Abstract
BACKGROUND AND OBJECTIVES
Several techniques are available to facilitate nasogastric (NG) tube insertion with or without using other instruments to guide the NG tube to the stomach. This study aimed to determine the success rate and time required for inserting NG tube by 2 non-instrumental methods of NG tube insertion and compare the findings with the common method of NG tube insertion.
DESIGN AND SETTINGS
A prospective randomized, controlled clinical trial carried out at Chang Gung Memorial Hospital in Taiwan.
SUBJECTS AND METHODS
A total of 150 patients were randomized into 3 groups: control group, neck flexion with lateral pressure group, and lifting of the larynx group. The number of attempted insertions, success rate, duration of insertion, and various complications were recorded.
RESULTS
Both neck flexion with lateral pressure and lifting of the thyroid cartilage techniques had high success rates; however, the time required to insert the NG tube was shortest in the thyroid cartilage lifting group.
CONCLUSION
Neck flexion with lateral pressure and lifting of the thyroid cartilage are convenient and reliable techniques for NG tube insertion without using any other instruments. Lifting of the thyroid cartilage had the highest success rate and was less time consuming than the other NG tube insertion techniques. Familiarization with the procedure influenced the success rate and the time required for insertion.
The insertion of a nasogastric (NG) tube in anesthetized or unconscious patients is a challenging process with a high rate of failed attempts.1,2 Many techniques have been suggested to facilitate NG intubation in anesthetized patients.2–16 Recently, two randomized, controlled studies compared interventional methods of NG tube insertion using various guidewires, GlideScope, slit tracheal tube, and frozen NG tubes and compared them with techniques not requiring anything but an NG tube such as the neck flexion with lateral pressure technique. 2,3
In this study, we compared two convenient methods of placing an NG tube with the most common method of NG tube insertion. We hypothesized that some simple techniques of NG tube insertion without using any other instruments may have a high success rate when performed by experienced clinicians.
SUBJECTS AND METHODS
The study protocol was approved by the Institutional Review Board of Chang Gung Memorial Hospital (No: 98-2669B) and the Australian New Zealand Clinical Trial Registry (ACTRN12611000423910). A written informed consent was obtained from each patient.
Study design
This was a prospective, randomized, clinical study. Preanesthesia assessment was carried out by an anesthesiologist who was blind to the study.
Inclusion criteria
Patients between 20 and 70 years of age with the ASA’s (American Society of Anesthesiologists’) physical status classification I to III, who received general anesthesia for gastrointestinal surgeries that required NG tube insertion, were enrolled in this study.
Exclusion criteria
Patients with particular predispositions to injury from NG tube placement were excluded, including those with head trauma, esophageal varices, alkali ingestion, nasal septal deviation, upper airway anomalies, and coagulopathy.
Interventions
General anesthesia was induced with intravenous injection of fentanyl 2 mg/kg, lidocaine 0.5 mg/kg, propofol 2 mg/kg, and cisatracurium 0.5 mg/kg. Female patients were intubated with a 7.0-mm internal diameter endotracheal tube. Male or females patients weighing over 80 kg were intubated with a 7.5-mm internal diameter endotracheal tube. Anesthesia was maintained by sevoflurane, and an end-tidal concentration of 1 to 1.5 minimum alveolar concentration was confirmed before starting any of the NG tube insertions.
An Fr. 14, 125-cm NG tube was used in all cases, and the insertion was performed by 2 anesthesiologists who were very experienced in NG tube insertion in anesthetized patients by these methods. Two cotton sticks were soaked in a water-soluble lubricant and inserted gently into the patients’ nostrils to check for patency. The distal end of the NG tube was lubricated in all cases and passed through the largest patent nostril to the nasopharynx. The tube was then advanced into the posterior oropharynx according to the selected technique. In Group C, the NG tube was inserted directly through a selected nostril with the head being maintained in the neutral position. In Group F, the patient’s head was flexed and lateral pressure was applied over the neck during placement of the NG tube. In Group L, NG tube insertion was facilitated by simply lifting the thyroid cartilage. Proper gastric placement was verified by epigastric auscultation and aspiration of gastric contents.
