Abstract
Objective
To analyse average lifespan and quantify the effect of avoidable/amenable mortality on the difference between state-specific mortality and a low-mortality benchmark in Mexico during 1990–2015.
Design
Retrospective cross-sectional demographic analysis using aggregated data.
Setting
Vital statistics from the Mexican civil registration system.
Participants
Aggregated national data (from 91.2 million people in 1995 to 119.9 in 2015) grouped in 64 populations (32 Mexican states (including Mexico City) by sex) with cause-of-death data.
Main outcome measures
Cause-specific contributions to the gap in life expectancy with a low-mortality benchmark in three age groups (0–14, 15–49 and 50–84 years).
Results
Infants and children under the age of 15 years show improvements towards maximal survival in all states. However, adult males aged 15 to 49 years show deterioration after 2006 in almost every state due to increasing homicides, and a slow recovery thereafter. Out of 35 potential years, females and males live on average 34.57 (34.48 to 34.67) and 33.80 (33.34 to 34.27), respectively. Adults aged 50 to 84 years show an unexpected decrease in the low mortality benchmark, indicating nationwide deterioration among older adults. Females and males in this age group show an average survival of 28.59 (27.43 to 29.75) and 26.52 (25.33 to 27.73) out of 35 potential years, respectively. State gaps from the benchmark were mainly caused by ischaemic heart diseases, diabetes, cirrhosis and homicides. We find large health disparities between states, particularly for the adult population after 2005.
Conclusions
Mexico has succeeded in reducing mortality and between-state inequalities in children. However, adults are becoming vulnerable as they have not been able to reduce the burden of violence and conditions amenable to health services and behaviours, such as diabetes, ischaemic heart diseases and cirrhosis. These trends have led to large health disparities between Mexican states in the last 25 years.
Keywords: health inequality, adult health, homicides, avoidable mortality, health behaviours
Strengths and limitations of this study.
We analyse nine cause-of-death groups using the concept of avoidable/amenable mortality, which enables us to capture recent changes in mortality in Mexico.
We introduce a methodology to quantify the impact of medically amenable mortality and behaviour-related conditions on life expectancy relative to a low mortality benchmark.
We analyse patterns in life expectancy for different age groups over time (1995–2015) and simultaneously account for changes in causes of death and inequality between states that have undergone major social and public health transitions.
Mortality data from Mexico are likely to present inaccuracies in cause-of-death classification due to comorbidities, particularly at older ages.
Our estimates of homicide mortality are likely to be underestimated due to inaccurate practices in counting and reporting and due to the large number of missing individuals in Mexico.
Introduction
The second half of the 20th century was marked by sizeable improvements in mortality, living conditions and health in most Latin American countries.1 In Mexico, these improvements have slowed down recently due to opposing trends in particular causes of death. For instance, homicide and diabetes increased during the first decade of the 2000s, even as infectious and respiratory diseases continued to fall over the same period. While life expectancy at birth increased by 4.3 years for males (from 67.6 to 71.9) and 3.4 years for females (from 73.8 to 77.2) between 1990 and 2000,2 between 2000 and 2010, life expectancy at birth entered into a period of stagnation for males and slowed progress for females.3
This period coincides with ongoing public health interventions, such as the Universal Vaccination Programme and established health systems (Instituto Mexicano del Seguro Social (IMSS), Instituto de Seguridad y Servicios Sociales de los Trabajadores del Estado (ISSSTE)), and with the implementation of a Universal Health Coverage programme (Seguro Popular). The latter programme provides primary and secondary healthcare to the uninsured population and distributes funds to cover catastrophic health expenditures.4 Further, since 1997 conditional cash transfer programmes were introduced to supply incentives for poor families to invest in education, health and nutrition.5 Some evidence suggests that Mexico experienced substantial decreases in infant and child mortality, and in the prevalence of acute malnutrition between 1980 and 2000 thanks in part to these interventions.6 Similarly, by 2012 Seguro Popular had provided health insurance coverage to an additional 52 million people in Mexico (or 44.4% of the population), leading to increased access to public healthcare and protection from the financial consequences of disease.7
Conditional cash transfers have focused on the poorest states, and Seguro Popular was introduced at different times in different states across the country. Although these actions underscore broad progress in public health interventions, they mask disparities between Mexican states and epidemiological patterns that differ between age groups. For instance, Mexico faces a rapid ageing process in which an interaction between infectious diseases and non-communicable conditions can be anticipated in the adult population. i 8 Therefore, it is necessary to assess the varied impacts that these interventions may have had on mortality in Mexican states at different ages.9
One approach to approximate the impact of healthcare and other interventions on survival, and to reveal potential areas of improvement is by operationalising the concept of avoidable or amenable mortality (hereafter abbreviated AM).10 11 This categorisation of mortality aims to measure the quality of health service systems by selecting certain causes of death that should not occur in the presence of effective and timely healthcare. Therefore, improvements in AM are expected over time, as has been observed in several countries. For example, among 19 industrialised countries, including 14 countries from Western Europe, USA, Canada, Australia, New Zealand and Japan, a reduction in AM rates was observed over the past 20 years.10 Avoidable mortality rates fell, on average, by 17% for males and 14% for females in these countries between 1997 and 2003. The USA lagged behind the other countries in this group, while Japan, France and Australia were the top performers. Despite mortality reductions from cancers and circulatory diseases for both sexes, disparities between countries persist, with the USA showing the smallest reductions (around 5%) for both sexes.10
In Mexico, the components of avoidable mortality have undergone opposing trends since the late 1990s. Mortality from infectious diseases and nutrition-related conditions decreased between 2000 and 2004,12 while deaths related to diabetes and ischaemic heart diseases (IHD) increased in the first decade of the 2000s.13 Importantly, increases in the latter causes of death were concentrated in the poorest states of the country.13
The objective of this research is twofold. First, we analyse trends in average lifespan for all 32 Mexican states, by sex, and over the full period from 1990 to 2015. This extends previous studies that focused on the 21st century.3 13–16 Our study period covers several public health interventions and captures several major trends in state and cause-of-death variation. Second, we further segment AM into health intervention-related and behaviour-related AM causes that best characterise the epidemiological patterns of Mexico.14 This lets us quantify the effect of the components of AM on the difference between state mortality levels and an easy-to-understand low-mortality benchmark calculated for large age groups (ie, 0–14, 15–49 and 50–84 years). This benchmark concept has been previously used in mortality studies.17–19 Deviations from the low-mortality benchmark indicate a strong potential for improvement.
