Abstract
BACKGROUND AND OBJECTIVES
To improve cardiovascular (CV) health of American population, the American Heart Association (AHA) developed definitions of ideal, intermediate, and poor CV health based on 7 accessible health metrics. The applicability of this construct and the distribution of its components in the community-based populations in the Middle East region have not been reported.
DESIGN AND SETTINGS
A prospective population-based cohort study conducted from 1999 to 2011.
METHODS
We used data from phase 4 of Tehran Lipid and Glucose Study (2009–2011) (2861 women and 2004 men, aged ≥ 20 years) to estimate the frequency of CV health levels (ideal, intermediate, and poor) in adults of both genders, and the frequency of each metric at each level of CV health. The median or mean of each CV health metric was also estimated in the whole spectrum of CV health in all subgroups.
RESULTS
Only 1 adult participant met all 7 ideal CV health metrics; 25.01% of women and 26% of men had intermediate CV health; 74.8% of women and 74% of men exhibited poor CV health. Only 19.7% of women and 10.3% of men had 5 or more ideal CV health metrics. Nonsmoking was the most frequent ideal health behavior. A total of 89.6% of participants had 1 or 2 ideal CV health behaviors. Ideal smoking and fasting plasma glucose had the highest frequency of CV health factors among others.
CONCLUSION
The frequency of ideal CV health was extremely low in this cohort of adults. The frequency of intermediate CV health was also low, and it may be significantly lower in the general population.
Despite the decline in cardiovascular disease (CVD) and stroke mortality rate that is primarily because of advances in evidence-based treatment of CVD and CVD risk factors (secondary and primary prevention), CVD and stroke are the leading cause of morbidity and mortality worldwide. Aging of population and increasing prevalence of obesity and diabetes contribute to the persistent CVD and stroke burden.1–3 Cardiovascular (CV) health status remains an important public health problem in the Middle East, and the prevalence of CVD and its associated risk factors is higher in the Middle East than in the Western societies.4,5 The Middle East is one region where lifestyle transformation is occurring. Increased fat and caloric intake and reduced physical activity are factors likely leading to the emergence of hypertension and atherosclerosis in this region. Thus, the examination of regional characteristics that may be leading to the increased CVD is needed. Despite the mortality and morbidity associated with CVD, many Middle Eastern countries lack surveillance data regarding CVD prevalence, incidence, and risk factors. Such information is crucial for monitoring problems and guiding interventions. 6
To prevent ongoing increase in CVD risk factors and CVD events, American Heart Association (AHA) developed a major new goal: “To improve CV health in the population as a whole” and presented definitions of ideal, intermediate, and poor CV health based on 7 modifiable health metrics including 4 CV health behaviors (no smoking, physical activity, healthy diet, and healthy body mass index [BMI]) and 4 CV health factors (smoking, fasting plasma glucose, total cholesterol, and blood pressure).1 In this study, for the first time, we used the AHA 2020 impact goals definitions to evaluate the applicability of this construct and the distribution of its components in a Middle Eastern community-based population.
METHODS
The details of Tehran Lipid and Glucose Study (TLGS) design have been published elsewhere.7 In brief, TLGS began in 1999 as a long-term community-based study for preventing non-communicable disorders (NCDs). The first phase of the study was a cross-sectional study to evaluate the prevalence of NCDs and their respective risk factors in 15 005 participants from district No.13 of Tehran, the capital city of Iran. The next phases of the study were designed as prospective follow-up studies in every 3 years. At each phase of the study, a limited physical examination including blood pressure, pulse rate, and anthropometrical measurements were performed and lipid profiles, fasting blood sugar, and 2-hour-postload glucose levels were measured.
For the present study, we used data from phase 4 that was performed in 2009–2011. In phase 4, 10 887 participants (20 years old or above) were included, of whom only 4865 (2861 women and 2004 men) participants aged ≥20 years, had complete data for CVDs and all 7 metrics of AHA’S definition of CV health, and were included in the present study. The only exclusion criterion was pregnancy. The proposal of this study was approved by the research council of the Research Institute for Endocrine Sciences of Shahid Beheshti University of Medical Sciences, and written informed consent was obtained from each subject.
Definition of CV health
We used AHA 2020 impact goals definitions of ideal, intermediate, and poor CV health. Criteria for CV health components are outlined in Table 1. Ideal CV health is defined as the simultaneous presence of 4 ideal health behaviors (no smoking within the last year, ideal BMI, ideal physical activity, and ideal diet); the simultaneous presence of 4 ideal health factors (no smoking within the last year, untreated total cholesterol <200 mg/dL, untreated blood pressure <120/80 mm Hg, and untreated fasting plasma glucose <100mm Hg), and the absence of CV diseases. Intermediate CV health is defined as the presence of at least 1 intermediate CV health metric without any poor health metrics. Poor CV health is defined as the presence of any poor CV health metrics.1
Table 1.
