Abstract
BACKGROUND AND OBJECTIVES
Patients with coronary artery disease (CAD) are at high risk of recurrent adverse cardiac events. Such risk can be diminished through a guideline-recommend optimal medical therapy (OMT), defined as adherence to appropriate antiplatelet therapy, lipid-lowering agents, beta-blockers and angiotensin-converting enzyme inhibitors, blood pressure <140/90 mm Hg (<130/80 mm Hg in diabetics and renal disease patients), low-density lipoprotein (LDL) <2 mmol/L, smoking cessation and aerobic physical activity, and hemoglobin (Hb) A1c <7%. Unfortunately, preliminary data suggest a wide gap between recommended and actual practices. The study aims to estimate the rate of achieving of OMT in CAD patients in Qassim Province.
DESIGN AND SETTINGS
This observational study enrolled 207 consecutive CAD patients seen in cardiology clinic in Prince Sultan Cardiac Center in Qassim between January 2012 and May 2012.
METHODS
Eligible participants were over the age of 18, with CAD documented by either noninvasive testing or by coronary angiogram. We collected the demographic, medications, laboratory, and clinical data through in-person interviews, medical records, and an electronic patient database.
RESULTS
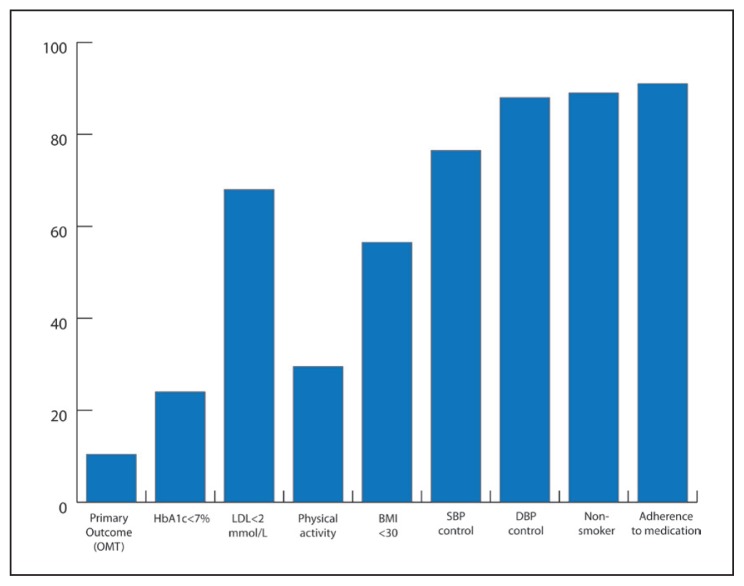
OMT was achieved in only 10.4% of CAD patients. The rate of achievement of target systolic blood pressure was 76.5%, target diastolic blood pressure 88%, target LDL 68%, adherence to medications 91%. Diabetes was common (64% of all patients), and only 24% of these patients achieved the target HbA1c.
CONCLUSION
The poor achievement of optimal medical therapy in CAD patients contributes to preventable mortality, morbidity, and health care costs. The observed shortcomings warrant investment in strategies to achieve OMT in these high-risk patients.
Coronary artery disease (CAD) creates an enormous worldwide burden, including substantial problems in personal, societal, and economic terms. Although CAD occurs in both developing and industrialized countries, it is particularly problematic in rapidly developing middle-income nations such as Saudi Arabia due to rapid declines in physical activity levels and increasing availability of inexpensive, high-calorie foods. The likelihood of recurrent cardiac events mandates aggressive risk factor control in this high-risk population through optimal medical therapy (OMT). As defined by The American Heart Association and American College of Cardiology,1 OMT includes adequate control of cardiovascular risk factors and adequate adherence to proven, recommended pharmacotherapy (Table 1).
Table 1.
Components of Optimal Medical Therapy (OMT).
|
Such medical therapy produces better long-term outcomes and is strongly recommended by all cardiovascular societies around the globe. OMT reduces the occurrence of myocardial infarction, revascularization, hospitalizations and stroke, and also reduces mortality.2 Unfortunately, research in the US and at the global level suggest that OMT is achieved in less than 50% of patients with CAD.3,4 Preliminary data from Saudi Arabia suggests an even wider gap between achieved and recommended practices.