We hypothesise age-dependent variations in mortality outcomes. In particular, since public health interventions are mainly focused on infant and child health, we expect convergence between states and improvement in survival for infants and children aged 0 to 15 years. For instance, the vaccination programme and Seguro Popular aim to cover all children, and recent evidence suggests a decrease in mortality below the age of 15 years due to a decline in infectious and respiratory diseases.20 On the contrary, we expect little improvement in survival for the young adult population (ages 15 to 35 years) due to the sudden and egregious rise in homicide mortality.21 We foresee health deterioration among older adults due to documented increases in diabetes mortality.20 Although every state has the commitment to provide universal coverage and equitable access to healthcare, we anticipate disparities in mortality improvements between states due to heterogeneous epidemiological transitions among states,16 and differences in the implementation and delivery of healthcare programmes.22
Data sources and methods
Our analyses are based on publicly available anonymised datasets. We used 100% sample death register microdata files produced by the Mexican Statistical Office (INEGI) for years 1990 to 2015.23 We aggregated individual deaths from these annual files by causes of death, single year of age, sex and state of residence at the time of death. Population estimates from 1990 to 2015 were produced by the Mexican Population Council (CONAPO).24 These population estimates adjust for age misstatement, undercounting, and interstate and international migration. Death counts and estimates of the population exposed to risk were used to calculate age and cause specific death rates by sex for each state from 1990 to 2015.
Classification of causes of death
To classify deaths, we use the AM concept.10 11 We group causes of death into nine categories based on recent classification adapted to the case of Mexico.14 The first category refers to those conditions that are susceptible to medical intervention, such as infectious and respiratory diseases, some cancers and circulatory conditions, and birth conditions, among others. We label this category as ‘Causes amenable to medical service’. We separate diabetes, IHD, lung cancer and cirrhosis as subcategories of AM because these causes are susceptible to both health behaviour and medical service, and because the first two represent major causes of death among Mexican adults.16 We also separate homicide, suicide and road traffic accidents because they have emerged as leading causes of death among young people, and the first one recently had a sizeable impact on life expectancy in Mexico.14 We grouped remaining causes into a single category labelled ‘Other causes’.
Death data were originally classified according to the International Classification of Diseases (ICD), revision 9 for years 1990 to 1997 and revision 10 for 1998 to 2015 (see online supplementary table 1 for details on ICD codes for each category). To check the validity of these cause-of-death codes in Mexico, we performed a sensitivity analysis and did not find major ruptures in mortality trends by AM classification (online supplementary figure 1).
bmjopen-2018-022350supp001.pdf (855.3KB, pdf)
Comorbidity in the old age population has increased in Mexico.25 As a result, inaccuracies may arise in cause of death registration due to problems associated with medical diagnosis, and selection and coding of the leading cause of death. Although analyses of older ages should consider multiple causes of death to better represent old age mortality, we focus on the primary cause of death. We truncate our analysis at age 85 to avoid misinterpreting results related to inaccurate cause-of-death coding practices.
Age groups
We calculate life expectancy in three large age groups to capture mortality differences over the life course. Life expectancy in each age group refers to the average years of life lived between two ages conditional on survival to the lower age bound. This measure is also known in demographic analysis as temporary life expectancy.26 The first age group contains infants and children aged 0–14 years. This group is likely to represent improvements in causes amenable to medical service (eg, infectious diseases and conditions of the perinatal period).3 The second group, aged 15–49 years, is used to capture the effect of homicide mortality and external causes historically related to the young-adult mortality hump, as well as maternal mortality for women.27 This age group had an important impact on changes in state life expectancy in the first decade of the 2000s.14 The third group covers older adults aged 50–84 years. Older adults are likely to represent a vulnerable group due to increases in non-communicable diseases and injury-related mortality in recent years.16 28
Low mortality benchmark
Our low mortality benchmark is calculated on the basis of the lowest observed mortality rates over all states by age, year, cause and sex. The resulting minimum mortality rate schedule has a unique age profile, and it determines our benchmark temporary life expectancy, which we calculate for our three age groups. This benchmark is a practical reference because it is based neither on a projection of improvements into the future nor on an arbitrary and likely dissimilar population. It can be treated as the best presently achievable mortality assuming perfect diffusion of the best available practices and technologies in Mexico.19
Methods
Cause-specific death rates underlie all indices reported in this work. To mitigate the impact of random variations over time and to correct for age heaping, we adjust these rates in two steps. First, we smooth cause-specific rates over age and time for each state and sex separately using a 2-d p-spline.29 Second, we rescale the smoothed cause-specific death rates to sum to the raw all-cause death rates for each sex and state. Period life tables up to age 84 for males and females from 1990 to 2015 and their benchmarks were calculated following standard demographic methods (for life table construction, see Chapter 2 of reference 31).30 31 We calculated temporary life expectancies26(see online supplementary file 1 for a technical overview and 95% CIs) and estimated cause-specific contributions to the difference between each state and the low mortality benchmark using standard decomposition techniques.32 The decomposition method used in this analysis is based on a model of demographic functions that change gradually over time.32 It is a stepwise-based demographic method and has been successfully used to decompose age-specific and cause-specific effects on life expectancy.33 We provide a short description in the online supplementary material and the results are fully reproducible from the R-code provided in the data sharing statement. Finally, to measure the level of disparity between states over time, we calculated the coefficient of variation of the gap between temporary life expectancy and the low mortality benchmark in each age group. This indicator is comparable over time and over age groups of different widths. We also performed two-way analysis of variance (ANOVA) and post hoc tests to analyse disparities in temporary life expectancy between Mexican states and age groups.
Patient involvement
No patients were involved in setting the research question, outcome measures or design of the study. No patients were asked to advise on the interpretation of the results and there are no plans on disseminating the results of this research to study participants or the relevant patient community.