American Heart Association 2020 strategic impact goals definitions of poor, intermediate, and ideal cardiovascular health for each goal/metric.
| Cardiovascular health goals/metrics | Poor | Intermediate | Ideal |
|---|---|---|---|
|
| |||
| Current smoking | Yes | Former, quit ≤12 mo previously | Never or quit >12 mo previously |
| Body mass index, kg/m2 | ≥30 | 25–29.9 | <25 |
| Physical activity level | None | 1–149 min/wk moderate intensity, 1–74 min vigorous intensity, 1–149 min/wk moderate+ vigorousa | ≥150 min/wk moderate intensity, ≥75 min/wk vigorous intensity, or ≥150 min/wk moderate+ vigorousb |
| Healthy diet score componentsb | 0–1 | 2–3 | 4–5 |
| Total cholesterol, mg/dL | ≥240 | 200–239 or treated to goal | <200, untreated |
| Blood pressure, mm Hg | SBP ≥140 or DBP ≥90 | SBP 120–139, or DBP 80–89, or treated to goal | <120/<80, untreated |
| Fasting plasma glucose, mg/dL | ≥126 | 100–125 or treated to goal | <100, untreated |
SBP: Systolic blood pressure, DBP: diastolic blood pressure.
Minutes of vigorous activity are equal to 2 times the minutes of moderate activity when moderate and vigorous activities are combined.
Healthy diet score components include: fruits and vegetables, ≥4.5 cups per day; fish, 2 or more 3.5-oz servings per week; fiber-rich whole grains (≥1.1 g fiber/10 g carbohydrate), 3 or more 1-oz-equivalent servings per day; sodium, ≤1500 mg/d; and sugar-sweetened beverages, ≤450 kcal/wk. Dietary recommendations are scaled according to a 2000-kcal/d diet (Circulation 2010, 121:586–613).
Diet scoring
Dietary assessment was performed through dietary habits and qualitative Food Frequency Questionnaire (FFQ) and two 24-hour dietary recalls.8 The Persian translated version of FFQ was reliable and valid for assessing the intake of several food groups for TLGS population.8 In the present study, we first excluded individuals with extreme energy intake (±3 SD). We then used 5 AHA’s ideal CV health components including: ≥4.5 cups per day of fruits and vegetables; ≥2 to 3.5 oz servings per week of fish; ≥3 1-oz equivalent servings per day of whole grains; <1500 mg per day sodium; and ≤36 oz per week of sugar-sweetened beverages (≤450 kcal per week) to categorize participants to ideal (4–5 component), intermediate (2–3 component), and poor (0 to 1 component) diet status.1
Physical activity
The physical activity level was assessed using Modifiable Activity Questionnaire (MAQ). Persian-translated MAQ had high reliability and moderate validity for TLGS population.9 We used AHA’s classification to categorize physical activity levels to ideal (≥150 min/week moderate intensity or ≥75 min/week of vigorous intensity), intermediate (1–149 min/week moderate intensity or 1–74 min/week vigorous intensity), and poor (none) activity.
Statistical analysis
Continuous variables with normal distribution were described by mean (SD) and compared by t test. Continuous variables without normal distribution were described by median (IQR) and compared by Mann-Whitney test. Categorical variables were described by percentage and compared by χ2 tests.
RESULTS
A total of 4865 participants (58.8% women) were included for the final analysis. Baseline characteristics and frequency of all CV health metrics based on health status (ideal, intermediate, and poor) and sex group are presented in Table 2.
Table 2.
Baseline characteristics and frequency distribution of CV health metrics adults.
| Variables | Women (n=2861) | Men (n=2004) | P value | ||
|---|---|---|---|---|---|
| Number | Percent | Number | Percent | ||
|
| |||||
| Age (mean [SD]) | 41(12.8) | 42 (14.6) | .017 | ||
| Educational level | |||||
| Illiterate | 63 | 2.2 | 7 | 0.3 | <.001 |
| <High school | 751 | 26.2 | 423 | 21.1 | |
| High school graduate | 1313 | 45.9 | 922 | 46 | |
| >High school | 734 | 25.7 | 652 | 32.5 | |
| BMI | |||||
| Ideal | 857 | 30 | 665 | 33.2 | <.001 |
| Intermediate | 1141 | 39.9 | 948 | 47.3 | |
| Poor | 863 | 30.2 | 391 | 19.5 | |
| Smoking | |||||
| Ideal | 2740 | 95.8 | 1433 | 71.5 | <.001 |
| Intermediate | 42 | 1.5 | 126 | 6.3 | |
| Poor | 79 | 2.8 | 445 | 22.2 | |
| Physical activity | |||||
| Ideal | 32 | 1.1 | 70 | 3.5 | <.001 |
| Intermediate | 1562 | 54.6 | 1338 | 66.8 | |
| Poor | 1267 | 44.3 | 596 | 29.7 | |
| Diet scoring | |||||
| Ideal | 82 | 2.9 | 27 | 1.3 | <.001 |
| Intermediate | 2217 | 77.5 | 1434 | 71.6 | |
| Poor | 562 | 19.6 | 543 | 27.1 | |
| Blood pressure | |||||
| Ideal | 1737 | 60.7 | 843 | 42.1 | <.001 |
| Intermediate | 799 | 27.9 | 812 | 40.5 | |
| Poor | 325 | 11.4 | 349 | 17.4 | |
| Total cholesterol | |||||
| Ideal | 1791 | 62.6 | 1248 | 62.3 | .43 |
| Intermediate | 809 | 28.3 | 591 | 29.5 | |
| Poor | 261 | 9.1 | 165 | 8.2 | |
| FPG | |||||
| Ideal | 2238 | 78.2 | 1449 | 72.3 | <.001 |
| Intermediate | 457 | 16 | 429 | 21.4 | |
| Poor | 166 | 5.8 | 126 | 6.3 | |
CV: Cardiovascular, BMI: body mass index, FPG: fasting plasma glucose.
