Why was the cohort set up?
The World Trade Center Health Program (WTCHP) General Responder Cohort (the cohort) consists of workers and volunteers who were part of the rescue and recovery effort that followed the 11 September 2001 attack on the World Trade Center towers. Fire Department of New York (FDNY) and Pentagon and Shanksville responders are not included in this cohort but are covered by other similar programmes.
This self-selected, open, de facto cohort began to form within a month of 9/11when the rescue and recovery workers began presenting with a variety of respiratory complaints at Mount Sinai’s Irving J. Selikoff Center for Occupational and Environmental Medicine.1–4 In 2002, the National Institute for Occupational Safety and Health (NIOSH) provided funds to provide a one-time medical evaluation, and support for physical and mental health treatment came from philanthropic sources. NIOSH also provided funding, in 2004, for additional medical evaluations and, in 2006, for treatment of both physical and mental health conditions. With the passing of the James Zadroga 9/11 Health and Compensation Act of 2010, 5 more years of medical monitoring and treatment were provided.
Who is in the cohort?
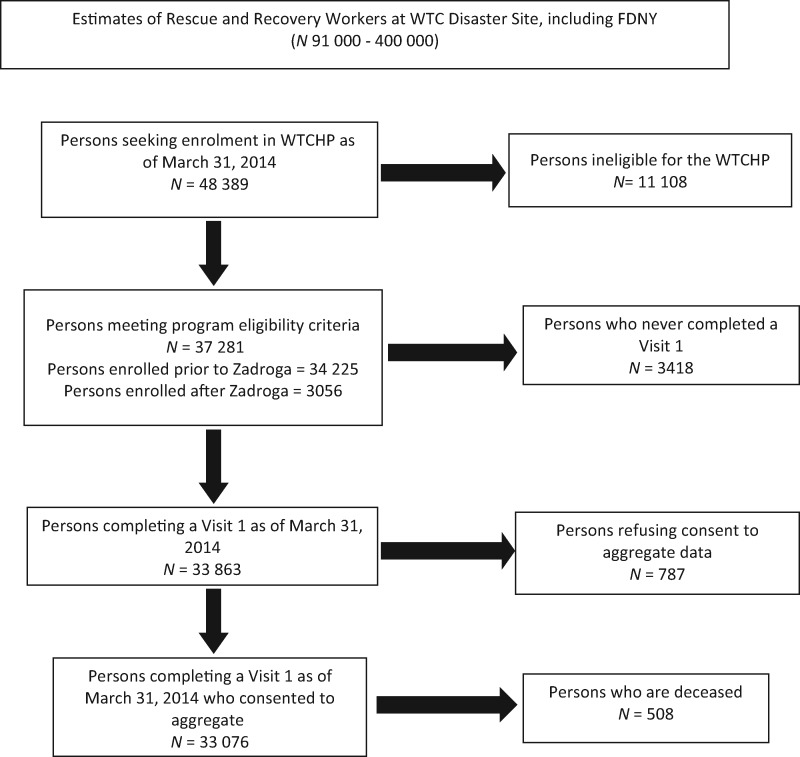
Estimates of how many rescue and recovery workers and volunteers worked on the WTC effort vary and may never be known, but the City of New York estimate is 91 000.5,6 As of 31 March 2014, the WTCHP had information on 48 389 potential enrollees (Figure 1), 34 225 of whom were eligible because of their participation in earlier programmes and 3056 more of whom were subsequently deemed eligible. Eligibility criteria are: (i) the person worked or volunteered on the WTC effort for either ≥4 h from 11 to 14 September 2001, or ≥24 h in September 2001 or ≥80 h from 11 September to 31 December 2001 (extended to July 2002 with the Zadroga Act); or (ii) the person handled and processed relevant human remains as a member of the Office of the Chief Medical Examiner for New York City; or (iii) the person worked for the Port Authority Trans Hudson Corporation (PATH) and spent ≥24 h between February 2002 and July 2002 cleaning PATH tunnels. Eligibility details are available elsewhere.7–9 Of the 37 281 deemed eligible, 33 863 (91%) completed a first visit and 33 076 of those (98%) consented to have their data aggregated. The WTCHP continues to enrol new members: from April 2012 to March 2014, the cohort grew by 138 per month, on average.