This study examined the patterns of suboptimal heart disease care in Qassim. It elucidated risk factor profiles among CAD patients in the Qassim region and measured the extent to which OMT was achieved. We hypothesized that OMT will be achieved in less than half of CAD patients and that patients with diabetes and/or obesity will be less likely to achieve OMT.
METHODS
We enrolled a total of 207 consecutive patients attending the outpatient clinic at Prince Sultan Cardiac Center in Qassim (PSCCQ), Saudi Arabia, between January 2012 and May 2012. Eligible participants were over the age of 18, with documented CAD (coronary catheterization, coronary computed tomography, or nuclear stress test). We excluded patients who refused or were unable to sign the consent form.
We collected the demographic data through in-person interviews, and clinical data through the medical record, electronic database, and the PSCCQ cath laboratory database. Adult cardiologists performed patients’ interviews. Blood chemistry results were obtained within 1 month of the clinic visit (26 patients, 13%) or at the time of clinic visit (181 patients, 87%).
To avoid potential errors in assessing what medications the patient was taking, we asked all the patients to bring their own medications to study appointments, rather than rely on the medical record or patient recall. Patient adherence to medications was assessed using the following 2 methods: (1) pill counts and (2) prescription claims. It has been suggested that the latter method is more accurate to assess adherence to medication.5 It was very difficult to define the benchmarking of adherence, but we opted to use the strictest definition, more than 95% of the doses of CAD medications.6
The primary outcome of this study is the rate of achievement of all components of OMT (blood pressure control; low-density lipoprotein [LDL] <2 mmol/L [100 mg/dL]; hemoglobin [Hb] A1c <7%; smoking cessation; physically active; adherence to all cardiac medications, namely aspirin, statin, beta-blocker, angiotensin-converting enzyme (ACE) inhibitor, and clopidogrel if indicated).
The secondary outcomes are the individual components of OMT.
Statistical analysis
This is a descriptive analysis to determine the underlying risk factors and adequacy of medical therapy among patients with CAD in Qassim province, Saudi Arabia. The descriptive analysis enabled the testing of the study’s Hypothesis 1 that posits that OMT was achieved in less than 50% of CAD patients. The study’s Hypothesis 2 suggests that diabetes and obesity were more common among those patients who fail to achieve OMT. Enrolment of 207 CAD patients provided adequate statistical power to reliably estimate the rate of OMT and to determine the statistical predictors of achieving OMT. The 95% confidence interval for estimating OMT that turns out to be 50% will be 43.8% to 56.2%. As an example of examining factors associated with greater or lesser likelihood of OMT, it was assumed that if patients with diabetes comprise 40% of the CAD patients, then a 20% absolute difference in OMT between diabetes (e.g., 30%, N=100) and no diabetes (e.g., 50%, N=100) would be detected at a statistical power of 88% at a 2-tailed P value of less than.05.
RESULTS
A total of 207 eligible patients with documented CAD over a period of 5 months were enrolled from outpatient clinic in PSCCQ. A total of 194 patients (94%) had documented CAD by coronary angiogram and 13 patient (6%) confirmed by non-invasive stress testing. The mean age was 60 (20) years and 28% were female. The majority of the patients underwent revascularization; 134 patients (65%) had percutaneous coronary intervention and 33 patients (16%) had coronary artery bypass graft surgery (CABG). Patients with diabetes were 132 (64%) in number, and only 30% were physically active (walking > 30 minutes/d). The baseline characteristics are shown in Table 2.
Table 2.