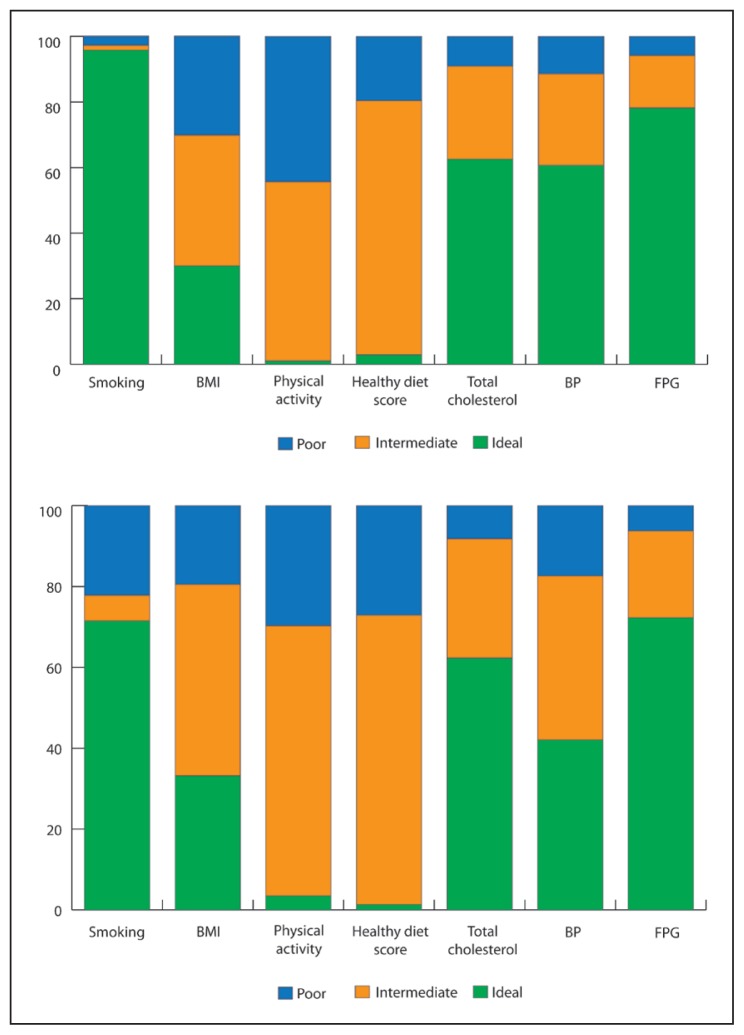
The majority of participants had an ideal smoking status. The frequency of ideal smoking status was significantly higher in women than in men (95.8% vs. 71.5%). Only 1/3 of men and less than 1/3 of women had ideal BMI. About 70% of women and 67% of men had overweight or obesity. The frequency of poor BMI (obesity) was significantly higher in women than in men (30.2% vs. 19.5%). Among all CV health behaviors, ideal physical activity and ideal diet had the lowest frequency. Only 1.1% of women and 3.5% of men had an ideal physical activity. Women exhibited higher frequency of poor physical activity; in contrast, men exhibited higher frequency of poor diet status. A total of 1.3% of men versus 2.9% of women had an ideal diet score (Figure 1).
Figure 1.
Distribution of CV health metrics among women (upper panel) and men (lower panel).
Ideal smoking and fasting plasma glucose (FPG) had the highest frequency of CV health factors among others. Women exhibited higher frequency of ideal FPG as compared to men (78.2% vs. 72.3%). About 6% of participants had poor FPG. Ideal BP was the least frequent CV health factor. The frequency of poor BP was higher in men than in women. The frequencies of ideal, intermediate, and poor total cholesterol were not significantly different between men and women (Figure 1).