Figure 1.
CONSORT diagram showing the flow of responders through the WTCHP for the General Responder Cohort.
Cohort demographics and other key characteristics are shown in Table 1. As of 31 March 2014, the cohort was primarily male (86%), White (57%) and non-Hispanic (70%). The majority spoke English as their primary language (89%), most were married or partnered (62%), and the reported median annual income in 2001 was $50000–$60000. High school graduation was common (81%) and 60% reported having attended or graduated college. The cohort’s mean age was 38.7 years (standard deviation 8.8) on 11 September 2001 and 43.8 years (9.1) at the first visit.
Table 1.
Characteristics of WTC General Responder Cohort (N = 33 076)
| Variable | Entire sample | Have certified condition | No certified condition |
|---|---|---|---|
| N | 33 076 | 15 133 | 17 943 |
| Mean age (SD) in years | |||
| On 11 September 2001 | 38.69 (8.8) | 39.27 (8.7) | 38.2 (8.9) |
| At Visit 1 | 43.82 (9.1) | 44.5 (9.0) | 43.2 (9.1) |
| Age Groups at Visit 1: n (%) | |||
| 20 to 24 | 217 (0.7%) | 84 (0.6%) | 133 (0.7%) |
| 25 to 29 | 1138 (3.4%) | 424 (2.8%) | 714 (4.0%) |
| 30 to 34 | 3424 (10.4%) | 1342 (8.9%) | 2082 (11.6%) |
| 35 to 39 | 6330 (19.1%) | 2695 (17.8%) | 3635 (20.3%) |
| 40 to 44 | 7620 (23.0%) | 3522 (23.3%) | 4098 (22.9%) |
| 45 to 49 | 6064 (18.3%) | 2923 (19.3%) | 3141 (17.5%) |
| 50 to 54 | 4043 (12.2%) | 1989 (13.1%) | 2054 (11.5%) |
| 55 to 59 | 2421 (7.3%) | 1270 (8.4%) | 1151 (6.4%) |
| 60 to 64 | 1206 (3.7%) | 589 (3.9%) | 617 (3.4%) |
| 65 and older | 613 (1.9%) | 295 (1.9%) | 318 (1.8%) |
| Sex: n (%) | |||
| Female | 4759 (14.4%) | 2268 (15.0%) | 2491 (13.9%) |
| Male | 28 317 (85.6%) | 12 865 (85.0%) | 15 452 (86.1%) |
| Race: n (%) | |||
| African American | 3448 (10.4%) | 1332 (8.8%) | 2116 (11.8%) |
| Asian/Pacific Islander | 461 (1.4%) | 171 (1.1%) | 290 (1.6%) |
| White | 18 760 (56.7%) | 9162 (60.5%) | 9598 (53.5%) |
| Other | 1030 (3.1%) | 457 (3.0%) | 573 (3.2%) |
| Unknown | 9377 (28.4%) | 4011 (26.5%) | 5366 (29.9%) |
| Hispanic: n (%) | 7259 (21.9%) | 3427 (22.6%) | 3832 (21.4%) |
| Primary language | |||
| English n (%) | 28 376 (85.8%) | 12 453 (82.3%) | 15 923 (88.7%) |
| Marital status: n (%) | |||
| Married or partnered | 20 561 (62.2%) | 9645 (63.7%) | 10 916 (60.8%) |
| Education: n (%) | |||
| < High school graduate | 2305 (7.0%) | 1152 (7.6%) | 1153 (6.4%) |
| High school graduate | 6781 (20.5%) | 3210 (21.2%) | 3571 (19.9%) |
| Some college | 11 831 (35.8%) | 5357 (35.4%) | 6474 (36.1%) |
| College graduate | 8213 (24.8%) | 3725 (24.6%) | 4488 (25.0%) |
| Unknown | 3946 (11.9%) | 1689 (11.2%) | 2257 (12.6%) |
| Monitoring visits (SD) | 3.4 (2.1) | 4.4 (2.0) | 2.6 (1.8) |
Certification is the WTCHP mechanism by which responders receive treatment.7,10 Certification requires medical professional attestation that exposures present during the WTC effort (e.g. airborne toxins, heavy lifting or repetitive strains on muscles and joints from work performed on the WTC effort) played a significant role in aggravating, contributing to or causing the physical or mental health condition. As of 31 March 2014, 46% (15 133 of the 33 076) were certified for at least one WTC-related condition.
