Abstract
Bleeding per rectum is an uncommon presentation in pediatric patients. Heterotopic gastric mucosa in the rectum is a rare cause of rectal bleeding. Here, we report a 3-year-old child with a bleeding rectal ulcer that was initially diagnosed and managed as a solitary rectal ulcer syndrome. After 1 month, the patient persisted to have intermittent rectal bleed and severe anal pain. Repeat colonoscopy showed the worsening of the rectal ulcer in size. Pediatric surgeon excised the ulcer, and histopathological examination revealed a gastric fundic-type mucosa consistent with the diagnosis of gastric heterotopia of the rectum. Over the following 18 months, our patient had experienced no rectal bleeding and remained entirely asymptomatic. In conclusion, heterotopic gastric mucosa of the rectum should be considered in the differential diagnosis of a bleeding rectal ulcer.
Bleeding per rectum is an uncommon symptom in pediatric patients. Heterotopic gastric mucosa in the rectum is a rare cause of rectal bleeding. Heterotopic gastric mucosa has been identified throughout the gastrointestinal tract including the nasopharynx, tongue, esophagus, small intestine, gallbladder, biliary tract, colon, and rectum.1 Typically, ectopic gastric mucosa is asymptomatic. The rarity of symptomatic rectal gastric mucosa, decreased awareness of pediatricians and gastroenterologists about the possibility of gastric heterotopia of rectum in the differential diagnosis of rectal bleeding, and non-specificity of clinical presentation lead to significant delay in diagnosis and late initiation of appropriate management. Here, we report a 3-year-old child with bleeding rectal ulcer due to rectal gastric heterotopia that was misdiagnosed as solitary rectal ulcer syndrome, with extensive review of pediatric medical published reports. We aim to increase the awareness of pediatricians and gastroenterologists about the possibility of heterotopic gastric mucosa in the rectum as a cause of rectal bleeding to make early diagnosis and initiate early management.
CASE
