2014;6(6):424–33. doi: 10.4330/wjc.v6.i6.424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Terkelsen CJ. Time to treatment-door-to-balloon time is not everything. Herz. 2014 doi: 10.1007/s00059-014-4125-y. Abstract. [DOI] [PubMed] [Google Scholar]
- 13.Bradley EH1, Nallamothu BK, Herrin J, et al. National efforts to improve door-to-balloon time results from the Door-to-Balloon Alliance. J Am Coll Cardiol. 2009;54(25):2423–9. doi: 10.1016/j.jacc.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 14.Lassen JF1, Botker HE, Terkelsen CJ. Timely and optimal treatment of patients with STEMI. Nat Rev Cardiol. 2013;10(1):41–8. doi: 10.1038/nrcardio.2012.156. [DOI] [PubMed] [Google Scholar]
- 15.Rasmussen MB1, Frost L, Stengaard C, et al. Diagnostic performance and system delay using telemedicine for prehospital diagnosis in triaging and treatment of STEMI. Heart. 2014;100(9):711–5. doi: 10.1136/heartjnl-2013-304576. [DOI] [PubMed] [Google Scholar]
- 16.ThorstedSorensen J1, Steengaard C, Holmvang L, et al. Primary percutaneous coronary intervention as a national Danish reperfusion strategy of ST-elevation myocardial infarction] Ugeskr Laeger. 2013;175(4):181–5. [PubMed] [Google Scholar]
- 17.Al-Mallah MH1, Alsheikh-Ali AA, Almahmeed W, et al. Missed opportunities in the management of ST-segment elevation myocardial infarction in the Arab Middle East: patient and physician impediments. Clin Cardiol. 2010;33(9):565–71. doi: 10.1002/clc.20802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alhabib KF, Sulaiman K, Al-Motarreb A, et al. Gulf RACE-2 investigators. Baseline characteristics, management practices, and long-term outcomes of Middle Eastern patients in the Second Gulf Registry of Acute Coronary Events (Gulf RACE-2) Ann Saudi Med. 2012;32(1):9–18. doi: 10.5144/0256-4947.2012.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Steg PG, James SK, Gersh BJ. 2012 ESC STEMI guidelines and reperfusion therapy: Evidence-based recommendations, ensuring optimal patient management. Heart. 2013;99(16):1156–7. doi: 10.1136/heartjnl-2013-304498. [DOI] [PubMed] [Google Scholar]
- 20.Fox KA1, Goodman SG, Klein W, et al. Management of acute coronary syndromes. Variations in practice and outcome; findings from the Global Registry of Acute Coronary Events (GRACE) Eur Heart J. 2002;23(15):1177–89. doi: 10.1053/euhj.2001.3081. [DOI] [PubMed] [Google Scholar]
- 21.Wood FO1, Leonowicz NA, Vanhecke TE, et al. Mortality in patients with ST-segment elevation myocardial infarction who do not undergo reperfusion. Am J Cardiol. 2012;110(4):509–14. doi: 10.1016/j.amjcard.2012.04.019. [DOI] [PubMed] [Google Scholar]
- 22.Al-Mallah MH1, Alsheikh-Ali AA, Almahmeed W, et al. Missed opportunities in the management of ST-segment elevation myocardial infarction in the Arab Middle East: patient and physician impediments. Clin Cardiol. 2010;33(9):565–71. doi: 10.1002/clc.20802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weaver WD. Time to thrombolytic treatment: factors affecting delay and their influence on outcome. J Am Coll Cardiol. 1995;25(7 Suppl):3S–9S. doi: 10.1016/0735-1097(95)00108-g. [DOI] [PubMed] [Google Scholar]
- 24.Welsh RC, Ornato J, Armstrong PW. Prehospital management of acute ST-elevation myocardial infarction: a time for reappraisal in North America. Am Heart J. 2003;145(1):1–8. doi: 10.1067/mhj.2003.47. [DOI] [PubMed] [Google Scholar]
- 25.Goff DC, Jr, Feldman HA, McGovern PG, et al. Prehospital delay in patients hospitalized with heart attack symptoms in the United States: the REACT trial. Rapid Early Action for Coronary Treatment (REACT) Study Group. Am Heart J. 1999;138(6 Pt 1):1046–57. doi: 10.1016/s0002-8703(99)70069-4. [DOI] [PubMed] [Google Scholar]
- 26.Goldberg RJ, Steg PG, Sadiq I, et al. Extent of, and factors associated with, delay to hospital presentation in patients with acute coronary disease (the GRACE registry) Am J Cardiol. 2002;89(7):791–6. doi: 10.1016/s0002-9149(02)02186-0. [DOI] [PubMed] [Google Scholar]
- 27.Goldberg RJ, Osganian S, Zapka J, et al. Prehospital delay in individuals with acute coronary disease: concordance of medical records and follow-up phone interviews. Cardiology. 2002;97(3):159–65. doi: 10.1159/000063333. [DOI] [PubMed] [Google Scholar]
- 28.Canto JG, Zalenski RJ, Ornato JP, et al. Use of emergency medical services in acute myocardial infarction and subsequent quality of care: observations from the National Registry of Myocardial Infarction. Circulation. 2002;106(24):3018–23. doi: 10.1161/01.cir.0000041246.20352.03. [DOI] [PubMed] [Google Scholar]
- 29.Qiu JP1, Zhang Q, Lu JD, et al. Direct ambulance transport to catheterization laboratory reduces door-to-balloon time in patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention: the DIRECT-STEMI study. Chin Med J Engl. 2011;124(6):805–10. [PubMed] [Google Scholar]
- 30.de Boer SP1, Oemrawsingh RM, Lenzen MJ, et al. Primary PCI during off-hours is not related to increased mortality. EurHeart J Acute Cardiovasc Care. 2012;1(1):33–9. doi: 10.1177/2048872612441581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kim SS1, Jeong MH2, Rhew SH1, et al. Korea Acute Myocardial Infarction Registry Investigators. Impact of patients’ arrival time on the care and in-hospital mortality in patients with non-ST-elevation myocardial infarction. Am J Cardiol. 2014;113(2):262–9. doi: 10.1016/j.amjcard.2013.09.013. [DOI] [PubMed] [Google Scholar]
- 32.Beigel R, Fefer P, Rosenberg N, et al. Antiplatelet effect of thienopyridine (clopidogrel or prasugrel) pretreatment in patients undergoing primary percutaneous intervention for ST elevation myocardial infarction. Am J Cardiol. 2013;112(10):1551–6. doi: 10.1016/j.amjcard.2013.07.010. [DOI] [PubMed] [Google Scholar]