Abstract
Objectives
To investigate the sex-specific prevalence of atrial fibrillation (AF), including subclinical AF found by screening in a general population aged 63–65 years. The prevalence of cardiovascular risk factors and their association with AF will also be investigated.
Design
Cross-sectional analysis of an observational, prospective, longitudinal, population-based cohort study.
Setting
General population in Akershus county, Norway.
Participants
Women and men born in 1950. We included 3706 of 5827 eligible individuals (63.6%); 48.8% were women.
Methods
All participants underwent extensive cardiovascular examinations, including 12-lead ECG. History of AF and other cardiovascular diseases were self-reported. Subsequent validation of all reported or detected AF diagnoses was performed.
Results
Mean age was 63.9±0.7 years. Prevalence of ECG-verified AF was 4.5% (women 2.4%, men 6.4%; p<0.001), including screen-detected AF in 0.3% (women 0.1%, men 0.6%; p<0.01). Hypertension was found in 62.0% (women 57.8%, men 66.0%; p<0.001). Overweight or obesity was found in 67.6% (women 59.8%, men 74.9%; p<0.001). By multivariate logistic regression, risk factors associated with AF were height (OR 1.67 per 10 cm; 95% CI 1.26 to 2.22; p<0.001), weight (OR 1.15 per 10 kg; 95% CI 1.01 to 1.30; p=0.03), hypertension (OR 2.49; 95% CI 1.61 to 3.86; p<0.001), heart failure (OR 3.51; 95% CI 1.71 to 7.24; p=0.001), reduced estimated glomerular filtration rate (OR 2.56; 95% CI 1.42 to 4.60; p<0.01) and at least one first-degree relative with AF (OR 2.32; 95% CI 1.63 to 3.31; p<0.001), whereas male sex was not significantly associated (OR 1.00; 95% CI 0.59 to 1.68; p=0.99).
Conclusion
In this cohort from the general population aged 63–65 years, we found a higher prevalence of known AF than previously reported below the age of 65 years. The additional yield of single time point screening for AF was low. Body size and comorbidity may explain most of the sex difference in AF prevalence at this age.
Trial registration number
NCT01555411; Results.
Keywords: atrial fibrillation, obesity, cardiovascular risk, prevalence, screening, cardiac epidemiology
Strengths and limitations of this study.
Unselected population-based cohort design inviting all residents in a geographical region born in 1950.
The study was conducted in a completely government-financed healthcare system with equal access for the entire population.
All reported and detected cases of atrial fibrillation (AF) were thoroughly validated.
The study relied on self-reported cardiovascular disease only, and negative responses to AF were not validated.
This report is a cross-sectional analysis of an age cohort study, making comparison to other study settings difficult.
Introduction
The prevalence of atrial fibrillation (AF) is on the rise and this arrhythmia is emerging as a major public health problem due to the associated stroke risk and related costs.1 2 The prevalence in the adult population has been estimated to be 1%–2%, but is probably as high as 2%–3%, based on recent data.1 Previous studies in specific age groups have reported a prevalence of AF of 4.2% among subjects 60–69 years of age.3 The increase in prevalence is most likely due to both ageing of the population and improved survival from other types of cardiovascular disease (CVD). Increased awareness and improved detection of subclinical AF may also be contributing factors.
Screening for AF has received increased attention lately. European guidelines recommend opportunistic screening by pulse palpation or ECG in all patients >65 years of age.4 Despite the emergence of technology for ambulant ECG monitoring, current recommendations are still based on single time point screening by standard ECG, enabling undetected AF to be diagnosed in 1.4% of the population ≥65 years.5 At this age and above, one or more additional risk factors for stroke, according to the CHA2DS2-VASc (Congestive heart failure, Hypertension, Age ≥75 (doubled), Diabetes, Stroke (doubled), Vascular disease, Age 65-74, and Sex (female)) score, provide a strong indication for anticoagulation.4 Hence, subjects with hypertension, diabetes or other risk factors for stroke represent a potential target group for screening for AF.6 Studies have shown that about 50% of incident AF could be attributed to elevated levels of risk factors for AF, of which elevated blood pressure and overweight were the most important contributors.7 This raises the issue of early detection and subsequent ‘upstream’ treatment of these conditions.
The primary objective of this study was to investigate the sex-specific prevalence of self-reported and ECG-validated AF, including subclinical AF found by screening, in a contemporary population-based cohort aged 63–65 years. Secondary objectives were to investigate the prevalence of cardiovascular risk factors and their association with AF.
Methods
Study population
The Akershus Cardiac Examination (ACE) 1950 Study is an observational, longitudinal, population-based cohort study of individuals born in 1950. The identity of all permanent residents of Akershus county born in 1950 were retrieved from the Norwegian Population Registry at the start of the study (n=5827). These were invited by letter and subsequent phone calls. Design and general methodology have been reported previously.8 In this article, we present data from a cross-sectional analysis of the baseline examination, performed in the period September 2012–May 2015.
Study variables
Clinical data included measurements of height, weight, seated blood pressure and 12-lead ECG. Body mass index (BMI) was calculated according to the standard formula (kg/m2), and categorised into overweight (BMI 25.0–29.9 kg/m2) and obesity (BMI ≥30.0 kg/m2). Body surface area (BSA; m2) was calculated by the Mosteller formula.9 A web-based questionnaire for registration of medical history and lifestyle was used. The questionnaire was formulated in the same manner as in previous large Norwegian population studies,10 and participants were urged to ask study personnel at the baseline visit if they were not able to respond adequately to all questions, to ensure high-quality data collection. Daily use of all types of medication was registered according to the Anatomical Therapeutic Chemical Classification System.