If the first attempted NG tube insertion failed, it was fully withdrawn and cleaned. The tube was relubricated and reinserted into the same nostril and advanced forward by the same technique. If both attempts at insertion were unsuccessful then the selected technique was considered a failure. All failure cases were rescued with the assistance of a laryngoscope and Magill forceps to advance the tube under direct vision.
The NG tube length required to reach the stomach was estimated by measuring the distance from the patient’s xiphoid process to the earlobe via the nose.17 The procedure start time was defined as when the NG tube was inserted into the chosen nostril. The end time was defined as the time after the successful insertion was verified by epigastric auscultation and aspiration of gastric contents.
The following data were recorded and calculated:
Success rates of the selected technique for the first attempt, second attempt, and overall.
Time required for the successful first attempt.
Time required to rescue the failed first attempt, which started from the moment that the first attempt was proven to be failed until the NG tube was successfully inserted. This included the time required to clean and relubricate the NG tube, time required for the second attempt, and laryngoscopy with Magill forceps when both attempts at insertion using the selected technique were unsuccessful.
The mean insertion time was the time required to successfully complete the procedure, starting from the moment the NG tube was inserted into the nostril until the successful insertion was verified.
Various complications during insertion, including kinking, knotting, and bleeding.
Randomization
A total of 150 patients were enrolled in the study. The patients were randomly allocated to 1 of the 3 groups using a computerized, random allocation software program: control group (Group C), neck flexion with lateral neck pressure technique (Group F), and lifting of the thyroid cartilage technique (Group L). The patients did not know which group they were enrolled in and the performer of the NG tube insertion was not informed of which group the patient was enrolled in, until sevoflurane end-tidal concentration of at least 1 minimum alveolar concentration was confirmed.
Statistical analysis
A pilot study of 15 cases per group suggested an approximate 25% improvement (60%–85%) in the success rate using these techniques. Consequently, power calculation (α=0.05 and β=0.2) indicated a minimum of 48 patients for each group. Demographic data were presented as count (percentage) for categorical data and mean (SD) for continuous data. Categorical data were analyzed using Pearson chi-square or Fisher exact test. Continuous data were analyzed using ANOVA or Kruskal–Wallis test. A P value of less than .05 was considered statistically significant. SPSS software version 17 (SPSS Inc., Chicago, IL, USA) was used for all statistical analyses.
RESULTS
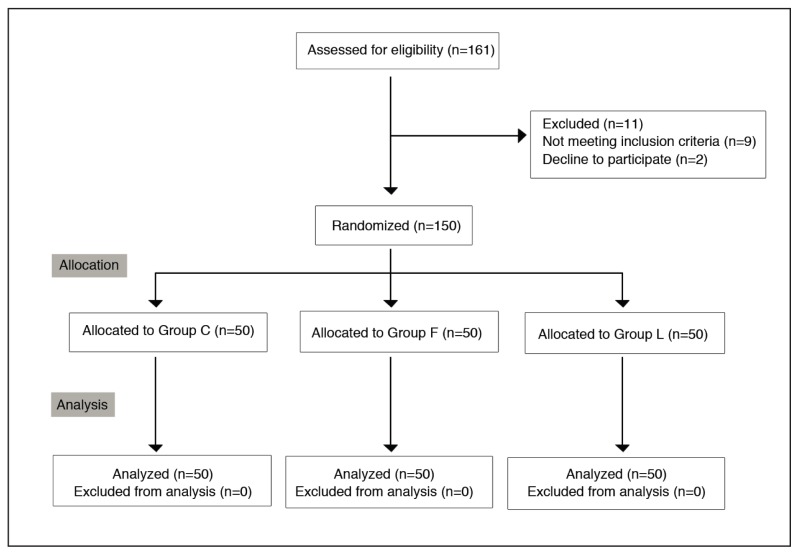
Of 161 patients who were initially assessed, 150 patients were enrolled into the study (Figure 1). No statistically significant differences were observed in the demographic data (gender, age, height, weight, and BMI) between all 3 study groups (Table 1).
Figure 1.