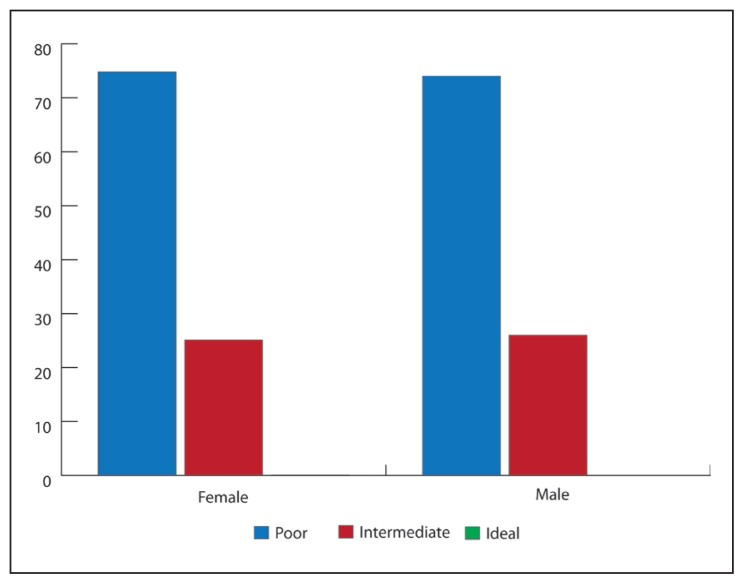
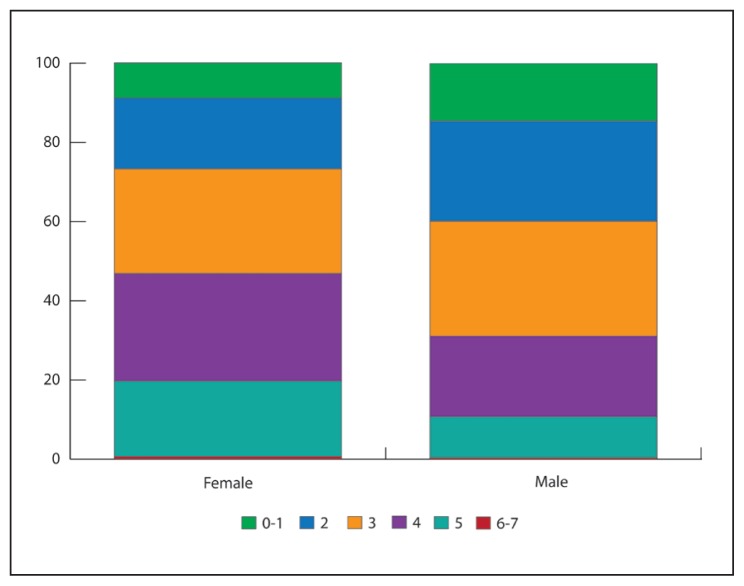
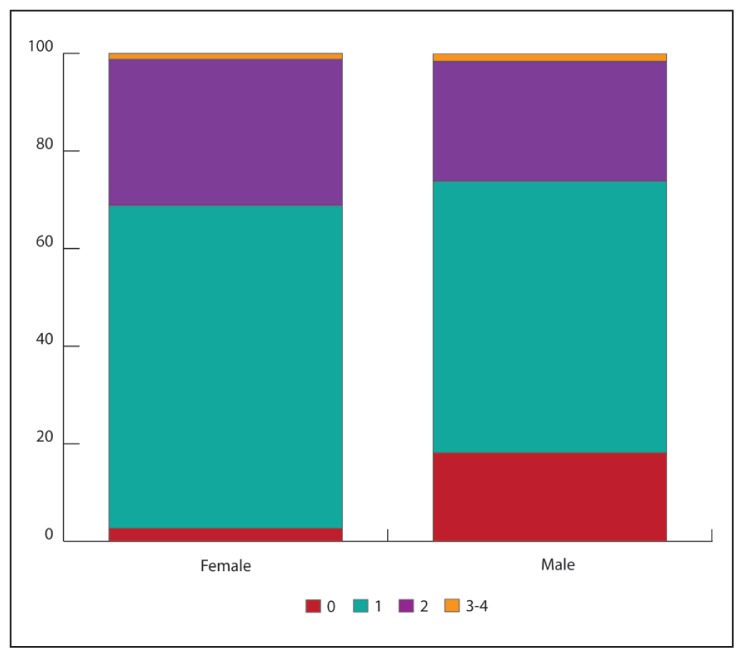
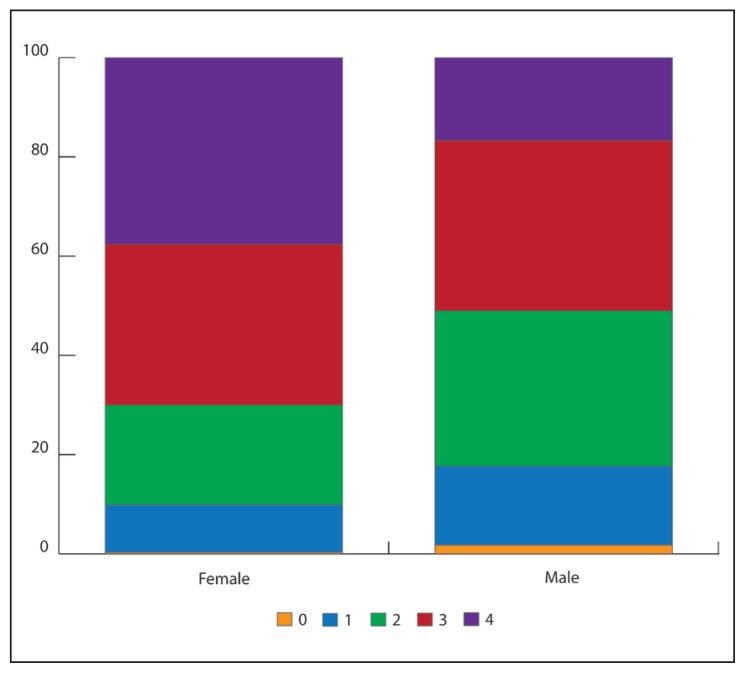
No men and only 1 woman exhibited an ideal level of all 7 CV health metrics and had ideal CV health (Figure 2). Approximately, 74% of participants had poor CV health and 25.5% exhibited intermediate CV health. Only 19.7% of women and 10.7% of men had 5 or more ideal CV health metrics. The majority of participants had 2 to 4 ideal CV health metrics. Only 1 man and 1 woman exhibited ideal level of all 4 CV health behaviors, and one-third participants had 3 CV health behaviors. More than 18% of men had no ideal health behaviors. About 37% of women and 17% of men exhibited an ideal level of all 4 CV health factors. Eight women and 37 men had no ideal health factors. Data pertaining to distribution of participants by number of ideal CV health metrics are shown in Figures 3, 4 and 5.
Figure 2.
Distribution of CV health status in adults ≥20 years old in TLGS 4.
