Abstract
Non-tuberculous mycobacteria (NTM) are composed of mycobacterial species other than the Mycobacterium tuberculosis complex. Initially thought to be mere contaminants when isolated from clinical specimens, literature is increasing by the day showing NTM as proven pathogens. Due to the difference in antimicrobial susceptibility of different species, it becomes imperative for the microbiology laboratory to identify them to the species level. Molecular methods are available for rapid and accurate identification, but in a resource limited nation, phenotypic methods, albeit time consuming, are of paramount importance. By means of this article, the authors intend provide a concise summary of the basic biochemical reactions which can be done to identify most commonly isolated NTM.
Keywords: Biochemical reactions, Non tuberculous mycobacteria, Phenotypic identification
1. Introduction
Non-tuberculous mycobacteria (NTM) are composed of mycobacterial species other than the Mycobacterium tuberculosis complex. They are widely distributed in nature and were initially thought to be mere contaminants when isolated. However, in the last few years they have been reported to cause a varied spectrum of diseases ranging from hospital acquired infections to infections following environmental exposure like hurricanes and tsunamis [1], [2], in both immunocompromised and immunocompetent individuals.
Epidemiological data from the Infectious Diseases Society of American Emerging Infections Network and information from referral centers suggest that NTM infections have been consistently on the rise [3]. Almost all diseases caused by rapidly growing mycobacteria in humans are due to M. fortuitum, M. chelonae, and M. abscessus [4]. They can affect respiratory tract, skin and soft tissue, causing diseases that include pulmonary infections [5], [6], [7], [8], and extra-pulmonary infections [6], [9], [10], [11], including traumatic and surgical wound infections [5], [12], [13], [14], [15], [16], [17], skin and soft tissue infections [2], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], implant-associated [29], [30], and catheter-associated infections [4], [31]. NTM have even been isolated from hospital cockroaches [32]. Sheer number of literature on NTM as pathogens highlight the importance of their identification which is still a dark zone, not many workers wanting to venture-into.
Numerous articles have been published on their classification [33], [34], ecology and physiology, virulence factors [35], risk factors [18], [36], [37], diseases and clinical features [11], [19]; and molecular characterization [38], [39], [40]. However, on review of literature very scanty data on phenotypic methods of identification of NTM is found, that too is scattered and difficult to comprehend for routine use by the students and laboratory staff. Hence, there is a necessity of information at one place for the benefit of research community. In a resource limited nation of South-East Asia, where laboratories have less than basic infrastructure, shortage of trained staff and molecular detection methods are available only in reference laboratories; there is a need to know phenotypic methods of speciation of NTM. This knowledge is required to prevent irrational use of antimicrobial agents as the susceptibility of Mycobacterium varies with species [41], [42], [43]. It should be remembered that all Mycobacterium isolates from patients are not Mycobacterium tuberculosis [44].
With the availability of commercial media and ready to use antibiotic susceptibility testing plates, reproducible and reliable results are obtained. This article is therefore, an attempt to describe the various simple yet cost effective methods of identification of the NTM species in a resource constrained setting.
2. Procedures
Described below are the procedures to perform various biochemical tests along with their principles. It is reiterated to follow universal safety precautions and all tests should be carried out in a bio-safety cabinet. Various biochemical tests with their principle and procedure are as follows:
2.1. Niacin accumulation test
-
•
Principle: All Mycobacterium species produce niacin ribonucleotide; but only M. tuberculosis, M. simiae and some strains of M. chelonae lack the enzymes to convert it further into nicotinamide adenine dinuceotide (NAD). Thus, niacin accumulates in the culture medium from which it can be extracted with sterile water or physiologic saline. The test demonstrates the presence of cyanogen chloride formed through the reaction of chloramine T and potassium thiocyanate in the presence of citric acid. The cyanogen chloride breaks the pyridine ring of niacin, forming the aldehyde gamma-carboxyglutamate that binds with the aromatic amine producing a yellow color.
-
•Materials: Niacin Detection Kit, Modified for Mycobacteria (K048; HiMedia Laboratories, Mumbai) which contains:
-
➢Part A
-
➢Part B
-
➢R055
-
➢
-
•
Procedure:
-
➢
Use only more than three week old mycobacterial culture grown on Lowenstein-Jensen (LJ) Medium Slants showing heavy growth. Cultures grown on other types of media do not produce enough niacin to yield a positive result by this method. (False negative test results, from the use of cultures, with too few organisms or from cultures grown on media other than LJ). Do not use this test on mixed cultures.
-
➢
Add 2 ml of sterile distilled water or saline to the slant.
-
➢
Cut or stab the slant with a spade or needle.
-
➢
Incubate the slant upright at 37 °C for two hours to allow extraction of niacin into the distilled water.
-
➢
Retain the slant in an upright position for five minutes.
-
➢
Use 1 ml of this solution as a test sample.
-
➢
Test isolate: Transfer content of Part A (1 ml) to Part B (1 ml). Use this as a reagent solution for further test.
-
➢
Transfer test sample (1 ml) to reagent solution (Part A+Part B) using a syringe.