Baseline characteristics.
| Sex | |
| Male, % (n) | 72 (149) |
| Female, % (n) | 28 (58) |
| Age, mean (SD) | 60.0 (10.9) |
| Education | |
| Educated, % (n) | 13 (24) |
| Illiterate, % (n) | 87 (164) |
| Nationality | |
| Saudi, % (n) | 91 (188) |
| Non-Saudi, % (n) | 9 (18) |
| Current smoker, % (n) | 11 (22) |
| Diabetes, % (n) | 64 (132) |
| Hypertension, % (n) | 70 (144) |
| Dyslipidemia, % (n) | 95 (194) |
| Obesity (BMI > 30), % (n) | 44 (83) |
| Family history of premature CAD, % (n) | 7 (14) |
| History of ACS, % (n) | 50 (103) |
| History of PCI, % (n) | 65 (134) |
| History of CABG, % (n) | 16 (33) |
| Angina, % (n) | 19 (40) |
| LVEF, mean (SD) | 11.3 (48.0) |
| LVEF = <30%, % (n) | 9 (17) |
| Significant valvular lesion, % (n) | 6.3 (13.0) |
| PVD | 4 (8) |
| CVA | 7 (16) |
| CKD | 4 (9) |
| Heart rate, beats/min, mean (SD) | 74.3 (11.7) |
| SBP, mm Hg, mean (SD) | 125.3 (13.6) |
| DBP, mm Hg, mean (SD) | 74.7 (8.3) |
| BMI, mean (SD) | 29.6 (5.7) |
| Total cholesterol, mmol/L, mean (SD) | 4.18 (1.1) |
| LDL, mmol/L, mean (SD) | 1.89 (0.8) |
| HDL, mmol/L, mean (SD) | 1.0 (0.5) |
| Triglycerides, mmol/L, mean (SD) | 1.5 (0.7) |
| CrCL, mL/min, mean (SD) | 96.0 (41.1) |
Values are % (n=number) or mean (SD= standard deviation).
ACS: acute coronary syndrome; BMI: Body mass index; CABG: coronary artery bypass grafting; CAD: coronary artery disease; CKD: chronic kidney disease; CrCL=creatinine clearance; CVA: cerebrovascular accident; DBP: diastolic blood pressure; HDL: high-density lipoprotein; LDL: low-density lipoprotein; LVEF: left ventricular ejection fraction; PCI: percutaneous coronary intervention; PVD: peripheral vascular disease; SBP: systolic blood pressure.
The primary outcome (achievement of optimal medical therapy) was achieved in only 10.4% (Table 3). The target blood pressure was achieved in 76.5% and 88% for systolic and diastolic blood pressure, respectively. Approximately 68% achieved treatment targets for low-density lipoprotein <2 mmol/L. Among the 132 diabetic patients, only 24% achieved the target HbA1C less than 7% and only 2 patients achieved the primary outcomes.
Table 3.
Primary outcomes and secondary outcomes.
| Primary outcomes, % (n) | |
| Achievement of OMT | 10.4 (15.0) |
| Secondary outcomes, % (n) | |
| Primary outcomes with or without physical activities | 25.5 (37) |
| LDL | 68 (98) |
| HbA1c < 7% | 24 (12) |
| Physically active | 29.5 (61) |
| SBP control | 76.5 (153) |
| DBP control | 88 (182) |
| Non-smoker, or ex-smoker | 89.4 (185) |
| Adherence to ASA | 96.5 (197) |
| Adherence to Clopidogrel | 95 (118) |
| Adherence to beta-blocker | 94 (169) |
| Adherence to ACEI | 94 (167) |
| Adherence to lipid-lowering agents | 93 (176) |
| Adherence to cardiac medications | 91(188) |
There were a high rate of achieving the target for smoking cessation; 90% of patients were non-smoker or ex-smoker. The adherence to medications was excellent as shown in Figure 1, where the adherence to aspirin, clopidogrel, beta-blocker, ACEI/angiotensin receptor blocker (ARB), and statin showed 95%, 95.5%, 94.4%, 94.3%, and 94.3%, respectively. The adherence to all 5 cardiac medications was 91%.
Figure 1.
Adherence to cardiac medications.