Figure 3.
Distribution of participants by the number of ideal CV health metrics in adults ≥20 years old, TLGS 4.
Figure 4.
Distribution of participants by the number of ideal CV health behaviors in adults ≥20 years old, TLGS 4.
Figure 5.
Distribution of participants by the number of ideal CV health factors in adults ≥20 years old, TLGS 4.
The mean distribution of CV health metrics are displayed in Table 3. The medians of ideal and intermediate physical activities, in minutes per week, are significantly lower in women than in men. There were no significant differences in mean BMI between women and men in participants with ideal or intermediate BMI, but the mean of poor BMI was significantly higher in women than in men. The mean systolic blood pressure and the mean diastolic blood pressure were higher in men than in women in all 3 levels of blood pressures. The mean total cholesterol in all 3 levels was similar in women and men.
Table 3.
Mean distribution of cardiovascular health metrics in ideal, intermediate, and poor CV heath.
| Variables | Women (n=2861) | Men (n=2004) | P value |
|---|---|---|---|
|
| |||
| Physical activity (min/wk) | Median (IQR) | Median (IQR) | <.001 |
| Ideal | 180.0 (166.2–224.8) | 233.6 (177.2–291.6) | |
| Intermediate | 22.2 (10.4–46.2) | 31.7 (13.4–62.3) | |
| BMI (kg/m2) | Mean (SD) | Mean (SD) | <.001 |
| Ideal | 22.3 (2.0) | 22.4 (2.0) | |
| Intermediate | 27.4 (1.4) | 27.3 (1.4) | |
| Poor | 33.9 (3.6) | 32.8 (2.7) | |
| SBP (mm Hg) | <.001 | ||
| Ideal | 101.4 (9.0) | 106/0 (8/0) | |
| Intermediate | 118.5 (9.9) | 120.5 (8.6) | |
| Poor | 139.5 (17.5) | 137.8 (14.8) | |
| DBP (mm Hg) | <.001 | ||
| Ideal | 67.9 (6.8) | 70.6 (6/0) | |
| Intermediate | 79.7 (5.6) | 80.9 (5.5) | |
| Poor | 91.1 (8.9) | 92.3 (9.8) | |
| Total cholesterol (mg/dL) | .37 | ||
| Ideal | 165.4 (21.8) | 164.5 (22.6) | |
| Intermediate | 208.7 (22.8) | 207.8 (25.6) | |
| Poor | 263.8 (23.9) | 265.9 (43.6) | |
| FPG (mg/dL) | <.001 | ||
| Ideal | 88.9 (5.8) | 90.2 (5.6) | |
| Intermediate | 105.5 (7.4) | 106.2 (7.0) | |
| Poor | 175.8 (51.7) | 181.1 (55.1) | |
CV: Cardiovascular, IQR: interquartile range, BMI: body mass index, SBP: systolic blood pressure, DBP: diastolic blood pressure, FPG: fasting plasma glucose.
DISCUSSION
This study that used AHA 2020 goals definitions of ideal, intermediate, and poor CV health to evaluate the CV health status in TLGS indicated that ideal CV health is extremely low in this population of adults. Only 1 participant had ideal CV health, and majority of participants (74.5%) exhibited poor CV health.
The low frequency of ideal CV health in our population is consistent with reports from other parts of the world: North America, Europe, and East Asian countries (Table 4).10–13 In the Atherosclerosis Risk in Communities study, only 0.1% of participants exhibited ideal CV health and 82.5% had poor CV health.11 In multiple reports from the National Health and Nutrition Examination Survey (NHANES) studies, the prevalence of ideal CV health was less than 2%.14–16 Given a less strict definition of ideal CV health (5 or more ideal CV health metrics), 16% of participants (19.7% of women and 10.7% of men) met ≥5 ideal CV health metrics. Regarding the extremely low prevalence of ideal CV health, a less strict definition of ideal CV health may be more logical. However, there is a strong relationship between the numbers of ideal CV health metrics and incidence of CVD outcomes. Meeting a greater number of CV health metrics is associated with a lower risk of CVD outcomes.16,17 The goal should be achievement of greater number of ideal CV health metrics by all individuals.
Table 4.
Comparison of cardiovascular status in our study and other studies.
| TLGS (Our study) % | ARIC % | Heart SCORE % | NHANES (1988–2010) % | CHED % | South European | |
|---|---|---|---|---|---|---|
|
| ||||||
| Sample size | 4865 | 12 744 | 1993 | 44 959 | 1 012 418 | 11 408 |
| Age | 41.4 (13.6) | 45–64 | 59 (7.5) | 45–46.8 | 42.7 (6.4) | >18 |
| Ideal (%) | 1 participant | 0.1 (n=17) | 0.1 (n=1) | <2 | 1.5 | 0.2 |
| Intermediate (%) | 25.5 | 17.4 | -------- | -------- | 33.9 | 19.8 |
| Poor (%) | 74.5 | 82.5 | -------- | -------- | 64.6 | 80.0 |
| ≥5 metrics | 16 | 12.2 | 5.3 | 21–28 | 30 | 15.5 |
| ≤3 metrics | 60 | >70 | 80.9 | 48–52 | 53 | 64.4 |
| 4 behavior | 2 participants | -------- | 2 | -------- | -------- | 0.8 |
| 3–4 behavior | 1.3 | -------- | 10.9 | -------- | -------- | 12 |
| 4 factors | 29 | -------- | 1.4 | -------- | -------- | 8.1 |
| 3–4 factors | 62 | -------- | 13.9 | -------- | -------- | 34.5 |
TLGS: Tehran Lipid and Glucose Study, ARIC: Atherosclerosis Risk in Communities study, SCORE: the heart strategies concentrating on risk evaluation (Heart SCORE) study, NHANES: National Health and Nutrition Examination Survey, CHED: Chinese Health Examination Database.
