Abstract
BACKGROUND AND OBJECTIVES
Psoriasis is a chronic inflammatory skin disease for which no specific reason has been found although various reasons have been suggested. Helicobacter pylori is a Gram-negative bacterium, which is essentially considered the cause of acute and chronic gastritis. Recently, several reports have suggested that H pylori could play a role in triggering psoriasis. The aim of this study was to determine the relationship between H pylori seropositivity and psoriasis.
DESIGN AND SETTINGS
This was a case-control study performed on patients with psoriasis vulgaris and healthy individuals in Fatemiye Hospital (referral center for the treatment of skin diseases), Semnan, Iran, during April 2011 to April 2012.
METHODS
A case-control study including 61 patients with psoriasis vulgaris (case group) and 61 healthy individuals (control group) without any known gastrointestinal complications were enrolled. All cases were tested for H pylori infection with serology (immunoglobulin G [IgG] anti-H pylori) using the enzyme-linked immunosorbent assay method.
RESULTS
Ten (16.4%) of the psoriatic patients and 8 (13%) of the control groups had an H pylori seropositive test result; the average of IgG serum level was 17.3 IU/ML in psoriatic patients and 16.1 IU/ML in the control group. The difference of serum level between the 2 groups was not meaningful (P=.302).
CONCLUSIONS
Our finding indicated that there was neither a significant relationship between psoriasis and the serum level of IgG anti-H pylori, nor a significant relationship between psoriasis severity and the serum level of IgG anti-H pylori. Further studies should be designed to find out whether infection with H pylori is one of the reasons causing or aggravating psoriasis.
Psoriasis is a common chronic inflammatory skin disorder characterized by sharply demarcated red scaly plaques, which may occur on any part of the body but preferentially at extensor areas. The prevalence is about 2% to 3% of the adult population and affects men and women equally and can be seen in all races.1,2 Psoriasis has grave impacts on the quality of life, even in patients with a mild disease.3 Researchers believe the disease is caused by genetic and environmental factors and is an autoimmune disease.4 The pathophysiology of psoriasis is characterized by an increase in antigen presentation, T-cell activation, and T-helper cell type 1 cytokines. Also, an increasing level of C-reactive protein levels and platelet activation factors has been observed.4,5 Heredity undoubtedly plays a role in causing psoriasis, and several psoriatic human genes have been identified. However, environmental factors also play a role in the etiology of this disease.4,6 These factors include trauma, endocrine and metabolic factors, drugs, smoking, alcohol, sunlight, and some infections. 2, 4 The role of infectious agents Streptococci A has been demonstrated.6 Recent studies have shown that H pylori may also, like the Streptococcus hemolytic group A, be a trigger factor in psoriasis,7–10 although some other studies have refuted this relationship.11,12 H pylori is a Gram-negative micro-aerophilic spiral bacterium that resides in the gastric mucosa and plays a role in the pathogenesis of gastritis and peptic ulceration.13,14 Recent evidence suggests that H pylori infection plays roles in the pathogenesis of various skin diseases.15,16 The prevalence of H pylori infection is 30% in the United States and other developed countries and is over 80% in developing countries.17 The infection is acquired by oral ingestion of the bacterium and is mainly transmitted within families in the early childhood.18 Several methods are available for the detection of H pylori infection. Serology investigation is specific in more than 90% of the cases.19 H pylori Infection produces IgG and IgM against H pylori; IgM increases in the serum in acute infections and IgG increases in chronic infections. The ELISA method can be used to determine the level of antibodies especially for epidemiological studies, for the detection of infection in individuals.20 H pylori infection develops gastrointestinal diseases and has recently been shown to develop extraintestinal diseases.21 Although psoriasis is not a life-threatening disease, and for those who are not suffering from it may not seem important, it can affect the quality of life of affected individuals. Due to the conflicting results regarding the relationship between psoriasis and H pylori, the aim of this study was to evaluate the relationship between the two.
METHODS
This case-control study was done on 61 patients with psoriasis vulgaris (cases) and 61 healthy individuals (controls) in Fatemiye Hospital (referral center for the treatment of skin diseases), Semnan, Iran, during April 2011 to April 2012. Before starting, the study was approved by the ethics committee of Semnan University of Medical Sciences, Iran. Otherwise healthy individuals that had visited the dermatologist for cosmetic problems (control group) and documented psoriasis vulgaris patients (case group) fulfilled the inclusion criteria. Patients with a history of gastrointestinal problem, those who used oral corticosteroid or β-Blockers, and who used topical and systemic medication for 2 and 6 months, respectively, were excluded. All patients submitted their voluntarily written consent for the study. On the first visit, all patients were examined by a dermatologist; then, checklists that included information about age, sex, medical history, and drug history were completed. Psoriatic patients were clinically assessed before treatment on the basis of the psoriasis area and severity index (PASI) score and percentage of body surface area involved. The PASI was used to determine the severity of skin disease. The effect of IgG against H pylori was examined in all patients using enzyme-linked immunosorbent assay (ELISA) kit (DRG Instruments, GmbH, Marburg, Germany) according to the manufacturer’s protocol. The statistical analysis of the results was performed using paired student t; Chi-square, and logistic regression tests in SPSS, version 18 for windows. In this study, the significance level was set at P values of equal and less than .05.