-
➢
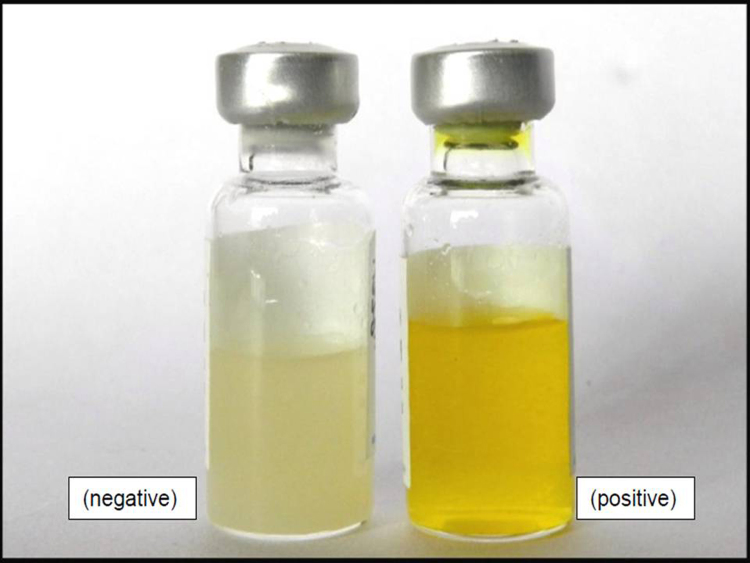
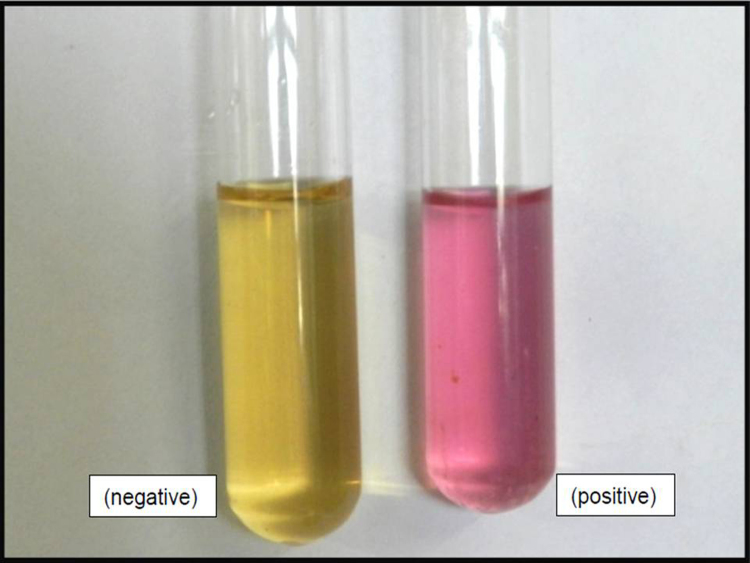
Positive reaction: Development of yellow color within five minutes (Fig. 1).
-
➢
Negative reaction: No development of yellow color within five minutes. Reagent solution remains colorless.
-
➢
Positive control: Transfer content of Part A (1 ml) to Part B (1 ml). Use this as a reagent solution for further test.
-
➢
Transfer 1 ml of R055 Reagent P to reagent solution (Part A+Part B) using syringe.
-
➢
Observe for development of yellow color within five minutes.
-
➢
Negative Control: Transfer content of Part A (1 ml) to part B (1 ml). Use this as a reagent solution for further test.
-
➢
Transfer 1 ml of sterile distilled water or saline into reagent solution (Part A + Part B) using syringe.
-
➢
Color of solution remains colorless after five minutes.
Fig. 1.
Niacin accumulation test.
2.2. Arylsulfatase test
-
•
Principle: Arylsulfatase is an enzyme that splits free phenolphthalein from the tripotassium salt of phenolphthalein disulfite. The test for the identification of Mycobacterium species is performed in a tube containing a substrate of phenolphthalein. After three (or fourteen) days of incubation of a subculture of the isolate to be tested, the appearance of pink color after addition of sodium carbonate indicates a positive reaction.
-
•
Materials: Wayne Sulfatase Agar Base (M1059; HiMedia Laboratories, Mumbai).
-
•
Procedure:
-
➢
Inoculate each tube of substrate with the test organism.
-
➢
Incubate the tube for three days (for Rapid Growers) or fourteen days (for Slow Growers) at 35 °C in the non CO2 incubator.
-
➢
Following incubation, add 1 ml of 2 N sodium carbonate and observe for color change.
-
•
Interpretation: Visually observe for color change from pale pink to deep red. The lack of color change indicates a negative reaction. False negative results can be due to cultures that are too old.
2.3. Nitrate reduction test
-
•
Principle: Mycobacteria producing nitrate reductase are capable of catalyzing the reduction of nitrate to nitrite. In the reaction, oxygen is extracted from nitrate according to the formula NO3 + 2e- + 2 H → NO2- + H2O. The produced nitrite is detected by the addition of α-naphthalamine and sulfanilic acid, which form the red diazonium dye, p-sulfobenzene-azo-α-naphthalamine.
-
•
Materials: Nitrate Reduction Test Kit for Mycobacteria (K043; HiMedia Laboratories, Mumbai) which contains:
-
➢
R056, Nitrate buffer in glass tube for Mycobacteria
-
➢
R060, Nitrate reagent for Mycobacteria
-
•
Procedure: The test is done with actively growing cultures that have been incubated for three to five weeks.
-
➢
A loopful of growth is emulsified aseptically in R056, Nitrate buffer and mixed well.
-
➢
Incubate at 37 °C for two hours.
-
➢
Acidify the buffer by adding two drops of 0.1 N HCl.
-
➢
Add two drops of rehydrated Nitrate reagent, R060 (rehydration is done by adding 5 ml sterile distilled water to R060) in above preparation, R056 under aseptic conditions.