Only 2 participants had all 4 ideal CV health behaviors, and 1.3% had 3 to 4 ideal CV health behaviors. The majority (73.9%) of men and 68.8% of women met only 0 to 1 ideal CV health behaviors. These results are especially concerning because TLGS is a cohort study, and the frequency of 0 to 1 ideal CV health behaviors might be higher in the community. There is a causal relationship between CV health behaviors and factors.14 However in our study, about 62% of participants exhibited 3 to 4 ideal CV health factors despite very low frequency of 3 to 4 ideal CV health behaviors (1.3%), which differs from other studies. This difference may be because of the following reasons: first, relatively younger age of our study population than other studies. 11,18 Younger individuals have higher frequency of ideal CV health factors than older individuals despite the lower frequency of ideal smoking and healthy diet.14 When individuals get older and develop CVD or CVD risk factors such as hypertension and diabetes mellitus, they might follow healthier lifestyle leading to lower frequency of 3 to 4 ideal CV health factors despite higher frequency of 3 to 4 ideal CV health behaviors in older populations. Second, the frequency of ideal physical activity may be underestimated in our study because we only considered leisure time physical activity. When we included household and job activities, the frequency of ideal physical activity was extremely overestimated, which was not consistent with other studies19–21 and was far from reality. Third, we considered all 5 components of AHA healthy diet leading to the lower frequency of ideal level of healthy diet and 3 to 4 ideal CV health behaviors than the other studies that used less strict diet scoring or included fruits and vegetables as sole criterion for healthy diet.16
Women exhibited greater numbers of ideal CV health metrics than men, which may be attributed to the lower frequency of smoking in women. The frequency of poor and intermediate smoking was about 14.2%, which was consistent with the results of previous Iranian reports. The prevalence of smoking has been reported 10.6% to 20.6% in previous studies.19,22,23 The Frequencies of ideal, intermediate, and poor BMI (overweight and obesity) were 31.3%, 42.9%, and 25.8%, respectively. These results are comparable with the reports from TLGS in phase 1 (1999–2001) and National Surveillance of Risk Factors of Non-Communicable Diseases in Iran. According to these two reports, the prevalence of overweight was 40% and 36.3%, respectively, and the prevalence of obesity was 23.1% and 22.3%, respectively.22,24
Overall, frequencies of ideal smoking, diet, BP, and FPG were higher in women than in men, which might be because of greater self-care in women. The frequency of ideal BMI was higher in men than in women owing to higher frequency of ideal physical activity and lower frequency of ideal smoking in men. Like other studies, the frequency of physical inactivity was higher in women than in men, which may be because of the limitation of sport places for women.
The medians of ideal and intermediate physical activities in women were less than in men, 180 and 22 versus 233.6 and 32 minutes per week of moderate intensity physical activity, respectively. These results were smaller in values than the results from NHANES 2003–2008, in which the medians of ideal and intermediate physical activities were 480 to 620 and 80 to 90 minutes per week, respectively. This difference may be attributed to the following two reasons: first, difference in cultural and socioeconomic factors and availability of sport places in these 2 communities; second, NHANES included sport, household, and transport activities, but our study included only sport and leisure time physical activities owing to overestimation of job and household activities by the participants. The means of BMI, cholesterol, FPG, and systolic and diastolic BP are comparable with other reports.11,22
There are causal relationships between physical inactivity, smoking, unhealthy dietary pattern and obesity and incidence of diabetes, hypertension, and hypercholesterolemia. Improvement in even a single CV health behavior can lead to improvement in multiple CV health factors.14 There is noteworthy evidence showing that following a healthy diet, moderate physical activity, smoking cessation, and BMI less than 25 kg/m2 associate with reduction in incidence of diabetes, hypertension, and hyperlipidemia.25–28
The limitations of the study merit were as follows: first, less than 50% of participants in TLGS phase 4 filled the FFQ. A comparison between responders and no responders showed that responders had better smoking status and lower means of BMI, FPG, total cholesterol, and hypertension, which were statistically significant. Second, the evaluation of dietary status is based on participants’ reports, and it is subject to measurement error. Third, physical activity is also based on participants’ reports, and measurement error is inevitable. We considered only sport and leisure time physical activity that may lead to underestimation of physical activity.
In summary, the frequency of ideal CV health was negligible and the frequency of intermediate CV health was about 25.5% in this cohort of adults. The majority of participants had poor CV health. Although 62% of participants exhibited 3 to 4 CV health factors, the frequency of 3 to 4 CV health behaviors was very low (1.3%). These results are especially concerning because they come from a general population-based cohort study; even the frequency of intermediate CV health might be much lower. To improve the CV health of population, we should improve CV health behaviors through multidisciplinary interventions. It needs the involvement of individuals, public health personnel, educators, and policy makers.
Acknowledgments
This study was supported by Grant No.121 from the National Research Council of the Islamic Republic of Iran. We express appreciation to the participants of district 13, Tehran, for their enthusiastic support.