The WTCHP groups related conditions into ‘care suites’. a concept deployed by NIOSH via which responders certified for any condition within a given care suite may receive treatment for other conditions within that same care suite without further certification (the care suite for obstructive airway disease includes asthma and bronchitis, and the care suite for upper respiratory disease includes chronic rhinitis and chronic sinusitis, for example). For the 15 133 responders certified for a care suite (hereafter, ‘certified responders’), the most common physical health certifications were for upper respiratory disease (79%), gastroesophageal reflux disease (GERD) (60%) and obstructive airway disease (48%); 15% of certified responders were certified with post-traumatic stress disorder (PTSD) and 13% for depression; 8% of certified responders had cancer, with prostate and unspecified skin cancers being the most common; 90% of certified responders contended with medical conditions classified under two or more care suites.
How often have WTCHP responders been followed up?
Every cohort member has had at least one monitoring examination. The mean number of examinations for the cohort was 3.4 (2.1) (see Table 1) on 31 March 2014: 75% had had at least two examinations and 58% had had at least three. Second visits did not start until 2 years after the first; were originally scheduled for 18-month intervals; and are now annual. The median number of days between the first and second examinations is 799 days (∼2.2 years). For all other monitoring examination visit pairs (second-to-third, third-to-fourth, etc.), the median number of days between visits is 454 days (∼15 months).
Medical treatment data are available for ∼18 300 of the cohort who opted to use the WTCHP to address their needs. These data include all paid pharmacy, inpatient, emergency department and ambulatory care claims for WTC-related conditions and conditions medically associated with WTCHP-related conditions. Most of these data are from certified responders, but some are from responders who had diagnostic workups paid for by the WTCHP to determine their eligibility for free treatment from the WTCHP.
What has been measured?
Measures and data collection instruments are summarized in Table 2 shows the percentages of visits for which each data collection instrument was completed, and the number of each visit. and described more fully below. Table 3
Table 4.
Selected exposure characteristics for 33 076 WTCHP general responders
| Exposure characteristic | n (%) |
|---|---|
| Occupation category | |
| Protective services | 16 097 (49) |
| Construction | 6 781 (21) |
| CM & IRGa | 3 011 (9) |
| Other | 6 067 (18) |
| Missing | 1 120 (3) |
| Exposure indexb | |
| Very high | 1 034 (3) |
| High | 5 624 (17) |
| Intermediate | 20 092 (61) |
| Low | 4 777 (14) |
| Missing | 1 549 (5) |
| Dust cloud exposure | |
| Directly in dust cloud | 6 724 (20) |
| Significant dust | 5 604 (17) |
| Some dust | 2 343 (7) |
| No dust/early arrival (11–14 September 2001) | 9 773 (30) |
| No dust/late arrival (15 September and later 2001) | 7 325 (22) |
| Missing | 1 307 (4) |
| Duration on site (days) | |
| 0–14 | 7 381 (22) |
| 15–59 | 9 954 (30) |
| 60–119 | 7 411 (22) |
| ≥120 | 7 490 (23) |
| Missing | 840 (3) |
| Location of work | |
| On debris pile | 11 859 (36) |
| Not on debris pile | 20 149 (61) |
| Missing | 1 068 (3) |
aCleaning and Maintenance and (electrical, telecommunications and other) Installation and Repair Groups.
bExposure index is a combination of dust cloud exposure, duration on site and location of work.9
Table 2.