-
•
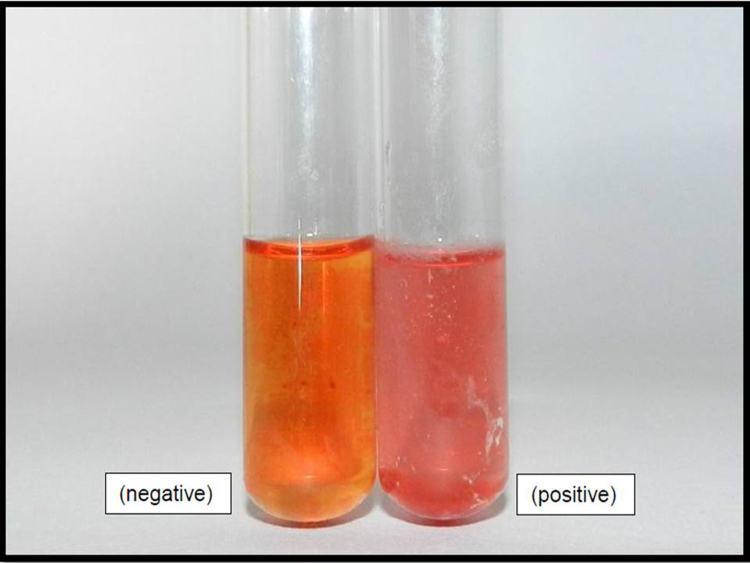
Interpretation: observe for the formation of red color (Fig. 2). Interpret the results in 30–60 s only. Negative test is indicated by no change in color.
Fig. 2.
Nitrate reduction test.
2.4. Catalase test
-
•
Principle: Catalase enzyme splits hydrogen peroxide into oxygen and water. The released oxygen is released as bubbles. Some forms of catalase are inactivated by heating at 68 °C for 20 min. The hydrogen peroxide used here is 30% concentration in 10% Tween-80 (detergent). The detergent helps to disperse the clumped hydrophobic bacteria into individual bacilli, thus maximizing the detection of catalase.
-
•
Materials:
-
➢
LJ deeps (LJ media is prepared and dispensed in tubes of 20 × 150 mm and coagulated in vertical position)
-
➢
Tween-peroxide solution (prepared by mixing equal volumes of 30% H2O2 and 10% Tween-80 immediately before use)
-
➢
Phosphate buffer (0.067 M)
-
•
Procedure:
-
➢
Inoculate LJ deeps with the test organism and incubate at 37 °C for two weeks
-
•
For thermo-stable catalase:
-
➢
Add 0.5 ml of sterile phosphate buffer in test tubes.
-
➢
Inoculate separate test tubes for separate organisms with a loopful of growth and emulsify thoroughly.
-
➢
Incubate the tube in a 68 °C water bath exactly for 20 min.
-
➢
Remove the tubes from water bath and cool to room temperature.
-
➢
Add 0.5 ml of freshly prepared tween-peroxide reagent.
-
➢
Allow the tubes to sit at room temperature for 20 min without shaking.
-
➢
Visually observe the evolution of bubbles.
-
•
Semiquantitative catalase test:
-
➢
To the inoculated LJ deeps add 1 ml of freshly prepared tween-peroxide reagent.
-
➢
Allow the test to sit at room temperature for five minutes.
-
➢
Measure the column of bubbles.
-
•
Interpretation:
-
➢
For thermo-stable catalase: evolution of bubbles indicate a positive test
-
➢
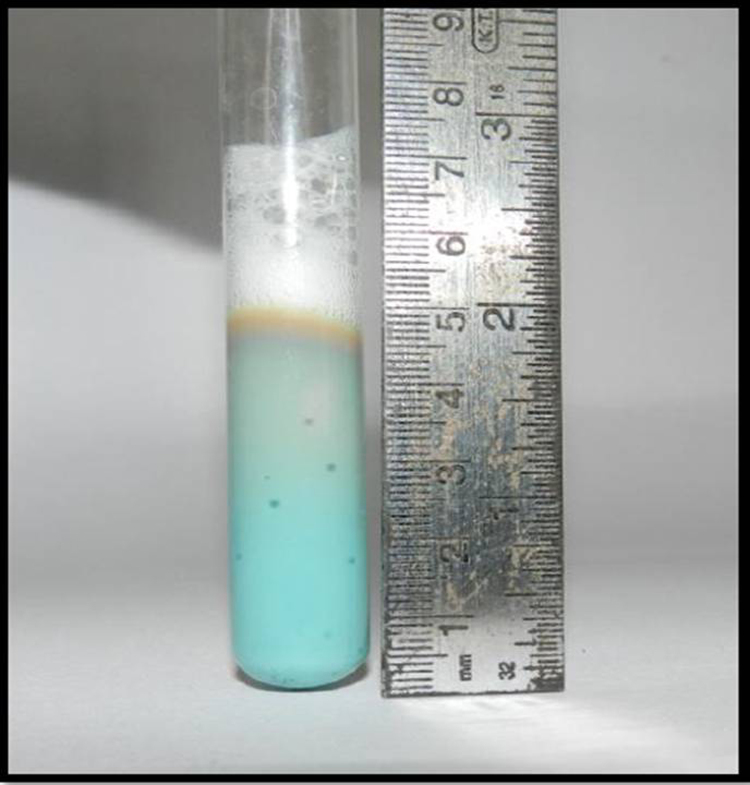
For Semiquantitative catalase test (Fig. 3, Fig. 4): measure the height of column of bubbles
-
➢
≥ 45 mm: High catalase reaction
-
➢
< 45 mm: Low catalase reaction
Fig. 3.
High catalase test (≥ 45 mm).
Fig. 4.
Low catalase test (< 45 mm).
2.5. Hydrolysis of polyoxyethylene monooleate or “Tween-80″
-
•
Principle: Some Mycobacterium species possess an enzyme that releases oleic acid from Tween-80. The color change from amber to pink is due to hydrolysis of Tween-80, which modifies the optical rotation of light passing through the substrate.