A 3-year-old male presented to the emergency department at King Fahad Medical City with a history of episodic rectal bleeding and anal pain for 8 months. The bleeding was described as bright red blood streaked on the stool and blood in the toilet bowl. He had occasional abdominal pain not associated with defecation. The anal pain was not related to episodes of hematochezia. There was no family history of any bleeding disorders, recurrent epistaxis, gastrointestinal polyps, or cancer. He had been investigated in 2 other local hospitals due to same complaint, and 2 colonoscopies had been done during the illness period but were reported to be normal. On physical examination, the height was 93 cm (75th centile) and the weight was 13 kg (75th centile); the abdomen was soft and lax without organomegaly.
On anal examination, he had no anal fissures or skin tags. Other systemic examination was unremarkable. Laboratory investigations showed normal complete blood count and coagulation profile. Stool examination for ova and parasites and culture were negative.
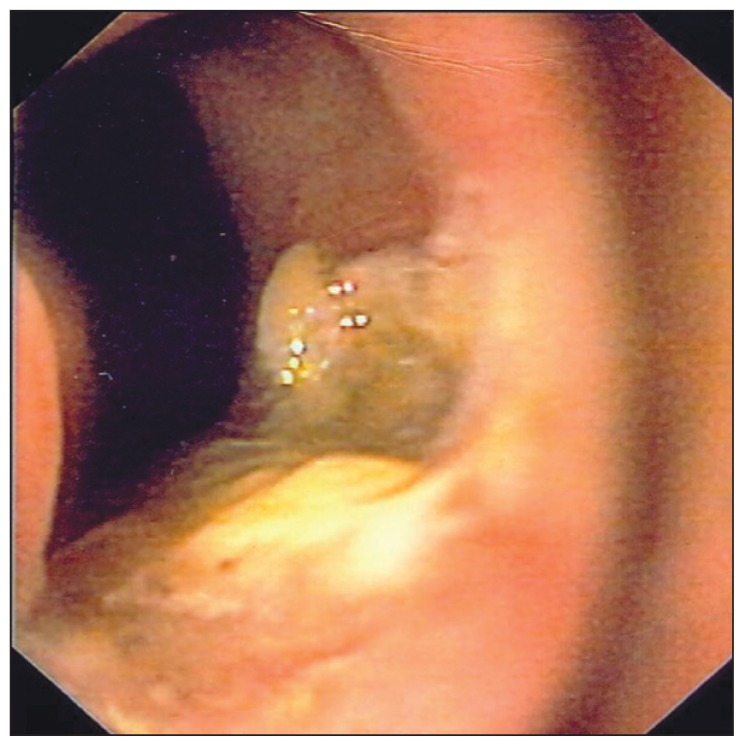
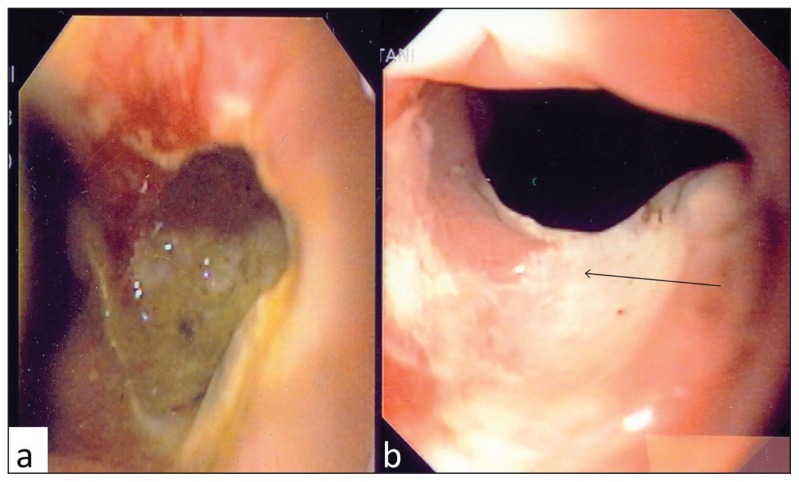
On colonoscopy, an ulcerative lesion of 2×2 cm was observed, which was 0.5 centimeter proximal to the dentate line of anal canal (Figure 1). Biopsies obtained from mucosa around the ulcer showed no specific histopathological changes. The child was managed as solitary rectal ulcer with rectal sucralfate and cortifoam enema. After 1 month, the patient persisted to have intermittent rectal bleed and severe anal pain. Repeated sigmoidoscopy showed worsening of the ulcer in size and depth (Figure 2a). Worsening of the ulcer despite traditional therapy of solitary rectal ulcer raised suspicion of different pathology and led to further diagnostic workup to exclude infectious and malignant etiologies. Biopsies from the edge of the ulcer and the rectal mucosa around the ulcer were subjected to Zeel-Nelson stain, mycobacterium tuberculosis DNA polymerase chain reaction test, lymphoma stain, and fungal stain, but all turned out to be negative. Magnetic resonance imaging of pelvis and abdomen was normal. Pediatric surgeon was consulted who performed cauterization of the ulcer. On follow up 1 month later, the child was asymptomatic and sigmoidoscopy revealed a healed ulcer (Figure 2b).
Figure 1.
An ulcerative lesion of 2×2 cm observed on colonoscopy.
Figure 2.
Sigmoidoscopy (a) showing worsening of the ulcer in size and (b) revealing a healed ulcer.
