Abstract
BACKGROUND AND OBJECTIVES
Vitiligo is a difficult disease to treat. Recently, a 308-nm excimer laser has been shown to be effective in treating vitiligo. In addition, the patients with vitiligo have impairment in their quality of life. The aim of the study was to investigate the clinical efficacy, safety, and psychosocial impact after treating vitiligo with the 308-nm excimer laser.
DESIGN AND SETTINGS
A prospective clinical trial conducted at dermatology clinics of hospitals affiliated with Qassim University, Saudi Arabia, from May 2012 to February 2013.
PATIENTS AND METHODS
Forty-eight patients with 105 vitiliginous patches were treated using a 308-nm excimer laser. The treatment was performed twice per week for a maximum of 48 treatments or 100% repigmentation of lesions whichever was achieved first. The assessment of the clinical response and recording of side effects were performed biweekly.
RESULTS
Out of 105 lesions in these patients, 63 lesions (60.0%) achieved over 75% repigmentation by laser treatment, 12 lesions (11.4%) showed 51% to 75% repigmentation, 9 lesions (8.6%) showed 26% to 50% repigmentation, and another 9 lesions (8.6%) showed 1% to 25% repigmentation, while 12 lesions (11.4%) showed no repigmentation. The average (±standard deviation [SD]) number of sessions needed to achieve repigmentation was 16.8 (8.0), whereas the average (±SD) number of sessions needed to realize Grade IV repigmentation was 20.2 (15). The type of repigmentation varied between lesions. Diffuse repigmentation was the most common pattern and occurred in 34 lesions (36.6%). Facial lesions responded better than lesions located elsewhere. Skin type did not play a statistically significant role (P=.07) in the lesions response to treatment. All side effects were mild and disappeared shortly after end of treatment sessions.
CONCLUSION
The clinical data indicate that the treatment of vitiligo using the 308-nm excimer laser is effective and safe and improves psychosocial quality of life. Lesion location, duration of disease, and treatment duration are factors affecting the clinical and psychological outcome.
Vitiligo is a common idiopathic, acquired disorder of cutaneous depigmentation. It affects 1% to 2% of the population with no predilection for age, sex, or racial background.1,2 Although there are several theories, including genetic, autoimmune, self-destructive, biochemical, and neuromechanism, the exact pathogenesis of the disease remains unknown.3,4 Various medical and surgical therapeutic options have been proposed to achieve repigmentation in the lesions or to stabilize the disease; however, the treatment of vitiligo still seems to be challenging.5
Recently, a 308-nm excimer laser has been shown to be a promising treatment for localized vitiligo.6,7 It also offers a hopeful treatment for UV-sensitive areas.8 The usefulness of the 308-nm excimer laser for treating vitiligo was demonstrated in many studies; however, the results of these studies suggest heterogeneity of responses depending on many clinical and demographic variables of patients.9–12
People affected by vitiligo have their quality of life deteriorated to a great extent.13–15 The disease produces an important psychological burden.16 It has been suggested that patients with vitiligo suffer from poor body image, low self-esteem and experience, and a considerable level of disability. Many patients are significantly distressed, especially in relation to social activities or negative reactions of others. The disease may also have a negative effect on sexual relationships.17 As the clinicians’ view of disease severity or quality of life does not necessarily correlate with the patient’s perception of disability caused by the disease,18 it is important to obtain a patient-based measurement of psychological impact on the patient life with the aim to evaluate the full impact of the disease. The purpose of this study was to investigate the clinical efficacy and the psychosocial impact on the patient life after the use of a 308-nm excimer laser in the treatment of vitiligo and to compare the clinical and demographic variables (age, sex, location of lesions, skin type, disease duration, etc.) influencing the treatment response.