Concerning AF, the participants were asked: ‘Have you ever been diagnosed with atrial fibrillation or atrial flutter?’ All self-reported AF were validated according to the following: (1) ECG documentation of AF or atrial flutter according to standard definitions,4 and if such was not available, (2) a solid description of AF or atrial flutter in the medical record (ie, direct current cardioversion or AF ablation procedure). All ECGs and medical records were evaluated by two physicians, of whom one was a cardiologist. Available information in the medical records including ECGs, as well as the study ECG, was used to classify AF as paroxysmal versus persistent/permanent. Participants without history of AF, but in whom AF was detected in the study ECG, were classified as previously undiagnosed AF. Participants also reported any familial AF history among first-degree relatives. For individuals with AF, we calculated the CHA2DS2-VASc stroke risk score. This was based on the presence or history of heart failure, hypertension, diabetes, stroke/transient ischaemic attack (TIA), myocardial infarction, age >65 years and female sex.
Hypertension was defined as the mean (from the second and third of three readings) systolic blood pressure ≥140 mm Hg or mean diastolic blood pressure ≥90 mm Hg, or current use of any antihypertensive medication. The diagnoses of heart failure, myocardial infarction and stroke or TIA were self-reported. Coronary artery disease was defined as self-reported myocardial infarction, percutaneous coronary intervention or coronary artery bypass grafting surgery.
Fasting blood samples were analysed on site and included lipids, blood glucose, haemoglobin A1c (HbA1c) and serum creatinine. The Chronic Kidney Disease Epidemiology Collaboration equation was used to calculate estimated glomerular filtration rate (eGFR).11 Reduced eGFR (eGFR <60 mL/min/1.73 m2), indicative of chronic kidney disease, was reported and used for the analyses. Hypercholesterolaemia was defined as total cholesterol ≥6.2 mmol/L and/or low-density lipoprotein (LDL) ≥4.1 mmol/L and/or use of lipid-lowering medication. Diabetes was defined as a self-reported diagnosis or use of hypoglycaemic medication or elevated glucose tests (both HbA1c ≥6.5% and fasting blood glucose ≥7.0 mmol/L).
Higher education was defined as >12 years of formal education, that is, college/university education at any level. Alcohol consumption, smoking and physical activity were self-reported. Physical activity was classified according to a previously validated model (details provided in online supplementary table 1).12
bmjopen-2018-021704supp001.pdf (457.6KB, pdf)
The data are reported according to the Strengthening the Reporting of Observational Studies in Epidemiology guidelines.13 The study complies with the Declaration of Helsinki, and written informed consent was obtained from all participants.
Statistical analysis
Continuous variables are reported as mean and SD, and Student’s t-test was used for between-group analysis. Continuous variables not normally distributed are reported as median with IQR and analysed with the Mann-Whitney U test. Categorical variables are presented as counts and/or proportions (%) and compared by the χ2 test or Fisher’s exact test as appropriate. Logistic regression analysis was used to assess associations between risk factors and AF. All available known risk factors for AF were selected from univariate analyses based on clinical and statistical significance (p value <0.20). Pearson correlation, as well as multicollinearity statistics, was run between each of the independent variables before inclusion in a multivariate logistic regression model. To assess the robustness of the model, we performed a sensitivity analysis in which all candidate variables were put into the same model. Secondary analyses replacing height and weight with the more commonly used BMI, as well as BSA, were also performed. P values are two-sided and considered significant when <0.05. Cases with missing data were omitted from descriptive statistics of that particular variable. Hence, the reported proportions represent the valid proportions. As for the regression analysis, a complete case analysis was performed. Statistics were performed using IBM SPSS Statistics for Windows, V.24.0 (IBM Corp., Armonk, New York, USA).
Patient and public involvement
The participants of this study represent a large age cohort from the general population. Although there was no public or participants’ involvement in the planning and design of the study, random samples of participants were, during the conduct of the baseline examinations, invited to respond to a questionnaire focusing on how they perceived their participation in the study, and if they had any suggestions to improve the study conduct. Individual study results (blood pressure, cholesterol levels, etc.) were sent to all study participants shortly after their study visit, accompanied by individual advice in case any further follow-up was recommended. All scientific study results are continuously communicated to the participants as well as the general population through local media and our own website www.ace1950.no. Newsletters with updated study information have also been sent to all study participants by mail. A ’participant advisory board' is now currently being formalised, and will be involved in the planning of further follow-up studies of this cohort.
Results
General cohort profile
A total of 3706 participants (from 5827 eligible residents; 63.6% participation rate) were enrolled and examined in the ACE 1950 Study. Women and men were evenly represented, with 1807 (48.8%) women and 1899 (51.2%) men (participation rate 63.7% among women, 63.5% among men; p=0.86). Akershus University Hospital enrolled 2473 participants, and Bærum Hospital (Vestre Viken Hospital Trust) 1233 participants, within their respective catchment areas. The majority were of Caucasian ethnicity (3624; 97.8%). All participants were born in 1950, and the mean age at inclusion was 63.9±0.7 years.
Baseline characteristics are presented in table 1. The prevalence of CVD and cardiovascular risk factors were generally higher in men than in women, with the exception that a higher number of women had hypercholesterolaemia (p<0.01). There were no sex differences in reported daily smoking (15.3% of women vs 13.7% of men; p=0.19). As shown in table 1, the majority of the cohort was overweight or obese. Obesity was found in 22.6% (24.1% of men, 21.1% of women; p=0.03).
Table 1.