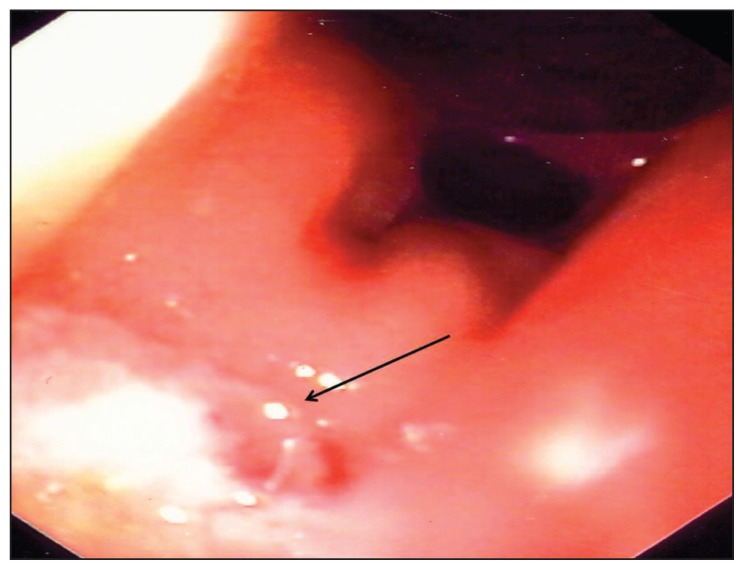
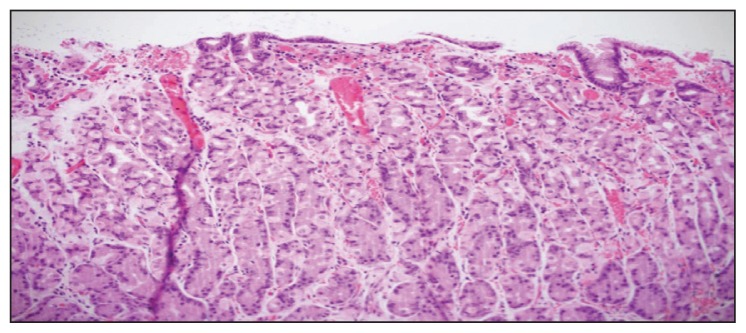
One year later, the patient presented with the same complaint of rectal bleeding and anal pain. Sigmoidoscopy showed recurrence of a small ulcer 1 × 1 cm at a different site than the first ulcer, located just above the dentate line of the anal canal (Figure 3). Pediatric surgeon excised the ulcer, and histopathological examination revealed a gastric fundic-type mucosa (Figure 4) consistent with the diagnosis of gastric heterotopia of the rectum. The staining of the excised specimen with Geimsa stain was negative for Helicobacter pylori organism. Meckel’s scan did not show any residual gastric mucosa in the rectum or in other parts of gastrointestinal tract. Over the following 18 months, our patient did not experience any recurrence of rectal bleeding and he remained entirely asymptomatic.
Figure 3.
Sigmoidoscopy showing recurrence of a small ulcer 1×1 cm at a different site than the first ulcer.
Figure 4.
Histopathological examination revealing a gastric fundic-type mucosa.
DISCUSSION
The most accepted hypothesis for heterotopia of gastric mucosa is an error of differentiation.1 Pluripotent endoderm stem cells have the capability of differentiating into all types of gastrointestinal epithelium. This theory is supported by immunocytochemical studies demonstrating that the metabolic and functional activity of gastric heterotopic mucosa, regarding the production of acid and mucin, is identical to that of the normal stomach.2
We searched the English-language published reports in Pubmed, Embase, and Medline (1966–2012) for pediatric cases of ectopic gastric mucosa using the following search words: gastric heterotopia, rectal gastric mucosa, rectal bleeding, and child. To the best of our knowledge, 24 pediatric cases of gastric heterotopia in the rectum have been reported so far. The review of published reports (Table 1) revealed that males were more commonly affected (M:F, 19:5), with an average age at presentation of about 7 years (range, 6 months to 17 years). The most common presentation of rectal gastric heterotopia was painless rectal bleeding (95.6%); other less common presentations included perianal ulceration (4.3%), anal pain (17%), abdominal pain (8.6%), and diarrhea (8%). Symptoms were present from 1 day to 12 years prior to diagnosis. Heterotopic gastric tissue has most commonly been identified in association with a polyp (n=11), followed by diverticula (n=5), ulcer (n=5), and in reddish-appearing mucosal plaque, folds, or flaps (n=4). The majority of the lesions were located more than 5 cm above from the anal verge. However, lesions less than 2 cm above the anal verge and more than 9 cm do occur.
Table 1.
