Abstract
Entrapment of the sciatic nerve is considered a challenging problem for orthopaedic surgeons. Many surgical interventions (open or endoscopic) have been described as treatments. We describe an endoscopic technique for release of the piriformis tendon and sciatic nerve exploration by the lateral approach through an incision on the iliotibial band.
Pain around the gluteal region or the posterolateral hip has recently been a matter of interest in the literature. A recognized cause of this type of pain is related to the sciatic nerve and is frequently due to compression of the nerve by adjacent structures on its path within the subgluteal space.
The entrapment of the sciatic nerve has been commonly attributed to compression from fibrovascular structures, the muscle/tendon complex of the piriformis, obturator internus/gemelli, and/or proximal hamstrings.
Introduced by Robinson in 1947,1 the piriformis syndrome described clinical characteristics that included posterior buttock pain. Freiberg et al.2 previously developed a more succinct set of criteria, including tenderness at the sciatic notch, a positive Lasègue sign, and improvement with conservative therapy. More recently, Martin et al.3 have described a detailed clinical history and diagnostic tests for this condition.
A review of the literature on piriformis syndrome, sciatica, and other conditions associated with low back pain or posterior buttock pain shows that there are still issues of uncertainty and controversy related to the proper diagnosis and treatment of this condition.4, 5, 6, 7, 8, 9, 10
Decompression of the sciatic nerve at the level of the piriformis muscle has been described as a treatment for symptomatic sciatic nerve entrapment.11 This has been done traditionally through an open posterior approach with varying results. More recently, endoscopic release of the piriformis tendon and exploration of the sciatic nerve have been described, positioning the patient supine and using anterior lateral and posterior lateral portals with standard and long 70° arthroscopes.10
We describe a technique for endoscopic release of the piriformis tendon and exploration of the sciatic nerve with the patient in the lateral decubitus position using lateral portals through a window on the iliotibial band (ITB). A normal-length 4.0-mm 30° arthroscope is used.
Surgical Technique
The patient is positioned laterally on a regular operating table (no traction is necessary because hip arthroscopy is not performed with this procedure). The operative side is prepared and draped to allow for free mobility of the lower extremity. The greater trochanter (GT) is marked on the skin, and a spinal needle is positioned at the lateral aspect of the GT using fluoroscopy. A distal trochanteric portal is positioned 4 to 5 cm distal to the spinal needle, and a proximal trochanteric portal (PTP) is positioned 4 to 5 cm proximal to the spinal needle (Fig 1, Video 1). A standard-length 4.0-mm 30° arthroscope (Conmed Linvatec, Largo, FL) is introduced at the distal trochanteric portal, and the spinal needle is identified lateral to the ITB. A shaver is introduced through the PTP and directed toward the spinal needle. The tip of the shaver is identified endoscopically, and inflow with saline is started with the pump at 30 mm Hg. The shaver is used to dissect the fatty tissue from the ITB proximal and distal to the position of the spinal needle between the portals. Hemostasis is performed during this step with a radiofrequency bipolar ablation device (Conmed Linvatec), which is alternated with the shaver (Conmed Linvatec) from the PTP. Once the ITB is identified, a longitudinal cut is performed 3 to 4 cm proximal and distal to the spinal needle using a radiofrequency monopolar hook (Smith and Nephew, Andover, MA). Small horizontal cuts at the midportion of the longitudinal ITB cut may be performed anteriorly and posteriorly to facilitate instrument mobility (Fig 2, Video 1). The arthroscope is advanced through the incision on the ITB, and the greater trochanteric bursa is resected until the GT is clearly identified (internal and external rotation of the hip during this step facilitates adequate identification of the GT). With the GT clearly visible, the posterior corner is located arthroscopically and with the image intensifier. A shaver and a radiofrequency bipolar ablation device (Conmed Linvatec) are alternated to dissect and locate the tendon of the piriformis muscle at its insertion on the posterior aspect of the GT. Fluoroscopy is also used to confirm the piriformis insertion. The piriformis tendon is released from its insertion on the GT using a radiofrequency monopolar hook in a retrograde fashion (Figs 3 and 4, Video 1).