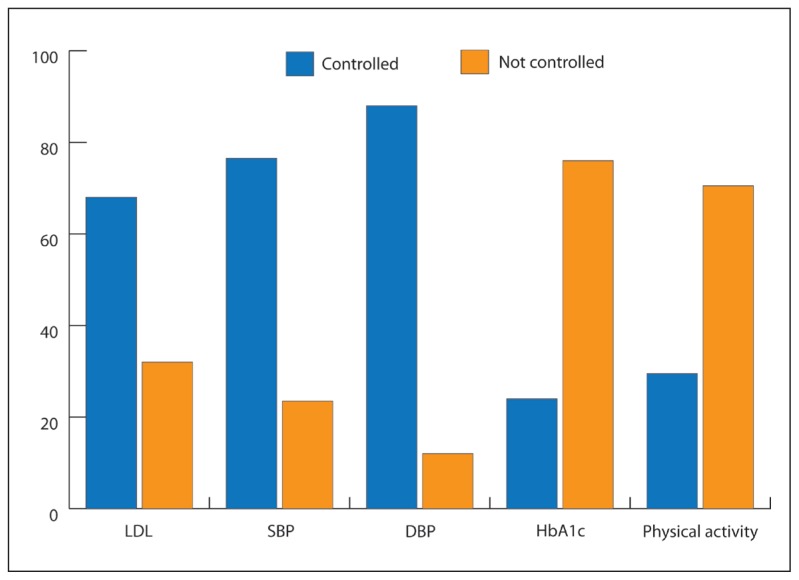
Among the OMT components, the worst were achievement of target HbA1c and physical activities as shown in Figure 2. When we exclude physical activities, the achievement of OMT was higher (25.5%). In addition, the achievement of OMT in diabetic patients was also higher (13.7%) when we exclude adherence to physical activities.
Figure 2.
Primary outcome and secondary outcome.
CAD risk factors and OMT achievement
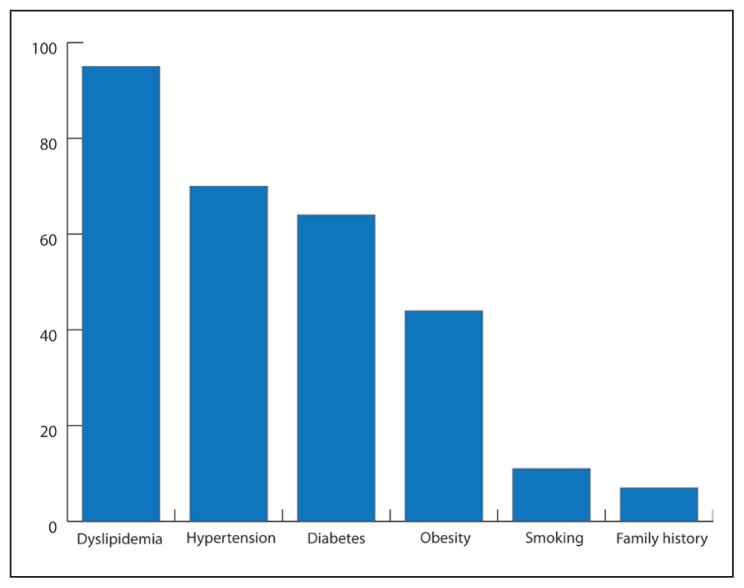
Among the risk factors for CAD patients, dyslipidemia and hypertension were most prevalent, which were present in 194 patients (95%) and 144 patients (70%), respectively (Figure 3). However, diabetes (132 patients [64%]) and physical inactivity (146 patients [70.5%]) were considered the main uncontrolled risk factors (Figure 4).
Figure 3.
Risk factors in coronary artery disease patients.
Figure 4.
Comparing controlled risk factors with non-controlled risk factors.
DISCUSSION
Despite having OMT recommended by all contemporary guidelines, it is hard to be achieved by most of real-life registries including our study. We found, among 207 screened CAD patients, only 10.4% of patients achieved OMT. This poor performance in medical therapy will make the extrapolation from different clinical trials more difficult.7,8 We have also found a different risk factor profile in our cohort as compared to the published studies in different countries. Two thirds of the CAD population in our study included patients with diabetes (64%). The prevalence of dyslipidemia is difficult to analyze because most patients think that they are dyslipidemic as they were on lipid-lowering agents. Lipid-lowering agent, namely statin therapy, is standard to all CAD patients regardless of their lipid profile.