Consort flow diagram. C: control, F: neck flexion with lateral pressure, L: lifting of the thyroid cartilage.
Table 1.
Patient characteristics.
| Variables | Group C (n=50) | Group F (n=50) | Group L (n=50) | Statistical test results |
|---|---|---|---|---|
|
| ||||
| Gender (male/female) | 22/28 | 24/26 | 23/27 | P=.923 (Pearson Chi-square test) |
| Age (y) | 56.3 (9.2) | 55.6 (9.5) | 55.8 (9.8) | P =.942 (ANOVA) |
| Height (cm) | 161.2 (6.9) | 161.0 (8.4) | 161.2 (7.4) | P=.988 (ANOVA) |
| Weight (kg) | 62.7 (10.8) | 61.7 (12.7) | 62.1 (9.0) | P=.890 (ANOVA) |
| BMI (kg/m2) | 24.1 (3.4) | 23.7 (4.1) | 23.9 (2.9) | P=.888 (ANOVA) |
Values are expressed as mean (SD) or numbers. C: Control, F: neck flexion with lateral pressure, L: lifting of the thyroid cartilage.
In Group C, a successful NG tube insertion was achieved in 30/50 patients (60%) (Table 2), with 26/50 (52%) tubes being inserted in the first attempt and 4/24 (16.7%) tubes in the second attempt. In Group F, the NG tube was placed successfully in 44/50 patients (88%, P<.003 compared with Group C). Successful insertions were recorded in 41/50 (82%) patients in the first attempt, and in 3/9 33%) patients in the second attempt. The success rates for NG tube insertion were high in Group F, but they were even higher in Group L, where 46/50 (92%) successful insertions were accomplished (P<.001 compared with Group C). Successful insertions were achieved in the majority 44/50 (88%) of patients in the first attempt, and only 6 second attempts were needed, of which 2 (33%) were successful.
Table 2.
Success rates of nasogastric tube insertion.
| Variables | Group C (n=50) | Group F (n=50) | Group L (n=50) | Statistical test results |
|---|---|---|---|---|
|
| ||||
| First attempt | 26 of 50 (52%) | 41 of 50 (82%) | 44 of 50 (88%) |
P values (Fisher exact test) F vs C P <.001 L vs C P<.001 F vs L P=.401 |
| Second attempt | 4 of 24 (16.7%) | 3 of 9 (33%) | 2 of 6 (33%) | |
| Overall success rate | 30 of 50 (60%) | 44 of 50 (88%) | 46 of 50 (92%) | P values (Fisher exact test) F vs C P=.003 L vs C P<.001 F vs L P=.505 |
Values are expressed as numbers (%). C: Control, F: neck flexion with lateral pressure, L: lifting of the thyroid cartilage.
The time required for a successful first attempt was 20.8 (4.8) s in Group C (Table 3), 25.6 (2.9) s in Group F, and 19.8 (4.0) s in Group L. The time required for a successful first attempt was longer in group F (P<.001 compared with Group C). There were no statistically significant differences in the time required for a successful first attempt between Groups C and L (P=.401). The mean time required to rescue a failed first attempt was 70.0 (18.1) s in Group C, 77.0 (18.9) s in Group F, and 55.5 (19.1) s in group L. The time required to rescue a failed first attempt was shorter in group L; however, there were no statistically significant differences when compared with the other groups. The mean insertion time was 26.7 (16.0) s in Group C, 29.5 (14.8) s in Group F, and 21.3 (8.4) s in Group L. The mean insertion time in Group L was significantly shorter compared with Group F (P=.012); however, there was no statistically significant difference when compared with Group C (P=.253).
Table 3.
Time required for successful nasogastric tube insertion.
| Variables | Group C | Group F | Group L | Statistical test results |
|---|---|---|---|---|
|
| ||||
| Time required for successful first attempt | 20.8 (4.8) | 25.6 (2.9) | 19.8 (4.0) |
P values (Kruskal–Wallis test) F vs C P<.001 L vs C P=.453 F vs L P<.001 |
| Time required to rescue a failed first attempt | 70.0 (18.1) | 77.0 (18.9) | 55.5 (19.1) |
P values (Kruskal–Wallis test) F vs C P=.077 L vs C P=.165 F vs L P=.083 |
| The mean insertion time: | 26.7 (16.0) | 29.5 (14.8) | 21.3 (8.4) | P values (ANOVA) F vs C P=1 L vs C P=.253 F vs L P=.012 |
Values are expressed as mean (SD). C: Control, F: neck flexion with lateral pressure, L: lifting of the thyroid cartilage.