PATIENTS AND METHODS
This was a clinical trial conducted at the dermatology clinics of Qassim University–affiliated hospitals, Saudi Arabia, between May 2012 and February 2013. Patients with vitiliginous lesions at different body sites were approached to participate in the study. Patients who had stable vitiligo and were not on any treatment for the last 8 weeks were enrolled in the study. After they were explained the treatment procedure and the possible side effects, their informed consents were taken for the treatment and photographs, and their demographic and phototherapeutic data were collected. The exclusion criteria included the following: pregnant and lactating women; patients having a history of photosensitive disorders, skin cancer, active vitiligo; patients under systemic and/or topical immunosuppressive treatments within the last 8 weeks; patients exposed extensively to sunlight or phototherapy in the 8 weeks before the study.
The treatment was made using a monochromatic 308-nm Xenon-Chloride Excimer laser (Photo Medex, Xtrac®, USA). The fixed technical parameters were as follows: pulse frequency 200 Hz and a maximal output of 600 mW/cm2 per pulse, pulse width 30 ns, and laser energy 20 mJ. Beam transmission was achieved by liquid light guide with variable spot size diameters of 15 mm, 20 mm, and 25 mm, which was changed according to the size of the lesions. The treatment end point was 48 treatments or 100% repigmentation, whichever was achieved first.
Before the start of the treatment, the minimal erythema dose was determined for each subject and the treatment started with 1 minimal erythema dose. This treatment was repeated twice a week on non-consecutive days. The dose given at each session depended on the extent of erythema observed after the previous treatment. If the erythematous response was severe and⁄or other signs of phototoxic side effects (i.e., burning, stinging, edema, blisters) were present, the session was skipped. If the erythematous response was moderate or slight, the dose was increased by 50 mJ/cm2. If there was no erythematous response, the dose was increased by100 mJ/cm2. During the treatment sessions, the eyes were protected with UV protective goggles. In all patients, at least 1 lesion was left untreated and served as controls.
The assessment of the clinical response and recording of side effects were performed biweekly, and photographs were taken before the treatment and after reaching the end point. The clinical response was assessed by 2 independent dermatologists. Repigmentation was graded on a 5-point scale (0: no repigmentation, 1: poor repigmentation (1–25%), I2: moderate repigmentation (26–50%), II3: good repigmentation (51–75%), and 4: excellent repigmentation (>75%).19 In the case of disagreement between the 2 evaluators, a common evaluation of the 2 dermatologists was done. If the disagreement persisted, the lowest evaluation was chosen. Then the pattern of repigmentation and its relation to the location of lesions, patient’s age, and duration of lesions were evaluated.
At the final visit, the patients’ satisfaction and the effect of treatment on their psychosocial status were evaluated using a short anonymous questionnaire. The questionnaire consisted of 6 multiple-choice questions on the social and psychological aspects of patients’ life. The questions were given 3 possible answers (less, same, more) to describe self-reported patient’s evaluation of their social and psychological aspects after receiving the treatment compared to their condition before the treatment. The questionnaire also included 2 questions (using 0 to 10 visual analogue scale)20: one was on the overall patient satisfaction with the treatment and the second one was on how much the patient recommends this treatment to others with the same condition.
RESULTS
Characteristics of the study patients
The demographic and clinical characteristics of the study population are shown in Table 1. A total of 105 lesions were treated by excimer laser. The head (35; 33.3%), upper limb (26; 24.8%), lower limb (29; 27.6%), and trunk (15; 14.3%) were the common sites for these lesions.
Table 1.
Demographic and clinical characteristics of the study subjects.
