Abstract
The liver transplantation program at KFSHRC has been active since 2001. More than 450 liver transplants have been performed so far. The program evolved from adult cadaveric transplant to living donor and recently to pediatric and split techniques. The 1-year survival of patients for both pediatric and adult exceeded 90% and the 5-year survival of patients is more than 80%. Associated with this success are challenges that include: organ shortage, quality of organ harvested, inability to meet the growing national need, increased demand of resource to meet the need of the program, and lack of a collaborative national strategy in organ donation and transplantation.
Though accurate epidemiological studies in Saudi Arabia (SA) on liver disease are generally lacking, it is estimated that between 700 and 1200 patients need liver transplantation annually. The need for transplantation forced patients to seek transplants abroad with inferior outcomes occasionally.1
Liver transplantation in SA was started in the early nineties to meet the need of patients with an end-stage liver disease.2,3 Several programs were started at a low scale.
Liver transplantation at King Faisal Hospital and Research Center (KFSHRC) was launched in 2001 and is continued to be active till date. Currently, the program performs living and cadaveric transplantation in children and adults. Recently, a split program was introduced. In this article, we describe the general performance of the split program over more than a decade, focusing specifically on mortality timing as an indicator of the quality of care at different stages of the transplant process. We also try to highlight the challenges faced from donor and recipient perspectives as well as what lies ahead in the context of the national need and available resources.
Method and Result
We retrospectively analyzed the patients who were transplanted from 2001 until the end of 2012. We specifically looked at the following 5 mortality indicators: mortality within 24 hours, mortality within hospital stay, mortality with normal functioning graft, mortality without normal functioning graft, and late mortality (after discharge).
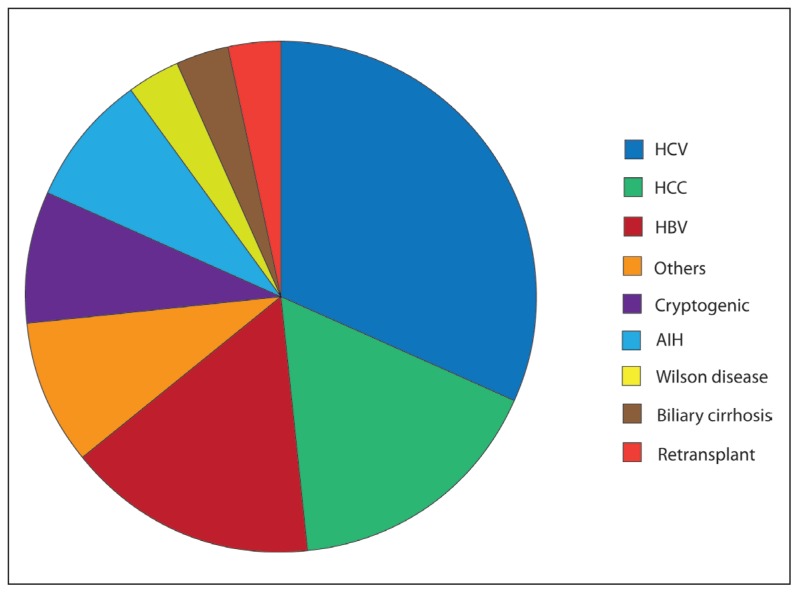
The total number of transplants were 478 (adult: 387 and pediatric: 91). The patients were stratified on the basis of the year they were transplanted. The mortality in each of patient cohorts was calculated and the patients were stratified according to the 5 mortality categories. Table 1 summarizes mortality data related to the timing, and Table 2 indicates the cause of death. Figure 1 summarizes the indication for transplant. The subgroup analysis of adult living donor stratified to MELD (model for end-stage liver disease) above and below 25 showed mortality of 15.4% versus 31%, respectively.
Table 1.
Mortality indicators of liver transplantation at KFSHRC from 2001–2012.
| Year | No. | Mortality | Total (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| LDLT | DDLT | TOTAL | Peri-operative (24 h) | Graft failure | Normal graft | ||||
| Hospital stay | Late mortality | Early mortality | Late mortality | ||||||
|
| |||||||||
| 2001 | 0 | 6 | 6 | 1 | 1 | 2 (33%) | |||
| 2002 | 1 | 6 | 7 | 1 | 1 (14%) | ||||
| 2003 | 2 | 7 | 9 | 1 | 1 (11%) | ||||
| 2004 | 17 | 14 | 31 | 3 | 5 | 3 | 11 (35%) | ||
| 2005 | 14 | 15 | 29 | 1 | 4 | 1 | 6 (21%) | ||
| 2006 | 10 | 25 | 35 | 3 | 6 | 9 (25.7%) | |||
| 2007 | 9 | 29 | 38 | 1 | 3 | 1 | 2 | 7 (18%) | |
| 2008 | 7 | 34 | 41 | 2 | 1 | 1 | 3 | 7 (17%) | |
| 2009 | 17 | 29 | 46 | 5 | 2 | 2 | 9 (20%) | ||
| 2010 | 15 | 31 | 46 | 3 | 2 | 5 (11%) | |||
| 2011 | 66 | 23 | 89 | 4 | 1 | 2 | 7 (8%) | ||
| 2012 | 76 | 25 | 101 | 2 | 6 | 3 | 11 (11%) | ||
| TOTAL | 234 | 244 | 478 | 5/478 (1.1%) | 21/478 (4.4 %) | 15/478 (3.1%) | 16/478 (3.3%) | 19/478 (4%) | 76 |
LDLT: Living donor liver transplant, DDLT: Deceased donor liver transplant.