Tubal kinking was the most common complication observed in Groups C, F, and L, occurring in 20 (40%), 8 (16%), and 6 (12%) patients, respectively (Table 4). The second most common complication was coiling of the NG tube in the mouth, which occurred simultaneously with kinking or individually in 19 (38%) Group C patients, and 2 (4%) patients in Group F. Bleeding was the third most common complication, which developed in 5 (10%) patients in Group C, 1 (2%) patient in Group F, and 1 (2%) patient in Group L, and the incidence of bleeding increased with repeated attempts. Bradycardia was recorded while re-attempting NG tube insertion for 1 (2%) patient in Group L. The knotting of the tube developed in 1 (2%) patient in Group F.
Table 4.
Complications of NG tube insertion as seen in this study.
| Complication | Group C (n=50) | Group F (n=50) | Group L (n=50) |
|---|---|---|---|
|
| |||
| Kinking | 20 (40%) | 8 (16%) | 6 (12%) |
| Coiling | 19 (38%) | 2 (4%) | 0 |
| Bleeding | 5 (10%) | 1 (2%) | 1 (2%) |
| Bradycardia | 0 | 0 | 1 (2%) |
| Knotting | 0 | 1 (2%) | 0 |
Values are expressed as numbers (%). C: Control, F: neck flexion with lateral pressure, L: lifting of the thyroid cartilage.
DISCUSSION
Direct NG tube insertion in anesthetized and intubated patients is difficult. Therefore, many techniques have been suggested to improve the success rate of NG tube insertion. Some studies have compared instrument or guide wire–assisted methods and other simple techniques of NG tube insertion.2,3
Appukutty and Shroff2 compared 3 different techniques with the most common method of NG tube insertion. Two of these techniques included using other instruments such as ureteral guide wires and slit tracheal tubes, and the third was a non-instrumental neck flexion and lateral pressure technique. They suggested that these techniques can increase the success rate of NG tube insertion, and also that neck flexion with lateral pressure is the easiest technique with a high success rate. Kirtania et al3 compared the success and failure rates of NG tube insertion using esophageal guide wires and other techniques described in previous studies (using ureteral guide wires, slit tracheal tubes, GlideScope, water-filled NG tubes, frozen NG tubes, neck flexion and lateral pressure, forward displacement of the larynx, and inflation of the esophagus with air). They concluded that an esophageal guide wire with forward displacement of the larynx nearly always resulted in the success of NG tube insertion.
In this study, we compared 3 methods of placing the NG tube without using any other instruments. Both head flexion with lateral neck pressure and lifting of the thyroid cartilage techniques had high success rates compared with the control group. Lifting of the thyroid cartilage technique had the highest success rate in this study; however, the reported success rates using these methods have differed from study to study (Table 5). These variations in success rates when using the same technique may be based on operator experience and familiarization with the procedure.
Table 5.
Comparison of the success rates using the techniques described in this study and two randomized studies.
| Author | References | Sample size in each method | Success rates | ||
|---|---|---|---|---|---|
| Group C | Group F | Group L | |||
|
| |||||
| Appukutty and Shroff | 2 | 50 in C 50 in F |
72% | 92% | _ |
| Kirtania et al | 3 | 100 in F 50 in L |
_ | 72% | 52% |
| (Authors of this study) | (Present study) | 50 in C 50 in F 50 in L |
60% | 88% | 92% |
Values are expressed as numbers or percentage. C: Control, F: neck flexion with lateral pressure, L: lifting of the thyroid cartilage.