Footnotes
Competing interests
The authors declare that they have no competing interests.
REFERENCES
- 1.Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. 2010;121(4):586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. Epub 2010/01/22. [DOI] [PubMed] [Google Scholar]
- 2.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, et al. Heart disease and stroke statistics--2013 update: a report from the American Heart Association. Circulation. 2013;127(1):e6–e245. doi: 10.1161/CIR.0b013e31828124ad. Epub 2012/12/15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ford ES, Ajani UA, Croft JB, Critchley JA, Labarthe DR, Kottke TE, et al. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. The New England journal of medicine. 2007;356(23):2388–98. doi: 10.1056/NEJMsa053935. Epub 2007/06/08. doi: 10.1056/NEJMsa053935. [DOI] [PubMed] [Google Scholar]
- 4.Hadaegh F, Harati H, Ghanbarian A, Azizi F. Prevalence of coronary heart disease among Tehran adults: Tehran Lipid and Glucose Study. Eastern Mediterranean health journal = La revue de sante de la Mediterranee orientale = al-Majallah al-sihhiyah li-sharq al-mutawassit. 2009;15(1):157–66. Epub 2009/05/28. [PubMed] [Google Scholar]
- 5.Motlagh B, O’Donnell M, Yusuf S. Prevalence of cardiovascular risk factors in the Middle East: a systematic review. European journal of cardiovascular prevention and rehabilitation: official journal of the European Society of Cardiology, Working Groups on Epidemiology & Prevention and Cardiac Rehabilitation and Exercise Physiology. 2009;16(3):268–80. doi: 10.1097/HJR.0b013e328322ca1b. Epub 2009/04/29. doi: 10.1097/HJR.0b013e328322ca1b. [DOI] [PubMed] [Google Scholar]
- 6.Mehio Sibai A, Nasreddine L, Mokdad AH, Adra N, Tabet M, Hwalla N. Nutrition transition and cardiovascular disease risk factors in Middle East and North Africa countries: reviewing the evidence. Annals of nutrition & metabolism. 2010;57(3 to 4):193–203. doi: 10.1159/000321527. Epub 2010/11/23. doi: 10.1159/000321527. [DOI] [PubMed] [Google Scholar]
- 7.Azizi F, Ghanbarian A, Momenan AA, Hadaegh F, Mirmiran P, Hedayati M, et al. Prevention of non-communicable disease in a population in nutrition transition: Tehran Lipid and Glucose Study phase II. Trials. 2009;10:5. doi: 10.1186/1745-6215-10-5. Epub 2009/01/27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Esfahani FH, Asghari G, Mirmiran P, Azizi F. Reproducibility and relative validity of food group intake in a food frequency questionnaire developed for the Tehran Lipid and Glucose Study. Journal of epidemiology/Japan Epidemiological Association. 2010;20(2):150–8. doi: 10.2188/jea.JE20090083. Epub 2010/02/16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Momenan AA, Delshad M, Sarbazi N, Rezaei Ghaleh N, Ghanbarian A, Azizi F. Reliability and validity of the Modifiable Activity Questionnaire (MAQ) in an Iranian urban adult population. Archives of Iranian medicine. 2012;15(5):279–82. Epub 2012/04/24. doi: 012155/AIM.007. [PubMed] [Google Scholar]
- 10.Wu HY, Sun ZH, Cao DP, Wu LX, Zeng Q. Cardiovascular health status in Chinese adults in urban areas: Analysis of the Chinese Health Examination Database 2010. International journal of cardiology. 2012 doi: 10.1016/j.ijcard.2012.09.235. Epub 2012/10/30. [DOI] [PubMed] [Google Scholar]
- 11.Folsom AR, Yatsuya H, Nettleton JA, Lutsey PL, Cushman M, Rosamond WD. Community prevalence of ideal cardiovascular health, by the American Heart Association definition, and relationship with cardiovascular disease incidence. Journal of the American College of Cardiology. 2011;57(16):1690–6. doi: 10.1016/j.jacc.2010.11.041. Epub 2011/04/16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Laitinen TT, Pahkala K, Magnussen CG, Viikari JS, Oikonen M, Taittonen L, et al. Ideal cardiovascular health in childhood and cardiometabolic outcomes in adulthood: the Cardiovascular Risk in Young Finns Study. Circulation. 2012;125(16):1971–8. doi: 10.1161/CIRCULATIONAHA.111.073585. Epub 2012/03/29. doi: 10.1161/CIRCULATIONAHA.111.073585. [DOI] [PubMed] [Google Scholar]
- 13.Graciani A, Leon-Munoz LM, Guallar-Castillon P, Rodriguez-Artalejo F, Banegas JR. Cardiovascular health in a southern Mediterranean European country: a nationwide population-based study. Circulation Cardiovascular quality and outcomes. 2013;6(1):90–8. doi: 10.1161/CIRCOUTCOMES.112.967893. Epub 2013/01/10. doi: 10.1161/CIRCOUTCOMES.112.967893. [DOI] [PubMed] [Google Scholar]