| Number of patients (M:F) | 48 (22:3) |
| Mean age in years (SD, range) | 29.0 (10.9, 16–50) |
| Gender | |
| Male | 22 (45.8) |
| Female | 26 (54.2) |
| Education N (%) | |
| Illiterate | 3 (6.2) |
| Secondary | 21 (43.8) |
| University | 20 (41.7) |
| Postgraduate | 4 (8.3) |
| Social status N (%) | |
| Single | 21 (43.7) |
| Married | 24 (50.0) |
| Divorced/Widowed | 3 (6.3) |
| Occupation N (%) | |
| Manual work | 3 (6.3) |
| Clerical | 12 (25.0) |
| Business | 5 (10.4) |
| Professional | 2 (4.2) |
| Student | 16 (33.3) |
| Housewife | 10 (20.8) |
| Fitz-Patrick skin type | |
| III | 16 (33.3) |
| IV | 21 (43.8) |
| V | 11 (22.9) |
| Mean duration of disease in years (SD, range) | 7.8 (4.3, 1–23) |
| Mean age of onset in years (SD, range) | 22.4 (9.7, 3–48) |
| Distribution of lesions (N=105) (%) | |
| Face | 22 (20.9) |
| Neck | 9 (8.6) |
| Trunk | 15 (14.3) |
| Upper limb | 30 (28.6) |
| Lower limb | 29 (27.6) |
Clinical efficacy
Ninety-three (88.6%) out of 105 lesions showed some degree of repigmentation by excimer laser treatment. A total of 63 (60.0%) vitiligo lesions demonstrated excellent “Grade IV” repigmentation (more than 75% of the treated area), 12 (11.4%) lesions showed good repigmentation, 9 (8.6%) lesions showed moderate repigmentation, 9 lesions (8.6%) showed poor repigmentation, and 12 lesions (11.4%) showed no repigmentation. The repigmentation was achieved in 16.8 (8.0) sessions; however 20.2 (15) sessions were needed to realize Grade IV repigmentation.
The type of repigmentation varied between lesions. While 34 (36.6%) of 93 lesions showed diffuse repigmentation, 25 (26.9%) and 20 (21.5%) lesions showed perifollicular repigmentation and marginal type of repigmentation, respectively. Only 14 (15.1%) lesions demonstrated the mixed type of repigmentation.
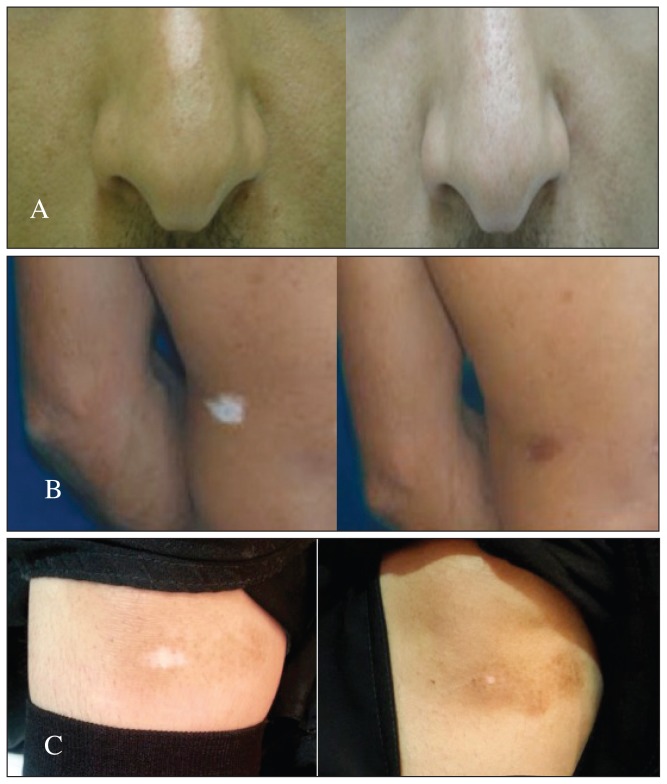
The response to treatment varied at different sites of involvement (Table 2). Facial lesions including face and neck responded better than lesions located elsewhere. Abdominal lesions responded better than back lesions, while legs responded better than thighs. Figure 1 shows different body sites with variable response to excimer laser before and after treatment.
Table 2.
Response to treatment in different body sites.
| Region | No. of lesions treated | >75% Response (%) | <75% Response (%)a |
|---|---|---|---|
|
| |||
| Face | 18 | 17 (94.4) | 1 (5.6) |
| Neck | 17 | 16 (94.1) | 1 (5.9) |
| Abdomen | 10 | 8 (80.0) | 2 (20.0) |
| Back | 5 | 3 (60.0) | 2 (40.0) |
| Thigh | 11 | 7 (63.6) | 4 (36.4) |
| Leg | 6 | 5 (83.3) | 1 (16.7) |
| Foot | 5 | 0 (0.0) | 5(100.0) |
| Knee | 7 | 4 (57.1) | 3 (42.9) |
| Upper arm | 5 | 1 (20.0) | 4 (80.0) |
| Forearm | 1 | 0 (0.0) | 1 (100.0) |
| Elbow | 6 | 1 (16.7) | 5 (83.3) |
| Hand | 14 | 1 (7.1) | 13 (92.9) |
| Total | 105 | 63 (60.0) | 42 (40.0) |
Includes 12 patients who did not respond to treatment.