Summary of reported pediatric cases of gastric heterotopia in rectum.
| Reference | Age/Sex | Presenting symptoms | Duration | Site of lesion | Lesion |
|---|---|---|---|---|---|
|
| |||||
| Shawartzenberg and Whitington15 | 6 mo/M | Intermittent rectal bleeding and colic | 4 mo | 2 cm from anus | Diverticulum |
| Sugarman et al16 | 13 mo/F | Rectal bleeding and ulcers | 1 d | 6 cm from anus | Polyp |
| Parkash et al17 | 18 mo/F | Perianal ulceration, pruritus ani, and anocutaneous fistula | 15 mo | Left posterior | Diverticulum |
| Murray et al18 | 2 y/F | Rectal bleeding | 16 mo | Throughout colon | Polypoid, ulcer |
| Wiersma et al19 | 2 y/M | Rectal bleeding | NA | 1 cm from the dentate line | Ulcer |
| Cheli et al20 | 2 y/M | Rectal bleeding | 1 y | 4 cm from anal verge | Mucosal lesion |
| Marines et al21 | 3 y/M | Rectal bleeding and abdominal pain | 5 mo | 5 cm from anus | Polyp |
| Garmendia et al22 | 4 y/M | Rectal bleeding, weight loss, and loose stools | NA | 5 cm from anorectal junction | Mass |
| Kalani et al5 | 4 y/M | Bloody diarrhea, ulcers, and rectovesical fistula | 1 yr | 2 cm above pectinate line | Mucosal fold |
| Stockman et al23 | 4 y/F | Rectal bleeding | 2 y | At 5 cm from anorectal junction | Diverticulum |
| Nigro et al24 | 5 y/M | Rectal bleeding | 1 mo | 6 cm from anal verge | Polyp |
| Sauer C et al13 | 5 y/F | Painless rectal bleeding | 2.5 y | 5 cm from anus | Polypoid lesion |
| Ewell and Jackson25 | 6 y/M | Rectal bleeding and ulcer | 1 wk | 5 cm above anus | Polyp |
| Thompson et al26 | 6 y/M | Rectal bleeding | NA | Anus | Diverticulum |
| Wolff M27 | 7 y/M | Rectal bleeding | NA | 8 cm from pectinate line | Polyp |
| Kestemberg et al7 | 9 y/M | Rectal bleeding | NA | Rectum | Polyp |
| Kumar et al28 | 10 y/M | Rectal bleeding and proctalgia | 2 yr | 9 cm from anal verge | Diverticulum |
| Lord and Tribe29 | 11 y/M | Rectal bleeding | 6 mo | 1 cm above anus | Mucosal flap |
| Carlei et al2 | 13 y/M | Rectal bleeding and tenesmus | 2–3 cm above dentate line | Ulcer | |
| Antonietta et al30 | 13 y/M | Rectal bleeding and tenesmus | 1 d | 2–3 cm above pectinate line | Ulcer |
| Picard et al31 | 14 y/M | Rectal bleeding and ulcers | 12 y | 3 cm above dentate line | Ulcer |
| Jordan et al32 | 16 y/M | Rectal bleeding, pain, and ulcer | 4 y | 4 cm above dentate line | Polyp |
| Edouard et al33 | 17 y/M | Rectal bleeding, rectal syndrome, and ulcer | 1 d | 3 cm from anus | Polyp |
| Kokil et al34 | 12 y/M | Rectal bleeding | 10 y | 3 cm from anus | Polyp |
| Present case | 3 y/M | Rectal bleeding anal pain | 8 mo | 0.5 cm proximal to dentate line | Rectal ulcer |
Cm: Centimeter, F: female, M: male, mo: month, NA: not available, Wk: week, y: year.
The natural history of gastric heterotopia is unknown. Serious complications because of heterotopic gastric mucosa included major gastrointestinal bleeding, bowel perforation, intussusception, and rectovesical fistula.3–6 H pylori organisms have been noted in rectal gastric heterotopic mucosa; the eradication of the organism resulted in the resolution of chronic active gastritis in the heterotopic mucosa.7 This finding supports the possibility that H pylori organisms might pass along the gastrointestinal tract in a viable form to colonize ectopic gastric tissue in the rectum and contribute to the ulceration and bleeding seen in these cases. It is unclear whether and how often heterotopic gastric mucosa progresses to malignancy. Although there have been no case reports that specifically describe malignant transformation of heterotopic gastric mucosa of the rectum, there have been 6 cases of gastric heterotopia of the esophagus that presented as adenocarcinoma8,9 and 1 report described a relationship between heterotopic gastric mucosa in the colon and a premalignant tubule-villous adenoma.10 All of these cases were in older adults, and the duration of gastric heterotopia in the esophagus was unknown.