Names and descriptions of primary data collection instruments from the World Trade Center Health Program General Responder Cohort
| Programme enrolment measures | |
| Program eligibility | This information was initially collected via phone and later collected via mail and/or fax. Work location, potential exposures and worker category (e.g. police, construction worker, etc.) on the WTC rescue and recovery effort were among the items collected |
| Contact information | Includes full name, home address, phone numbers (home, work and mobile), and e-mail addresses |
| Demographics | Date of birth, sex and preferred language. Demographic information (race, ethnicity, marital status, educational attainment level, income level in 2001 and employment status) in addition to that collected during registration and enrolment is obtained at the first clinic visit via interviewer-administered medical questionnaire (IAMQ), a Patient Information Form and, until its discontinuation in 2010, a Self-Administered Medical Questionnaire (SAMQ) |
| Monitoring visit questionnaires | |
| Mail Home Questionnaire (MHQ) | Mailed to programme participants before their monitoring visits. The MHQ primarily acts as a memory recall assistance tool. It provides programme participants a means to prepare needed information: occupational and medical histories, medication history and current use, surgical procedures, diagnosed conditions, allergies, snoring, sleep apnoea and muscle or joint pain. Questions also capture marital status and reproductive history |
| Exposure Assessment Questionnaire (EAQ) | Collected at the first monitoring visit only. The EAQ is an interviewer-administered questionnaire used to assess exposures to potentially harmful physical and psychological conditions from work before 9/11, from work on the WTC recovery effort, and from current work. Questions ask about both overall exposure history and specific exposures related to work on the WTC recovery effort; hygiene at the WTC site; and the use of personal protective equipment at the WTC site |
| Interviewer-Administered Medical Questionnaire (IAMQ) | Collected at each monitoring visit. The IAMQ is a structured, medical history questionnaire that is administered by a trained medical professional. The IAMQ gathers information about medical conditions (e.g. self-reported symptoms, diagnostic testing and diagnosed medical conditions), family medical, alcohol and tobacco histories |
| Self-Administered Mental Health Questionnaire (SAMHQ) | Collected at second monitoring visit and at each subsequent monitoring visit. The SAMHQ’s primary focus is on self-reported mental health functioning. Questions are asked about general health (SF-12®), mental health symptoms (PTSD, panic disorder, generalized anxiety disorder, major depression), alcohol use and life stressors |
| Monitoring visit physical examination measures | |
| Physical examination (PE) | Performed at each monitoring visit. The PE is performed by a physician and takes 20 min to complete, on average. It includes measurements of height, weight, blood pressure, pulse rate and respiration. The physician also conducts musculoskeletal and neurological examinations, and examines the ears, eyes, nose, sinuses, throat, neck, chest, heart, abdomen, extremities and skin. Presence of musculoskeletal problems prompts the physician to perform more detailed and thorough examination with respect to complaints made by the responder. Findings are documented on a customized form |
| Laboratory tests | Collected at each monitoring visit. Clinical chemistry laboratory tests included during the examination include complete blood counts with differential and comprehensive metabolic panels, hepatic enzyme tests, lipid panels, lactate dehydrogenase, glomerular filtration rate and urinalysis. Laboratory test data are available for cohort members monitored by Mount Sinai’s Irving J Selikoff Center for Occupational and Environmental Medicine (Sinai); 55% of the cohort was monitored by Sinai as of 31 March 2014 |
| Pulmonary function test (PFT) | Pulmonary function is tested at each monitoring visit. Trained spirometry technicians measure PFT using spirometers which are calibrated daily via prescribed calibration methods. Technicians enter responder’s name, age and race (for normative comparison) into the spirometer. Baseline PFT examinations include pre- and post-bronchodilator PFTs. Since 2008, only pre-bronchodilator PFTs have been performed during monitoring visits |
Table 3.