Figure 1.
Different body sites with variable response to excimer laser treatment (before and after treatment). A) Face; B) Trunk; C) Knee.
The t effect of skin type on the response to treatment was not statistically significant (P=.07). Among those patients who had skin type III, the good response to treatment was observed in 70.6% of lesions, whereas similar response in patients with type IV and V were 55% and 54.5%, respectively (Table 3). None of the study patient had skin type I or II.
Table 3.
Response to treatment according to skin type (48 patients).
| Fitz-patrick skin type | >75% Response (%) | <75% Response (%) | Total |
|---|---|---|---|
|
| |||
| III | 12 (70.6) | 5 (29.4) | 17 |
| IV | 11 (55.0) | 9 (45.0) | 20 |
| V | 6 (54.5) | 5 (45.5) | 11 |
| Total | 29 (60.4) | 19 (39.6) | 48 |
The degree of repigmentation was not influenced by age group (P=.30), as was observed ion patients after dividing them into 3 age groups: younger than 20 years, 20 to 39 years, and older than 40 years. Additionally, gender of patients, social class, education, and occupation had no significant role in determining the response to this treatment (P=.26, .28, .08, .19, respectively). Conversely, there was a significant relationship between the rate of repigmentation and the duration of the disease and location of the lesions (P=.003 and .000, respectively). Regarding the location of lesions, the rate of repigmentation was faster in the following order: face and neck, abdomen and back, leg and arm, and finally hand and foot. All the untreated control patches from the 48 patients remained unchanged.
Factors influencing repigmentation were determined using multivariate analysis, and it was found that disease duration was a significant negative factor (b=–0.24, P=.03); patients with longer disease duration tended to show lesser rates of repigmentation. On the contrary, treatment duration (b=0.33, P=.037) was found to be a positive significant factor, as patients with longer treatment duration showed more rates of repigmentation.
Side effects
The most commonly seen side effects were limited to mild-to-moderate erythema, pruritus/itching, and small circumscribed blisters or edema at laser-treated skin site (presumably most often because of overlap in laser spot administration). Sixty-four lesions (61.0%) were followed by erythema, 33 lesions (31.5%) showed itching, and 9 lesions (8.6%) demonstrated small blisters and desquamations during the treatment. We also observed that patients with dark skin demonstrated less rates of side effects.
Psychosocial impact
All the treated 48 patients returned the self-reported psychosocial questionnaires. Table 4 summarizes patients’ response to this questionnaire. Twenty-two patients (45.8%) showed less worry about their appearance and body image after the laser treatment. Twelve patients (25%) showed an improvement in their ability to make friends or to meet others. Additionally, self-confidence and self-esteem showed a marked improvement after treatment where 20 patients (41.7%) responded positively to this question. Also, 21 patients (43.8%) revealed less anxiety while only 11 patients (22.9%) showed less depression after the treatment. The question about how much the patient feels that others treat him/her differently because of his/her condition after laser treatment had a low score, with only 6 patients (12.5%) who demonstrated improvement after treatment. Results of this study showed that patients’ worry about their appearance and body image, self-confidence and self-esteem, and decreased anxiety after treatment with excimer laser were significantly associated with the location of treatment (P=.023, .034, .041, respectively). In addition, patients’ worry about their appearance and decreased anxiety after treatment were significantly associated with being females (P=.032, .012, respectively). However, other demographic and clinical variables were not found to be significantly associated with any of the questions describing the psychosocial impact of treatment on patients with vitiligo.
Table 4.