Simple non-instrumental techniques such as lifting of the thyroid cartilage or neck flexion with lateral neck pressure have relatively high success rates in the first attempt of insertion. Unfortunately, after a failure, subsequent attempts using the same technique have low success rates due to a “memory effect,” that is, in subsequent attempts, the NG tube tends to kink at the same place. In addition, the warming of the NG tube to body temperature makes it softer, which can also contribute to the subsequent failure.2,4
The mean time required for a successful insertion by these convenient and non-instrumental techniques was relatively shorter than the time required for NG insertion by other instrumental techniques in previous studies. As almost no instruments are required during NG tube insertion, time can be saved even after the procedure because there is no need to wash or sterilize any instruments. The shortest mean insertion time was recorded in the lifting of thyroid cartilage group. The mean time required for a successful insertion was also influenced by operator experience and familiarization with the procedure.
Hypothetically, if the success rate of NG tube insertion in the first attempt by a selected technique is high, then less time is required to rescue failed attempts and the mean time of insertion by this technique will be short. In this study, lifting of the thyroid cartilage technique had the highest success rate of NG tube insertion in the first attempt (P<.001 compared with Group C), however there were no statistically significant differences in the time required to rescue the failed attempts between all 3 groups. The mean insertion time of the group with the highest success rate in the first attempt (Group L) was the shortest among all 3 groups; however, there was no significant difference when compared with the control group that had the lowest success rate in the first attempt of insertion. Therefore, to reduce the time required to rescue a failed attempt and to increase the success rate of a second attempt, we suggest changing to other techniques or using techniques that have guaranteed or near guaranteed success of NG tube insertion for subsequent attempts. In this study and many previous studies, failed intubations were rescued through the assistance of a laryngoscope with Magill forceps. Kirtania et al3 mentioned that esophageal guide wire–assisted techniques have near guaranteed success of NG tube insertion. These and any other instrumental techniques may have very high success rates; however, we suggest that they should be used as “rescue technique” when NG tube insertion by a simple less-instrumental technique has failed.
Kinking and coiling of the NG tube were the most common complications in this study, which is consistent with previous reports.2,17 Repeated attempts and instrumentation have been reported to increase the incidence of traumatic bleeding.2 In this study, there were lower incidences of kinking, coiling, and bleeding in the lifting of the thyroid cartilage and neck flexion groups than in the control group. Therefore, choosing a technique with a high success rate without the use of other instruments can decrease the incidence of these complications. However, vigorous palpitation of the thyroid cartilage and adjacent structures may activate a carotid sinus reflex, as observed in 1 patient in Group L where a slight decrease in the heart rate was noted after repeated attempts. This patient’s heart rate was restored shortly after stopping neck manipulation. However, neck manipulation can allow for the detection of tubal impactions that can be corrected by a slight rotation of the NG tube.
Finally, it is important to mention that lifting of the thyroid cartilage can be performed in all patients except for those with severe swelling over the neck area, or those with neck masses such as patients with deep neck infections or a massive thyroid mass where lifting of the thyroid cartilage is difficult and unsafe. In such patients, the neck flexion technique is more appropriate to place an NG tube under anesthesia. In contrast, it is wise to avoid using the neck flexion technique in patients with a limited range of neck motion such as in those with cervical spine injury, or in those with previous cervical spine surgeries. In such cases, NG tube insertion can be facilitated by gentle lifting of the thyroid cartilage.
In conclusion, neck flexion with lateral pressure and lifting of the thyroid cartilage are 2 of the most convenient, fast, and reliable techniques for NG tube insertion in anesthetized patients without the need of other instruments. The proper use of the lifting of the thyroid cartilage technique provides a high success rate of NG tube insertion and is less time consuming than any other techniques of NG tube insertion. We suggest the use of this technique for routine performances and to save all other instrumental techniques for the rescue of difficult placements or in cases where neck manipulation is contraindicated. Finally, familiarization with the procedure can greatly influence the success rate and time required for insertion.
Acknowledgments
Hsiao-Jung Tseng and Yu-Jr Lin, Biostatistical Center for Clinical Research.