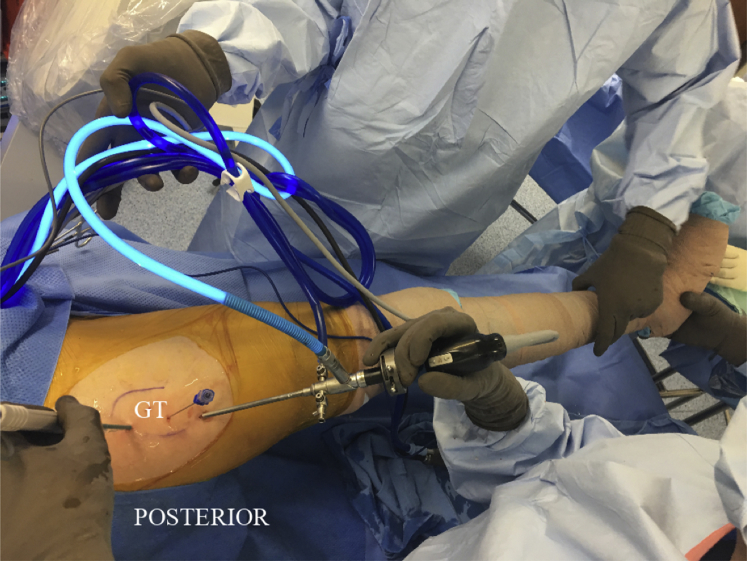
Fig 1.
Patient in the left lateral decubitus position. The right leg is draped free. A 30° arthroscope is positioned at the distal trochanteric portal. The radiofrequency ablation device is placed at the proximal trochanteric portal. The spinal needle is used to indicate the position of the lateral aspect of the greater trochanter (GT) as the incision on the iliotibial band is performed.
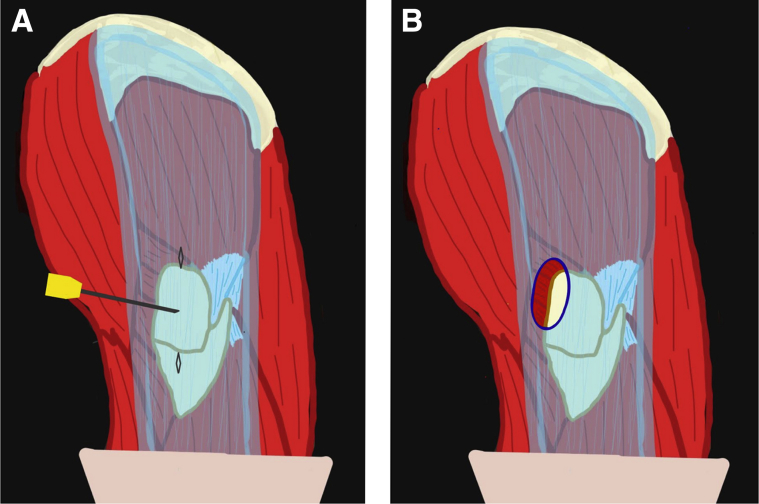
Fig 2.
Endoscopic incision on the iliotibial band, right hip. (A) The spinal needle is positioned lateral to the greater trochanter; it will serve as a guide to place the incision on the iliotibial band. (B) Defect on the iliotibial band when the incision is completed. The portals on the skin are demonstrated proximal and distal to the needle.
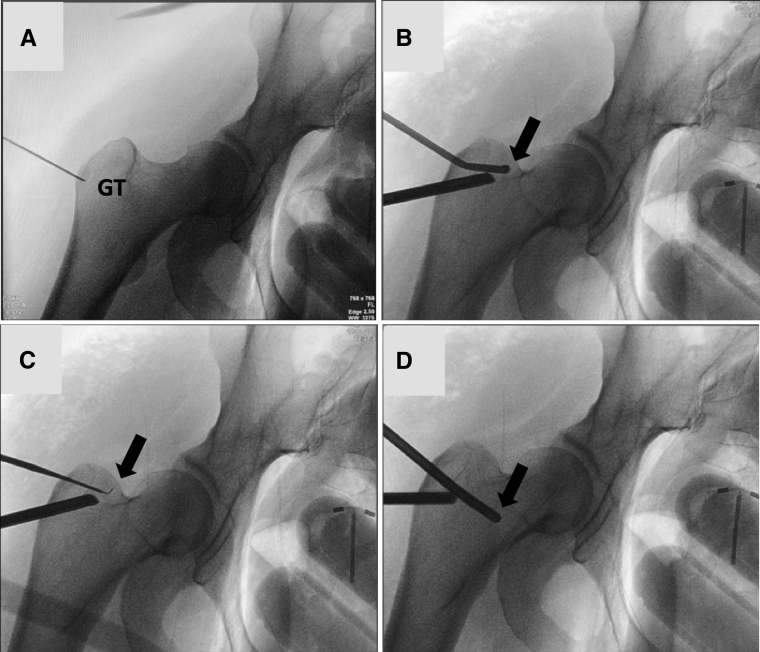
Fig 3.