Results
Trends in life expectancy for Mexican states by age groups
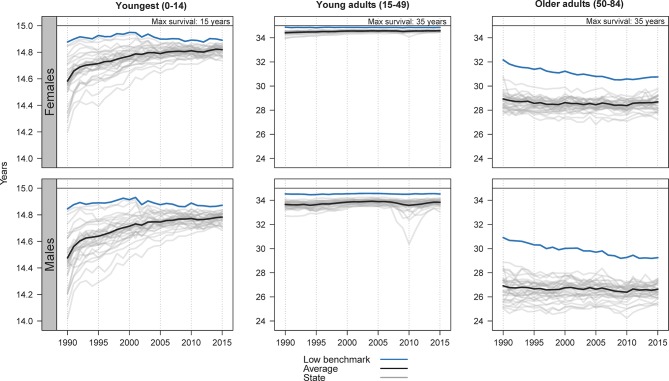
Figure 1 presents temporary life expectancy by state for infants and children (ages 0–14), young adults (15–49) and older adults (50–84) over the period 1990–2015. Grey lines refer to each of the 32 states, black lines represent the state average and the blue lines represent the low mortality benchmark. The black line at the top of each panel indicates the maximum liveable years in each age group: 15 for the youngest group, and 35 for young and older adults conditional on surviving to ages 15 and 50, respectively. Any gap between a state line and the blue line represents potential life expectancy gains if mortality were to drop to the low mortality benchmark.
Figure 1.
State-specific life expectancy trends (grey), average (black) and low mortality benchmark (blue) for three age groups, the youngest (0–14 years), young adults (14–49 years) and older adults (50–84 years) by sex for the period 1990–2015. Source: calculations based on INEGI and CONAPO files. CONAPO, Mexican Population Council; INEGI, Mexican Statistical Office.
All states show improvements in the youngest age group since 1990, approaching the low mortality benchmark, which itself is very close to maximum survival below age 15. This was observed even in the southern states such as Puebla, Chiapas and Tabasco which have lagged in reducing mortality in this age group throughout the entire period.
Male life expectancy between ages 15 and 49 showed a sudden drop after 2005 in almost every state in Mexico. In 2005, young males in this age group had a temporary life expectancy of 33.9 years (95% CI 33.5 to 34.2) averaged over states. By 2010, the number of states below this level had increased from 14 to 23. Chihuahua, Sinaloa and Durango, in the northern region, experienced a substantial mortality shock in 2010 in this age group and consequently recorded the largest gap from the low mortality benchmark. By 2015, the state average (33.8 years, 95% CI 33.3 to 34.3) had almost recovered to its 2005 level. Trends for females are closer to the low mortality benchmark.
Among older adults, life expectancy between ages 50 and 84 shows stagnation and deterioration over the entire period of observation. Even the low mortality benchmark exhibits a gradual downward trend, pointing to a generalised mortality increase. The state average female life expectancy declined from 28.8 years (95% CI 27.4 to 30.2) in 1990 to 28.3 years (95% CI 27.4 to 29.2) in 2010. By 2015, this average only managed to recover to 28.6 years (95% CI 27.4 to 29.8). Among males, the average over states decreased from 26.7 years (95% CI 24.7 to 28.8) in 1990 to 26.3 years (95% CI 24.9 to 27.6) in 2010, and 26.5 years (95% CI 25.3 to 27.7) in 2015. Furthermore, we fitted three linear models by sex and for both sexes, and the slope coefficient was significant in all of them at the level of p<0.005. These results suggest that the decline observed was significant. As with young adult males, some states experienced deterioration after 2005, with a minor recovery since 2010.
Health disparities between states and age groups
Figures 2–5 show results only for males because they exhibit the largest departures from the low mortality benchmark and higher inequality. Results for females are shown in the online supplementary file 1.
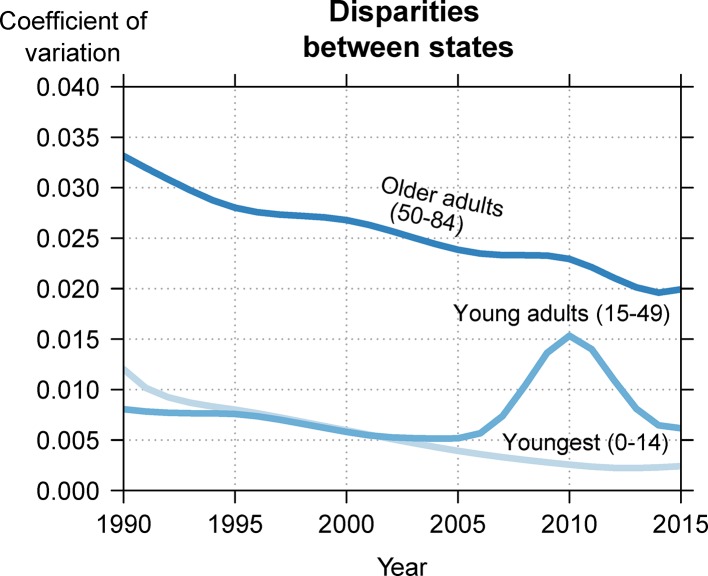
Figure 2 shows trends in inequalities between states in Mexico for males in our three age groups, as measured by the coefficient of variation (results for females are reported in online supplementary figure 2). This indicator measures the between-state variation in the state-specific benchmark within each of the three age groups. Larger values are related to higher disparities between states. Trends show mixed patterns of convergence with temporary divergence around 2010, and with females in all cases showing less between-state inequality than males over the entire period studied.
Figure 2.
Inequality in male life expectancy between states for the youngest (0–14 years), young adults (15–49 years) and older adults (50–84 years), 1990–2015. Source: calculations based on INEGI and CONAPO files. CONAPO, Mexican Population Council; INEGI, Mexican Statistical Office.
There are important differences in inequality levels and trends between age groups. Since 1990, state inequality in life expectancy in the youngest age group has been decreasing. Among females, young adults show even lower between-state disparity than infants and children. However, for males in the young adult age group, there was a crossover in the early 2000s, with the coefficient of variation increasing after 2005. The highest values are observed in the period 2009–2011. By 2015, state inequalities among young adults had decreased substantially, but remained higher than that of the youngest age group. Older adults show substantially higher inequality than the other age groups over the entire period studied, but also show steady convergence between states. From 2013, both males and females show a potential rise in disparities between states, but we caution that this rise could be random variation as it only appears for 2 years (online supplementary figure 2).