Baseline characteristics of the ACE 1950 cohort
| Total n=3706 |
Men n=1899 |
Women n=1807 |
P value | |
| Age | 63.9±0.7 | 63.9±0.7 | 63.9±0.6 | 0.34 |
| Caucasian ethnicity | 97.8 | 97.4 | 98.2 | 0.08 |
| Higher education | 46.4 | 50.2 | 42.3 | <0.001 |
| BMI | 27.2±4.4 | 27.7±4.0 | 26.6±4.8 | <0.001 |
| Overweight/obesity (BMI ≥25) | 67.6 | 74.9 | 59.8 | <0.001 |
| Systolic blood pressure, mm Hg | 138±19 | 139±18 | 137±20 | 0.02 |
| Diastolic blood pressure, mm Hg | 77±10 | 80±10 | 74±9 | <0.001 |
| Hypertension | 62.0 | 66.0 | 57.8 | <0.001 |
| Myocardial infarction | 4.3 | 7.4 | 0.9 | <0.001 |
| Coronary heart disease | 7.1 | 11.5 | 2.4 | <0.001 |
| Heart failure | 1.6 | 2.3 | 0.9 | 0.001 |
| Atrial fibrillation | 4.5 | 6.4 | 2.4 | <0.001 |
| Stroke/TIA | 3.8 | 5.0 | 2.5 | <0.001 |
| Diabetes mellitus | 8.6 | 11.6 | 5.4 | <0.001 |
| Reduced eGFR | 3.9 | 3.4 | 4.3 | 0.16 |
| Hypercholesterolaemia | 52.6 | 50.6 | 54.7 | 0.01 |
| COPD | 7.2 | 6.9 | 7.4 | 0.60 |
| Obstructive sleep apnoea | 6.2 | 9.0 | 3.2 | <0.001 |
| Current daily smoking | 14.5 | 13.7 | 15.3 | 0.19 |
| Current or former daily smoking | 61.8 | 62.2 | 61.5 | 0.64 |
| Daily moist tobacco (‘snus’) | 2.2 | 3.8 | 0.4 | <0.001 |
| Alcohol | ||||
| >14 standard drinks/week | 2.8 | 4.3 | 1.2 | <0.001 |
| ‘Binge drinking’ | 16.3 | 25.3 | 6.9 | <0.001 |
| Physical activity level | ||||
| Inactive | 19.1 | 22.5 | 15.4 | <0.001 |
| Low | 19.7 | 19.7 | 19.7 | 0.98 |
| Medium | 40.3 | 34.7 | 46.1 | <0.001 |
| High | 21.0 | 23.1 | 18.8 | 0.001 |
| Medication | ||||
| Any cardiovascular medication (ATC C) | 46.1 | 50.0 | 41.9 | <0.001 |
| Diuretics (ATC C03) | 3.1 | 2.9 | 3.3 | 0.52 |
| Beta blockers (ATC C07) | 13.4 | 16.7 | 9.9 | <0.001 |
| Calcium channel blockers (ATC C08) | 8.1 | 9.7 | 6.4 | <0.001 |
| Agents acting on the renin-angiotensin system (ATC C09) | 26.9 | 30.6 | 23.0 | <0.001 |
| Lipid-modifying agents (ATC C10) | 26.2 | 29.6 | 22.5 | <0.001 |
Categorical variables are reported as percentages. Continuous variables are presented as mean±SD. P values indicate difference between sexes. Higher education: ≥12 years of formal education.
‘Binge drinking’ is defined as heavy episodic drinking (at least five standard drinks of alcohol) at least once per month. Details for classification of physical activity level are provided in online supplementary table 1. Medication: self-reported cardiovascular medication according to ATC classification.
ATC, Anatomical Therapeutic Chemical; BMI, body mass index (kg/m2); COPD, chronic obstructive pulmonary disease; eGFR, estimated glomerular filtration rate; TIA, transient ischaemic attack.
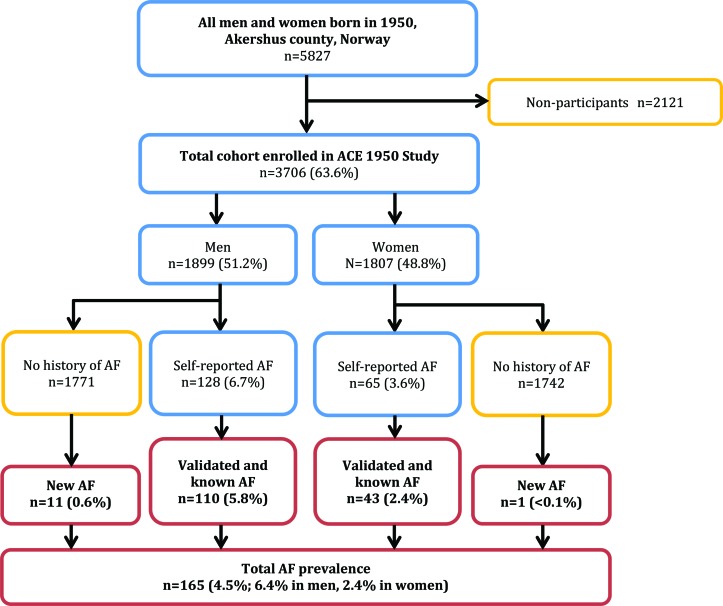
Prevalence of known and unknown AF
A flowchart illustrating the validation of AF is shown in figure 1. History of AF was reported by 193 (5.2%) participants. After validation, 153 (4.1%) had a verified AF diagnosis. Hence, the positive predictive value (PPV) of self-reported AF, compared with the direct review of medical records and ECGs, was 79.3%. Previously unknown AF was diagnosed by ECG in 12 (0.3%) participants. The total prevalence of validated AF was 4.5% (n=165; 2.4% among women, 6.4% among men; p<0.001), as shown in figure 1 and table 2. Nine subjects had a history of atrial flutter (or atrial flutter in study ECG), without any previous diagnosis of AF. These were counted as AF. Permanent AF was identified in 48 cases (table 2).