Psychosocial impact after excimer laser treatment.
| Less N (%) |
Same N (%) |
More N (%) |
|
|---|---|---|---|
|
| |||
| How much worry do you feel about your appearance and body image after laser treatment? | 22 (45.8) | 16 (33.3) | 10 (20.8) |
| How much ability do you have to make friends or meet other after laser treatment? | 1 (2.1) | 35 (72.9) | 12 (25.0) |
| How much do you feel that others treat you differently because of your condition after laser treatment? | 1 (2.1) | 41 (85.4) | 6 (12.5) |
| How much self-confidence and self-esteem do you have after laser treatment? | 5 (10.4) | 23 (47.9) | 20 (41.7) |
| How much anxiety do you feel after laser treatment? | 21 (43.8) | 17 (35.4) | 10 (20.8) |
| How much depression do you fee after laser treatment? | 11 (22.9) | 33 (68.8) | 4 (8.3) |
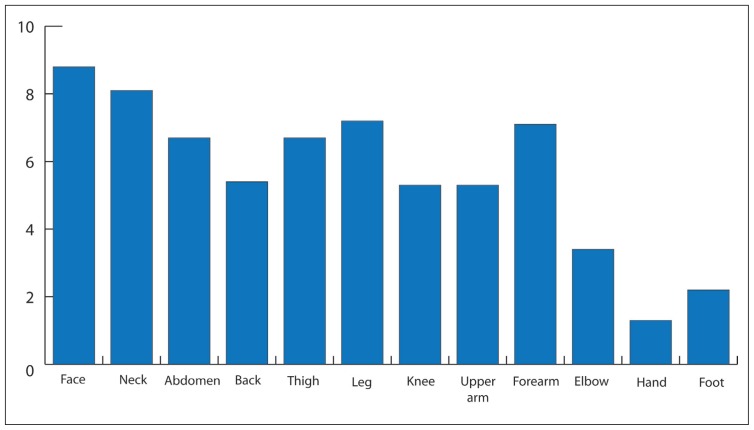
In their response to the 2 questions based on (0–10) visual analog scale, the average overall satisfaction of study patients with the result of the treatment was 5.74 (SD=3.26). Similarly, the patients recommended the excimer laser treatment to other similar patients with an average of 5.71 (SD=3.65). The mean overall satisfaction scores for women and men were 6.4 (3.22) and 4.95 (3.36), respectively. Thus, the overall satisfaction with the treatment was significantly more in females than in males (P=.023). The mean satisfaction score was highest in the age group of over 40 years, but it was not statistically different between the age groups (P=.29). The mean satisfaction score was significantly associated with the location of the lesion. Figure 2 shows that patients with lesions on the face and neck demonstrated the highest mean satisfaction score after treatment (8.5 [0.9]). On the contrary, patients with lesions of hands and feet showed the least satisfaction after treatment with a mean score of 1.5 (0.6). Patients with lesions on other parts of the body, for example, trunk, upper limbs, and lower limbs, showed moderate satisfaction after treatment (mean score, 6.3, 4.5, and 6.4, respectively). In addition, the duration of treatment had a significant negative relationship with the satisfaction score (P<.05). However, satisfaction was not significantly affected by the marital state of the patient, education, occupation, duration of disease, or age of disease onset (P>.05). Additionally, patients’ recommendation of the excimer laser treatment to other similar patients was found significantly associated with the patients’ satisfaction (P<.05), where patients with higher satisfaction were more likely to recommend treatment to others.
Figure 2.
Mean satisfaction scores.