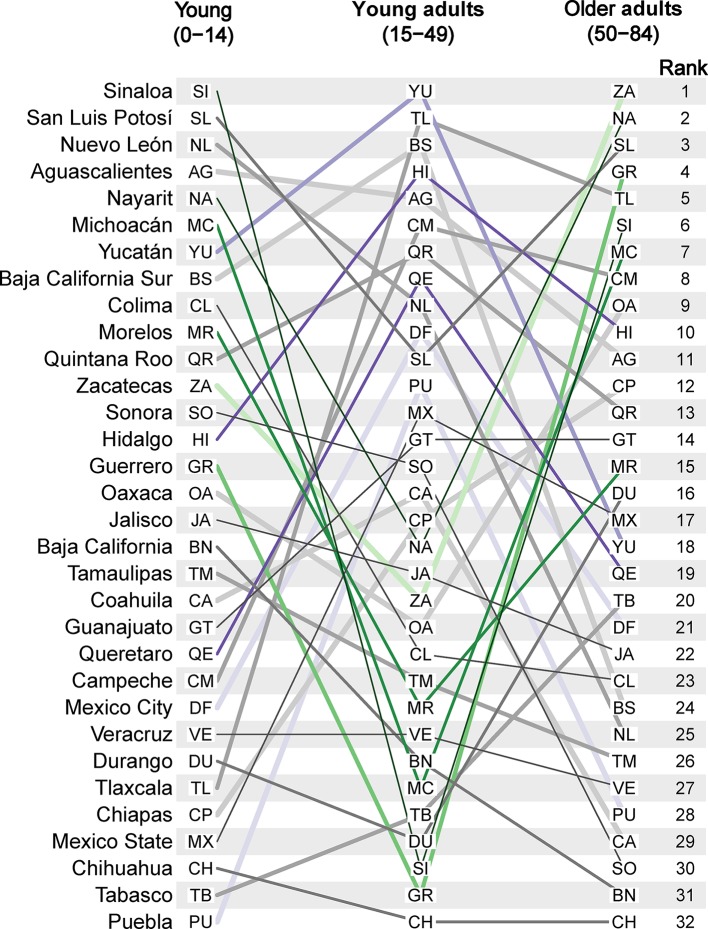
To illustrate discordance between age groups within each state, figure 3 shows the state ranking of temporary life expectancy for the years 2010–2015 for males in each age group (see online supplementary figure 3 for females’ results). States at the top show the highest values in temporary life expectancy, while states in the bottom refer to the lowest expectancies. We chose to highlight those states with the most discordant age rankings. Green and purple lines refer to selected states that show drastic changes in the ranking between different age groups. For example, Sinaloa, in the northern part of Mexico, holds the record life expectancy below age 15; however, young adults (15–49 years) show one of the lowest expectancies, while older adults are in the sixth position out of 32. Similar trajectories are shown with green lines for Nayarit and Michoacán in the central region, Zacatecas in the North, as well as Morelos and Guerrero from the southern region. Conversely, the pattern of age discordance in Hidalgo, Querétaro and Mexico City from the central region, and Yucatán and Puebla in the South (purple lines) is summarised by changing from a low rank in the youngest age group to a high rank in young adults, followed by low rank in older adults.
Figure 3.
Discordant age rankings for average male life expectancy 2010–2015 for the youngest (0–14 years), young adults (14–49 years) and older adults (50–84 years). Source: calculations based on INEGI and CONAPO files. CONAPO, Mexican Population Council; INEGI, Mexican Statistical Office.
We performed a two-way ANOVA on temporary life expectancy by state and age groups controlling for year. There was a statistically significant interaction between the effects of states and age groups (F=12.25, p<0.001) indicating, as shown in figure 3, that part of the existing variation in the country is due to variability within each state. There were also significant differences in temporary life expectancy between age groups (p<0.001) and states (p<0.001) reflecting between-state variability, as shown in figure 2.
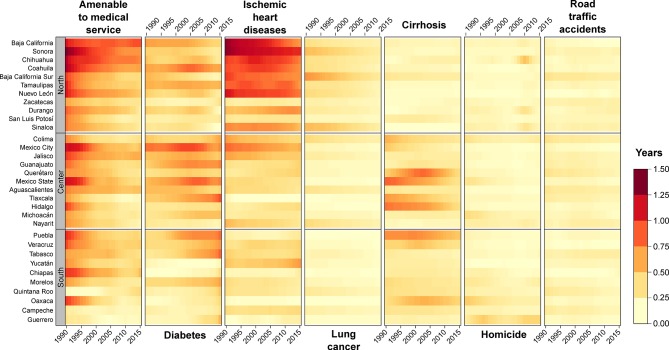
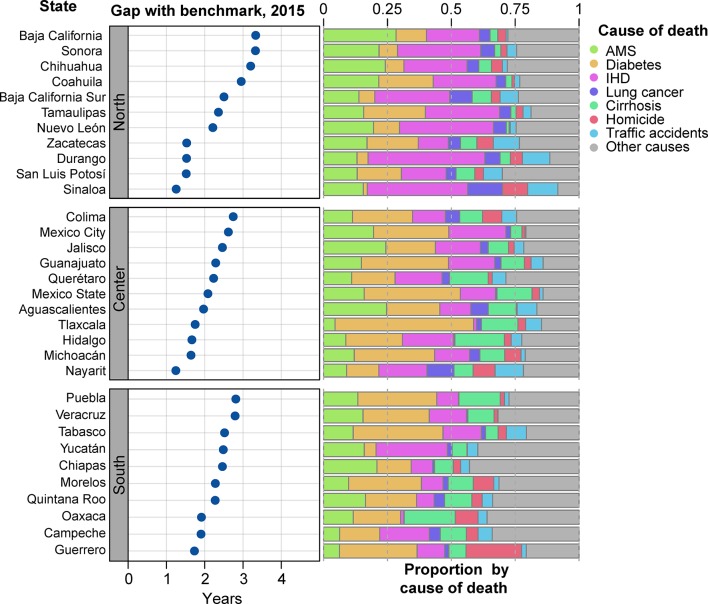
Cause decomposition analysis
In figures 4 and 5, the Mexican states in each region are arranged according to the largest gap with the low mortality benchmark among older adult males in 2015. Figure 4 shows how causes amenable to medical service, diabetes, IHD, lung cancer, cirrhosis, homicide and road traffic accidents contributed to the gap between each state and the low mortality benchmark from 1990 to 2015 for older males (ages 50–84). These are the causes of death that contributed the most to holding states back from achieving the low mortality benchmark. Light-yellow colours indicate negligible contributions, which means that are very close to the low mortality benchmark within each category. Darker red hues indicate larger contributions to the gap. If a state is improving during the period, it shows a transition from red to light yellow.