-
•
Materials:
-
➢
Phosphate buffer 0.067 M pH 7.0
-
➢
Add the following, in order, to 100 ml of phosphate buffer: 0.5 ml of Tween-80 and 2 ml of a 0.1% aqueous solution of neutral red. Dispense 2 ml into screw cap tubes. Autoclave for 15 min at 121 °C. The substrate should be amber after autoclaving. Store in the dark in the refrigerator for no more than two weeks.
-
•
Procedure: Inoculate the tubes with the organisms from a culture two weeks old. Make a heavy inoculums by picking up the colonies with a swab. Incubate at 37 °C in dark.
-
•
Interpretation: Observe after 24 h. If negative, read again at five and ten days. Compare the color of the liquid with that in the control tubes.
-
➢
Positive test is indicated by a change of color from amber to pink or red. If no change of color, it is negative (Fig. 5).
-
•
NOTE: it is necessary that the medium changes color. If colonies are red, but the medium remains amber, the test is reported as negative.
Fig. 5.
Tween-80 hyrolysis test.
2.6. Citrate utilization
-
•
Principle: Sodium citrate is a salt of citric acid, a simple organic compound found as one of the metabolites in the Krebs cycle. Some bacteria can obtain energy by using citrate as the sole source of carbon. This is an important test for the identification of many bacterial species and differentiation of Rapid Growers. Any medium used to detect citrate utilization by test bacteria must be devoid of protein and carbohydrates as sources of carbon. The test medium contains sodium citrate as the sole source of carbon and ammonium phosphate as the sole source of nitrogen. The bacteria that can utilize citrate can also extract nitrogen from the ammonium salt, with the production of ammonia, leading to alkalinisation of the medium thereby turning the bromothymol blue indicator to blue.
-
•
Materials: Simmons citrate media.
-
•
Procedure: A colony is picked from growth on LJ medium and inoculated as a single streak on the slant surface of the citrate agar tube. The tube is incubated at 35 °C for up to seven days
-
•
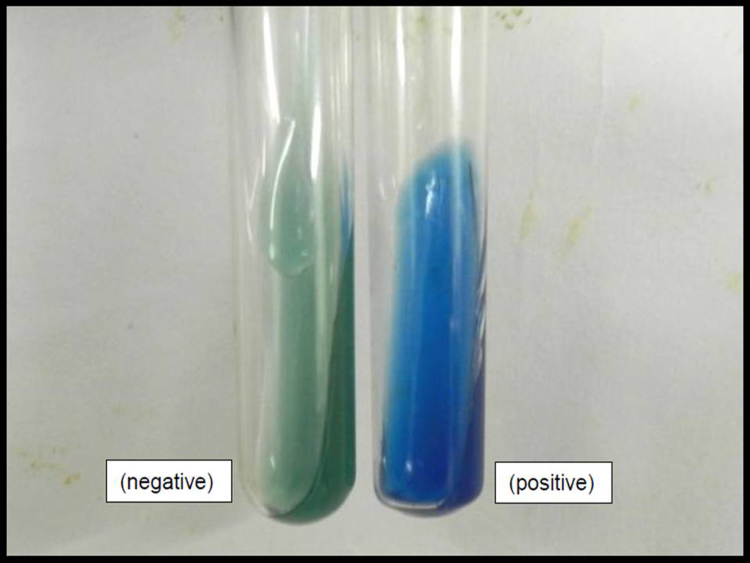
Interpretation: Development of deep blue color is representative of a positive test. A positive test may also be read without a blue color if there is visible colony growth along the inoculation streak line; which is possible because for growth to be visible, the organism must enter the log phase, possible only if carbon and nitrogen have been assimilated (Fig. 6).
Fig. 6.
Citrate utilization test.
2.7. Iron uptake from the medium
-
•
Principle: The ability certain mycobacteria to take up iron from an inorganic iron containing reagent in the culture medium.
-
•
Materials:
-
➢
Two week old culture.
-
➢
20% ferric ammonium citrate (prepared by dissolving 20 g of ferric ammonium citrate to 100 ml deionised water and autoclaving).
-
•
Procedure:
-
➢
Add as many drops of sterile 20% ferric ammonium citrate as there are millilitres of media to the bottle (for example, add 15 drops of 20% ferric ammonium citrate for 15 ml of LJ media).
-
➢
Incubate the slants at 30 °C for up to three weeks.
-
•
Interpretation: Visually examine the surface of slants for the presence of dark rust brown colored colonies (Fig. 7).
Fig. 7.
Test for iron uptake from the medium (dark brown colonies).
2.8. Urea hydrolysis
-
•
Principle: Many Mycobacterium species possess urease enzyme that hydrolyzes urea to form carbon dioxide and ammonia. The ammonia released results in the alkalinisation and an increase in the pH of the medium turning the indicator pink.
-
•
Materials: Urea broth which contains:
Base –
-
➢
Peptone 1 g
-
➢
NaCl 5 g
-
➢
KH2PO4 2 g
-
➢
Glucose 1 g
-
➢
Phenol red (0.4% in 5% alcohol) 3 ml
-
➢
Distilled water 1 L
-
➢
Final pH = 7
To 4.5 ml base, 0.5 ml of 20% urea solution is added
-
•
Procedure:
-
➢
Inoculate each tube with a loopful of growth from an actively growing culture and emulsify thoroughly.
-
➢
Incubate at 35 °C for five days.
-
•
Interpretation: Visually examine the tubes. Color change from yellow to pink or red indicates a positive reaction. No color change is a negative reaction (Fig. 8).