Percentage of visits for which each data collection instrument was completed and visit count
| Instrument | Visit 1 | Visit 2 a | Visit 3 | Visit 4 | Visit 5 | Visit 6 | Visit 7 | Visit 8 | Visit 9 | Visit 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| EAQb | 98% | Administered at Visit 1 only | ||||||||
| SAMQc | 86% | Administered at Visit 1 only | ||||||||
| MHSQd | 97% | Administered at Visit 1 only | ||||||||
| IAMQe | 99% | 77% | 99% | 99% | 100% | 100% | 100% | 100% | 100% | 100% |
| SAMHQf | n/a | 95% | 96% | 95% | 94% | 88% | 83% | 88% | 95% | 87% |
| PEg | 99% | 71% | 96% | 97% | 98% | 99% | 99% | 100% | 100% | 100% |
| DISh | n/a | 70% | 29% | 28% | 27% | 26% | 25% | 26% | 24% | 20% |
| No. visits | 33 076 | 26 420 | 20 690 | 15 983 | 11 905 | 8183 | 5000 | 2430 | 782 | 60 |
aWith the exception of Visit 1, all visits are ongoing.
bExposure Assessment Questionnaire; cSelf-Administered Medical Questionnaire; dMental Health Screening Questionnaire (Visit 1 version of the SAMHQ); eInterviewer-Administered Medical Questionnaire; fSelf-Administered Mental Health Questionnaire; gPhysical Examination; hDiagnostic Interview Schedule; n/a = not applicable.
Eligibility, contact information and demographics
Two methods of cohort enrolment have been used. Until the end of June 2011, registration, eligibility determination and enrolment instruments were administered to all those who called a local New York City telephone number or a toll-free number or who sent in a form with a telephone number to receive a call from the Program’s Phone Bank. From 1 July 2011, potentially eligible participants completed and returned (faxed or mailed) for review a Responder Eligibility Application available from the federally run WTCHP website [www.cdc.gov/wtc/eligiblegroups.html]. Both methods obtained the information shown in Table 2, but only the initial method obtained union or organizational affiliation. The principal difference between the two enrolment methods is that the federal enrolment method seeks only demographic information and contact information, whereas the earlier method sought additional information such as maiden name where applicable, alternative address and full contact information for people who will always know how to contact the responder, in case WTCHP contact with the responder is lost. These additional data are now sought from the responder by the Data Center. Updates are solicited at subsequent visits.
General Information Form
The General Information Form is a brief survey given to each responder at each visit that asks for: current employment status; insurance coverage (if any); and Workers Compensation or Line of Duty claims (if any).
Interviewer-Administered Medical Questionnaire
Questions related to symptoms focus on the onset, duration, progression, triggers, relieving factors, diagnostic testing and previous evaluation by a physician. Responders are also asked about any symptoms other than those addressed by the questionnaire. Interviewer-Administered Medical Questionnaire (IAMQ) sections address the following areas of concern: lower respiratory, cardiovascular, reactive airway, upper respiratory, gastrointestinal, musculoskeletal systems, cancer (diagnoses and early signs) and general medical conditions (e.g. interstitial lung disease, diabetes).
Exposure Assessment Questionnaire
The particular potential hazards assessed via the Exposure Assessment Questionnaire (EAQ) are noxious substances (e.g. asbestos, silica dust, pesticides), high noise levels, ergonomic risk factors (e.g. repetitive motions, manual lifting, vibrations/impacts from use of tools), particular WTC-related tasks, and work in confined spaces. Self-reported exposure measures are checked for data integrity (e.g. data entry errors resulting in implausible or impossible numbers of hours worked). There is no independent exposure measure against which the self-reported exposures can be validated.