Fluoroscopic series of the right hip demonstrating the piriformis release technique. (A) The spinal needle is placed on the lateral aspect of the greater trochanter (GT) to guide adequate placement of the incision on the iliotibial band. (B) A 30° arthroscope is positioned through the distal trochanteric portal and is viewing a radiofrequency ablation device (arrow), which is coming through the proximal trochanteric portal. The ablation device is used to dissect and expose the piriformis tendon close to its insertion at the GT. (C) A radiofrequency hook probe (arrow) is positioned through the proximal trochanteric portal and is used to release the piriformis tendon from its insertion on the GT as viewed with a 30° arthroscope positioned through the distal trochanteric portal. (D) A shaver is positioned through the proximal trochanteric portal and is advanced deeper posteriorly to the femur toward the sciatic nerve to release it from the muscle belly or fibrotic bands; a 30° arthroscope is positioned through the distal trochanteric portal.
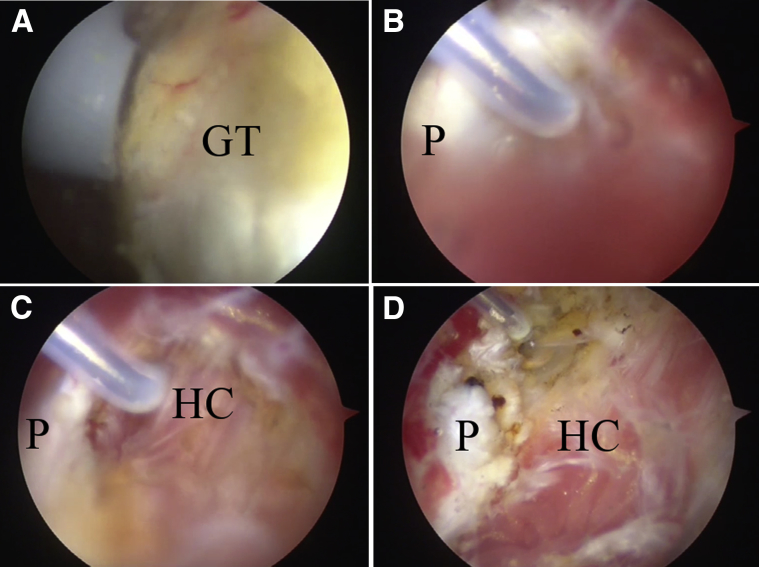
Fig 4.
Endoscopic series demonstrating the technique for release of the piriformis tendon of the right hip with the patient in the lateral decubitus position. (A) The radiofrequency ablation device is positioned through the proximal trochanteric portal toward the posterior superior corner of the greater trochanter (GT) as viewed with a 30° arthroscope positioned through the distal trochanteric portal. (B) A radiofrequency hook probe is positioned through the proximal trochanteric portal and is used to release the piriformis tendon (P); a 30° arthroscope is positioned through the distal trochanteric portal. (C) Halfway through the release of the piriformis tendon (P), the posterior hip capsule (HC) is visible under the tendon. (D) After the release is completed, the retracted stump of the piriformis tendon (P) is next to the posterior hip capsule (HC).
The arthroscope is advanced posteriorly, and the sciatic nerve is identified. Flexion and extension of the hip are carried out to confirm mobility of the sciatic nerve. Fibrovascular bands and adhesions compressing or restricting mobility of the sciatic nerve are identified and resected using the radiofrequency ablation device and a shaver (Conmed Linvatec; Fig 5, Video 1). Finally, hemostasis is verified and the portals on the skin are closed and draped.