RESULTS
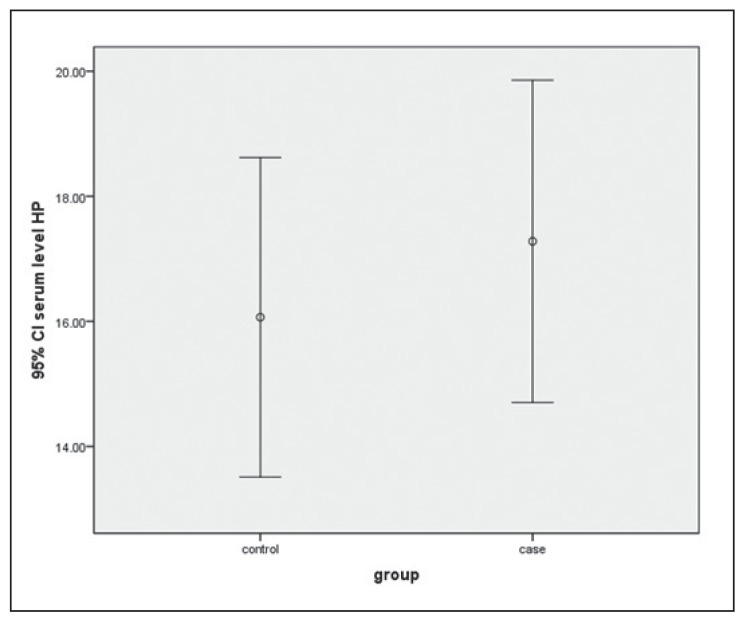
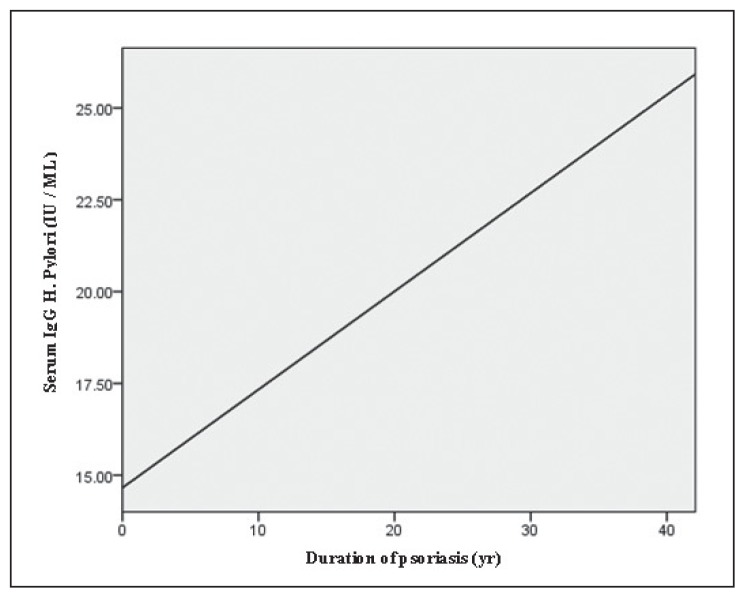
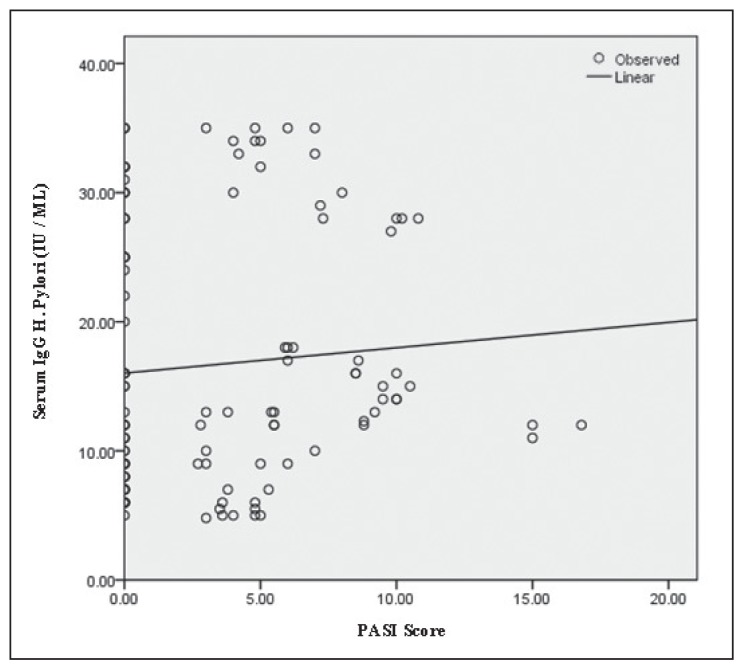
About 33 (54%) of psoriasis patients and 37 (60%) of the controls were female. Both groups were matched for sex (P=.464). In psoriasis patients, the age ranged from 9 to 61 years with a mean (SD) 33.3 (13.7) years and in the control group, the age ranged from 17 to 60 years with a mean (SD) 28/3 (8.4) years; the difference was significant (P=.017). The mean (SD) number of years that have passed since the development of psoriasis in 61 patients was 9.8 (8.3) years, with a median of 8 years. The PASI score range was 2.7 to 16.8 in patients with a mean (SD) 6.6 (3.1). The mean (SD) serum IgG in psoriasis patients was 17.3 (10.1) IU/ML and in the control group, 16.1 (10) IU/ML. Distribution levels were not significantly different between the 2 groups (P=.302) (Figure 1). Due to the lack of homogeneity between the 2 groups in terms of age, the logistic revealed that there were significant differences (P=.001, CI=0.41–1.42) (Figure 2). Regression analysis to examine the relationship between PASI score and serum IgG showed no significant correlation (P=.39) (Figure 3).
Figure 1.
Mean (SD) serum IgG levels in the control group and psoriasis patients (case).
Figure 2.
Regression analysis to examine the relationship between serum IgG and duration of psoriasis.
Figure 3.
Regression analysis to examine the relationship between PASI score and serum IgG. PASI: Psoriasis area and severity index.
DISCUSSION
The relationship between psoriasis and H pylori is a challengeable issue in dermatology and gastroenterology. Our study reported no significant relationship between anti-H pylori serum IgG levels and psoriasis. Also no significant differences were found between psoriasis severity and IgG levels against H pylori. However, we found a significant