Fig. 8.
Urea hydrolysis test.
2.9. Growth in the presence of 5% NaCl
-
•
Principle: Ability of the mycobacterial species to grow in the presence of 5% NaCl in LJ medium.
-
•
Materials:
-
➢
LJ with 5% NaCl in slants
-
➢
LJ without 5% NaCl in slants
-
•
Procedure:
-
➢
Make a 1 McFarland standard suspension of the test organism and inoculate 0.1 ml each in LJ with and without 5% NaCl.
-
➢
Incubate the media with caps loose at 30 °C for a week.
-
➢
Interpretation: record the test positive when there is growth in both the bottles and negative if growth is only in LJ without 5% NaCl. Repeat the test if there is no growth in any of the bottles.
2.10. Growth in MacConkey agar without crystal violet
-
•
Principle: The ability to grow on MacConkey agar formulated without crystal violet.
-
•
Materials: MacConkey agar without crystal violet
-
•
Procedure:
-
➢
Inoculate a fresh MacConkey agar plate with the test organism from a week old growth on LJ media.
-
➢
Incubate at 30 °C for 11 days.
-
•
Interpretation: Observe MacConkey agar for growth at five and 11 days. The positive test organism will show growth along the entire streak area and possibly a color change in the medium in five to 11 days. The absence of growth indicates a negative test.
2.11. Tellurite reduction
-
•
Principle: This test is based on the ability of certain mycobacteria to reduce tellurite salts to metallic tellurium forming a black precipitate.
-
•
Materials:
-
➢
7H9 medium.
-
➢
0.2% solution of potassium tellurite.
-
•
Procedure:
-
➢
Inoculate 7H9 medium with the test organism and incubate at 37 °C for seven days.
-
➢
After day seven, add two drops of 0.2% solution of potassium tellurite and re-incubate at 37 °C for three more days. For some species, incubation maybe required for up to nine days.
-
•
Interpretation:
-
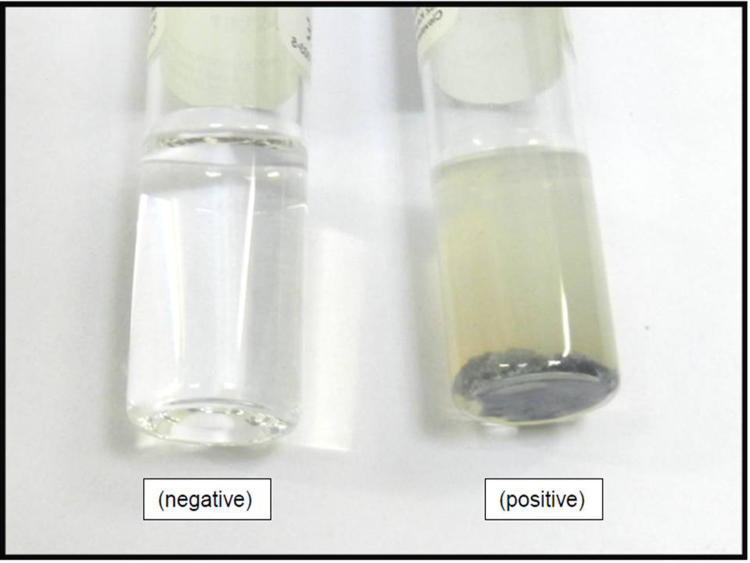
➢
Formation of black metallic precipitate indicates a positive test (Fig. 9).
-
➢
Brown discoloration is considered negative.
Fig. 9.
Tellurite reduction test.
3. Conclusion
In this review, the authors have tried to explain minimum number of tests required to differentiate most commonly isolated species of NTM. Summary of the same is mentioned in Table 1. By explaining the procedures in a lucid step-by-step manner, the authors hope that this review will cater the needs of faculty, students and technicians alike when working with NTM. This text should be supplemented with books on the subject for detailed description of specific organisms. Phenotypic methods are not a replacement of molecular methods and are time consuming [45]. It is suggested that molecular methods should be used when urgent diagnosis is needed and for the confirmation of atypical strains.
Table 1.
Biochemical characteristics of commonly isolated NTM.