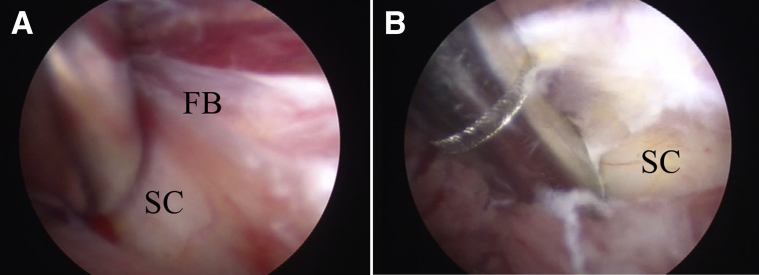
Fig 5.
Endoscopic series demonstrating the release of fibrous bands around the sciatic nerve of the right hip with the patient in the lateral decubitus position. (A) With a shaver positioned through the proximal trochanteric portal and once the sciatic nerve (SC) is located, release of the fibrotic bands (FB) around the nerve is performed. (B) The vasa nervorum increase on the sciatic nerve (SC) after release of the fibrous band. The shaver is positioned through the proximal trochanteric portal and is used to probe the nerve; a 30° arthroscope is positioned through the distal trochanteric portal.
Discussion
The reports in the literature are varied; most are case reports and small series with variable results. The largest cohorts were published by Fishman et al.,8 Indrekvam and Sudmann,12 and Benson and Schutzer.13 The results from these 3 studies showed an improvement achieving more than 50% symptom relief. Open surgical release was published by Byrd7 in 2005; he reported results in 7 patients: 5 patients were deemed to have an excellent result based on their extreme satisfaction because of complete alleviation of their preoperative symptoms, and the other 2 patients had limited improvement. In the study of Martin et al.11 describing an endoscopic release of the piriformis and sciatic nerve exploration in a cohort of 35 patients with a diagnosis of deep gluteal syndrome, the mean patient age was 47 years (range, 20 to 66 years). The mean duration of symptoms was 3.7 years (range, 1 to 23 years). The mean preoperative visual analog scale score was 6.9 ± 2.0, and the mean preoperative modified Harris hip score was 54.4 ± 13.1 (range, 25.3 to 79.2). The Benson outcome ratings were 11 excellent, 5 good, 2 fair, and 5 poor; these results are consistent with the results presented in this article. In our study, 1 patient (a man) had a fair outcome in the Benson outcome rating; in this case, the patient had concomitant pathologies (obesity, body mass index of 31.1, open surgery bursectomy, L5-S1 disc disease, diabetes mellitus, smoking), history of traumatic injury, and occasional narcotic use to control the pain but not the radicular symptoms, which were believed to be inconsequential compared with his preoperative pain. He returned to work and daily activities in 6 months.
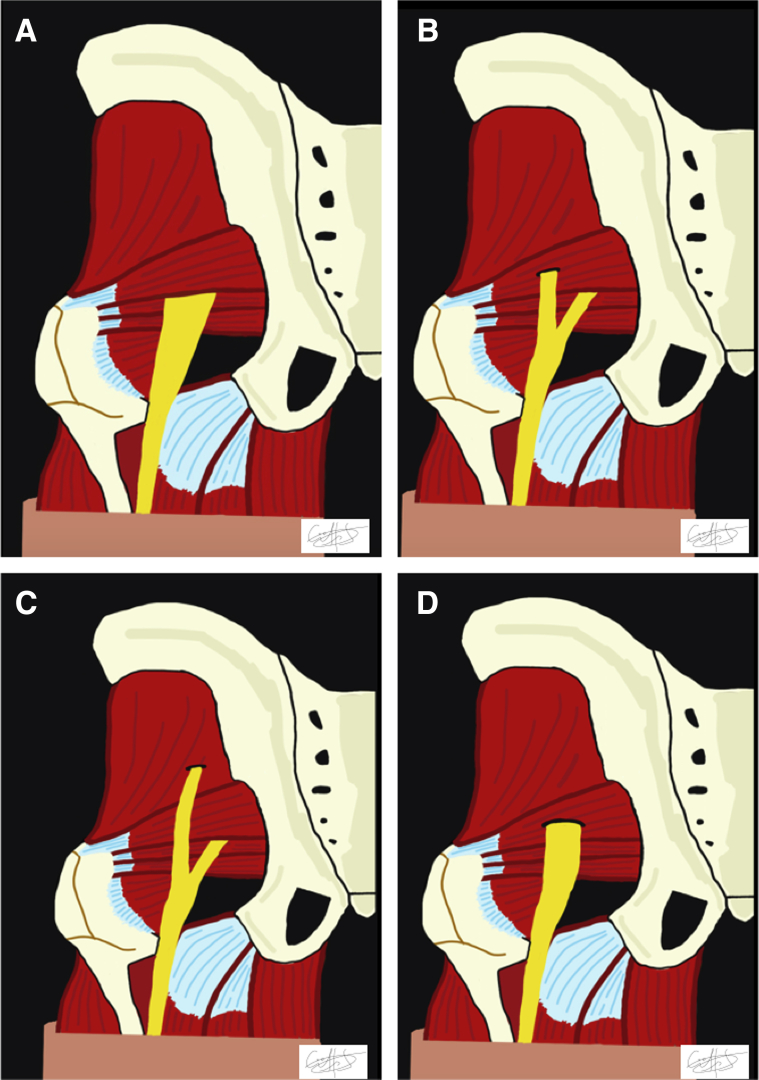
We have described an endoscopic technique to release the piriformis tendon with sciatic nerve exploration by the lateral decubitus approach through an incision on the ITB. This technique is described for the case of a sciatic nerve emerging as a single trunk under the muscle belly of the piriformis tendon (Fig 6, Table 1). We believe that this technique is highly reproducible and very safe to surrounding structures.