The definitive diagnosis of gastric heterotopia requires histopathological demonstration of a gastric mucosa outside the stomach. Technetium scanning can be used as adjunctive aid in the localization of gastric heterotopias,11,12 but direct visualization and biopsy are needed to confirm the diagnosis. In many of the cases cited in Table 1, the symptoms were present for many years, and patients underwent extensive work-up prior to diagnosis including laparotomy in 1 case. Endoscopist may miss the lesion if it is too close to the anal verge, which emphasizes on the importance to carefully inspect the rectal segment just above the anus during colonoscopy for rectal bleeding. Sampling error, when biopsies are obtained from an inappropriate site, is another reason for delay in the diagnosis of gastric heterotopia of the rectum.
Gastric heterotopia of the rectum, presenting with a bleeding ulcer, can be mistaken with solitary rectal ulcer. These two different rectal pathologies should be differentiated because the therapy is different, and indeed the use of steroid enema to treat solitary rectal ulcer can worsen the outcome of ulcer secondary to gastric heterotopia, as in our case. Constipation and rectal prolapse usually accompany solitary rectal ulcer, while anal pain occurs with rectal gastric heterotopia. The definitive diagnosis of both entities mandates histopathological confirmation. The characteristic histopathological findings of solitary rectal ulcer constitute elongation with fibrosis and extension of fibers from the muscularis mucosa into the lamina propria, while the histopathological diagnosis of gastric heterotopia necessitates the demonstration of gastric mucosa.
In a number of case reports, patients with heterotopic gastric mucosa were treated with H2 receptor blockers or proton pump inhibitors.11,12 These therapies may ameliorate or eliminate symptoms, but they do not cause involution of the mucosal abnormalities; when the medication is discontinued, bleeding quickly recurs.13 Given concerns for possible malignant transformation over the long term, the resection of the lesion should be performed surgically or endoscopically.14 No recurrences have been reported.
In conclusion, heterotopic gastric mucosa of rectum should be considered in the differential diagnosis of a bleeding rectal ulcer to prompt early diagnosis and surgical resection of the ectopic gastric mucosa.
REFERENCES
- 1.Morrison JE. Foetal and neonatal pathology. Washington DC: Butterworth; 1963. pp. 297–8. [Google Scholar]
- 2.Carlei F, Pietroletti R, Lomanto D, Barsotti P, Crescenzi A, Pistoia MA, et al. Heterotopic gastric mucosa of the rectum--characterization of endocrine and mucin-producing cells by immunocytochemistry and lectin histochemistry. Report of a case. Dis Colon Rectum. 1989;32:159–64. doi: 10.1007/BF02553831. [DOI] [PubMed] [Google Scholar]
- 3.Lambert MP, Heller DS, Bethel C. Extensive gastric heterotopia of the small intestine resulting in massive gastrointestinal bleeding, bowel perforation, and death: report of a case and review of the published reports. Pediatr Dev Pathol. 2000;3:277–280. doi: 10.1007/s100249910036. [DOI] [PubMed] [Google Scholar]