| S. No. | Biochemical reaction | Positive | Negative |
|---|---|---|---|
| 1. | Niacin accumulation test | M. simiae, M. chelonae (certain strains) | M. avium, M. intracellulare, M. fortuitum and other NTM |
| 2. | Arylsufatase test | M. fortuitum, M. chelonae, M. abscessus, M. ulcerans, M. xenopi | M. avium, M. intracellulare, M. smegmatis, M. kansasii, M. simiae, M. szulgai, M. scrofulaceum, M. gordonae |
| 3. | Nitrate reduction test | M. ulcerans, M. szulgai, M. fortuitum, M. smegmatis, M. kansasii | M. avium, M. intracellulare, M. chelonae, M. abscessus, M. ulcerans, M. simiae, M. scrofulaceum, M. gordonae, M. xenopi |
| 4. | Thermostable catalase | M. fortuitum, M. chelonae, M. abscessus, M. ulcerans, M. szulgai, M. kansasii, M. simiae, M. scrofulaceum, M. gordonae, M. smegmatis, M. xenopi | M. marinum, M. avium, M. intracellulare |
| 5. | High catalase | M. fortuitum, M. chelonae, M. abscessus, M. smegmatis, M. kansasii, M. marinum, M. ulcerans, M. simiae, M. szulgai, M. scrofulaceum, M. gordonae | -nil- |
| 6. | Low catalase | M. xenopi, M. avium, M. intracellulare | |
| 7. | Hydrolysis of Tween-80 | M. kansasii, M. marinum, M. gordonae, M. fortuitum, M. smegmatis | M. avium, M. intracellulare, M. ulcerans, M. scrofulaceum, M. xenopi |
| 8. | Citrate utilization | M. chelonae, M. smegmatis | M. fortuitum, M. abscessus |
| 9. | Iron uptake from the medium | M. fortuitum, M. smegmatis | M. chelonae, M. ulcerans, M. kansasii, M. marinum, M. simiae, M. szulgai, M. scrofulaceum, M. gordonae, M. xenopi, M. avium, M. intracellulare, M. abscessus |
| 10. | Urea hydrolysis | M. kansasii, M. marinum, M. simiae, M. szulgai, M. scrofulaceum, M. fortuitum, M. chelonae, M. abscessus | M. avium, M. intracellulare, M. gordonae, M. xenopi |
| 11. | Growth in presence of 5% NaCl | M. fortuitum, M. abscessus, M. smegmatis | M. gordonae, M. ulcerans, M. kansasii, M. marinum, M. simiae, M. szulgai, M. scrofulaceum, M. xenopi, M. avium, M. intracellulare, M. chelonae |
| 12. | Growth in MacConkey agar without crystal violet | M. fortuitum, M. abscessus | M. ulcerans, M. kansasii, M. marinum, M. simiae, M. szulgai, M. scrofulaceum, M. gordonae, M. xenopi, M. chelonae |
| 13. | Tellurite reduction | M. avium, M. intracellulare, M. simiae, M. fortuitum, M. abscessus, M. chelonae, M. xenopi (9 days), M. scrofulaceum (9 days) | M. ulcerans, M. kansasii, M. marinum, M. gordonae, |
Conflicts of interest
None to declare
Contributor Information
Gurpreet S. Bhalla, Email: gsbmicrobiology@gmail.com.
Manbeer S. Sarao, Email: manbir.sarao@gmail.com.
Dinesh Kalra, Email: docdkk@yahoo.com.
Kuntal Bandyopadhyay, Email: bandykuntal@gmail.com.
Arun Ravi John, Email: arun_medico2003@yahoo.co.in.
References
- 1.Noe R., Cohen A.L., Lederman E., Gould L.H., Alsdurf H., Vranken P. Skin disorders among construction workers following Hurricane Katrina and Hurricane Rita: an outbreak investigation in New Orleans, Louisiana. Arch. Dermatol. 2007;143(11):1393–1398. doi: 10.1001/archderm.143.11.1393. [DOI] [PubMed] [Google Scholar]
- 2.Appelgren P., Farnebo F., Dotevall L., Studahl M., Jonsson B., Petrini B. Late-onset posttraumatic skin and soft-tissue infections caused by rapid-growing mycobacteria in tsunami survivors. Clin. Infect. Dis. 2008;47(2):e11–e16. doi: 10.1086/589300. [DOI] [PubMed] [Google Scholar]
- 3.De Groote M.A., Huitt G. Infections due to rapidly growing mycobacteria. Clin. Infect. Dis. 2006;42(12):1756–1763. doi: 10.1086/504381. [DOI] [PubMed] [Google Scholar]
- 4.Wallace R.J., Jr. Recent changes in taxonomy and disease manifestations of the rapidly growing mycobacteria. Eur. J. Clin. Microbiol. Infect. Dis. 1994;13(11):953–960. doi: 10.1007/BF02111497. [DOI] [PubMed] [Google Scholar]
- 5.Wallace R.J., Jr., Swenson J.M., Silcox V.A., Good R.C., Tschen J.A., Stone M.S. Spectrum of disease due to rapidly growing mycobacteria. Rev. Infect. Dis. 1983;5(4):657–679. doi: 10.1093/clinids/5.4.657. [DOI] [PubMed] [Google Scholar]
- 6.Simons S., van Ingen J., Hsueh P.R., Van Hung N., Dekhuijzen P.N., Boeree M.J. Nontuberculous mycobacteria in respiratory tract infections, eastern Asia. Emerg. Infect. Dis. 2011;17(3):343–349. doi: 10.3201/eid1703100604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Taylor J.L., Palmer S.M. Mycobacterium abscessus chest wall and pulmonary infection in a cystic fibrosis lung transplant recipient. J. Heart Lung Transplant. 2006;25(8):985–988. doi: 10.1016/j.healun.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 8.da Costa A.R., Lopes M.L., Leao S.C., Schneider M.P., de Sousa M.S., Suffys P.N. Molecular identification of rapidly growing mycobacteria isolates from pulmonary specimens of patients in the State of Para, Amazon region, Brazil. Diagn. Microbiol. Infect. Dis. 2009;65(4):358–364. doi: 10.1016/j.diagmicrobio.2009.08.003. [DOI] [PubMed] [Google Scholar]