Figure 4.
Cause-specific contributions to the gap between states and low mortality benchmark for older male adults (50–84 years), 1990–2015. Source: calculations based on INEGI and CONAPO files. CONAPO, Mexican Population Council; INEGI, Mexican Statistical Office.
Figure 5.
State-specific gap with the low mortality benchmark and its cause-of-death composition for older male adults (50–84 years) in 2015. Source: calculations based on INEGI and CONAPO files. CONAPO, Mexican Population Council; INEGI, Mexican Statistical Office.
Medically amenable causes of death show gradual improvements in most states from 1990 to 2015, bringing them closer to the benchmark in this category. However, large disparities persist between states and a strong potential for improvements remain. For example, Baja California, Sonora, Chihuahua and Coahuila from the northern region show substantial contributions to the gap. Diabetes mortality has increasingly contributed to widening the benchmark gap in several states, including Coahuila and Tamaulipas in the North, Mexico City, Guanajuato, Mexico state, and Tlaxcala in the central region, and Puebla, Veracruz and Tabasco in the South. Similarly, IHD significantly affects the northern part of the country, while cirrhosis is mostly concentrated in the South. Lung cancer and road traffic accidents have lower contributions to the benchmark gap, but these remain important causes of death. Homicides increased the gap in this age group in some states after 2005, such as Chihuahua, Durango and Sinaloa in the North, Colima, Michoacán and Nayarit in the central region, and Guerrero in the South.
Females show similar regional patterns to males, although of lower magnitudes. For males, causes amenable to medical service, diabetes and IHD contributed the largest share to the gap with the low mortality benchmark among older adult females. In the youngest age group, improvements in life expectancy and in reducing the gap with the low mortality benchmark were mainly driven by causes amenable to medical service among both females and males. Finally, homicide mortality and road traffic accidents are the main drivers of the gap with the benchmark among young male adults (ages 15–49). Importantly, homicides contributed more than 2.5 years to the gap with the low mortality benchmark in 2010 in the northern state of Chihuahua, and several states from the North and South of Mexico showed substantial impacts from homicide after 2005. Results for all age groups are shown in online supplementary figures 4–9.
Potential gains and causes of death in 2015
Figure 5 breaks down the state-specific low mortality benchmark gap for males aged 50–84 years into potential gains and their cause of death composition. The left panel shows the potential gains for older adults if the low mortality benchmark were achieved for each state in 2015. The right panel shows the proportion of potential gains due to specific causes of death in the same year.
Every state in Mexico could increase survival by at least 1 year on average in older adult ages if they were to achieve the low mortality benchmark. However, for 17 of them the gap with the benchmark is higher than 2 years, and for 3 states in the northern region it is greater than 3 years. For females, except for Sinaloa and Nayarit, all states show the potential to gain over an additional year of life between ages 50 and 84.
More than half of these potential gains in life expectancy between ages 50 and 84 are due to medically amenable causes, diabetes, IHD and cirrhosis in every state in Mexico (right panel). This is true also for females. Although older males show lower impact of homicide mortality on potential gains compared with young adult males (15–49 years), its effect is present in almost every state, particularly in Guerrero, Morelos in the South, Nayarit and Colima in the central region and Sinaloa in the North. Results for all the age groups for the years 2005, 2010 and 2015 are shown in the online supplementary figures 10–18.
Discussion
In Mexico since 1990, life expectancy in three large age groups has followed discordant patterns of rise, stagnation and deterioration. These patterns were driven mainly by causes of death that are amenable to medical service (such as infectious and respiratory diseases) and health behaviours (such as homicides, suicide, diabetes, IHD and cirrhosis). Patterns in these two large cause-of-death categories led to high levels of health inequality in the country.
Life expectancy below age 15 converged towards the low mortality benchmark and maximum survival in all 32 Mexican states. These results underscore public health interventions aimed at infants and children. This is supported by evidence that vaccination coverage has been achieved for the entire young population and that health insurance coverage has improved due to vaccination programmes and the implementation of Seguro Popular along with improvements in previously existing health systems, respectively.9 Causes amenable to medical service are at the heart of such improvements, consisting of decreases in infectious and respiratory diseases associated with public health interventions targeting children.6 For example, Puebla and Tlaxcala (in the South and central regions, respectively) were the states with the lowest life expectancy below age 15 in 1990, but they have since improved by more than half a year. Moreover, the average over states improved from 14.5 in 1990 to 14.8 in 2015, with no state below 14.7. Because of continuous and nationwide convergence towards the low mortality benchmark, inequalities between states in life expectancy below age 15 have been reduced.
Opposing the optimistic trend of infants and children, increases in homicide mortality reversed gains in male life expectancy, particularly between ages 15 and 49 years. These results are consistent with previous studies quantifying the effect of homicide mortality on the stagnation of national life expectancy at birth in the first decade of the 21st century,3 and with the reversal experienced in life expectancy in most states between 2005 and 2010.14 Our results extend such findings by adding 5 years of data and segmenting by three age groups capturing stages of the life course.34 We found that after 10 years of the unexpected rise in homicide mortality, most states have experienced a slow and partial recovery since 2010. However, the impact of homicide is still higher than the levels observed pre-2005. Between 2010 and 2015, homicides accounted for most of the gap between states and the low mortality benchmark in ages 15–49. For this age group, the states that show the greatest benchmark gap for homicide in 2015 are Guerrero in the South, and Sinaloa and Chihuahua in the North, which could gain 1 year, and half a year (each), respectively, if homicides were reduced to the level of the southern state of Yucatán, which in this case makes up 100% of the benchmark. Moreover, health inequalities in life expectancy between states followed the rise in homicides after 2005 (figure 2), and the considerable discordance between age groups (figure 3) was likely due in great part to homicide mortality in ages 15–49. It is unclear how these levels of state life expectancy will change with the new reports which highlight a 3-year increase in homicide in Mexico.23, ii Further, the exposure that people have had to violence has triggered mental health problems, for example, a widespread heightened perception of vulnerability.15 At the same time, suicide is strongly linked to mental disorders.35 Thus, if the Mexican health system does not have proper interventions to handle the mental health needs of the population, an increase in suicides might be observed in the future.
