Abstract
Cefriaxone is a third-generation cephalosporin that might rarely cause a severe allergic reaction. Acute cardiac emergencies are quite rare in the setting of drug allergies. Here, we report the first case of myocardial infarction and AV-block after intravenous cefriaxone administration.
Cefriaxone is a widely used broad-spectrum anti-microbial agent. A few adverse reactions to the molecule have been described so far. Although hypersensitivity reactions have been rarely reported, these reactions are more likely to occur in individuals with a history of cephalosporin hypersensitivity and/or a history of sensitivity to multiple allergens.1,2 The concurrence of acute coronary syndromes (ACS) with mast cell activation induced by allergic or hypersensitivity and anaphylactic or anaphylactoid reactions have been reported infrequently. As it was first described by Kounis as “allergic angina syndrome” progressing to “allergic myocardial infarction,” the condition has been called “Kounis syndrome” (KS) recently.3–6 Herein, we present a patient who developed ACS after intravenous (IV) ceftriaxone administration, and we describe the pathophysiology and clinical implications of this syndrome.
To the best of our knowledge, this is the first case of ST-segment elevation inferior wall myocardial infarction with AB-block and angiographic evidence of diffuse right coronary artery spasm after IVceftriaxone administration.
CASE
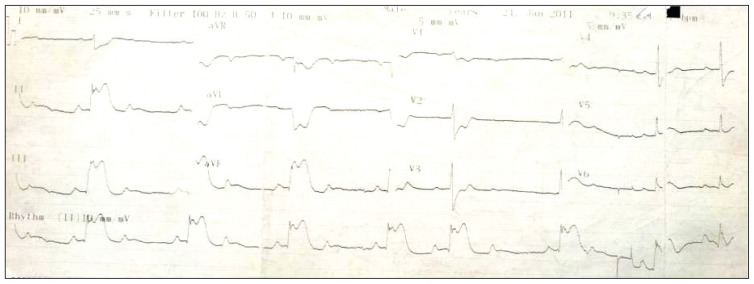
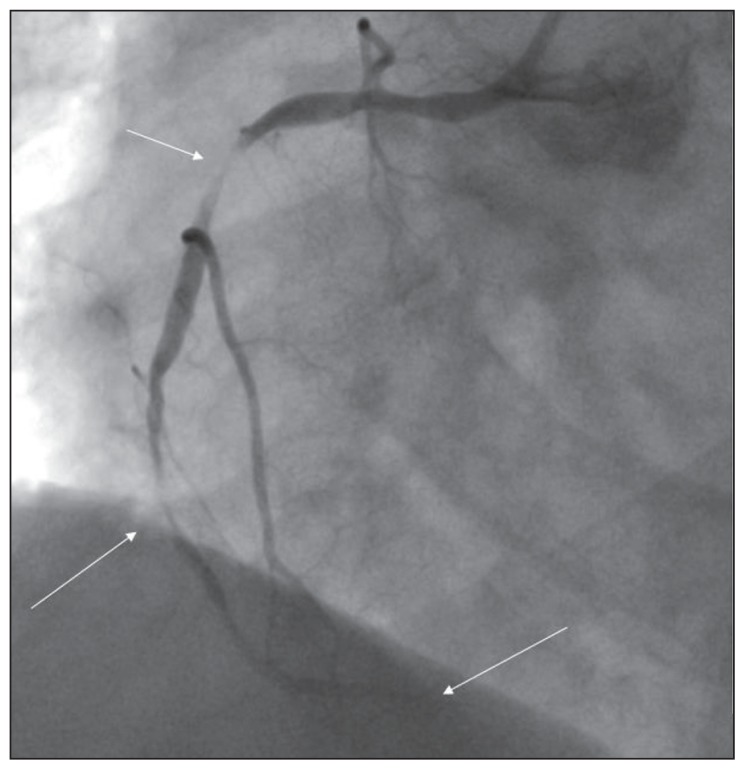
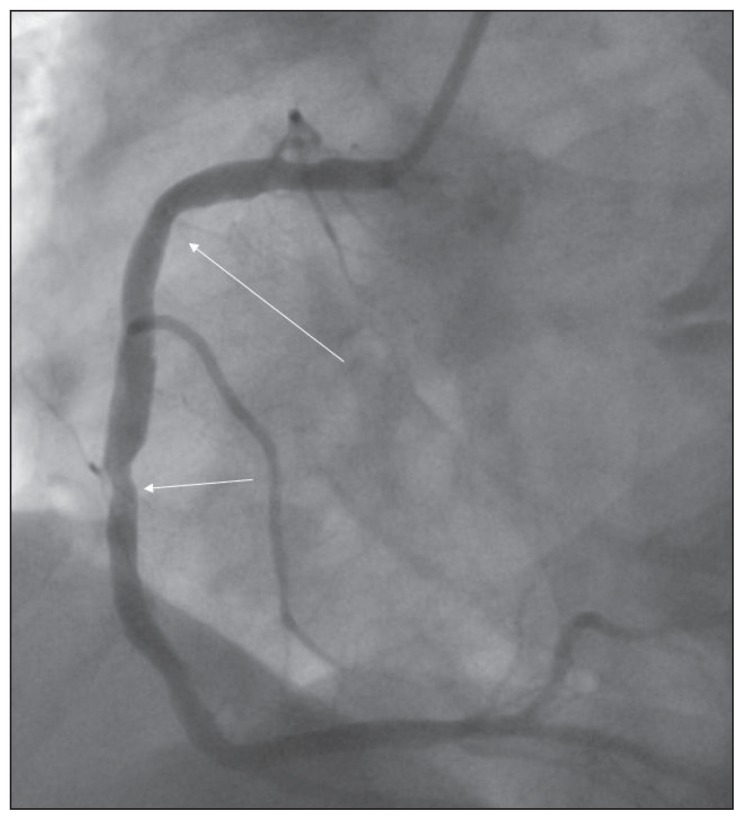
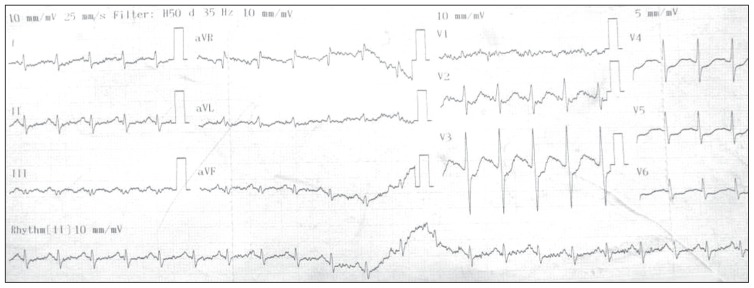
A 65-year-old man was admitted to the general medical ward for an acute urinary tract infection of 5 days’ duration. The patient claimed burning micturation, increase urination frequency, and suprapubic pain with no fever. He had neither a medical history of coronary artery disease, nor allergy, cutaneous, or respiratory evidence of anaphylaxis. On physical examination, he looked in good general condition; his blood pressure was 155/80 mm Hg and pulse 80 bpm, he was afebrile, and had mild loin tenderness. Laboratory tests showed a slight neutophilic leukocytosis (white blood cells [WBC] 13 300/mm3) with pyuria (15 neutrophil/high-power field). Pulse oxymetry was satisfactory (98%), and electrocardiogram (ECG) showed normal frequency with normal sinus rhythm. A right brachial venous canula was positioned, and 1 g ceftriaxone was IV administered. Within 10 minutes after administration, he complained of epigastric pain, malaise, shortness of breath, central chest pain, and drowsiness, and then collapsed. He was sweaty and dyspneic, blood pressure was 80/50 mm Hg, pulse was 35 bpm, and he was hypoxic with 75% oxygen saturation. Cardiopulmonary resuscitation was started; the patient was intubated and IV saline infusion was initiated. An urgent 12-lead ECG was performed, which revealed ST-segment elevation in leads 11.111 and aVF with 2:1 AV-block (Figure 1). Intravenous heparin (5 000 U) was given to the patient. He was admitted to the catheterization laboratory, and immediate coronary angiography was done for possible primary angioplasty. Coronary angiography revealed normal left coronary system, tight multiple stenotic segments of right coronary artery, and normal ventriculography (Figure 2). These lesions looked like spasm more than thrombus. Right Intracoronary nitroglycerin (100 μg) was administered, and 5 seconds later right coronary angiogram revealed no previous stenotic segments and insignificant plaques (Figure 3). The ECG on monitor reverted to sinus rhythm with no AV-block, and systolic blood pressure stabilized at about 110 to 120 mm Hg. The patient was monitored for 15 minutes in cath lab and then transferred to the coronary care unit with the diagnosis of coronary spasm secondary to ceftriaxone ingestion. Calcium antagonist, diltiazem (90 mg), was administered twice a day. Laboratory analysis showed the elevation of cardiac troponin from 0.01 ng/mL to 1.6 ng/mL (normal level: 0.01–0.03 ng/mL). A 12-lead ECG revealed normal sinus rhythm with no AV-block (Figure 4). The patient was extubated next morning, and he showed continuous improvement. Transthoracic echocardiography revealed normal wall motions. His recovery was uneventful, and he was discharged on his fourth day at the hospital.