Fig 6.
Anatomic variants of the relationship between the sciatic nerve and the piriformis muscle. (A) Most common presentation, a single-trunk sciatic nerve that emerges under the muscle belly of the piriformis. (B) A bifurcated sciatic nerve in which one of the branches pierces through the piriformis muscle belly. (C) A bifurcated sciatic nerve in which the branches go above and below the muscle belly of the piriformis muscle. (D) A single-trunk sciatic nerve that pierces through the muscle belly of the piriformis.
Table 1.
Pearls and Pitfalls of the Endoscopic Release of the Piriformis Tendon and Sciatic Nerve Exploration
| Pearls | Pitfalls |
|---|---|
| Lateral release of the piriformis tendon (at its insertion on the greater trochanter) is indicated in the case of a single sciatic nerve that passes deeply to the muscle belly of the piriformis. | When the sciatic nerve pierces through the muscle belly of the piriformis, it must be released at the site of compression; the same is true for a bifurcated nerve that passes around or pierces the muscle belly of the piriformis. |
| The pump pressure is initially set at 30 mm Hg but can be safely increased to 50 mm Hg. | Adequate hemostasis is mandatory at every step of the procedure to obtain an adequate view of every structure. |
| Nerve monitoring may be needed at least for the initial learning curve for this procedure. | |
| Fluoroscopy guidance is advisable. | |
| Inexperience with proximal greater trochanter anatomy can negatively affect the outcome. |
The advantages of this technique are seen mainly in the endoscopic versus an open approach. Improved visualization and less soft-tissue and muscle damage are possible with the arthroscope. The lateral decubitus position allows surgeons to visualize the complex anatomy in this region. This helps prevent damage to important arteriovenous and neural structures.
The limitations of this technique are that intra-articular assessment of the hip is not performed concomitantly. However, it has been our experience that the two do not often occur together, so the limitation is not major.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: V.M.I. is a consultant for Conmed Linvatec, Depuy-Synthes, and Zimmer-Biomet. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The patient is positioned laterally on a regular operating table. The operative side is prepared and draped to allow for free mobility of the lower extremity. A standard length 4.0-mm 30° arthroscope (Conmed Linvatec, Largo, FL) is advanced through the incision on the ITB, and the greater trochanteric bursa is resected until the GT is clearly identified (internal and external rotation of the hip during this step facilitates adequate identification of the GT). With the GT clearly visible, the posterior corner is located arthroscopically and with the image intensifier. A shaver and a radiofrequency bipolar ablation device (Conmed Linvatec) are alternated to dissect and locate the tendon of the piriformis muscle at its insertion on the posterior aspect of the GT. Fluoroscopy is also used to confirm the piriformis insertion. The piriformis tendon is released from its insertion on the GT using a radiofrequency monopolar hook in a retrograde fashion. The arthroscope is advanced posteriorly, and the sciatic nerve is identified. Flexion and extension of the hip are carried out to confirm mobility of the sciatic nerve. Fibrovascular bands and adhesions compressing or restricting mobility of the sciatic nerve are identified and resected using the radiofrequency ablation device and a shaver. Finally, hemostasis is verified and the portals on the skin are closed and draped.