Figure 1.
Flow chart of Akershus Cardiac Examination (ACE) 1950 study population and atrial fibrillation (AF) prevalence.
Table 2.
Prevalence of validated atrial fibrillation (AF) at 63–65 years
| Total, n (%) (n=3706) |
Men, n (%) (n=1899) |
Women, n (%) (n=1807) |
|
| Total AF | 165 (4.5) | 121 (6.4) | 44 (2.4) |
| Paroxysmal AF | 105 (2.8) | 73 (3.9) | 32 (1.8) |
| Persistent/permanent AF | 48 (1.3) | 37 (2.0) | 11 (0.6) |
| Previously undiagnosed AF | 12 (0.3) | 11 (0.6) | 1 (0.1) |
Previously undiagnosed cases were not classified as paroxysmal/persistent as further follow-up was performed in the clinical setting after the baseline visit.
Clinical characteristics of AF
Table 3 shows sex-specific characteristics of individuals with AF compared with the rest of the cohort. Both women and men with AF were significantly taller and heavier than those without AF. Other measures of body size, such as waist and hip circumference, and BSA, were also higher among individuals with AF, regardless of sex. Obesity was found in 41.8% of participants with AF versus 21.7% in unaffected participants (p<0.001). Hypertension, heart failure and reduced eGFR were more prevalent in individuals with AF of both sexes, whereas coronary heart disease was more prevalent only among men with AF. Otherwise, there were only minor sex differences. With regard to level of physical activity, there were no significant differences between the groups.
Table 3.
Clinical characteristics of study population by AF prevalence and sex
| Men | Women | |||||
| AF (n=121) |
Without AF (n=1778) | P value | AF (n=44) |
Without AF (n=1763) |
P value | |
| Height, cm | 180.4±6.7 | 178.8±6.5 | <0.01 | 168.7±7.0 | 165.3±5.9 | <0.001 |
| Weight, kg | 94.0±15.7 | 88.3±13.6 | <0.001 | 79.6±16.5 | 72.8±13.4 | <0.01 |
| BMI | 28.9±4.9 | 27.6±3.9 | <0.01 | 27.9±5.6 | 26.6±4.7 | 0.07 |
| Obesity (BMI ≥30) | 52 (43.0) | 405 (22.8) | <0.001 | 17 (38.6) | 365 (20.7) | <0.01 |
| Waist circumference, cm | 103.4±12.9 | 99.3±11.0 | 0.001 | 93.3±12.7 | 87.7±12.4 | <0.01 |
| Hip circumference, cm | 104.0±9.6 | 101.5±6.8 | <0.01 | 105.5±9.6 | 102.1±9.2 | 0.01 |
| Waist to hip ratio | 0.99±0.08 | 0.97±0.07 | 0.02 | 0.88±0.07 | 0.85±0.08 | 0.04 |
| Body surface area, m2 | 2.16±0.19 | 2.09±0.18 | <0.001 | 1.92±0.22 | 1.82±0.18 | <0.01 |
| Hypertension | 101 (83.5) | 1152 (64.8) | <0.001 | 37 (84.1) | 1007 (57.2) | <0.001 |
| Myocardial infarction | 18 (14.9) | 123 (6.9) | 0.001 | 0 (0) | 17 (1.0) | 0.51 |
| Coronary heart disease | 28 (23.1) | 191 (10.7) | <0.001 | 0 (0) | 44 (2.5) | 0.29 |
| Heart failure | 13 (10.7) | 30 (1.7) | <0.001 | 3 (6.8) | 14 (0.8) | <0.001 |
| Stroke/TIA | 9 (7.4) | 86 (4.8) | 0.20 | 3 (6.8) | 42 (2.4) | 0.06 |
| Diabetes mellitus | 13 (10.7) | 207 (11.6) | 0.76 | 4 (9.1) | 93 (5.3) | 0.27 |
| Reduced eGFR | 11 (9.1) | 54 (3.1) | <0.001 | 5 (11.4) | 73 (4.2) | 0.02 |
| Obstructive sleep apnoea | 15 (12.4) | 156 (8.8) | 0.18 | 3 (6.8) | 54 (3.1) | 0.16 |
| No comorbidity* | 15 (12.4) | 455 (25.6) | 0.001 | 6 (13.6) | 594 (33.7) | <0.01 |
| Hospitalisation last 12 months | 28 (23.1) | 201 (11.3) | <0.001 | 16 (36.4) | 204 (11.6) | <0.001 |
| Current daily smoking | 10 (8.3) | 249 (14.1) | 0.08 | 8 (18.2) | 265 (15.2) | 0.58 |
| Familial AF† | 31 (25.6) | 272 (15.3) | <0.01 | 25 (56.8) | 408 (23.1) | <0.001 |
| Higher education‡ | 61 (50.4) | 889 (50.2) | 0.97 | 18 (40.9) | 745 (42.3) | 0.85 |
| Physical activity level | ||||||
| Inactive | 30 (25.6) | 390 (22.3) | 0.40 | 11 (25.6) | 259 (15.1) | 0.06 |
| Low/medium | 55 (47.0) | 960 (54.9) | 0.10 | 27 (62.8) | 1129 (65.9) | 0.67 |
| High | 32 (27.4) | 399 (22.8) | 0.26 | 5 (11.6) | 325 (19.0) | 0.22 |
| Heart rate§ | 56±8 | 61±10 | <0.001 | 59±8 | 65±10 | <0.01 |
| PQ interval¶ | 185±29 | 175±27 | <0.01 | 182±44 | 165±25 | 0.04 |
| QRS duration¶ | 105±22 | 98±14 | <0.01 | 90±14 | 88±10 | 0.28 |
Categorical variables are reported as counts with percentages in parentheses. Continuous variables are reported as mean±SD. P values indicate difference between AF and non-AF (within each sex).