Self-Administered Medical Questionnaire
Until its use was discontinued in 2010, the Self-Administered Medical Questionnaire (SAMQ), completed at intake examinations, ascertained a wide variety of information including: self-report on any injuries and illnesses while working or volunteering on the WTC effort; claims filed with Workers’ Compensation, Social Security Income Disability, FEMA (Federal Emergency Management Agency), Unemployment Insurance or elsewhere, for any injuries or illnesses resulting from WTC work; demographics (income in 2001, current sources of income and benefits, number of children, marital status and educational attainment); and reproductive and sexual health.
Self-Administered Mental Health Questionnaire
In addition to the Self-Administered Mental Health Questionnaire (SAMHQ) completed at the second and subsequent monitoring visits described in Table 2, a baseline Mental Health Screening Questionnaire (MHSQ) was also administered. Baseline and follow-up SAMHQs differ slightly in their components but both address general health, post-traumatic stress disorder (PTSD), panic disorder, generalized anxiety disorder, major depression [and Center for Epidemiologic Studies Depression (CES-D) scale], daily activities performed in the past month, alcohol use and distressing events other than 9/11. They also both contain a life impact survey (e.g. major life events in the year before or since 9/11, experiences with death, work and retirement), questions on loss or injuries on 9/11, life experiences during or after 9/11, important sources of support, stress counselling or service needs, behavioural problems in their children since 9/11, and coping capabilities.
Diagnostic Interview Schedule
The Diagnostic Interview Schedule (DIS) is administered to every responder at the second visit and assesses psychological trauma, PTSD, depression and alcohol consumption. From the third visit on, a mental health clinician determines, based on results from the SAMHQ and the clinician’s assessment, which, if any, components of the DIS are to be administered.
Mail Home Questionnaire
The data that the responder records in the Mail Home Questionnaire (MHQ) are collected in the other instruments that are shown in Table 2 and described in this section.
Cancer Registry Links
Linkages [all Institutional Review Boad (IRB) approved] between the cohort and several state cancer registries (Connecticut, Florida, North Carolina, New Jersey, New York and Pennsylvania) as well as the National Death Index (NDI) exist. The most recent linkages are up to 2012 for the state cancer registry data, and up to the end of 2011 for the NDI.
What has been found?
The characteristics of the cohort are summarized in Tables 1 (general description), 3 (number of visits and instruments completed at each visit) and 4 (exposure characteristics).
A 5-year assessment found that 44% of previously asymptomatic responders had developed lower respiratory symptoms and 55% had developed upper respiratory symptoms.11 The conclusion at 5 years was that pulmonary function symptoms were prevalent and persistent. A 10-year assessment corroborated these findings and added to them.12 Cumulative incidences for asthma, sinusitis and abnormal spirometry were 27.6%, 42.3% and 41.8%, respectively.9 The incidence of sarcoid-like granulomatous pulmonary disease has been estimated to be 32 per 100 000 person-years, a rate that is elevated compared with published background rates.13
Multiple comorbidities in these responders are not uncommon: the analysis we report herein showed that, despite the fact that cardiovascular, renal, hepatic and diabetic conditions are not certifiable and thus not considered, 22% of the responders had two certified WTC conditions, 20% had three conditions and 15% had four conditions; 61 responders had 10 or more conditions. A syndrome of asthma, GERD and sinusitis has been observed in about 10% of the cohort. More than 20% of the cohort is suffering persistent physical and mental health problems. For example, the cumulative incidences for depression, PTSD and panic disorder in the non-police responders are 27.5%, 31.9% and 21.2%, respectively, and approximately 6% of the cohort suffers from all three (these figures might underestimate the true extent of mental health problems).14
Typical cancer latency periods (15–20 years) currently preclude assessment of a causal relationship between WTC exposure and cancer. Preliminary work has shown elevated standardized incidence ratios for all-cancer-sites-combined, thyroid, prostate, soft tissue and combined haematopoietic cancer.15 Increased thyroid and prostate rates are likely due to overdiagnosis bias.16 There is some indication that multiple myeloma might also be increased.17 Similar incidence rates for all the above cancers have been reported in other WTC-related cohorts.18
What are the main strengths and weaknesses?