DISCUSSION
Vitiligo is a difficult disease to treat. Response rates for the various modalities of treatment are highly variable. The best results are achieved with surgical methods especially if followed by Psoralen-Ultraviolet A (PUVA) radiation.21 Among the non-surgical methods, band ultraviolet B (UVB) therapy, broadband UVB, topical class 3 and 4 corticosteroids, and PUVA therapy proved significant responses.21,22 However, these modalities require months to years for significant improvement to occur and some of them are associated with side effects such as nausea, vomiting, phototoxicity, and extension of radiation to the non-affected skin with a potential increase in the risk of cancer. Skin atrophy, striae, and telangiectasia are seen with corticosteroids.23
Recently, the 308-nm excimer laser has been shown to be effective in treating vitiliginous lesions. It has some advantages over other methods of treatment. It requires relatively short time, delivers treatment only to affected areas (with uninvolved areas of skin being saved), and can reach areas inaccessible to conventional phototherapeutic modalities. Conversely, it is time-consuming and inefficient to treat larger patches.5–9
This study confirms that the 308-nm excimer laser is effective for the treatment of localized vitiligo. A total of 93 lesions out of 105 (88.6%) showed some degree of repigmentation, while 12 lesions (11.4%) showed no repigmentation. The average number of sessions needed to achieve repigmentation was 16.8 (8), whereas the average number of sessions needed to realize excellent “Grade IV” repigmentation was 20.2 (15). Our findings are similar to results obtained by other studies.5–12, 23
This study showed good therapeutic results on the face, neck, and abdomen. In the extremities, the results were more favorable on the lower than on the upper limbs. Lesions on hands and feet had the least favorable results. These findings are comparable to other studies. 5–9 The reasons for this body site variation are unknown, although it has been hypothesized to be related to lower hair-growth density and the fewer melanocytes in the low-response body sites.10
Interestingly, the results of this study showed that the diffuse pattern was the most common repigmentation pattern and that the early and excellent rate of repigmentation (>75%) was significantly associated with the diffuse pattern. This result is similar to that of Parsad et al24 who showed that the speed of repigmentation is much faster when repigmentation starts in a diffuse type as compared with perifollicular and marginal repigmentation. In this study, perifollicular pattern was the next common followed by the marginal pattern while the mixed pattern was the least common pattern of repigmentation.
In the past, it was believed that vitiligo lesions were devoid of melanocytes and that only hair follicles could act as reservoirs. However, recent studies explained that melanocytes are still present in the depigmented epidermis of stable vitiligo lesions for a long period.25 Other study26 also suggested an alternative source of melanocytes such as melanocyte precursors or stem cells. Accordingly, melanocytes remaining in the lesions might explain the diffuse pattern of repigmentation. However, the marginal pattern is possibly explained by migration of activated melanocytes from the surrounding normal skin.
Minor side effects were noted after treatment. Mild-to-moderate erythema was more manifest in areas of overlap. All adverse effects including erythema, itching, and blisters disappeared 3 to 5 days after the end of treatment sessions. These results show that the use of the 308-nm excimer laser for the treatment of vitiligo is relatively safe and more convenient compared to other available modalities of treatment for vitiligo with small patches. In this study design, we used a questionnaire that asks patients to compare their after-treatment psychosocial condition with their before-treatment psychosocial condition. The results demonstrated obvious influence of the treatment on the psychological and social condition of the patients. Worry about appearance and body image has been reduced significantly after laser treatment in about 46% of patients. Self-confidence, ability to make friends, and to lead a positive social life have been improved in a significant number of patients. Additionally, anxiety and, to a lesser extent, depression have been reduced after treatment.
Female patients had a significant higher rate of satisfaction with the excimer laser treatment. This is in accordance with other studies that showed that psychosocial reactions to vitiligo were different for men and women. Stress, worry, depression, self-confidence, personal satisfaction, and social life showed differences between the gender, women being significantly more affected than men and more influenced by any clinical improvement due to treatment.14–16 In addition, the overall satisfaction with the treatment was influenced significantly by the location of the lesions. Patients with lesions in the exposed parts of the body such as face and neck demonstrated high satisfaction with treatment. Efficacy of excimer laser on treatment of lesions on face and neck has been demonstrated in many studies.6,7,10 However, hands and feet did not show a good response to laser treatment, which explains the significant low satisfaction with the treatment. This study highlights the role of treatment in influencing the social and psychological life of the patients and acknowledges the psychosocial needs and support that the patients require. In addition to treatment, physicians should provide individualized education, continuous support, and coping strategies.17
In conclusion, the use of the 308-nm excimer laser for the treatment of localized vitiligo is effective and relatively safe and more convenient compared to other available modalities of treatment. This intervention is also associated with improved psychological and social conditions of the patients.