*No comorbidity: neither hypertension, coronary heart disease, heart failure, stroke, diabetes, reduced eGFR, obstructive sleep apnoea nor obesity.
†Familial AF: self-report of at least one first-degree relative with known AF.
‡Higher education: ≥12 years of formal education.
§Heart rate: beats per minute in 12-lead ECG.
¶PQ interval and QRS duration are reported in ms. For heart rate, PQ interval and QRS duration, all subjects with AF in study ECG were excluded (n=60).
AF, atrial fibrillation; BMI, body mass index, kg/m2; eGFR, estimated glomerular filtration rate; TIA, transient ischaemic attack.
A higher number of both women and men with AF reported a first-degree relative with known AF, compared with the rest of the cohort (33.9% vs 19.2%; p<0.001; table 3). Familial AF was more prevalent in women with AF than in men with AF (56.8% vs 25.6%; p<0.001).
Risk factors for AF
Risk factors associated with AF, assessed by logistic regression, are reported in table 4. In univariate analysis, male sex was associated with increased likelihood of having AF. However, in multivariate analysis, sex was not associated with AF, when adjusting for height, weight and other risk factors. Height, weight, hypertension, heart failure, reduced eGFR and family history of AF were all significantly associated with AF in multivariate analysis. A sensitivity analysis, in which all independent variables were included, did not change the results (see online supplementary table 2). In secondary analyses, height and weight were replaced with BMI or BSA. In these analyses, male sex remained significantly associated with AF, and a strong association to AF was found for both BMI and BSA, while only minor changes were seen for other variables (data not shown).
Table 4.
Risk factors associated with atrial fibrillation (AF)
| Univariate OR (95% CI) |
P value | Multivariate OR (95% CI) |
P value | |
| Male sex | 2.73 (1.92 to 3.87) | <0.001 | 1.00 (0.59 to 1.68) | 0.99 |
| Height per 10 cm | 1.90 (1.59 to 2.28) | <0.001 | 1.67 (1.26 to 2.22) | <0.001 |
| Weight per 10 kg | 1.42 (1.29 to 1.55) | <0.001 | 1.15 (1.01 to 1.30) | 0.03 |
| Hypertension* | 3.27 (2.15 to 4.97) | <0.001 | 2.49 (1.61 to 3.86) | <0.001 |
| Heart failure | 8.53 (4.71 to 15.48) | <0.001 | 3.51 (1.71 to 7.24) | 0.001 |
| Familial AF† | 2.16 (1.55 to 3.02) | <0.001 | 2.32 (1.63 to 3.31) | <0.001 |
| Reduced eGFR | 2.87 (1.66 to 4.95) | <0.001 | 2.56 (1.42 to 4.60) | <0.01 |
| Coronary heart disease | 2.88 (1.88 to 4.41) | <0.001 | 1.56 (0.95 to 2.57) | 0.08 |
| History of stroke/TIA | 2.09 (1.13 to 3.86) | 0.02 | 1.43 (0.74 to 2.78) | 0.29 |
| OSA | 1.94 (1.17 to 3.23) | 0.01 | 1.11 (0.63 to 1.97) | 0.71 |
| Physical activity (low/normal as ref.)‡ | ||||
| Inactive | 1.61 (1.10 to 2.37) | 0.02 | 1.38 (0.92 to 2.07) | 0.12 |
| High level | 1.30 (0.88 to 1.94) | 0.19 | 1.20 (0.80 to 1.81) | 0.38 |
| Diabetes | 1.24 (0.74 to 2.08) | 0.41 | – | – |
| Daily smoking | 0.72 (0.44 to 1.19) | 0.20 | – | – |
| High alcohol consumption§ | 0.81 (0.45 to 2.78) | 0.81 | – | – |
Variables with p<0.20 in univariate logistic regression analysis are included in the multivariate analysis (a complete analysis of all candidate variables are included in online supplementary table 2).
Bold font indicates a significant association in multivariate analysis.
*Hypertension: mean systolic blood pressure ≥140 mm Hg, or mean diastolic blood pressure ≥90 mm Hg, or current use of any antihypertensive medication.
†Familial AF: self-report of at least one first-degree relative with known AF.
‡Physical activity (PA) level: Inactive and high level of PA compared with low/medium PA (combined to one group) as the reference group.
§High alcohol consumption: >14 standard drinks/week (both sexes).
eGFR, estimated glomerular filtration rate; OSA, obstructive sleep apnoea; TIA, transient ischaemic attack.
Stroke risk in AF
The median CHA2DS2-VASc stroke risk score among AF subjects was 1 (IQR 1–2) in men and 2 (IQR 2–2) in women (see online supplementary table 3). In total, 83.6% in the AF group fulfilled our criteria for hypertension. As many as 41.1% of individuals with AF had elevated blood pressure (≥140/≥90 mm Hg) at the ACE 1950 baseline visit, regardless of ongoing treatment. Details of stroke risk and medication in individuals with AF are presented in online supplementary table 3. Furthermore, characteristics of screen-detected AF (n=12) are shown in online supplementary table 4. These individuals were generally low risk; the median CHA2DS2-VASc score was 1 (total range 0–2). However, 75.0% were overweight and 66.7% had hypertension.
Missing data
Basic clinical variables, including height, weight and ECG were available from all 3706 participants, whereas blood pressure was missing in only two participants. Data was missing for <1% of the participants for all reported variables, including all self-reported CVD, except for physical activity in which 2.3% (n=84) had missing data on at least one of three physical activity questions.