The large cohort size, yearly assessment and data breadth and depth are the major strengths of this programme. Loss to follow-up leading to underestimation of particular certified conditions with long latencies is obviously a concern.
The large size and complexity of this cohort necessitates several caveats regarding this population: self-selection bias concerns arise from participation in the WTCHP being entirely voluntary, and it is difficult to assess how representative this cohort is of all WTC responders because of the substantial uncertainty in the total number of responders who worked on the WTC effort (and, consequently, what proportion of them are currently enrolled in the WTCHP).
Data collection methods present some limitations since most of the health information is self-reported. Onset and duration of symptoms, dates of diagnosis, or medications taken in the past can be difficult to recall. It is also important to consider recall bias. People may have joined the programme many years after 11 September 2001. Information such as when they started work on the WTC effort, their number of hours worked, the types of personal protective equipment they used and their perceived risk of exposure may be difficult to remember years after the fact and/or memories can be distorted by the emotional nature of the event.
Another limitation for many analyses is the lack of a suitable external control group for this unique cohort. Unlike the Fire Department of New York (FDNY), which performed yearly monitoring for all its firefighters and FDNY EMS (Emergency Medical Services) before 9/11, there is no consistent, reliable source of baseline data for our cohort. Finally, the healthy worker effect (i.e. workers commonly having lower rates of disease than the general population because severely ill and disabled individuals are less likely to be employed) can also contribute to the complexity of study of the cohort.19
Can I get a hold of the data? Where can I find out more?
Most of the data are available, cleaned annually 45 days after the anniversary of 9/11. Investigators wishing to learn more about the data available, or to request data from the General Responder Cohort Data Center of the WTCHP, can email: [WTCHPDataRequest@mssm.edu]. Please include a brief description of the research project. Applicants will be sent a Data Use Agreement to complete and, if applicable, must have Institutional Review Board approval for their study from their own institution before data can be released.
Funding
This publication was supported via contracts and grants 200‐2002‐00384, U10-OH008216/23/25/32/39/75 and 200‐2011‐39356/61/77/84/85/88 from the Centers for Disease Control and Prevention/National Institute for Occupational Safety and Health (CDC/NIOSH). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of CDC/NIOSH.
Profile in a nutshell
The WTCHP General Responder Cohort is a self-selected, open cohort of workers and volunteers who were part of the rescue and recovery effort following the 11 September 2001 attack on the World Trade Center. The cohort was set up to meet the de facto health needs of the responders.
The cohort consists of 33 076 people who worked on the World Trade Center rescue and recovery effort.
An initial examination is followed by annual monitoring examinations. Examinations include a physical examination, pulmonary function tests, blood analyses, questionnaires and interviews.
Datasets include results from physical examinations, pulmonary function tests, blood analyses and responses to questionnaires and interviews which query exposures to noxious substances as well as physical and mental health symptoms and conditions. Medical claims are available for cohort members who receive free treatment through the programme. Linkages exist to several state cancer registries and to the National Death Index.
To learn more about data availability, please email a brief description of a planned research project to: [WTCHPDataRequest@mssm.edu]. Applicants will be sent a Data Use Agreement to complete and, if applicable, must have Institutional Review Board approval for their study from their own institution before data can be released.
Acknowledgements
We are grateful to: the responders; all past and present staff of the Programmes; the work force, community and volunteer organization programme stakeholders; and the philanthropic sources that funded treatment from 2003 to 2006.
Conflict of interest: None declared.