- 14.Shay CM, Ning H, Allen NB, Carnethon MR, Chiuve SE, Greenlund KJ, et al. Status of cardiovascular health in US adults: prevalence estimates from the National Health and Nutrition Examination Surveys (NHANES) 2003–2008. Circulation. 2012;125(1):45–56. doi: 10.1161/CIRCULATIONAHA.111.035733. Epub 2011/11/19. doi: 10.1161/CIRCULATIONAHA.111.035733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ford ES, Greenlund KJ, Hong Y. Ideal cardiovascular health and mortality from all causes and diseases of the circulatory system among adults in the United States. Circulation. 2012;125(8):987–95. doi: 10.1161/CIRCULATIONAHA.111.049122. Epub 2012/02/01. doi: 10.1161/CIRCULATIONAHA.111.049122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yang Q, Cogswell ME, Flanders WD, Hong Y, Zhang Z, Loustalot F, et al. Trends in cardiovascular health metrics and associations with all-cause and CVD mortality among US adults. JAMA: the journal of the American Medical Association. 2012;307(12):1273–83. doi: 10.1001/jama.2012.339. Epub 2012/03/20. doi: 10.1001/jama.2012.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dong C, Rundek T, Wright CB, Anwar Z, Elkind MS, Sacco RL. Ideal cardiovascular health predicts lower risks of myocardial infarction, stroke, and vascular death across whites, blacks, and hispanics: the northern Manhattan study. Circulation. 2012;125(24):2975–84. doi: 10.1161/CIRCULATIONAHA.111.081083. Epub 2012/05/24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bambs C, Kip KE, Dinga A, Mulukutla SR, Aiyer AN, Reis SE. Low prevalence of “ideal cardiovascular health” in a community-based population: the heart strategies concentrating on risk evaluation (Heart SCORE) study. Circulation. 2011;123(8):850–7. doi: 10.1161/CIRCULATIONAHA.110.980151. Epub 2011/02/16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hatmi ZN, Tahvildari S, Gafarzadeh Motlag A, Sabouri Kashani A. Prevalence of coronary artery disease risk factors in Iran: a population based survey. BMC cardiovascular disorders. 2007;7:32. doi: 10.1186/1471-2261-7-32. Epub 2007/11/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Esteghamati A, Khalilzadeh O, Rashidi A, Kamgar M, Meysamie A, Abbasi M. Physical activity in Iran: results of the third national surveillance of risk factors of non-communicable diseases (SuRFNCD -2007) Journal of physical activity & health. 2011;8(1):27–35. doi: 10.1123/jpah.8.1.27. Epub 2011/02/08. [DOI] [PubMed] [Google Scholar]
- 21.Momenan AA, Delshad M, Mirmiran P, Ghanbarian A, Azizi F. Leisure Time Physical Activity and Its Determinants among Adults in Tehran: Tehran Lipid and Glucose Study. International journal of preventive medicine. 2011;2(4):243–51. Epub 2011/12/17. [PMC free article] [PubMed] [Google Scholar]
- 22.Azizi F, Rahmani M, Emami H, Mirmiran P, Hajipour R, Madjid M, et al. Cardiovascular risk factors in an Iranian urban population: Tehran lipid and glucose study (phase 1) Sozial- und Praventivmedizin. 2002;47(6):408–26. doi: 10.1007/s000380200008. Epub 2003/03/20. [DOI] [PubMed] [Google Scholar]
- 23.Meysamie A, Ghaletaki R, Haghazali M, Asgari F, Rashidi A, Khalilzadeh O, et al. Pattern of tobacco use among the Iranian adult population: results of the national Survey of Risk Factors of Non-Communicable Diseases (SuRFNCD -2007) Tobacco control. 2010;19(2):125–8. doi: 10.1136/tc.2009.030759. Epub 2009/12/17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Esteghamati A, Meysamie A, Khalilzadeh O, Rashidi A, Haghazali M, Asgari F, et al. Third national Surveillance of Risk Factors of Non-Communicable Diseases (SuRFNCD -2007) in Iran: methods and results on prevalence of diabetes, hypertension, obesity, central obesity, and dyslipidemia. BMC public health. 2009;9:167. doi: 10.1186/1471-2458-9-167. Epub 2009/06/02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Goodpaster BH, Delany JP, Otto AD, Kuller L, Vockley J, South-Paul JE, et al. Effects of diet and physical activity interventions on weight loss and cardiometabolic risk factors in severely obese adults: a randomized trial. JAMA: the journal of the American Medical Association. 2010;304(16):1795–802. doi: 10.1001/jama.2010.1505. Epub 2010/10/12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Harati H, Hadaegh F, Momenan AA, Ghanei L, Bozorgmanesh MR, Ghanbarian A, et al. Reduction in incidence of type 2 diabetes by lifestyle intervention in a middle eastern community. American journal of preventive medicine. 2010;38(6):628–36. doi: 10.1016/j.amepre.2010.03.003. e1. Epub 2010/05/25. doi: 10.1016/j.amepre.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 27.Esmaillzadeh A, Azadbakht L. Food intake patterns may explain the high prevalence of cardiovascular risk factors among Iranian women. The Journal of nutrition. 2008;138(8):1469–75. doi: 10.1093/jn/138.8.1469. Epub 2008/07/22. [DOI] [PubMed] [Google Scholar]
- 28.Mozaffarian D, Kamineni A, Carnethon M, Djousse L, Mukamal KJ, Siscovick D. Lifestyle risk factors and new-onset diabetes mellitus in older adults: the cardiovascular health study. Archives of internal medicine. 2009;169(8):798–807. doi: 10.1001/archinternmed.2009.21. Epub 2009/04/29. [DOI] [PMC free article] [PubMed] [Google Scholar]