Discussion
Principal findings
The key results of this study were that we identified a high prevalence of verified AF, whereas single time point screening by 12-lead ECG identified only 0.3% new cases in an unselected contemporary population aged 63–65 years. Body size and cardiovascular comorbidity, but not sex, were independently associated with prevalent AF at this age.
Strengths and limitations
Strengths of this study include the unselected population-based design and complete, or nearly complete, data on all participants. For example, 12-lead ECGs were available from all 3706 participants. The thorough validation of all self-reported AF cases also strengthens our findings.
Limitations include uncertainty about the accuracy of self-reported CVD. In particular, we believe heart failure and history of stroke have a high degree of uncertainty, whereas diseases such as diabetes and myocardial infarction may be more easily defined and recognised in the population. The diagnosis of hypertension should, ideally, be based on serial or ambulant blood pressure measurements. Hence, the prevalence may be overestimated.
Negative responses to self-reported AF were not validated. However, this may only have led to an underestimation of the prevalence, due to the unknown number of false negative responses. A validation of self-reported AF in the Nord-Trøndelag Health Study (HUNT) questioned the use of self-reported AF, as sensitivity was low and many AF cases were missed.14 Our study was not designed as a validation study and therefore sensitivity and specificity of self-reported AF could not be estimated. Still, the PPV of self-reported AF in our study, 79.3%, was much higher than found in the HUNT study (PPV 56%).14 Furthermore, classification of AF as paroxysmal or persistent/permanent was made based on available ECGs and medical records, and we cannot rule out that some individuals may have been misclassified.
By its design, our study depicts a limited age group, making comparison to other studies difficult. Finally, the study was designed as a cardiovascular cohort study with a special focus on AF. Hence, individuals with known AF may have been more motivated to participate than unaffected individuals, which may represent a selection bias.
Prevalence of AF
To the best of our knowledge, no other study based on unselected population data has reported a prevalence of AF as high as 4.5% below the age of 65 years. Most comparable studies have reported a prevalence of 3.7%–4.2% in the age group 60–69 years.1 3 A Swedish study found 2.9% in the more comparable age group 60–64 years,15 while the Rotterdam study reported <2% in this age group.16 AF prevalence in our study is particularly high for men (6.4%), while a few studies have reported a prevalence >2.4% among women at this age.3 17 18
Single time point screening for AF
The true prevalence of AF cannot be found by single time point ECGs, as some cases will be missed due to the paroxysmal nature of the arrhythmia. Still, opportunistic single time point screening is recommended in current guidelines.4 However, this is based on studies in which single time point screening typically identified 1.0%–1.6% unknown AF by methods comparable to our study.5 19
The lower yield of screening in our study may partly be explained by the high prevalence of known AF, and the fact that the population under study has a high level of education and lives in a setting with good access to healthcare and primary care in particular. The population examined was just below 65 years. Hence, our findings confirm that yield of screening in this age group is low. While some studies with similar population-based design have found comparable low rates of new AF,20 others have shown a much higher yield by more extensive methods such as intermittent or continuous ECG registrations.21 22 The large discrepancies between studies supports the recommendation that future AF screening should be country specific and health system specific.23
A recent white paper on AF screening concluded that screen-detected AF found on single time point screening should be considered for stroke prevention in the same manner as clinical AF.23 More extensive screening methods should be considered in selected groups, particularly in those >65 years and with additional risk factors. Although alternative methods such as dedicated blood pressure devices have shown promising results as a primary step in screening,24 ECG confirmation is still mandated for the diagnosis of AF.
Risk factors for AF
Apart from age, hypertension has been accepted as the most important risk factor for AF for decades, largely due to its high occurrence in the general population.25 More recent data have shown, however, that the risk in both sexes may be higher from obesity.26 Similar trends have been found in the Framingham Heart Study, in which diabetes and increased BMI have been identified as emerging risk factors.27
Height has been demonstrated to be a risk factor for AF and other CVD, independent from weight.28 It has also been shown that use of BMI as a measure of body size leads to loss of predictive information, compared with weight and height separately.29 Most studies, including ours, have found that age-adjusted prevalence of AF is higher in men than in women.30 Still, male sex was, in our study, not associated with AF after assessing the impact of height, weight and other risk factors. This may indicate that differences in the distribution of AF risk factors, including body height and weight, may account for most, if not all, of the higher prevalence of AF in men at this age. This is consistent with findings from three large cohorts resulting in the Cohorts for Heart and Aging Research in Genomic Epidemiology (CHARGE) AF risk score for AF prediction, in which height and weight, but not sex, were found to predict AF.6
In our study, we found that most AF subjects were defined as hypertensive, nearly half were obese, and only 13% had no known comorbidity. The rising prevalence of obesity during the last decades may have contributed to an increasing AF prevalence.26 Our findings support this theory; however, we cannot draw any conclusions based on our limited data.
The heritability of AF is well established. For many individuals with AF, the arrhythmia is probably a multifactorial and polygenic phenomenon, and a number of genetic variants associated with increased risk have been identified.31 Some studies have also shown a strong association between self-reported familial AF and AF occurrence, independent of other risk factors, including genetic variants.32 In line with these studies, we found that AF occurred twice as often in subjects who had at least one first-degree relative with AF, at any age, compared with those without familial AF.
Stroke risk in AF
Stroke prevention is of utmost importance in AF, and guideline adherence improves outcomes.33 In this cohort, stroke risk in the AF group was low (see online supplementary table 3). Use of anticoagulation was reported only in 47% of individuals with AF. However, many turned 65 years shortly after inclusion and their indication for anticoagulation would then have been strengthened. Within the small group of individuals with screen-detected AF, the stroke risk was even lower.