Among the most important findings in our study were the increased prevalence of diabetes among CAD patients and high rate of suboptimal therapy (only 32 patients [24%] achieved the target HbA1c and only 2 patients [1.5%] achieved optimal medical therapy). Al-Nozha et al showed that the prevalence of diabetes increased from 19% to 24% from 1990s to 2000s, respectively.9–11 Similar poor control of diabetes was seen in other studies in Saudi Arabia.12 This poor control might be secondary to multiple reasons including (1) unhealthy life style, (2) little access to medical education, (3) limited access to diabetes specialists, (4) changing dietary habits to carbohydrate-rich diet, particularly dates (Qassim is a well-known area of specific brand of date),5,13 and (5) genetic predisposition to type 2 diabetes producing more resistant type of diabetes.
The LDL goal was achieved in 68% of patients. However, we noticed during data collection that only 13% of patients had the latest lipid profile. The majority of patients had no lipid profile in their medical files for more than 1 year. This poor medical assessment of CAD patient mostly related to physicians and not patients because no order was found for reviewing medical files.
The adherence to medications was achieved in 91% of patient as compared to <50% in multiple other studies.3,4 Our excellent performance on adherence to medication was most likely related to the traditions in Gulf states, as family bonds are very strong and the illness of one family member involves the rest of the family. CAD generally affects an old person, who might be a father or a mother, and children seek reward from the Almighty by attending to their parents and serving them well. So, one of the family members is responsible to be with the patient and ensure timely medication.
The overall performance to achieve OMT is poor, particularly among patients with diabetes and those who are physically inactive. The prevalence of physical inactivity was high in Saudi Arabia.14,15 The potential reasons of physical inactivity given by patients are varied, including (1) high prevalence of osteoarthritis, (2) hot weather, and (3) unavailability of walking spaces nearby; however, the majority did not give a specific reason. As a policy implication, we suggest that greater attention be paid to increasing patient physical activity level. Both CAD patients and their physician may need to be reminded of the important benefits of physical activity. In addition, providing better access to physical activity opportunities should be undertaken. We have noticed that building such facilities outside the housing areas might not be beneficial because most of the patients prefer to exercise near home.
The observed shortfalls in OMT may be due to a number of factors, including (1) inadequate knowledge of clinical goals on the part of both patients and physicians, (2) lack of close follow-up, (3) an inadequate health care system that emphasizes technologically advanced acute care services, and (4) human resource limitations. Our findings suggest multiple potential reasons of our shortfalls in OMT and how we can improve the knowledge on the part of both patients and physicians and how we can optimize the health care system in all aspects. These issues need to be explored in future research applying similar strategies to other epidemic non-communicable diseases.16–19 Among these strategies is the casemanagement strategy that acts as a focused cardiac rehabilitation and education strategy.20–26 The cost of such intervention may be more cost effective in reducing adverse cardiac event in such high-risk patients.27,28
The limitations of our study are as follows: (1) a small cross-sectional sample in 1 cardiac center; (2) one-third of the patients resided in a different province called Hail, 300 km away, which made a close follow-up almost impossible; and (3) lipid profiles of most of the patients from Hail were not obtained and were omitted from the denominator while calculating the achievement of LDL target. Interestingly, we found that the medical files of 87% of patients did not have the lipid profiles, and we suggested them to get their lipid profile done at the time of their first encounter.
We recommend careful monitoring of lipid profile and HbA1c every 6 months. However, lipid profiles and HbA1c should be assessed after 6 weeks of any change in medical therapy. Adequate medical education and adherence to medical therapies are the primary determinants of treatment success.
In conclusion, the poor achievement of OMT in CAD patients (10.4%) contributes to preventable mortality, morbidity, and health care costs. The high prevalence of diabetes in CAD patients with poor glycemic control is an example among the observed shortcomings that warrant investment in strategies to achieve OMT in these high-risk patients.