- 9.Alcaide F., Esteban J. [Cutaneous and soft skin infections due to non-tuberculous mycobacteria] Enferm. Infecc. Microbiol. Clin. 2010;28(Suppl 1):46–50. doi: 10.1016/S0213-005X(10)70008-2. [DOI] [PubMed] [Google Scholar]
- 10.Piersimoni C., Scarparo C. Extrapulmonary infections associated with nontuberculous mycobacteria in immunocompetent persons. Emerg. Infect. Dis. 2009;15(9):1351–1358. doi: 10.3201/eid1509.081259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ingram C.W., Tanner D.C., Durack D.T., Kernodle G.W., Jr., Corey G.R. Disseminated infection with rapidly growing mycobacteria. Clin. Infect. Dis. 1993;16(4):463–471. doi: 10.1093/clind/16.4.463. [DOI] [PubMed] [Google Scholar]
- 12.Wallace R.J., Jr., Musser J.M., Hull S.I., Silcox V.A., Steele L.C., Forrester G.D. Diversity and sources of rapidly growing mycobacteria associated with infections following cardiac surgery. J. Infect. Dis. 1989;159(4):708–716. doi: 10.1093/infdis/159.4.708. [DOI] [PubMed] [Google Scholar]
- 13.Muthusami J.C., Vyas F.L., Mukundan U., Jesudason M.R., Govil S., Jesudason S.R. Mycobacterium fortuitum: an iatrogenic cause of soft tissue infection in surgery. ANZ J. Surg. 2004;74(8):662–666. doi: 10.1111/j.1445-1433.2004.03018.x. [DOI] [PubMed] [Google Scholar]
- 14.Kannaiyan K., Ragunathan L., Sakthivel S., Sasidar A.R., Muralidaran, Venkatachalam G.K. Surgical site infections due to rapidly growing mycobacteria in puducherry, India. J. Clin. Diagn. Res. 2015;9(3):DC05–DC08. doi: 10.7860/JCDR/2015/10572.5638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Verghese S., Agrawal P., Benjamin S. Mycobacterium chelonae causing chronic wound infection and abdominal incisional hernia. Indian J. Pathol. Microbiol. 2014;57(2):335–337. doi: 10.4103/0377-4929.134736. [DOI] [PubMed] [Google Scholar]
- 16.Chaudhuri S., Sarkar D., Mukerji R. Diagnosis and management of atypical mycobacterial infection after laparoscopic surgery. Indian J. Surg. 2010;72(6):438–442. doi: 10.1007/s12262-010-0164-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Duarte R.S., Lourenco M.C., Fonseca Lde S., Leao S.C., Amorim Ede L., Rocha I.L. Epidemic of postsurgical infections caused by Mycobacterium massiliense. J. Clin. Microbiol. 2009;47(7):2149–2155. doi: 10.1128/JCM.00027-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wallace R.J., Jr., Brown B.A., Onyi G.O. Skin, soft tissue, and bone infections due to Mycobacterium chelonae chelonae: importance of prior corticosteroid therapy, frequency of disseminated infections, and resistance to oral antimicrobials other than clarithromycin. J. Infect. Dis. 1992;166(2):405–412. doi: 10.1093/infdis/166.2.405. [DOI] [PubMed] [Google Scholar]
- 19.Kothavade R.J., Dhurat R.S., Mishra S.N., Kothavade U.R. Clinical and laboratory aspects of the diagnosis and management of cutaneous and subcutaneous infections caused by rapidly growing mycobacteria. Eur. J. Clin. Microbiol Infect. Dis. 2013;32(2):161–188. doi: 10.1007/s10096-012-1766-8. [DOI] [PubMed] [Google Scholar]
- 20.Regnier S., Cambau E., Meningaud J.P., Guihot A., Deforges L., Carbonne A. Clinical management of rapidly growing mycobacterial cutaneous infections in patients after mesotherapy. Clin. Infect. Dis. 2009;49(9):1358–1364. doi: 10.1086/606050. [DOI] [PubMed] [Google Scholar]
- 21.Lee W.J., Kang S.M., Sung H., Won C.H., Chang S.E., Lee M.W. Non-tuberculous mycobacterial infections of the skin: a retrospective study of 29 cases. J. Dermatol. 2010;37(11):965–972. doi: 10.1111/j.1346-8138.2010.00960.x. [DOI] [PubMed] [Google Scholar]
- 22.Wang H., Jin P., Wu Q. Disseminated cutaneous infection with Mycobacterium abscessus in a patient with a low CD4+ T cell count. Eur. J. Dermatol. 2008;18(3):337–340. doi: 10.1684/ejd.2008.0400. [DOI] [PubMed] [Google Scholar]
- 23.Uslan D.Z., Kowalski T.J., Wengenack N.L., Virk A., Wilson J.W. Skin and soft tissue infections due to rapidly growing mycobacteria: comparison of clinical features, treatment, and susceptibility. Arch. Dermatol. 2006;142(10):1287–1292. doi: 10.1001/archderm.142.10.1287. [DOI] [PubMed] [Google Scholar]
- 24.Kang G.C., Gan A.W., Yam A., Tan A.B., Tay S.C. Mycobacterium abscessus hand infections in immunocompetent fish handlers: case report. J. Hand Surg. Am. 2010;35(7):1142–1145. doi: 10.1016/j.jhsa.2010.04.015. [DOI] [PubMed] [Google Scholar]
- 25.Kullavanijaya P., Rattana-Apiromyakij N., Sukonthapirom-Napattalung P., Sirimachand S., Duangdeeden I. Disseminated mycobacterium chelonae cutaneous infection: recalcitrant to combined antibiotic therapy. J. Dermatol. 2003;30(6):485–491. doi: 10.1111/j.1346-8138.2003.tb00421.x. [DOI] [PubMed] [Google Scholar]