Clinical implications
Increased awareness with regard to detection and treatment of AF is desirable, particularly because of the increased stroke risk. However, it is still unknown whether screening or more active case finding for AF will be effective in reducing stroke rates. Current guidelines advise health personnel to carry out simple measures such as pulse palpation and 12-lead ECG more frequently at the age of 65 years and above, or even in younger age groups if risk factors for stroke are present.4 New and portable single-lead ECG devices may make these recommendations easier to implement, as single time point or even repeated measurements can be performed more easily.23 However, it is still unknown in which groups of the population screening may be justified. The low yield of single time point screening in our study supports the opinion that screening below the age of 65 years may only be recommended in selected high-risk groups.
The high prevalence of obesity and untreated hypertension found in this cohort is alarming. These conditions can potentially be prevented in primary care and by public health measures. Prevention of AF by early detection and treatment of these conditions may be as important as early detection of AF itself. Nearly half of AF individuals in this study were found with elevated blood pressure, regardless of treatment, underlining a potential also for improved treatment within this group.
Conclusion
The prevalence of known AF was higher than previously reported below the age of 65 years, and higher in men than in women. Single time point screening for AF revealed a low number of previously unknown AF. Height, weight and comorbidity, but not sex, were independently associated with AF at this age.
Supplementary Material
Acknowledgments
We thank all our study participants for their participation. We also thank our dedicated study staff at the Department of Medical Research, Bærum Hospital, Vestre Viken Hospital Trust and at the Clinical Trial Unit, Division of Medicine, Akershus University Hospital.
Footnotes
Contributors: TB, KS, TO, PS, HR and AT designed the study. TB, MNL, HI-H, JB, MOP, ENA, TV, BK and IEC have performed the baseline examinations and the acquisition of data. TB and PS have performed the validation of atrial fibrillation diagnoses, supported by MNL, JB and AT. TB and MNL have performed the statistical analysis. TB has written the manuscript. AT was the principal investigator (PI) and HR was the co-PI of the study. All authors have revised the manuscript for important intellectual content and have read and approved the final manuscript.
Funding: This work was supported by the non-governmental patient organisation Norwegian Health Association (‘Nasjonalforeningen for folkehelsen’), Vestre Viken Hospital Trust and Akershus University Hospital.
Competing interests: TB has (outside this work) received honoraria from Boehringer-Ingelheim, Bayer and Pfizer/Bristol-Myers Squibb. TO has (outside this work) received honoraria or research support from Abbott, AstraZeneca, Bayer, Novartis, Roche, Singulex and Thermo Fisher. HR has (outside this work) received honoraria or research support from Novartis, CardiNor AS and SpinChip Diagnostics. TO and HR are partners in a patent filed by the University of Oslo regarding the use of secretoneurin as a biomarker in patients with cardiovascular disease and patients with critical illness.
Patient consent: Obtained.
Ethics approval: Regional Ethics Committee, South-East Norway (ref. 2011/1475).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: The data set used in this study is not publicly available, as the Data Protection Authority approval and patient consent do not allow for such publication. However, the study group welcomes initiatives for cooperation, and data access may be granted upon application. More information on: www.ace1950.no.
References
- 1. Zoni-Berisso M, Lercari F, Carazza T, et al. Epidemiology of atrial fibrillation: European perspective. Clin Epidemiol 2014;6:213–20. 10.2147/CLEP.S47385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wolowacz SE, Samuel M, Brennan VK, et al. The cost of illness of atrial fibrillation: a systematic review of the recent literature. Europace 2011;13:1375–85. 10.1093/europace/eur194 [DOI] [PubMed] [Google Scholar]
- 3. Friberg L, Bergfeldt L. Atrial fibrillation prevalence revisited. J Intern Med 2013;274:461–8. 10.1111/joim.12114 [DOI] [PubMed] [Google Scholar]
- 4. Kirchhof P, Benussi S, Kotecha D, et al. ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J 2016;2016:2893–962. [DOI] [PubMed] [Google Scholar]
- 5. Lowres N, Neubeck L, Redfern J, et al. Screening to identify unknown atrial fibrillation. A systematic review. Thromb Haemost 2013;110:213–22. 10.1160/TH13-02-0165 [DOI] [PubMed] [Google Scholar]
- 6. Alonso A, Krijthe BP, Aspelund T, et al. Simple risk model predicts incidence of atrial fibrillation in a racially and geographically diverse population: the CHARGE-AF consortium. J Am Heart Assoc 2013;2:e000102 10.1161/JAHA.112.000102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Huxley RR, Lopez FL, Folsom AR, et al. Absolute and attributable risks of atrial fibrillation in relation to optimal and borderline risk factors: the Atherosclerosis Risk in Communities (ARIC) study. Circulation 2011;123:1501–8. 10.1161/CIRCULATIONAHA.110.009035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Berge T, Vigen T, Pervez MO, et al. Heart and Brain Interactions--the Akershus Cardiac Examination (ACE) 1950 Study Design. Scand Cardiovasc J 2015;49:308–15. 10.3109/14017431.2015.1086813 [DOI] [PubMed] [Google Scholar]
- 9. Mosteller RD. Simplified calculation of body-surface area. N Engl J Med 1987;317:1098 10.1056/NEJM198710223171717 [DOI] [PubMed] [Google Scholar]