Figure 1.
12-lead ECG shows ST-segment elevation in leads 11.111 and aVF with 2:1 AV-block.
Figure 2.
Right coronary angiogram shows multiple tight stenotic segments.
Figure 3.
Right coronary angiogram after intracoronary nitrate.
Figure 4.
ECG revealed normal sinus rhythm with no AV-block.
He was seen doing well in the outpatient clinic 3 months later. His case was considered as myocardial infarction due to an allergic reaction because of the following reasons: symptoms of chest pain, electrocardiogram changes of ST-segment elevation in inferior leads and A-block, diffuse right coronary spasm after ceftriaxone injection and resolution after intracoronary nitrate injection, and cardiac marker elevation., This condition is commonly known as Kounis syndrome. In our patient, the coronary spasm lasted about 20 minutes, till intracoronary nitrate was given.
DISCUSSION
The development of ACS after exposure to an allergic insult is an unexpected and rarely reported phenomenon. This concept of “coincidental occurrence of chest pain and allergic reactions accompanied by clinical and laboratory findings of angina pectoris” was first described in 1991 and named as the “Kounis syndrome.”3–6 Many hypotheses have been proposed to explain a causal relationship between allergic reactions and acute coronary events after the recognition of this clinical entity. Of these, mast cell–driven vasospastic and inflammatory response acting on the coronary endothelium has gained acceptance as the main causative mechanism. Mast cells are found in most parts of the human body including the coronary vessels. During an acute allergic reaction, activated mast cells degranulate and release a number of mediators, such as histamine, tryptase, platelet-activating factor, leukotrienes, and thromboxane, which were experimentally shown to lead coronary artery spasm or plaque rupture.
Two variants of the Kounis syndrome have been described as follows: type 1 refers to patients with normal coronary arteries who develop coronary vasospasm and type 2 occurs in patients with atheromatous coronary artery disease in whom plaque rupture is incriminated for the ensuing angina episode.7 Until now, the Kounis syndrome was found to be related with poisons, venoms, drugs, and contrast agents. Among these, antibiotics– related ACS is rare and is reported commonly with penicillin in the course of an anaphylactic shock where coronary hypoperfusion and epinephrine–induced vasospasm were strongly proposed to explain the underlying mechanism of myocardial injury.8 However, allergy–induced acute coronary events in the absence of anaphylaxis are increasingly encountered in clinical practice, suggesting the mast cell–based vasospasm as the principal mechanism.9
It is also hypothesized that there is a threshold level of mast cell content above which it can provoke coronary artery spasm and plaque rupture. This threshold level is closely associated with the allergen concentration, patient’s sensitivity, and route of antigen entrance.10 There are studies reporting that immunoglobulin E antibodies with different specificities can have additive effect, and corresponding antigens can trigger mediator release when the patient is simultaneously exposed to them. This leads to suggest that atopic individuals are more vulnerable to coronary artery spasm than normal people.3–6 The Kounis syndrome can appear in elderly as well as in pediatric age,11,12 although predictive risk factors have not been identified.