- 26.Quinones C., Ramalle-Gomara E., Perucha M., Lezaun M.E., Fernandez-Vilarino E., Garcia-Morras P. An outbreak of mycobacterium fortuitum cutaneous infection associated with mesotherapy. J. Eur. Acad. Dermatol. Venereol. 2010;24(5):604–606. doi: 10.1111/j.1468-3083.2009.03461.x. [DOI] [PubMed] [Google Scholar]
- 27.Panossian A., Cohen M.J., Posalski I. Upper extremity mycobacterium chelonae cutaneous infection. Plast. Reconstr. Surg. 2011;127(6):163e–165ee. doi: 10.1097/PRS.0b013e318213a27b. [DOI] [PubMed] [Google Scholar]
- 28.Haas S.R., Hodge M.B., Duncan R.A. Cushing's syndrome presenting as disseminated cutaneous mycobacterium chelonae infection. Clin. Infect. Dis. 2001;33(6):e51–e53. doi: 10.1086/322629. [DOI] [PubMed] [Google Scholar]
- 29.Cornelius L., Reddix R., Burchett C., Bond G., Fader R. Cluster of mycobacterium fortuitum prosthetic joint infections. J. Surg. Orthop. Adv. 2007;16(4):196–198. [PubMed] [Google Scholar]
- 30.Wang S.X., Yang C.J., Chen Y.C., Lay C.J., Tsai C.C. Septic arthritis caused by Mycobacterium fortuitum and Mycobacterium abscessus in a prosthetic knee joint: case report and review of literature. Intern. Med. 2011;50(19):2227–2232. doi: 10.2169/internalmedicine.50.5610. [DOI] [PubMed] [Google Scholar]
- 31.Tazawa S., Marumo K., Higuchi D., Yoshizawa Y. Mycobacterium fortuitum infection caused by the organism in subcutaneous abscess mediated by central venous catheter. Kekkaku. 2006;81(10):609–612. [PubMed] [Google Scholar]
- 32.Pai H.H., Chen W.C., Peng C.F. Isolation of non-tuberculous mycobacteria from hospital cockroaches (Periplaneta americana) J. Hosp. Infect. 2003;53(3):224–228. doi: 10.1053/jhin.2002.1355. [DOI] [PubMed] [Google Scholar]
- 33.Runyon E.H. Anonymous mycobacteria in pulmonary disease. Med. Clin. North Am. 1959;43(1):273–290. doi: 10.1016/s0025-7125(16)34193-1. [DOI] [PubMed] [Google Scholar]
- 34.Runyon E.H. Unclassified mycobacteria. Am. Rev. Respir. Dis. 1960;81:428–429. doi: 10.1164/arrd.1960.81.3.428. [DOI] [PubMed] [Google Scholar]
- 35.Falkinham J.O., 3rd Epidemiology of infection by nontuberculous mycobacteria. Clin. Microbiol. Rev. 1996;9(2):177–215. doi: 10.1128/cmr.9.2.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Brown-Elliott B.A., Wallace R.J., Jr. Clinical and taxonomic status of pathogenic nonpigmented or late-pigmenting rapidly growing mycobacteria. Clin. Microbiol. Rev. 2002;15(4):716–746. doi: 10.1128/CMR.15.4.716-746.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Safranek T.J., Jarvis W.R., Carson L.A., Cusick L.B., Bland L.A., Swenson J.M. Mycobacterium chelonae wound infections after plastic surgery employing contaminated gentian violet skin-marking solution. N. Engl. J. Med. 1987;317(4):197–201. doi: 10.1056/NEJM198707233170403. [DOI] [PubMed] [Google Scholar]
- 38.Domenech P., Menendez M.C., Garcia M.J. Restriction fragment length polymorphisms of 16S rRNA genes in the differentiation of fast-growing mycobacterial species. FEMS Microbiol. Lett. 1994;116(1):19–24. doi: 10.1111/j.1574-6968.1994.tb06669.x. [DOI] [PubMed] [Google Scholar]
- 39.Kusunoki S., Ezaki T. Proposal of Mycobacterium peregrinum sp. nov., nom. rev., and elevation of Mycobacterium chelonae subsp. abscessus (Kubica et al.) to species status: mycobacterium abscessus comb. nov. Int J. Syst. Bacteriol. 1992;42(2):240–245. doi: 10.1099/00207713-42-2-240. [DOI] [PubMed] [Google Scholar]
- 40.Pitulle C., Dorsch M., Kazda J., Wolters J., Stackebrandt E. Phylogeny of rapidly growing members of the genus Mycobacterium. Int. J. Syst. Bacteriol. 1992;42(3):337–343. doi: 10.1099/00207713-42-3-337. [DOI] [PubMed] [Google Scholar]
- 41.Han X.Y., De I., Jacobson K.L. Rapidly growing mycobacteria: clinical and microbiologic studies of 115 cases. Am. J. Clin. Pathol. 2007;128(4):612–621. doi: 10.1309/1KB2GKYT1BUEYLB5. [DOI] [PubMed] [Google Scholar]
- 42.Swenson J.M., Wallace R.J., Jr., Silcox V.A., Thornsberry C. Antimicrobial susceptibility of five subgroups of mycobacterium fortuitum and mycobacterium chelonae. Antimicrob. Agents Chemother. 1985;28(6):807–811. doi: 10.1128/aac.28.6.807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cavusoglu C., Gurpinar T., Ecemis T. Evaluation of antimicrobial susceptibilities of rapidly growing mycobacteria by Sensititre RAPMYCO panel. New Microbiol. 2012;35(1):73–76. [PubMed] [Google Scholar]
- 44.Yu X.L., Lu L., Chen G.Z., Liu Z.G., Lei H., Song Y.Z. Identification and characterization of non-tuberculous mycobacteria isolated from tuberculosis suspects in Southern-central China. PLoS One. 2014;9(12):e114353. doi: 10.1371/journal.pone.0114353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Springer B., Stockman L., Teschner K., Roberts G.D., Bottger E.C. Two-laboratory collaborative study on identification of mycobacteria: molecular versus phenotypic methods. J. Clin. Microbiol. 1996;34(2):296–303. doi: 10.1128/jcm.34.2.296-303.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]