relationship between the duration of psoriasis and serum IgG anti-H pylori levels. Fabrizi et al11 in Italy (in 2007) showed that 10% of people with psoriasis and 17% of the control group have H pylori Infection.11 This study result is compatible with our study. In a study by Wedi and Kapp in Germany (in 2002), no relationship between psoriasis and H pylori was seen.12 Additional studies are contrary to the results of this study; for example, in a study by Qayoom and Ahmad in India (in 2003), the incidence of H pylori infection in psoriatic patients was 44%, while in the control group it was only 10%.7 Also Halasz CL in 1996 showed that the prevalence of IgG against H pylori was in 54% of psoriatic patients, but this study had no control group for comparison.8 In a study by Onsun et al9 in 2012, 300 patients with psoriasis and 150 healthy individuals were enrolled. The PASI score in patients infected with H pylori was clearly higher, and simultaneous treatment of psoriasis and H pylori in patients with psoriasis was more effective than psoriasis treatment alone.9 In contrast to our study, they suggested that H pylori infection plays a role in psoriasis severity, and H pylori treatment was effective in the treatment of psoriasis. In our study, the only significant relationship was seen between the duration of psoriasis and the serum IgG level against H pylori. This may be due to the use of topical or systemic immunosuppressive drugs over time that gave psoriatic patients greater susceptibility to H pylori infection. Today, the existing controversy about the relationship between psoriasis and H pylori infection is perhaps due to difference in sample sizes, severity of disease, and difference in the level of public health. So it appears that the relationship between psoriasis and H pylori infection is not clear. Finally more researches need to be done to clarify this issue.