- 4.Chandrakamol B. Gastric heterotopia in the ileum causing hemorrhage. J Pediatr Surg. 1978;13:484–487. doi: 10.1016/s0022-3468(78)80310-8. [DOI] [PubMed] [Google Scholar]
- 5.Kalani BP, Vaezzadeh K, Sieber WK. Gastric heterotopia in the rectum complicated by rectovesical fistula. Dig Dis Sci. 1983;28:378–380. doi: 10.1007/BF01324959. [DOI] [PubMed] [Google Scholar]
- 6.Dubilier LD, Caffrey PR, Hyde GL. Multifocal gastric heterotopia in a malformation of the colon presenting as a megacolon. Am J Clin Pathol. 1969;51:646–653. doi: 10.1093/ajcp/51.5.646. [DOI] [PubMed] [Google Scholar]
- 7.Kestemberg A, Marino G, de Lima E, Garcia FT, Carrascal E, Arredondo JL. Gastric heterotopic mucosa in the rectum with Helicobacter pylori-like organisms: a rare cause of rectal bleeding. Int J Colorectal Dis. 1993;8:9–12. doi: 10.1007/BF00341269. [DOI] [PubMed] [Google Scholar]
- 8.Christensen WN, Sternberg SS. Adenocarcinoma of the upper esophagus arising in ectopic gastric mucosa. Two case reports and review of the published reports. Am J Surg Pathol. 1987;11:397–402. doi: 10.1097/00000478-198705000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Berkelhammer C, Bhagavan M, Templeton A, Raines R, Walloch J. Gastric inlet patch containing submucosally infiltrating adenocarcinoma. J Clin Gastroenterol. 1997;25:678–681. doi: 10.1097/00004836-199712000-00025. [DOI] [PubMed] [Google Scholar]
- 10.Cappell MS. Colonic tubulovillous adenoma associated with gastric heterotopia. N J Med. 1995;92:512–515. [PubMed] [Google Scholar]
- 11.Sfakianakis GN, Haase GM. Abdominal scintigraphy for ectopic gastric mucosa: a retrospective analysis of 143 studies. AJR Am J Roentgenol. 1982;138:7–12. doi: 10.2214/ajr.138.1.7. [DOI] [PubMed] [Google Scholar]
- 12.Steele SR, Mullenix PS, Martin MJ, Ormseth E, Weppler E, Graham J, et al. Heterotopic gastric mucosa of the anus: a case report and review of the published reports. Am Surg. 2004;70:715–19. [PubMed] [Google Scholar]
- 13.Sauer CG, Bickston SJ, Borowitz SM. Gastric heterotopia of the rectum. J Pediatr Gastroenterol Nutr. 2010;50:329–33. doi: 10.1097/MPG.0b013e3181a1c476. [DOI] [PubMed] [Google Scholar]
- 14.Muto M, Miyamoto S, Hosokawa A, Doi T, Ohtsu A, Yoshida S, et al. Endoscopic mucosal resection in the stomach using the insulated-tip needle-knife. Endoscopy. 2005;37:178–182. doi: 10.1055/s-2004-826194. [DOI] [PubMed] [Google Scholar]
- 15.Shawartzenberg SJ, whitington PF. Rectal gastric mucosa heterotopia as a cause of hematochezia in an infant. Dig Dis Sci. 1983;28:470–3. doi: 10.1007/BF02430537. [DOI] [PubMed] [Google Scholar]
- 16.Sugarman GI, Weitzman JJ, Isaacs H, Jr, Beck DB. Rectal bleeding from gastric tissue in the rectum. Lancet. 1970;1:251. doi: 10.1016/s0140-6736(70)90623-9. [DOI] [PubMed] [Google Scholar]
- 17.Parkash S, Veliath AJ, Chandrasekaran V. Ectopic gastric mucosa in duplication of the rectum presenting as a perianal fistula. Dis Colon Rectum. 1982;25:225–226. doi: 10.1007/BF02553109. [DOI] [PubMed] [Google Scholar]
- 18.Murray FE, Lombard M, Dervan P, Fitzgerald RJ, Crowe J. Bleeding from multifocal heterotopic gastric mucosa in the colon controlled by an H2 antagonist. Gut. 1988;29:848–851. doi: 10.1136/gut.29.6.848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wiersma R, Hadley GP, Govender D, Grant HW. Rectal gastric heterotopia in infancy. J Pediatr Surg. 2002;37:1481–1482. doi: 10.1053/jpsu.2002.35420. [DOI] [PubMed] [Google Scholar]