Table 2.
Mortality-related complications post-liver transplantation. Multiple causes of death are counted.
| Type of complication | Number of patients |
|---|---|
|
| |
| PNF | 10 |
| HCV recurrence | 6 |
| De novo malignancy | 8 |
| Sepsis | 19 |
| Other disease recurrence | 2 |
| Organ failure | 18 |
| Vascular complications | 8 |
| Tumor recurrence | 7 |
| Small for size syndrome | 2 |
| Chronic rejection | 1 |
| PSC | 1 |
| CPM | 1 |
| GVHD | 2 |
PNF: Primary Non Function; HCV: Hepatitis C Virus, PSC: Primary Sclerosing Cholangitis CPM: Central Pontine Myelitis; GVHD: Graft-Vs-Host Disease.
Figure 1.
Indications for liver transplantation.
The most common indication in adults was hepatitis C cirrhosis (38%). Hepatocellular was the main indication in almost 20% of the cases. Milan criteria were generally applied4 and were extended to the University of San Francisco for living donor liver transplant.5 The number of referrals to KFSHRC for liver transplant exceeds 650 annually, and between 55% and 65% cases are accepted for evaluation. The average number of the cadaveric waiting list is between 60 and 80, with the waiting list mortality of 20% to 30%.
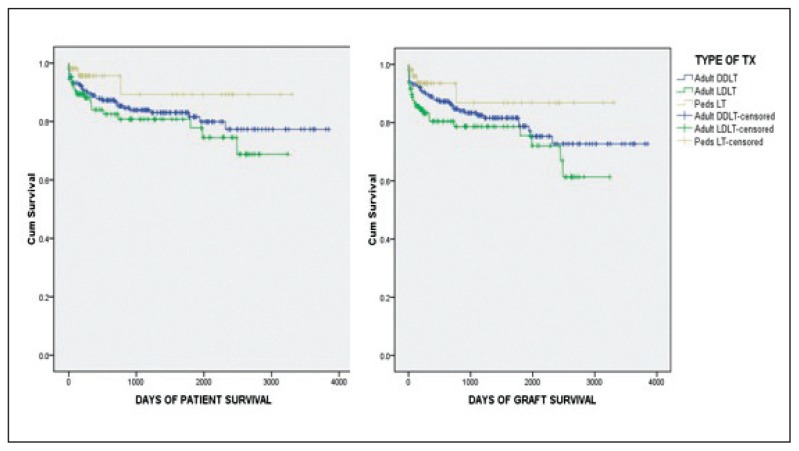
Initially only cadaveric transplant was performed; early on living donor liver transplant was introduced, which made up one third of the total number of transplants. In the last 2 years, living donor liver transplant made more than two third of the total number of transplants. Other salient feature of the program included the introduction of split-liver transplantation, which was performed in 3 donors. Re-transplantation was performed in 14 patients (2.9%) with the 65% survival rate. The Kaplan-Meier graft and patient survival for the whole program up to 2011 is shown in Figure 2.
Figure 2.
Actuarial Kaplan-Meier graft and patient survival in DDLT, LDLT, and pediatric transplant (Peds LT) from 2001–2011).
Discussion
Starting and sustaining a successful liver transplantation program is a major undertaking for any institution no matter how advanced its setup is. At KFSHRC, the quality of the program has been comparable to the international standard since its inception in 2001. The scaling up of the program was difficult early on; however, after easing of many administrative and logistical obstacle, the number of transplant has doubled over 2011 to 2012 and continued to grow maintaining the same quality.
The demand of the program has increased with the increasing number of referrals. Though the need is partially met by living donor liver transplant, the situation with cadaveric transplant is not as good. Patients have been accumulating on the waiting list, with more than one third either die or get delisted as a result of severe organ shortage and late referrals. Our data also indicated an inferior result of living donors in high MELD recipients who were referred late. The pediatric population not having a living donor has been a major problem that the program faced. Though split graft is becoming a standard of practice to the extent of questioning the need for pediatric living donor liver transplant,6 the case in SA is not the same. Though we efficaciously managed to do a successful split, the scarcity of organs combined with the poor quality of these organs made split grafting a rare occurrence. The quality of organ in SA remains to be problematic secondarily to logistical issues. As a matter of fact, when the program was managed by an overseas team in 1994, the rate of primary non-function was as high as 25% with a much higher graft dysfunction.7
Several authors uncovered donor risk factors that may influence the outcome of liver transplantation. These risk factors in general are as follows: donor demographics, donor disease, donor cause and mechanism of death, and allocation factor.8 A composite risk factor was also proposed.9,10 It remains to be seen whether these factors are applicable to the donor population in Saudi Arabia wherein issues in the medical management of donor seems to be more important.