- 10. Naess O, Søgaard AJ, Arnesen E, et al. Cohort profile: cohort of Norway (CONOR). Int J Epidemiol 2008;37:481–5. 10.1093/ije/dym217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med 2009;150:604–12. 10.7326/0003-4819-150-9-200905050-00006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Aspenes ST, Nauman J, Nilsen TI, et al. Physical activity as a long-term predictor of peak oxygen uptake: the HUNT Study. Med Sci Sports Exerc 2011;43:1675–9. 10.1249/MSS.0b013e318216ea50 [DOI] [PubMed] [Google Scholar]
- 13. von Elm E, Altman DG, Egger M, et al. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 2007;335:806–8. 10.1136/bmj.39335.541782.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Malmo V, Langhammer A, Bønaa KH, et al. Validation of self-reported and hospital-diagnosed atrial fibrillation: the HUNT study. Clin Epidemiol 2016;8:185–93. 10.2147/CLEP.S103346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Andersson P, Löndahl M, Abdon NJ, et al. The prevalence of atrial fibrillation in a geographically well-defined population in northern Sweden: implications for anticoagulation prophylaxis. J Intern Med 2012;272:170–6. 10.1111/j.1365-2796.2012.02519.x [DOI] [PubMed] [Google Scholar]
- 16. Heeringa J, van der Kuip DA, Hofman A, et al. Prevalence, incidence and lifetime risk of atrial fibrillation: the Rotterdam study. Eur Heart J 2006;27:949–53. 10.1093/eurheartj/ehi825 [DOI] [PubMed] [Google Scholar]
- 17. Gómez-Doblas JJ, Muñiz J, Martin JJ, et al. Prevalence of atrial fibrillation in Spain. OFRECE study results. Rev Esp Cardiol 2014;67:259–69. 10.1016/j.rec.2013.07.014 [DOI] [PubMed] [Google Scholar]
- 18. Nyrnes A. Atrial fibrillation in the tromsø study 1994-2007 (ph.d. thesis): The Arctic University of Norway, Faculty of Health Sciences, 2016. [Google Scholar]
- 19. Fitzmaurice DA, Hobbs FD, Jowett S, et al. Screening versus routine practice in detection of atrial fibrillation in patients aged 65 or over: cluster randomised controlled trial. BMJ 2007;335:383 10.1136/bmj.39280.660567.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Schnabel RB, Wilde S, Wild PS, et al. Atrial fibrillation: its prevalence and risk factor profile in the German general population. Dtsch Arztebl Int 2012;109:293–9. 10.3238/arztebl.2012.0293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Healey JS, Alings M, Ha A, et al. Subclinical atrial fibrillation in older patients. Circulation 2017;136:1276–83. 10.1161/CIRCULATIONAHA.117.028845 [DOI] [PubMed] [Google Scholar]
- 22. Svennberg E, Engdahl J, Al-Khalili F, et al. Mass screening for untreated atrial fibrillation: the STROKESTOP study. Circulation 2015;131:2176–84. 10.1161/CIRCULATIONAHA.114.014343 [DOI] [PubMed] [Google Scholar]
- 23. Freedman B, Camm J, Calkins H, et al. Screening for atrial fibrillation: a report of the AF-SCREEN International Collaboration. Circulation 2017;135:1851–67. 10.1161/CIRCULATIONAHA.116.026693 [DOI] [PubMed] [Google Scholar]
- 24. Omboni S, Verberk WJ. Opportunistic screening of atrial fibrillation by automatic blood pressure measurement in the community. BMJ Open 2016;6:e010745 10.1136/bmjopen-2015-010745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kannel WB, Abbott RD, Savage DD, et al. Epidemiologic features of chronic atrial fibrillation: the Framingham study. N Engl J Med 1982;306:1018–22. 10.1056/NEJM198204293061703 [DOI] [PubMed] [Google Scholar]
- 26. Magnussen C, Niiranen TJ, Ojeda FM, et al. Sex differences and similarities in atrial fibrillation epidemiology, risk factors, and mortality in community cohorts: results From the BiomarCaRE Consortium (Biomarker for Cardiovascular Risk Assessment in Europe). Circulation 2017;136:1588–97. 10.1161/CIRCULATIONAHA.117.028981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Schnabel RB, Yin X, Gona P, et al. 50 year trends in atrial fibrillation prevalence, incidence, risk factors, and mortality in the Framingham Heart Study: a cohort study. Lancet 2015;386:154–62. 10.1016/S0140-6736(14)61774-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Allan V, Honarbakhsh S, Casas JP, et al. Are cardiovascular risk factors also associated with the incidence of atrial fibrillation? A systematic review and field synopsis of 23 factors in 32 population-based cohorts of 20 million participants. Thromb Haemost 2017;117:837–50. 10.1160/TH16-11-0825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Karas MG, Yee LM, Biggs ML, et al. Measures of body size and composition and risk of incident atrial fibrillation in older people: the cardiovascular health study. Am J Epidemiol 2016;183:998–1007. 10.1093/aje/kwv278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Staerk L, Sherer JA, Ko D, et al. Atrial fibrillation: epidemiology, pathophysiology, and clinical outcomes. Circ Res 2017;120:1501–17. 10.1161/CIRCRESAHA.117.309732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Christophersen IE, Rienstra M, Roselli C, et al. Large-scale analyses of common and rare variants identify 12 new loci associated with atrial fibrillation. Nat Genet 2017;49:946–52. 10.1038/ng.3843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Lubitz SA, Yin X, Fontes JD, et al. Association between familial atrial fibrillation and risk of new-onset atrial fibrillation. JAMA 2010;304:2263–9. 10.1001/jama.2010.1690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lip GY, Laroche C, Popescu MI, et al. Improved outcomes with European Society of Cardiology guideline-adherent antithrombotic treatment in high-risk patients with atrial fibrillation: a report from the EORP-AF General Pilot Registry. Europace 2015;17:1777–86. 10.1093/europace/euv269 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2018-021704supp001.pdf (457.6KB, pdf)