- 20.Cheli M, Alberti D, Vavassori D, Sonzogni A, Pedretti E, Locatelli G. Heterotopic rectal gastric mucosa: a rare cause of lower gastrointestinal bleeding in children. Case report and review of pediatric published reports. Eur J Pediatr Surg. 2007;17:50–54. doi: 10.1055/s-2007-964916. [DOI] [PubMed] [Google Scholar]
- 21.Menchaca Marines MC, Posselt HG, Waag KL. Ectopic gastric mucosa in the rectum: a rare cause of rectal bleeding in children. J Pediatr Gastroenterol Nutr. 1988;7:293–297. doi: 10.1097/00005176-198803000-00023. [DOI] [PubMed] [Google Scholar]
- 22.Garmendia M, Aparicio JR, Martinez J, Casellas JA. Heterotopic gastric mucosa in the rectum. Gastrointest Endosc. 2007;65:921–22. doi: 10.1016/j.gie.2006.07.017. [DOI] [PubMed] [Google Scholar]
- 23.Stockman JM, Young VT, Jenkins AL. Duplication of the rectum containing gastric mucosa. JAMA. 1960;173:1223–25. doi: 10.1001/jama.1960.73020290004010a. [DOI] [PubMed] [Google Scholar]
- 24.Nigro ND, Hiratzka T. Aberrant gastric mucosa in the rectum: a case report. Dis Colon Rectum. 1961;4:275–76. doi: 10.1007/BF02616605. [DOI] [PubMed] [Google Scholar]
- 25.Ewell G, Jackson R. Aberrant gastric mucosa in the rectum with ulceration and hemorrhage. Wis Med J. 1939;38:641–643. [Google Scholar]
- 26.Thompson RJ, Charlton FG, Jaffray B. Acid-secreting rectal duplication cyst with associated peptic ulcer eroding through the anal sphincters. J Pediatr Surg. 2002;37:E37. doi: 10.1053/jpsu.2002.36210. [DOI] [PubMed] [Google Scholar]
- 27.Wolff M. Heterotopic gastric epithelium in the rectum: a report of three new cases with a review of 87 cases of gastric heterotopia in the alimentary canal. Am J Clin Pathol. 1971;55:604–16. doi: 10.1093/ajcp/55.5.604. [DOI] [PubMed] [Google Scholar]
- 28.Kumar R, Shun A, Arbuckle S, Gaskin K. Diverticular rectal duplication with heterotopic gastric mucosa in a child: a rare cause of rectal bleeding. J Paediatr Child Health. 2000;36:191–92. doi: 10.1046/j.1440-1754.2000.00482.x. [DOI] [PubMed] [Google Scholar]
- 29.Lord PH, Tribe CR. Gastric tissue in the rectum. Lancet. 1970;1:566–567. doi: 10.1016/s0140-6736(70)90799-3. [DOI] [PubMed] [Google Scholar]
- 30.Antonietta Pistoia M, Guadagni S, Ventura T, Pistoia F, Carboni M. Gastric heterotopia of the rectum. Endoscopy. 1986;18:34. doi: 10.1055/s-2007-1018320. [DOI] [PubMed] [Google Scholar]
- 31.Picard EJ, Picard JJ, Jorissen J, Jardon M. Heterotopic gastric mucosa in the epiglottis and rectum. Am J Dig Dis. 1978;23:217–21. doi: 10.1007/BF01072320. [DOI] [PubMed] [Google Scholar]
- 32.Jordan FT, Mazzeo RJ, Soiderer MH. Heterotopic gastric mucosa of the rectum. A rare cause of rectal bleeding. Arch Surg. 1983;118:878–80. doi: 10.1001/archsurg.1983.01390070086019. [DOI] [PubMed] [Google Scholar]
- 33.Edouard A, Jouannelle A, Amar A, Doutone P, Maurice P, Galand A. Heterotopie de muqueuse gastrique darts le rectum avec ulceration. Gastroenterol Clin Biol. 1983;7:39–42. [PubMed] [Google Scholar]
- 34.Kokil G, Pulimood A, Mathai J. A rare case of a rectal polyp with gastric heterotopia. Indian J Pathol Microbiol. 2011;54:848–9. doi: 10.4103/0377-4929.91521. [DOI] [PubMed] [Google Scholar]