Acknowledgments
The study is sponsored by Qassim University College of Medicine research grant. Thanks to Dr. Mohammed Abdulzaher who helped us in auditing the data collection and to the nursing staff in the outpatient department of Prince Sultan Cardiac Center, Qassim University, Saudi Arabia.
REFERENCES
- 1.Smith SC, Allen J, Blair SN. AHA/ACC Guidelines for Secondary Prevention for Patients with Coronary and Other Atherosclerotic Vascular Disease: 2006 Update. Circulation. 2006;113:2363–72. doi: 10.1161/CIRCULATIONAHA.106.174516. [DOI] [PubMed] [Google Scholar]
- 2.Bramlage P, Messer C, Bitterlich N, et al. The effect of optimal medical therapy on 1-year mortality after acute myocardial infarction. Heart. 2010;96:604–9. doi: 10.1136/hrt.2009.188607. [DOI] [PubMed] [Google Scholar]
- 3.William B, Borden WB, Redberg RF, et al. Patterns and Intensity of Medical Therapy in Patients Undergoing Percutaneous Coronary Intervention. JAMA. 2011;305(18):1882–9. doi: 10.1001/jama.2011.601. [DOI] [PubMed] [Google Scholar]
- 4.Bhatt DL, Steg PG, Ohman EM, et al. International Prevalence, recognition, and treatment of cardiovascular risk factors in outpatients with atherothrombosis. JAMA. 2006;295(2):180–118. doi: 10.1001/jama.295.2.180. [AUTHOR: Please check the page range, which does not seem to be correct] [DOI] [PubMed] [Google Scholar]
- 5.Fairman K, Matheral B. Evaluating Medication Adherence: Which Measure Is Right for Your Program. J Managed Care Pharm. 2000:499–504. [Google Scholar]
- 6.Osterberg L, Blaschke Adherence to medication. N Engl J Med. 2005;353:487–97. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 7.Boden WE, O’Rourke RA, Teo KK. Optimal Medical Therapy with or without PCI for stable Coronary disease. N Eng J Med. 2007;356(15):1503–16. doi: 10.1056/NEJMoa070829. [DOI] [PubMed] [Google Scholar]
- 8.Mason DJ, Boden WE, Weintraub WS, Calfas KJ, O’Rourke RA. Is Optimal Medical Therapy as Used in the COURAGE Trial Feasible for Widespread Use? Curr Treat Options Cadiovasc Med. 2011;13(1):16–25. doi: 10.1007/s11936-010-0104-7. [DOI] [PubMed] [Google Scholar]
- 9.Alwan A. Cardiovascular diseases in the Eastern Mediterranean Region. World health statistics quarterly. 1993;46(2):97–100. [PubMed] [Google Scholar]
- 10.Al-Nozha MM, Osman AK. Risk factors for Coronary artery disease in different regions of Saudi Arabia. East Meditrr Health J. 2000;6(2):465–74. [PubMed] [Google Scholar]
- 11.Al-Nozha MM, Arafah MR, Al-Mazrou YY, et al. Coronary artery disease in Saudi Arabia. Saudi med J. 2004;25(9):1165–71. [PubMed] [Google Scholar]
- 12.Al-Hussein FA. Diabetes control in a primary care setting: a retrospective study of 651 patients. Ann Saudi Med. 2008;28(4):267–71. doi: 10.5144/0256-4947.2008.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Al-Kanhal MA, Osman Ali K. Changing food consumption pattern and health in Saudi Arabia. Paper presented at the WHO symposium on “The epidemiologic transition/transaction and health in developing countries”; College of Medicine, K. S. U., Riyadh. Nov. 1994; pp. 27–29. [Google Scholar]
- 14.Al-Nozha MM, Al-Hazzaa HM, Arafah MR, et al. Prevalence of physical activity and inactivity among Saudis aged 30–70 years. A population-based cross-sectional study. Saudi Med J. 2007;28(4):559–68. [PubMed] [Google Scholar]
- 15.Al-Hazzaa HM. Prevalence of physical inactivity in Saudi Arabia: a brief review. East Mediterr Health J. 2004;10(4–5):663–70. [PubMed] [Google Scholar]