REFERENCES
- 1.Bong CL, Macachor JD, Hwang NC. Insertion of the nasogastric tube made easy. Anesthesiology. 2004;101:266. doi: 10.1097/00000542-200407000-00058. [DOI] [PubMed] [Google Scholar]
- 2.Appukutty J, Shroff PP. Nasogastric tube insertion using different techniques in anesthetized patients: a prospective, randomized study. Anesth Analg. 2009;119:832–835. doi: 10.1213/ane.0b013e3181af5e1f. [DOI] [PubMed] [Google Scholar]
- 3.Kirtania J, Ghose T, Garai D, Ray S. Esophageal guidewire-assisted Nasogastric Tube insertion in anesthetized and intubated patients: a prospective randomized controlled study. Anesth Analg. 2012;114:343–348. doi: 10.1213/ANE.0b013e31823be0a4. [DOI] [PubMed] [Google Scholar]
- 4.Tsai YF, Luo CF, Illias A, Lin CC, Yu HP. Nasogastric tube insertion in anesthetized and intubated patients: a new reliable method. BMC gastroenterology. 2012;12:99. doi: 10.1186/1471-230X-12-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lind LJ, Wallace DH. Submucosal passage of a nasogastric tube complicating attempted intubation during anesthesia. Anesthesiology. 1978;49:145–147. doi: 10.1097/00000542-197808000-00023. [DOI] [PubMed] [Google Scholar]
- 6.Mundy D. Another technique for insertion of nasogastric tubes. Anesthesiology. 1979;50:374. doi: 10.1097/00000542-197904000-00022. [DOI] [PubMed] [Google Scholar]
- 7.Mahajan R, Gupta R, Sharma A. Role of neck flexion in facilitating nasogastric tube insertion. Anesthesiology. 2005;103:446–447. doi: 10.1097/00000542-200508000-00034. [DOI] [PubMed] [Google Scholar]
- 8.Ozer S, Benumof JL. Oro- and nasogastric tube passage in intubated patients: fiberoptic description of where they go at the laryngeal level and how to make them enter the esophagus. Anesthesiology. 1999;91:137–143. doi: 10.1097/00000542-199907000-00022. [DOI] [PubMed] [Google Scholar]
- 9.Gombar S, Khanna AK, Gombar KK. Insertion of a nasogastric tube under direct vision: another atraumatic approach to an age-old issue. Acta Anaesthesiol Scand. 2007;51:962–963. doi: 10.1111/j.1399-6576.2007.01347.x. [DOI] [PubMed] [Google Scholar]
- 10.Mahajan R, Gupta R, Sharma A. Insertion of a nasogastric tube using a modified ureteric guide wire. J Clin Anesth. 2009;21:387–388. doi: 10.1016/j.jclinane.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 11.Chun DH, Kim NY, Shin YS, Kim SH. A randomized, clinical trial of frozen versus standard nasogastric tube placement. World J Surg. 2009;33:1793–1794. doi: 10.1007/s00268-009-0144-x. [DOI] [PubMed] [Google Scholar]
- 12.Matsuki A, Zsigmond EK. Simple and reliable method of inserting a nasogastric tube during anaesthesia. Br J Anaesth. 1972;44:610. doi: 10.1093/bja/45.10.1062. [DOI] [PubMed] [Google Scholar]
- 13.Hunter C, Cohen S. A new use for the GlideScope. Anesth Analg. 2006;13:509. doi: 10.1213/01.ANE.0000227427.99390.24. [DOI] [PubMed] [Google Scholar]
- 14.Campbell B. A novel method of nasogastric tube insertion. Anaesthesia. 1997;52:1234. [PubMed] [Google Scholar]
- 15.Hung CW, Lee WH. A novel method to assist nasogastric tube insertion. Emerg Med J. 2008;25:23– 25. doi: 10.1136/emj.2007.049312. [DOI] [PubMed] [Google Scholar]
- 16.Mahajan R, Gupta R. Another method to assist nasogastric tube insertion. Can J Anaesth. 2005;52:652–653. doi: 10.1007/BF03015781. [DOI] [PubMed] [Google Scholar]
- 17.McConnell EA. Inserting a nasogastric tube. Nursing. 1997;27:72. doi: 10.1097/00152193-199701000-00026. [DOI] [PubMed] [Google Scholar]