References
- 1. Levin S, Herbert R, Skloot G et al. Health effects of World Trade Center site workers. Am J Ind Med 2002;42:545–47. [DOI] [PubMed] [Google Scholar]
- 2. Skloot G, Goldman M, Fischler D et al. Respiratory symptoms and physiologic assessment of ironworkers at the World Trade Center disaster site. Chest 2004;125:1248–55. [DOI] [PubMed] [Google Scholar]
- 3. Levin S, Herbert R, Moline J et al. Physical health status of World Trade Center rescue and recovery workers and volunteers – New York City, July 2002–August 2004. MMWR 2004;53:807–12(reprinted in JAMA 2004;292:1811–13). [PubMed] [Google Scholar]
- 4. Landrigan P, Lioy P, Thurston G et al. Health and environmental consequences of the World Trade Center disaster. Environ Health Perspect 2004;112:731–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. New York City. 9/11 Health: Rescue and Recovery Workers.http://www nyc gov/html/doh/wtc/html/rescue/rescue shtml 2014 [8 September 2104, date last accessed].
- 6. Savitz D, Oxman R, Metzger K et al. Epidemiologic research on man-made disasters: strategies and implications of cohort definition for World Trade Center worker and volunteer surveillance program. Mount Sinai J Med 2008;75:77–87. [DOI] [PubMed] [Google Scholar]
- 7. Centers for Disease Control and Prevention. World Trade Center Health Program Requirements for Enrollment, Appeals, Certification of Health Conditions, and Reimbursement. Druid Hills, GA: CDC, 2011. [Google Scholar]
- 8. Centers for Disease Control and Prevention. World Trade Center Health Program Requirements for the Addition of New WTC-Related Health Conditions. Druid Hills, GA: CDC, 2011. [Google Scholar]
- 9. Wisnivesky J, Teitelbaum S, Todd A et al. Persistence of multiple illnesses in World Trade Center rescue and recovery workers: a cohort study. Lancet 2011;378:888–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Centers for Disease Control and Prevention. World Trade Center Health Program; Amendments to List of WTC-Related Health Conditions; Cancer; Revision. Druid Hills, GA: CDC, 2014. [Google Scholar]
- 11. Herbert R, Moline J, Skloot G et al. The World Trade Center disaster and the health of workers: five-year assessment of a unique medical screening program. Environ Health Perspect 2006;114:1853–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lucchini R, Crane M, Crowley L et al. The World Trade Center health surveillance program: results of the first 10 years and implications for prevention. G Ital Med Lav Erg 2012;34(Suppl 3):529–33. [PubMed] [Google Scholar]
- 13. Crowley LE, Herbert R, Moline JM et al. “Sarcoid like” granulomatous pulmonary disease in World Trade Center disaster responders. Am J Ind Med 2011;54:175–84. [DOI] [PubMed] [Google Scholar]
- 14. Ghuman SJ, Brackbill RM, Stellman SD, Farfel MR, Cone JE. Unmet mental health care need 10‐11 years after the 9/11 terrorist attacks: 2011‐2012 results from the World Trade Center Health Registry. BMC Public Health 2014;22:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jordan HT, Stellman SD, Morabia A et al. Cardiovascular disease hospitalizations in relation to exposure to the September 11, 2001 World Trade Center disaster and posttraumatic stress disorder. J Am Heart Assoc 2013;2:e000431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Solan S, Wallenstein S, Shapiro M et al. Cancer incidence in World Trade Center rescue and recovery workers, 2001‐2008. Environ Health Perspect 2013;121:699–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Moline JM, Herbert R, Crowley L et al. Multiple myeloma in World Trade Center responders: a case series. J Occup Environ Med 2009;51:896–902. [DOI] [PubMed] [Google Scholar]
- 18. Li JH, Cone JE, Kahn AR et al. Association between World Trade Center exposure and excess cancer risk. JAMA 2012;308:2479–88. [DOI] [PubMed] [Google Scholar]
- 19. Choi BCK. Definition, sources, magnitude, effect modifiers, and strategies of reduction of the healthy worker effect. J Occup Environ Med 1992;34:979–88. [PubMed] [Google Scholar]