The population aged 50–84 years shows the largest low mortality benchmark gap in both females and males. Out of 35 liveable years in this age group, females lived on average 28.6 years and males 26.5 in 2015 without any clear improvement in the 26 years since 1990. Even the low mortality benchmark itself shows a downward trend for males and females (figure 1). Moreover, this age group exhibits the highest inequality between states in the last 26 years. Our results show that causes of death holding states back from the low mortality benchmark vary between regions. Causes amenable to medical service showed gradual improvements in almost every state since 1990. However, in some states of the northern region such as Baja California, Sonora and Chihuahua, these causes of death still show large room for improvements among older adults. Diabetes, IHD and cirrhosis account for most of the gap with the benchmark mortality, and these display large regional differences. For example, IHD is mostly concentrated in the North (figure 4), while cirrhosis and diabetes show a stronger impact in the central and southern regions. These results are supported by previous evidence documenting an increase in adult mortality rates from chronic kidney disease, diabetes and cirrhosis since 2000.16 Lung cancer and homicides had a lower impact on life expectancy for this age group, and both are higher in the northern part of the country.
Strengths and limitations of the study
Our analytical approach enables us to measure the years of life expectancy that could be gained in Mexican states by improving medically amenable mortality and behaviour-related mortality to the lowest levels presently observed in Mexico. This concept allows us to analyse patterns in life expectancy for different age groups over time and simultaneously account for changes in causes of death and inequality between states that have undergone major social and public health transitions.
The limitations of our study should be mentioned. First, mortality data from Mexico are likely to present inaccuracies in cause-of-death classification due to comorbidities, particularly at older ages.36 To mitigate this, we focus on ages below 85 and broad cause-of-death groups. In addition, road traffic accidents and homicides may happen not in the place of residence but in another state, which might cause differences in state-specific mortality. Moreover, our estimates regarding homicide mortality are likely to be underestimated due to inaccurate coding and reporting practices and due to the large number of missing individuals in Mexico.37 38 Similarly, in 1997, a change in diagnosis criterion for diabetes took place, and this could have an impact on trends of mortality caused by diabetes in years adjacent to 1997.39 In addition, under-reported deaths and ill-defined causes of death could potentially bias our results. Mexico is considered to have high-quality data according to the Pan American Health Organization’s criteria. Under-reported deaths are estimated to be around 0.8%,40 41 while ill-defined causes of death fell from 2.1% of all deaths around 2000 to 1.7% more recently.40 We expect our main findings to be robust given the small percentages of ill-defined and under-reported deaths. Finally, small population sizes could bias our results. As a robustness check, we calculated CIs (95%) for all our estimates of temporary life expectancy, including the benchmark (see online supplementary material) and did not find major differences with our main results.
Avoidable mortality should be understood as an indicator of potential weaknesses with respect to healthcare and some public health policies and not as a definitive assessment.10 The number of deaths that should be considered avoidable is not clear.42 For instance, some researchers consider only half of heart disease mortality to be avoidable.43 44 There is no direct information to precisely measure percentages of avoidable mortality within cause groups in Mexico. Nonetheless, the difference between a given mortality schedule and the best mortality schedule of the same year can be conceived of as a minimal definition of avoidable mortality. The benchmark mortality schedule sets a lower bound to how much mortality could have been avoided. Certainly, even the best mortality schedule will contain elements of mortality that most would consider avoidable. To the extent that the components of the benchmark schedule were indeed attained somewhere in Mexico, one can view any excess mortality with respect to the benchmark schedule as presently avoidable. We believe this perspective improves on the AM concept by giving a directly measurable standard against which to estimate avoidable deaths.
Implications of findings
Beyond the mortality implications of the rise in homicide, violence has had a toll on perceived vulnerability in the country.15 The recent increase in homicides in some states could trigger an increase in the perception of vulnerability, which would result in a higher average lifetime experience of fear in specific states. Although we are not able to link the trends in mortality among young adults in Mexico with specific public policies, some evidence suggests that the propagation of homicide mortality is not only a result of the war between drug cartels but also because of the implementation of specific policies aimed to mitigate drug cartel operations after 2006.45 There is no simple way to lessen the impact of homicide mortality, but it is clear that the government has not been able to reduce its burden to levels observed before 2005. Furthermore, state homicide rates may underestimate the effect of violence in particular localities. For example, Guerrero in the South has two of the most dangerous cities in the world, iii but no information is available on the heterogeneity in homicide mortality for the rest of the state.
The fact that in 2015 older adults in Mexico could add more than 1 year of life in every state for males, and in 30 states for females by achieving the benchmark mortality levels, underscores vulnerability in these ages. Public health interventions targeting specific causes of death for this age group according to the epidemiological profile of each state would not only increase state life expectancy but it would also forge a path towards more equality between states in health outcomes. More than half of the potential gains in life expectancy between ages 50 and 84 are due to avoidable mortality, and to a large extent mortality related to health behaviours and medically amenable causes. For instance, obesity and overweight, risk factors for diabetes and IHD, have dramatically increased since the 1990s in low/middle-income countries because of the consumption of cheap, energy-dense food and reduced physical activity.46 Mexico, along with the USA, has the highest prevalence of overweight and obesity among all OECD (Organisation for Economic Co-operation and Development) countries20 and one of the highest in Latin America, along with Chile, El Salvador, Honduras and Paraguay.47 However, obesity prevalence is not homogeneous across Mexico. The highest rates of obesity are concentrated in the northern and central regions20 and in urban areas of the country,48 which roughly matches our regional pattern of IHD and diabetes mortality.
Conclusion
Mexico stands today at an advanced stage of the epidemiological transition.16 However, this transition was achieved rapidly and the health system is ill-prepared for the burden of non-communicable diseases.49 The cardiovascular mortality reductions that brought the developed world into advanced levels of life expectancy are still in progress in Mexico. Nevertheless, no single solution is available to reduce behavioural mortality in this country since, as we show, great heterogeneity in mortality levels exist between states.