REFERENCES
- 1.Malhotra N, Dytoc M. The pathogenesis of vitiligo. J Cutan Med Surg. 2013;17:153–72. doi: 10.2310/7750.2012.12005. [DOI] [PubMed] [Google Scholar]
- 2.Halder RM, Nootheti PK. Ethnic skin disorders overview. J Am Acad Dermatol. 2003;48:S143–8. doi: 10.1067/mjd.2003.274. [DOI] [PubMed] [Google Scholar]
- 3.Grimes PE. White patches and bruised souls: advances in the pathogenesis and treatment of vitiligo. J Am Acad Dermatol. 2004;51:S5–7. doi: 10.1016/j.jaad.2004.01.007. [DOI] [PubMed] [Google Scholar]
- 4.Njoo MD, Westerhof W. Vitiligo: pathogenesis and treatment. Am J Clin Dermatol. 2001;2:167–81. doi: 10.2165/00128071-200102030-00006. [DOI] [PubMed] [Google Scholar]
- 5.Whitton ME, Pinart M, Batchelor J, Lushey C, Leonardi-Bee J, Gonzalez U. Interventions for vitiligo. Cochrane Database Syst Rev. 2010;20:CD003263. doi: 10.1002/14651858.CD003263.pub4. [DOI] [PubMed] [Google Scholar]
- 6.Zhang XY, He YL, Dong J, Xu JZ, Wang J. Clinical efficacy of a 308 nm excimer laser in the treatment of vitiligo. Photodermatol Photoimmunol Photomed. 2010;26:138–42. doi: 10.1111/j.1600-0781.2010.00509.x. [DOI] [PubMed] [Google Scholar]
- 7.Wang HW, Zuo YG, Jin HZ, Liu YH, Ma DL, Jiang GT, Li HC, Liu J, Yan Y. Efficacy and safety of 308 nm excimer laser for vitiligo. Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2009;31:34–6. [PubMed] [Google Scholar]
- 8.Casacci M, Thomas P, Pacifico A, Bonnevalle A, ParoVidolin A, Leone G. Comparison between 308-nm monochromatic excimer light and narrow-band UVB phototherapy (311–313 nm) in the treatment of vitiligo-a multicentre controlled study. J Eur Acad Dermatol Venereol. 2007;21:956–63. doi: 10.1111/j.1468-3083.2007.02151.x. [DOI] [PubMed] [Google Scholar]
- 9.Greve B, Raulin C, Fischer E. Excimer laser treatment of vitiligo - critical retrospective assessment of own results and literature overview. J Dtsch Dermatol Ges. 2006;4:32–40. doi: 10.1111/j.1610-0387.2006.05879.x. [DOI] [PubMed] [Google Scholar]
- 10.Hofer A, Hassan AS, Legat FJ, Kerl H, Wolf P. The efficacy of excimer laser (308 nm) for vitiligo at different body sites. J European Academy of Dermatology and Venereology. 2006;20:558–64. doi: 10.1111/j.1468-3083.2006.01547.x. [DOI] [PubMed] [Google Scholar]
- 11.Cazzaniga S, Sassi F, Mercuri SR, Naldi L. Prediction of clinical response to excimer laser treatment in vitiligo by using neural network models. Dermatology. 2009;219:133–7. doi: 10.1159/000225934. [DOI] [PubMed] [Google Scholar]
- 12.Al-Otaibi SR, Zadeh VB, Al-Abdulrazzaq AH, Tarrab SM, Al-Owaidi HA, Mahrous R, Kadyan RS, Najem NM. Using a 308-nm excimer laser to treat vitiligo in Asians. Acta Dermatovenerol Alp Panonica Adriat. 2009;18:13–8. [PubMed] [Google Scholar]
- 13.Al Robaee AA. Assessment of quality of life in Saudi patients with vitiligo in a medical school in Qassim province, Saudi Arabia. Saudi Med J. 2007;28:1414–7. [PubMed] [Google Scholar]
- 14.Borimnejad L, Parsa YZ, NikbakhtNa A, Firooz A. Quality of life with vitiligo: comparison of male and female Muslim patients in Iran. Gender Med. 2006;3:124–30. doi: 10.1016/s1550-8579(06)80201-9. [DOI] [PubMed] [Google Scholar]