In published reports, more than 30 cases of the Kounis syndrome induced by betalactams have been reported, 4 and amoxicillin is the most frequently involved molecule followed by ampicillin, penicillin G, various cephalosporins, and piperacillin/tazobactam. However, no case of the Kounis syndrome due to the infusion of ceftriaxone has been ever reported previously.13–21 The Kounis syndrome potentially represents a lethal and underestimated clinical emergency, and its treatment requires an urgent intensive-type therapy with a high cardiac expertise.
In our patient, myocardial injury occurred in the absence of an anaphylactic reaction, strengthening the concept of mast cell–based pathophysiology. However, his chest pain developed suddenly without any apparent allergic reaction, postulating a possible local effect of ceftriaxone directly on the coronary mast cells. This sole cardiac involvement may represent another edge of allergic reactions ranging from urticaria to anaphylaxis. The reason for this variation in clinical manifestations is also a subject of investigations.
Concerning the type of the Kounis syndrome in the present case, the transiency of ST segment elevations and the absence of a definite thrombosed related artery that could account for these electrocardiographic changes indicate coronary spasm and type 1 variant. However, the presence of atheromatous coronary lesions refers to the type 2 Kounis syndrome. We speculate a third variant that should be taken into consideration to describe such patients with preexisting coronary artery disease experiencing vasospasm without plaque rupture.
The patients admitting with chest pain and electrocardiographic abnormalities should also be interrogated for any history of recent exposure to any allergic insult including drugs. The people who have a prehistory of atopia must be evaluated with a more probable diagnosis of the Kounis syndrome. On the basis of the anticipated vasospastic mechanism, nitrates or calcium channel blockers may be attempted as an alternative first-line therapy before considering unnecessary intervention with fibrinolytic agents or percutaneous revascularization; otherwise, coronary angiography should be done as soon as possible before giving potent anticoagulant and antiplatelet therapy.
Footnotes
Conflict of interest
Non-declared.
REFERENCES
- 1.Norrby SR. Side effects of cephalosporins. Drugs. 1987;34(supp 2):105. doi: 10.2165/00003495-198700342-00009. [DOI] [PubMed] [Google Scholar]
- 2.Kelkar PS, Li JT. Cephalosporin allergy. N Engl J Med. 2001;354:804. doi: 10.1056/NEJMra993637. [DOI] [PubMed] [Google Scholar]
- 3.Kounis NG, Zavras GM. Histamine-induced coronary artery spasm: the concept of allergic angina. Br J Clin Pract. 1991;45:121–128. [PubMed] [Google Scholar]
- 4.Biteker M. Current understanding of Kounis syndrome. Expert Rev Clin Immunol. 2010;6:1–12. doi: 10.1586/eci.10.47. [DOI] [PubMed] [Google Scholar]
- 5.Kounis NG. Kounis syndrome (allergic angina and allergic myocardial infarction): a natural paradigm? Int J Cardiol. 2006;110:7–16. doi: 10.1016/j.ijcard.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 6.Matucci A, Rossi O, Cecchi L, Vultaggio A, Parronchi P, Brugnolo F, Maggi E, Romagnani S. Coronary vasospasm during an acute allergic reaction. Allergy. 2002;57:867–868. doi: 10.1034/j.1398-9995.2002.23575_11.x. [DOI] [PubMed] [Google Scholar]
- 7.Biteker M. A new classification of Kounis syndrome. Int J Cardiol. 2010;145:553. doi: 10.1016/j.ijcard.2010.05.020. [DOI] [PubMed] [Google Scholar]