REFERENCES
- 1.Stern RS, Nijsten T, Feldman SR, Margolis DJ, Rolstad T. Psoriasis is common, carries a substantial burden even when not extensive, and is associated with widespread treatment dissatisfaction. J Investig Dermatol Symp Proc. 2004;9(2):136–9. doi: 10.1046/j.1087-0024.2003.09102.x. [DOI] [PubMed] [Google Scholar]
- 2.Christophers E. Psoriasis--epidemiology and clinical spectrum. Clin Exp Dermatol. 2001;26(4):314–20. doi: 10.1046/j.1365-2230.2001.00832.x. [DOI] [PubMed] [Google Scholar]
- 3.Rapp SR, Feldman SR, Exum ML, Fleischer AB, Jr, Reboussin DM. Psoriasis causes as much disability as other major medical diseases. J Am Acad Dermatol. 1999;41(3 Pt 1):401–7. doi: 10.1016/s0190-9622(99)70112-x. [DOI] [PubMed] [Google Scholar]
- 4.Nestle FO, Kaplan DH, Barker J. Psoriasis. N Engl J Med. 2009;361(5):496–509. doi: 10.1056/NEJMra0804595. [DOI] [PubMed] [Google Scholar]
- 5.Krueger JG, Bowcock A. Psoriasis pathophysiology: current concepts of pathogenesis. Ann Rheum Dis. 2005;64(Suppl 2):ii30–6. doi: 10.1136/ard.2004.031120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Griffiths CEM, Camp RDR, Barker JNWN. Psoriasis. In: Burns TSB, Cox N, Griffiths C, editors. Rook’s Textbook of Dermatology. Malden, Massachusetts, USA: Blackwell Publishing, Inc; 2008. [Google Scholar]
- 7.Qayoom S, Ahmad QM. Psoriasis and Helicobacter Pylori. Indian J Dermatol Venereol Leprol. 2003;69(2):133–4. [PubMed] [Google Scholar]
- 8.Halasz CL. Helicobacter pylori antibodies in patients with psoriasis. Arch Dermatol. 1996;132(1):95–6. [PubMed] [Google Scholar]
- 9.Onsun N, Arda Ulusal H, Su O, Beycan I, Biyik Ozkaya D, Senocak M. Impact of Helicobacter Pylori infection on severity of psoriasis and response to treatment. Eur J Dermatol. 2012;22(1):117–20. doi: 10.1684/ejd.2011.1579. [DOI] [PubMed] [Google Scholar]
- 10.Ali M, Whitehead M. Clearance of chronic psoriasis after eradication therapy for Helicobacter pylori infection. J Eur Acad Dermatol Venereol. 2008;22(6):753–4. doi: 10.1111/j.1468-3083.2007.02452.x. [DOI] [PubMed] [Google Scholar]
- 11.Fabrizi G, Carbone A, Lippi ME, Anti M, Gasbarrini G. Lack of evidence of relationship between Helicobacter pylori infection and psoriasis in childhood. Arch Dermatol. 2001;137(11):1529. [PubMed] [Google Scholar]
- 12.Wedi B, Kapp A. Helicobacter pylori infection in skin diseases: a critical appraisal. Am J Clin Dermatol. 2002;3(4):273–82. doi: 10.2165/00128071-200203040-00005. [DOI] [PubMed] [Google Scholar]
- 13.Peek RM, Jr, Blaser MJ. Helicobacter pylori and gastrointestinal tract adenocarcinomas. Nat Rev Cancer. 2002;2(1):28–37. doi: 10.1038/nrc703. [DOI] [PubMed] [Google Scholar]
- 14.Sibony M, Jones NL. Recent advances in Helicobacter pylori pathogenesis. Curr Opin Gastroenterol. 2012;28(1):30–5. doi: 10.1097/MOG.0b013e32834dda51. [DOI] [PubMed] [Google Scholar]
- 15.Hernando-Harder AC, Booken N, Goerdt S, Singer MV, Harder H. Helicobacter pylori infection and dermatologic diseases. Eur J Dermatol. 2009;19(5):431–44. doi: 10.1684/ejd.2009.0739. [DOI] [PubMed] [Google Scholar]
- 16.Moravvej H, Hoseini H, Barikbin B, Malekzadeh R, Razavi G. Relationship of Helicobacter pylori with lichen planus. Indian Journal of Dermatology. 2007;52(3):138. [Google Scholar]
- 17.Malaty HM, Graham DY. Importance of childhood socioeconomic status on the current prevalence of Helicobacter pylori infection. Gut. 1994;35(6):742–5. doi: 10.1136/gut.35.6.742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rowland M, Kumar D, Daly L, O’Connor P, Vaughan D, Drumm B. Low rates of Helicobacter pylori reinfection in children. Gastroenterology. 1999;117(2):33641. doi: 10.1053/gast.1999.0029900336. [DOI] [PubMed] [Google Scholar]
- 19.Suerbaum S, Michetti P. Helicobacter pylori infection. N Engl J Med. 2002;347(15):1175–86. doi: 10.1056/NEJMra020542. [DOI] [PubMed] [Google Scholar]
- 20.Smoak BL, Kelley PW, Taylor DN. Seroprevalence of Helicobacter pylori infections in a cohort of US Army recruits. Am J Epidemiol. 1994;139(5):513–9. doi: 10.1093/oxfordjournals.aje.a117034. [DOI] [PubMed] [Google Scholar]
- 21.Parsonnet J, Isaacson PG. Bacterial infection and MALT lymphoma. N Engl J Med. 2004;350(3):213–5. doi: 10.1056/NEJMp038200. [DOI] [PubMed] [Google Scholar]