- 15.SchmidOtt G, Kunsebeck HW, Jecht E, Shimshoni R, Lazaroff I, Schallmayer S, Calliess IT, Malewski P, Lamprecht F, Götz A. Stigmatization experience, coping and sense of coherence in vitiligo patients. J Eur Acad Dermatol Venereol. 2007;21:456–61. doi: 10.1111/j.1468-3083.2006.01897.x. [DOI] [PubMed] [Google Scholar]
- 16.Mechri A, Amri M, Douarika AA, li Hichem BH, Zouari B, Zili J. Psychiatric morbidity and quality of life in vitiligo: a case controlled study. Tunis Med. 2006;84:632–5. [PubMed] [Google Scholar]
- 17.Ongenae K, Beelaert L, Van GN, Naeyaert JM. Psychosocial effects of vitiligo. J Eur Acad Dermatol Venereol. 2006;20:1–8. doi: 10.1111/j.1468-3083.2005.01369.x. [DOI] [PubMed] [Google Scholar]
- 18.Ongenae K, Van GN, De SS, Vander HY, Naeyaert JM. Management of vitiligo patients and attitude of dermatologists towards vitiligo. Eur J Dermatol. 2004;14:177–81. [PubMed] [Google Scholar]
- 19.Spencer JM, Nossa R, Ajmeri J. Treatment of vitilligo with the 308-nm excimer laser: a pilot study. J Am Acad Dermatol. 2002;46:727–31. doi: 10.1067/mjd.2002.121357. [DOI] [PubMed] [Google Scholar]
- 20.Wewers ME, Lowe NK. A critical review of visual analogue scales in the measurement of clinical phenomena. Research in Nursing and Health. 1990;13:227–36. doi: 10.1002/nur.4770130405. [DOI] [PubMed] [Google Scholar]
- 21.Njoo MD, Westerhoff W, Bos JD, Bossuyt PMM. The development of guidelines for the treatment of vitiligo. Arch Dermatol. 1999;135:1514–21. doi: 10.1001/archderm.135.12.1514. [DOI] [PubMed] [Google Scholar]
- 22.Tjioe M, Otero ME, Van de Kerkhof PCM, Gerritsen MJP. Quality of life in vitiligo patients after treatment with long-term narrow-band ultraviolet B phototherapy. J Euro Acad Dermatol Venereol. 2005;19:56–60. doi: 10.1111/j.1468-3083.2004.01124.x. [DOI] [PubMed] [Google Scholar]
- 23.Yang Y, Chol HR, Ho J, Lee M. Clinical study of repigmentation patterns with either narrowband ultraviolet B (NBUVB) or 308 nm excimer laser treatment in Korean vitiligo patients. Inter J Dermatol. 2010;49:317–23. doi: 10.1111/j.1365-4632.2009.04332.x. [DOI] [PubMed] [Google Scholar]
- 24.Parsad D, Pandhi R, Dogra S, Kumar B. Clinical study of repigmentation patterns with different treatment modalities and their correlation with speed and stability of repigmentation in 352 vitiligionous patches. J Am Acad Dermatol. 2004;50:63–7. doi: 10.1016/s0190-9622(03)00786-2. [DOI] [PubMed] [Google Scholar]
- 25.Tobin DJ, Swanson NN, Pittelkow MR, Peters EM, Schallreuter KU. Melanocytes are not absent in lesional skin of long duration vitiligo. J Pathol. 2000;191:407–16. doi: 10.1002/1096-9896(2000)9999:9999<::AID-PATH659>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 26.Davids LM, du Toit E, Kidson SH, Todd G. A rare repigmentation pattern in a vitiligo patient: a clue to an epidermal stem-cell reservoir of melanocytes? Clin Exp Dermatol. 2009;34:246–8. doi: 10.1111/j.1365-2230.2008.02793.x. [DOI] [PubMed] [Google Scholar]