Signs of a fragile situation in the health and mortality of the oldest age group are highlighted by the decline in the low mortality benchmark used in our analysis. Population ageing could scale up this situation if timely preventive measures are not put in place. Furthermore, a resurgence of violent deaths14 15 21 has created a new burden in Mexican society.
As is the case in many low/middle-income countries, Mexico will have to face these new challenges with a broad strategy. This should include a continuous and adaptable health system ready for the current and future health adversities at the physical, mental and societal levels. Many other institutions will also have to coevolve including importantly the development of an education system that embraces and encourages physical and healthy activities to diminish risk factors that contribute to the high prevalence of obesity and cirrhosis in Mexico. Finally, the burden of violence in recent years demonstrates the failure of current policies trying to mitigate violence in the country. New strategies that replace current ones are needed and embracing evidence-based policies (eg, drug policies) could be a new venue to eradicate the consequences of violence on the Mexican population.
Supplementary Material
Acknowledgments
JMA acknowledges the support from the Max Planck Society (LIFEINEQ group), the European Doctoral School of Demography and his current institution. All authors are grateful with the University Library of SDU for the Open Access fee.
Footnotes
The percentage of the population aged 65 or older is projected to go from 6.0% in 2015 to 10.2% in 2030 (Reference: CONAPO).
https://www.businessinsider.com.au/homicides-hit-new-high-mexico-alongside-increase-in-robberies-2017–11?r=US&IR=T.
JMA and TR contributed equally.
Contributors: JMA and TR contributed to data collection, study design, data analysis and interpretation of the results, and wrote the first draft of the paper. VC-R contributed to the study design, interpretation of the results, drafting of the paper and finalising the paper. JMA is the guarantor of this study.
Funding: This study was supported by Syddansk Universitet, Max-Planck-Gesellschaft (ERC grant no: 716323) and European Doctoral School of Demography.
Competing interests: None declared.
Patient consent: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: All data used are publicly available in references 22 and 23. All the study is fully replicable at https://github.com/jmaburto/DecompMex.
References
- 1. World Health Organization. The world health report 2000: health systems: improving performance. Geneva: World Health Organization, 2000. [Google Scholar]
- 2. Mexican Society of Demography. Conciliación demográfica de México y entidades federativas 1990–2010. Mexico City: SOMEDE-CONAPO, 2010. [Google Scholar]
- 3. Canudas-Romo V, García-Guerrero VM, Echarri-Cánovas CJ. The stagnation of the Mexican male life expectancy in the first decade of the 21st century: the impact of homicides and diabetes mellitus. J Epidemiol Community Health 2015;69:28–34. 10.1136/jech-2014-204237 [DOI] [PubMed] [Google Scholar]
- 4. Knaul FM, Frenk J. Health insurance in Mexico: achieving universal coverage through structural reform. Health Aff 2005;24:1467–76. 10.1377/hlthaff.24.6.1467 [DOI] [PubMed] [Google Scholar]
- 5. Neufeld LM. The oportunidades program and child growth: Mexico perspectives: handbook of growth and growth monitoring in health and disease: Springer, 2012:1659–71. [Google Scholar]
- 6. Sepúlveda J, Bustreo F, Tapia R, et al. Improvement of child survival in Mexico: the diagonal approach. Lancet 2006;368:2017–27. 10.1016/S0140-6736(06)69569-X [DOI] [PubMed] [Google Scholar]
- 7. Knaul FM, González-Pier E, Gómez-Dantés O, et al. The quest for universal health coverage: achieving social protection for all in Mexico. Lancet 2012;380:1259–79. 10.1016/S0140-6736(12)61068-X [DOI] [PubMed] [Google Scholar]
- 8. Bygbjerg IC. Double burden of noncommunicable and infectious diseases in developing countries. Science 2012;337:1499–501. 10.1126/science.1223466 [DOI] [PubMed] [Google Scholar]
- 9. Urquieta-Salomón JE, Villarreal HJ. Evolution of health coverage in Mexico: evidence of progress and challenges in the Mexican health system. Health Policy Plan 2016;31:28–36. 10.1093/heapol/czv015 [DOI] [PubMed] [Google Scholar]
- 10. Nolte E, McKee CM. Measuring the health of nations: updating an earlier analysis. Health Aff 2008;27:58–71. 10.1377/hlthaff.27.1.58 [DOI] [PubMed] [Google Scholar]
- 11. Nolte E, McKee M. Measuring the health of nations: analysis of mortality amenable to health care. BMJ 2003;327:1129 10.1136/bmj.327.7424.1129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Franco-Marina F, Lozano R, Villa B, et al. La mortalidad en México, 2000-2004. Muertes evitables: magnitud, distribución y tendencias: Dirección General de Información en Salud, Secretaría de Salud México, 2006. [Google Scholar]
- 13. Dávila-Cervantes CA, Agudelo-Botero M. Mortalidad evitable en México y su contribución a los años de vida perdidos: Análisis por grado de marginación estatal, 2001-2010. Papeles de población 2014;20:267–86. [Google Scholar]
- 14. Aburto JM, Beltrán-Sánchez H, García-Guerrero VM, et al. Homicides in mexico reversed life expectancy gains for men and slowed them for women, 2000-10. Health Aff 2016;35:88–95. 10.1377/hlthaff.2015.0068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Canudas-Romo V, Aburto JM, García-Guerrero VM, et al. Mexico’s epidemic of violence and its public health significance on average length of life. J Epidemiol Community Health 2017;71:188–93. 10.1136/jech-2015-207015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gómez-Dantés H, Fullman N, Lamadrid-Figueroa H, et al. Dissonant health transition in the states of Mexico, 1990-2013: a systematic analysis for the global burden of disease study 2013. Lancet 2016;388:2386–402. 10.1016/S0140-6736(16)31773-1 [DOI] [PubMed] [Google Scholar]
- 17. Whelpton PK, Eldridge HT, Seigel JS. Forecasts of the population of the United States, 1945-1975: US Govt. Print. Off, 1948. [Google Scholar]
- 18. Wunsch G. A minimum life-table for Europe. Europ Demogr Inf Bull 1975;5:2–10. 10.1007/BF02968526 [DOI] [Google Scholar]
- 19. Vallin J, Meslé F. Minimum mortality: a predictor of future progress? Population 2008;63:557–90. 10.3917/pope.804.0557 [DOI] [Google Scholar]
- 20. González-Pier E, Barraza-Lloréns M, Beyeler N, et al. Mexico’s path towards the sustainable development goal for health: an assessment of the feasibility of reducing premature mortality by 40% by 2030. Lancet Glob Health 2016;4:e714–e725. 10.1016/S2214-109X(16)30181-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gamlin J. Violence and homicide in Mexico: a global health issue. Lancet 2015;385:605–6. 10.1016/S0140-6736(15)60234-3 [DOI] [PubMed] [Google Scholar]
- 22. Frenk J. Bridging the divide: global lessons from evidence-based health policy in Mexico. Lancet 2006;368:954–61. 10.1016/S0140-6736(06)69376-8 [DOI] [PubMed] [Google Scholar]
- 23. INEGI. Estadísticas vitales Mortalidad: National Institute of Statistics Mexico, 2017. [Google Scholar]
- 24. CONAPO. Mexican population council: population estimates 2017. 2017. https://datos.gob.mx/busca/dataset/activity/proyecciones-de-la-poblacion-de-mexico (accessed 21 Apr 2017).