It is estimated that more than 250 organs could be produced annually, wherein currently the number of cadaveric liver transplant did not exceed 100 in the country.11 A joint effort between Saudi Center for Organ Transplantation, Ministry of Health hospitals, and Transplant Center need to take a much more accelerated pace to streamline the organ donation process at the national level.12 It is unlikely that living donor liver transplant will meet the need of patients with the end-stage organ failure in SA; it is also not possible that one institution will be able to cope with the burden of a large liver transplantation program. It is suggested that an aggressive and proactive approach toward organ donation be pursued to support the 4 liver transplantation programs in SA and that adequate resources be made available to them to meet the needs for liver transplant for patients with the end-stage liver failure.
Conclusion
The experience at KFSHRC with the liver transplantation program demonstrated that major medical institutions in SA can sustain a successful liver transplantation program with the quality comparable to the programs in Europe and North America. A major reform in the organ donation program logistics needs to be undertaken as soon as possible to make use of the big potential of cadaveric donation. Major medical institutions are required to understand the needs for their transplantation programs in terms of resource and administrative support. The mechanism to reward these governmental medical institutions, which has chosen to harness liver transplantation, need to be established by decision makers at a higher level.
REFERENCES
- 1.Allam N, Al Saghier M, el Sheikh Y, et al. Clinical outcomes for Saudi and Egyptian patients receiving deceased donor liver transplantation China. Am J Transplant. 2010;10:1834–1841. doi: 10.1111/j.1600-6143.2010.03088.x. [DOI] [PubMed] [Google Scholar]
- 2.Jawdat M, Qattan N, Bassas A, Al Karawi MA, Mohamed E, Khallil H. The first liver transplant in Saudi Arabia and the Arab world. Hepatogastroenterology. 1993;40:297–300. [PubMed] [Google Scholar]
- 3.Al Sebayel MS, Ramirez CB, Abou Ella K. The first 100 liver transplants in Saudi Arabia. Transplant Proc. 2001 Aug;33(5):2709. doi: 10.1016/s0041-1345(01)02155-8. [DOI] [PubMed] [Google Scholar]
- 4.Mazzaferro V, Regalia E, Doci R, Andreola S, Pulvirenti A, Bozzetti F, Montalto F, Ammatuna M, Morabito A, Gennari L. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996;11:693–9. doi: 10.1056/NEJM199603143341104. [DOI] [PubMed] [Google Scholar]
- 5.Yao FY, Ferrell L, Bass NM, Watson JJ, Bacchetti P, Venook A, Ascher NL, Roberts JP. Liver transplantation for hepatocellular carcinoma: expansion of the tumor size limits does not adversely impact survival. Hepatology. 2001;6:1394–4. doi: 10.1053/jhep.2001.24563. [DOI] [PubMed] [Google Scholar]
- 6.Emre S, Umman V. Split liver transplantation: an overview. Transplant Proc. 2011 Apr;43(3):884–7. doi: 10.1016/j.transproceed.2011.02.036. [DOI] [PubMed] [Google Scholar]
- 7.Rezeig M, Nezamuddin N, Abdulkarim A, Pruet T, Ali A, Ahmed R, Al Quiz M, Shabib S. Orthotopic Liver Transplantation at King Faisal Specialist Hospital and Research Center: 1994–1995. Saudi Journal of Kidney Disease and Transplantation. 1996;7(2):182–184. [PubMed] [Google Scholar]
- 8.Freeman. Deceased donor risk factors influencing liver transplant outcome. Transplant International. 2013;26:463–470. doi: 10.1111/tri.12071. [DOI] [PubMed] [Google Scholar]
- 9.Feng S, Goodrich NP, Bragg-Gresham JL, et al. Characteristics associated with liver graft failure: the concept of a donor risk index. Am J Transplant. 2006;6:783. doi: 10.1111/j.1600-6143.2006.01242.x. [DOI] [PubMed] [Google Scholar]
- 10.Braat AE, Blok JJ, Putter H, et al. The Eurotransplant Donor Risk Index in Liver Transplantation: ET-DRI; for the European Liver and Intestine Transplant Association (ELITA) and Eurotransplant Liver Intestine Advisory Committee (ELIAC) Am J Transplant. 2012;12:2789. doi: 10.1111/j.1600-6143.2012.04195.x. [DOI] [PubMed] [Google Scholar]
- 11.Al-Sebayel M, Al-Enazi A, Al-Sofayan M, et al. Improving organ donation in central Saudi Arabia. Saudi Med J. 2004;25:1366–8. [PubMed] [Google Scholar]
- 12.Al-Sebayel M. The status of cadaveric organ donation for liver transplantation in Saudi Arabia. Saudi Med J. 2002;23:509–1. [PubMed] [Google Scholar]