- 8.Kilic D, Evrengul H, Ozcan AV, Tanriverdi H, Cagliyan O, Kaftan A. Acute ST segment elevation myocardial infarction after sulbactam-ampicillin induced anaphylactic shock in an adult with significant coronary artery disease: a case report. Int J Cardiol. 2009;135:30–3. doi: 10.1016/j.ijcard.2008.03.069. [DOI] [PubMed] [Google Scholar]
- 9.Vivas D, Rubira JC, Ortiz AF, Macaya C. Coronary spasm and hypersensitivity to amoxicillin: Kounis or not Kounis syndrome? Int J Cardiol. 2008;128:279–81. doi: 10.1016/j.ijcard.2007.06.029. [DOI] [PubMed] [Google Scholar]
- 10.Koutsojannis Mazarakis A, Kounis CMNG, Alexopoulos D. Cefuroxime-induced coronary artery spasmmanifesting as Kounis syndrome. Acta Cardiol. 2005;60:341–5. doi: 10.2143/AC.60.3.2005015. [DOI] [PubMed] [Google Scholar]
- 11.Biteker M, Duran NE, Biteker FS, Gunduz S, Gokdeniz T, Kaya HH, Astarcioglu MA, Crossref MM. Kounis syndrome secondary to cefuroximeaxetil use in an octuagenarian. J Am Geriatric Soc. 2008;56:1757–8. doi: 10.1111/j.1532-5415.2008.01912.x. [DOI] [PubMed] [Google Scholar]
- 12.Biteker M, Duran NE, Biteker FS, Gunduz S, Gokdeniz T, Yildiz M, Ozkan M. Allergic myocardial infarction in childhood; Kounis syndrome. Eur J Pediatr. 2010;169:27–9. doi: 10.1007/s00431-009-0965-5. [DOI] [PubMed] [Google Scholar]
- 13.Ridella M, Bagdure S, Nugent K, Cevik C. Kounis syndrome following the betalactam antibiotics use: review of literature. Inflamm Allergy Drug Targets. 2009;8:11–6. doi: 10.2174/187152809787582462. [DOI] [PubMed] [Google Scholar]
- 14.Romano Á, Of Fonso M, Violet M, Adesi FB, Come A. Selective hypersensitivity to piperacillin. Allergy. 2000;55:787. doi: 10.1034/j.1398-9995.2000.00725.x. [DOI] [PubMed] [Google Scholar]
- 15.Muscat G, Galdi E, Scibilia J, Dellabianca Á, Omodeo P, City G, Viiadini G, Bircaldi GP. Occupational asthma, rhintis and urticaria two to piperacillin sodium in to pharmaceutical worker. Eur Respir J. 1995;8:467–9. doi: 10.1183/09031936.95.08030467. [DOI] [PubMed] [Google Scholar]
- 16.Bahn J, Lee J, Eom K, Jang S, Jung K. Occupational contact anaphylaxis from piperacillin in a nurse with atopic dermatitis. J Allergy Clin Immunol. 2006;S134:521. [Google Scholar]
- 17.Rank MA, Park MA. Anaphylaxis to piperacilln-tazobactam despite to negative penicillin skin tests. Allergy. 2007;62:964–5. doi: 10.1111/j.1398-9995.2007.01418.x. [DOI] [PubMed] [Google Scholar]
- 18.Kim JE, Kim SH, Kim JH, Bahn JW, Jin HJ, Ye YM, Park HS. A case of piperacillin-induced occupational anaphylaxis: detection of serum IgE to piperacillin–HSA–conjugate. J Korean Med Sci. 2011;26:682–5. doi: 10.3346/jkms.2011.26.5.682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sáenz de San Pedro B, Mayorga C, Torres MJ, Florido JF, Quiralte J, Blanca M. Boosted IgE response after anaphylaxis reaction to cefuroxime with crossreactivity with cefotaxime. Ann Allergy Asthma Immunol. 2002;89:101–3. doi: 10.1016/s1081-1206(10)61919-9. [DOI] [PubMed] [Google Scholar]
- 20.Ilhan E, Güvenç TS, Poyraz E, Ayhan E, Soylu O. Kounis syndrome secondary to cefuroxime axetil use in an asthmatic patient. Int J Cardiol. 2009;137:67–9. doi: 10.1016/j.ijcard.2009.04.026. [DOI] [PubMed] [Google Scholar]
- 21.Calogiuri GF, Nettis E, Di leo E, Vacca A, Ferrannini A, Kounis N. kounis syndrome induced by intravenous administration 0f piperacillin/tazobectam. International journal of cardiology. 2012;155:e42–e44. doi: 10.1016/j.ijcard.2011.07.049. [DOI] [PubMed] [Google Scholar]