References
- 1.Robinson D.R. Piriformis syndrome in relation to sciatic pain. Am J Surg. 1947;73:355–358. doi: 10.1016/0002-9610(47)90345-0. [DOI] [PubMed] [Google Scholar]
- 2.Freiberg A.H., Vinke T.H. Sciatica and the sacroiliac joint. J Bone Joint Surg Am. 1934;16:126–136. [Google Scholar]
- 3.Martin H.D., Kivlan B.R., Palmer I.J. Nerve entrapment lesions of the hip and thigh. In: DeLee J.C., Drez D. Jr., Miller M.D., editors. DeLee and Drez’s orthopaedic sports medicine. Ed 4. Saunders Elsevier; Philadelphia: 2015. [Google Scholar]
- 4.Hopayian K., Song F., Riera R. The clinical features of the piriformis syndrome: A systematic review. Eur Spine J. 2010;19:2095–2109. doi: 10.1007/s00586-010-1504-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lewis A.M., Layzer R., Engstrom J.W. Magnetic resonance neurography in extraspinal sciatica. Arch Neurol. 2006;63:1469–1472. doi: 10.1001/archneur.63.10.1469. [DOI] [PubMed] [Google Scholar]
- 6.Filler A.G., Haynes J., Jordan S.E. Sciatica of non-disc origin and piriformis syndrome: Diagnosis by magnetic resonance neurography and interventional magnetic resonance imaging with outcome study of resulting treatment. J Neurosurg Spine. 2005;2:99–115. doi: 10.3171/spi.2005.2.2.0099. [DOI] [PubMed] [Google Scholar]
- 7.Byrd J.W.T. Piriformis syndrome. Oper Tech Sports Med. 2005;2:71–79. [Google Scholar]
- 8.Fishman L.M., Dombi G.W., Michaelsen C. Piriformis syndrome: Diagnosis, treatment, and outcome—A 10-year study. Arch Phys Med Rehabil. 2002;83:295–301. doi: 10.1053/apmr.2002.30622. [DOI] [PubMed] [Google Scholar]
- 9.Filler A.G. Piriformis and related entrapment syndromes: Diagnosis and management. Neurosurg Clin N Am. 2008;19:609–622. doi: 10.1016/j.nec.2008.07.029. [DOI] [PubMed] [Google Scholar]
- 10.Martin H.D., Atem M., Palmer I.J. Endoscopic sciatic nerve decompression: Operative technique. Oper Tech Sports Med. 2012;20:325–333. [Google Scholar]
- 11.Martin H.D., Shears S.A., Smathers A.M. The endoscopic treatment of sciatic nerve entrapment/deep gluteal syndrome. Arthroscopy. 2011;27:172–181. doi: 10.1016/j.arthro.2010.07.008. [DOI] [PubMed] [Google Scholar]
- 12.Indrekvam K., Sudmann E. Piriformis muscle syndrome in 19 patients treated by tenotomy—A 1- to 16-year follow-up study. Int Orthop. 2002;26:101–103. doi: 10.1007/s00264-001-0319-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Benson E.R., Schutzer S.F. Posttraumatic piriformis syndrome: Diagnosis and results of operative treatment. J Bone Joint Surg Am. 1999;81:941–949. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The patient is positioned laterally on a regular operating table. The operative side is prepared and draped to allow for free mobility of the lower extremity. A standard length 4.0-mm 30° arthroscope (Conmed Linvatec, Largo, FL) is advanced through the incision on the ITB, and the greater trochanteric bursa is resected until the GT is clearly identified (internal and external rotation of the hip during this step facilitates adequate identification of the GT). With the GT clearly visible, the posterior corner is located arthroscopically and with the image intensifier. A shaver and a radiofrequency bipolar ablation device (Conmed Linvatec) are alternated to dissect and locate the tendon of the piriformis muscle at its insertion on the posterior aspect of the GT. Fluoroscopy is also used to confirm the piriformis insertion. The piriformis tendon is released from its insertion on the GT using a radiofrequency monopolar hook in a retrograde fashion. The arthroscope is advanced posteriorly, and the sciatic nerve is identified. Flexion and extension of the hip are carried out to confirm mobility of the sciatic nerve. Fibrovascular bands and adhesions compressing or restricting mobility of the sciatic nerve are identified and resected using the radiofrequency ablation device and a shaver. Finally, hemostasis is verified and the portals on the skin are closed and draped.