- 25. Patel KV, Peek MK, Wong R, et al. Comorbidity and disability in elderly Mexican and Mexican American adults: findings from Mexico and the southwestern United States. J Aging Health 2006;18:315–29. 10.1177/0898264305285653 [DOI] [PubMed] [Google Scholar]
- 26. Arriaga EE. Measuring and explaining the change in life expectancies. Demography 1984;21:83–96. 10.2307/2061029 [DOI] [PubMed] [Google Scholar]
- 27. Canudas-Romo V, Liu L, Zimmerman L, et al. Potential gains in reproductive-aged life expectancy by eliminating maternal mortality: a demographic bonus of achieving MDG 5. PLoS One 2014;9:e86694 10.1371/journal.pone.0086694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. González-González C, Sánchez-García S, Juárez-Cedillo T, et al. Health care utilization in the elderly Mexican population: expenditures and determinants. BMC Public Health 2011;11:192 10.1186/1471-2458-11-192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Camarda CG. Mortality smooth: an R package for smoothing poisson counts with p-splines. J Stat Softw 2012;50:1–24. 10.18637/jss.v050.i01 25317082 [DOI] [Google Scholar]
- 30. Wilmoth JR, Andreev K, Jdanov D, et al. Methods protocol for the human mortality database. 9 Rostock: University of California, Berkeley, and Max Planck Institute for Demographic Research, 2007:10–11. [Google Scholar]
- 31. Preston S, Heuveline P, Guillot M. Demography: measuring and modeling population processes. 2000.
- 32. Horiuchi S, Wilmoth JR, Pletcher SD. A decomposition method based on a model of continuous change. Demography 2008;45:785–801. 10.1353/dem.0.0033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Aburto JM, van Raalte A. Lifespan dispersion in times of life expectancy fluctuation: the case of Central and Eastern Europe. Demography. In Press;2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Remund A, Camarda CG, Riffe T. A cause-of-death decomposition of young adult excess mortality. Demography 2018;55:1–22. 10.1007/s13524-018-0680-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Zalsman G, Hawton K, Wasserman D, et al. Suicide prevention strategies revisited: 10-year systematic review. Lancet Psychiatry 2016;3:646–59. 10.1016/S2215-0366(16)30030-X [DOI] [PubMed] [Google Scholar]
- 36. Hernández B, Ramírez-Villalobos D, Romero M, et al. Assessing quality of medical death certification: concordance between gold standard diagnosis and underlying cause of death in selected Mexican hospitals. Popul Health Metr 2011;9:38 10.1186/1478-7954-9-38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Steinberg N. Neither rights nor security: killings, torture, and disappearances in mexico’s war on drugs: human rights watch. 2011.
- 38. Wright MW. Epistemological ignorances and fighting for the disappeared: lessons from Mexico. Antipode 2017;49:249–69. 10.1111/anti.12244 [DOI] [Google Scholar]
- 39. Gavin JR, Alberti KG, Davidson MB, et al. Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care 2003;26:S5–20. [DOI] [PubMed] [Google Scholar]
- 40. World Health Organization. Global health observatory data repository 2018. 2018;364. [Google Scholar]
- 41. World Health Organization. Enfermedades transmisibles y análisis de salud/información y análisis de Salud: situación de salud en las Américas: indicadores básicos 2013. OPS Washington, 2013. [Google Scholar]
- 42. Beltrán-Sánchez H. Avoidable mortality. International handbook of adult mortality: Springer, 2011:491–508. [Google Scholar]
- 43. Nolte E, McKee CM. In amenable mortality--deaths avoidable through health care--progress in the US lags that of three European countries. Health Aff 2012;31:2114–22. 10.1377/hlthaff.2011.0851 [DOI] [PubMed] [Google Scholar]
- 44. Holland WW. Commentary: should we not go further than descriptions of avoidable mortality? Int J Epidemiol 2003;32:447–8. 10.1093/ije/dyg157 [DOI] [PubMed] [Google Scholar]
- 45. Espinal-Enríquez J, Larralde H. Analysis of México’s narco-war network (2007-2011). PLoS One 2015;10:e0126503 10.1371/journal.pone.0126503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Hossain P, Kawar B, El Nahas M. Obesity and diabetes in the developing world--a growing challenge. N Engl J Med 2007;356:213–5. 10.1056/NEJMp068177 [DOI] [PubMed] [Google Scholar]
- 47. Aschner P. Obesity in Latin America In: Metabolic syndrome: a comprehensive textbook, 2016:33–9. [Google Scholar]
- 48. Kuri-Morales P, Emberson J, Alegre-Díaz J, et al. The prevalence of chronic diseases and major disease risk factors at different ages among 150,000 men and women living in Mexico City: cross-sectional analyses of a prospective study. BMC Public Health 2009;9:9 10.1186/1471-2458-9-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Rivera JA, Barquera S, Campirano F, et al. Epidemiological and nutritional transition in Mexico: rapid increase of non-communicable chronic diseases and obesity. Public Health Nutr 2002;5:113–22. 10.1079/PHN2001282 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2018-022350supp001.pdf (855.3KB, pdf)