- 16.Aubert RE, Herman WH, Waters J, et al. Nurse case management to improve glycemic control in diabetic patients in a health maintenance organization. A randomized, controlled trial. Ann Intern Med. 1998;129(8):605–12. doi: 10.7326/0003-4819-129-8-199810150-00004. [DOI] [PubMed] [Google Scholar]
- 17.Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the Incidence of type 2 diabetes with lifestyle intervention or metformin! N Eng J Med. 2002;346(6):393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goldberg JH, Kiernan M. Innovative techniques to address retention in a behavioral weight-loss trial. Health Educ Res Aug. 2005;20(4):439. doi: 10.1093/her/cyg139. [DOI] [PubMed] [Google Scholar]
- 19.Janson SL, Alioto ME, Boushey HA Asthma Clinical Trials Network. Attrition and retention of ethnically diverse subjects in a multicenter randomized controlled research trial. Control Clin Trials Dec. 2001;22(6 Suppl):236S–43S. doi: 10.1016/s0197-2456(01)00171-4. [DOI] [PubMed] [Google Scholar]
- 20.DeBusk RF, Miller NH, Superko HR, et al. A case- management system for coronary risk factor modification after acute myocardial infarction. Ann Intern Med. 1994;120:721–9. doi: 10.7326/0003-4819-120-9-199405010-00001. [DOI] [PubMed] [Google Scholar]
- 21.Stafford RS, Berra K. Critical Factors in Case Management: Practical Lessons from a Cardiac Case Management Program. Disease Management. 2007;10:197–207. doi: 10.1089/dis.2007.103624. [DOI] [PubMed] [Google Scholar]
- 22.DeBusk RF. MULTIFIT: a new approach to risk factor modification. Cardiol Clin. 1996;14(1):143–57. doi: 10.1016/s0733-8651(05)70267-8. [DOI] [PubMed] [Google Scholar]
- 23.Fonarow GC, Gawlinski A, Moughrabi S, Tillisch JH. Improved treatment of coronary heart disease by implementation of a Cardiac Hospitalization Atherosclerosis Management Program (CHAMP) Am J Cardiol. 2001;87(7):819–22. doi: 10.1016/s0002-9149(00)01519-8. [DOI] [PubMed] [Google Scholar]
- 24.Becker DM, Yanek LR, Johnson WRJ, et al. Impact of a community-based multiple risk factor intervention on cardiovascular risk in black families with a history of premature coronary disease. Circulation. 2005;111(10):1298–1304. doi: 10.1161/01.CIR.0000157734.97351.B2. [DOI] [PubMed] [Google Scholar]
- 25.Ma J, Lee K, Berra K, Stafford RS. Implementation of case management to reduce cardiovascular disease risk in the Stanford and San Mateo Heart to Heart randomized controlled trial: study protocol and baseline characteristics. Implementation Science. 2006;1:21. doi: 10.1186/1748-5908-1-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stafford RS, Berra K. Critical Factors in Case Management: Practical Lessons from a Cardiac Case Management Program. Disease Management. 2007;10:197–207. doi: 10.1089/dis.2007.103624. [DOI] [PubMed] [Google Scholar]
- 27.Weintraub WS, Boden WE, Zhang Z, et al. Cost-Effectiveness of Percutaneous Coronary Intervention in optimally treated stable Coronary patients. Circulation: Cardiovascular Quality and outcomes. 2008;1:12–20. doi: 10.1161/CIRCOUTCOMES.108.798462. [DOI] [PubMed] [Google Scholar]
- 28.Haskell WL, Alderman EL, Fair JM, et al. Effects of intensive multiple risk factor reduction on coronary atherosclerosis and clinical cardiac events in men and women with coronary artery disease. The Stanford Coronary Risk Intervention Project (SCRIP) Circulation. 1994;89(3):975–90. doi: 10.1161/01.cir.89.3.975. [DOI] [PubMed] [Google Scholar]