Abstract
BACKGROUND AND OBJECTIVES
Knowledge regarding traumatic spine injuries (TSIs) is essential for effective prevention strategies, particularly in the developing world, where majority of the population is younger and organized prevention programs are scarce. Therefore, our objective was to describe TSI mechanisms, demographics, patterns, and outcomes in children and adolescents.
DESIGN AND SETTINGS
Retrospective chart review in a major trauma center from May 2001 to May 2009 in Riyadh, Saudi Arabia.
PATIENTS AND METHODS
Detailed chart reviews were done for all consecutive TSI patients ≤18 years old. Cases were identified through the trauma database registry that included admitted patients.
RESULTS
Of the 3796 cases identified, 120 cases (3.2%) sustained 141 TSIs (mean age: 13.5 years; males: 83.8%). TSI was most common among children from 16 to 18 years old. Overall, motor vehicle collision (MVC) was the most common injury mechanism (60.8%). However, younger patients (<12 years) sustained more pedestrian injuries (40.6%). Among MVC cases with known seat belt statuses (43.8%), 90.6% were not wearing seat belts. The cervical spine level was the most commonly affected (55.8%) region, especially in children <12 years old (88%). More than 1 affected spinal level was found in 23.3% cases. Spinal cord injuries were found in 19.2% cases. Overall, mortality was 8.3%, and half of these mortalities were secondary to pedestrian injuries. A total of 22.7% of cases were discharged with neurological deficits.
CONCLUSION
The high frequency and severity of MVC and pedestrian injuries observed in the present study raise significant concerns regarding the safety of children on the roads. Spine involvement was age specific; younger patients tended to have more cervical injuries, and older patients exhibited more thoracic spine involvement.
Traumatic spine injuries (TSIs) in children are relatively infrequent.1–5 TSIs constitute 5% of child trauma and 1% to 10% of all reported spinal injuries.6–8 The annual incidences of pediatric TSI are 66 and 74 cases per million people in Finland and the United States, respectively.5,9 The mortality rates of TSI have been reported to be higher in adults (estimated at 25%–32%), and mortality is most frequently associated with organ injuries.10–16 Associated neurological compromises have been reported to occur at rates of 25% to 50%.10,12 Males are more frequently affected than females, presumably owing to greater riskier behavior and reduced seat belt use.3,5,17,18
The pediatric spine is more flexible than the adult spine, which results in different patterns of injury.17,19 For example, infants exhibit a low incidence of TSI because hyper-lax ligaments enhance the elasticity of their spines. Furthermore, the facet joints of infants are more horizontally oriented, infants’ neck muscles are underdeveloped, and infants have larger head sizes in relation to their torsos.17,20,21 Therefore, most infant spine injuries involve the craniocervical area.21 In contrast, older children (older than ~8 years) have stronger muscles, less elastic ligaments, well-calcified bones with increased densities and sizes, and more developed body structures in which the head is smaller in relation to the torso.20,22 These anatomical developments shift the risk of spinal injuries in adults to the level of the spine’s fulcrum (C5–C6).20,22
In the developing world, traumatic injuries in adults and children are primarily attributable to motor vehicle collisions (MVCs), which tend to involve males more commonly than females.18,23,24 However, a high percentage of pediatric head traumas are related to pedestrian injuries.23 Epidemiological studies on TSI in children of Saudi Arabia are scarce. Individual reports commenting on the frequencies with which camel accidents cause significant spinal injuries in adults have been published.25–27 Our primary goal was to identify the mechanisms and patterns of spinal injuries in patients 18 years of age or below in a major trauma center. Our secondary goal was to identify the epidemiological characteristics and outcomes of such injuries. Such data will enhance our understanding of pediatric TSI and facilitate injury prevention strategies and health service allocation.
PATIENTS AND METHODS
Study design and setting
This is a retrospective study conducted at King Abdulaziz Medical City (KAMC), Riyadh. All consecutive cases with any traumatic spine injury in patients of 18 years of age or below from May 2001 to May 2009 were included. Spinal injury was defined in the database as any fracture in the spine with or without spinal cord injury (SCI). Exclusion criteria included pathologic fractures or birth-related injuries.
Cases were identified from the trauma database of the KAMC Trauma Registry (KAMC-TR). This database is a prospectively recorded database of all admitted trauma cases. A full-time registrar is responsible for data collection and patient follow-up until discharge. Annual audits of 5% of the data against medical records are performed for quality assurance. Additionally, a cross-check of the database is performed against daily reports of all discharged trauma patients, which are generated from the medical records.
The study was conducted in the city of Riyadh, which comprises 24.1% of the country’s population and is home to 5.8 million residents.28 The median age of the Saudi population is 21 years, and children under 19 years of age constitute 41.7% of the total population. 13 Major traumas are transferred to designated hospitals based on the geographic location. KAMC is one of the largest dedicated centers for trauma in the country.
Data variables
Data were gathered through a detailed review of all medical files of the included patients. Factors pertaining to patient and injury characteristics, hospital admissions, surgical interventions, and clinical statuses at the most recent follow-up were included.
Injury assessment was performed at hospital presentation using the injury severity score (ISS) and the Glasgow coma scale (GCS). The ISS is a well-established trauma scoring system that ranges from 1 to 75; major traumas are indicates by scores greater than 16.29,30 The GCS is an objective measure for the assessment of an individual’s conscious state following head injury and ranges between 3 (deep unconsciousness) and 15 (fully awake).31
With the goal of implementing an applicable trauma prevention strategy, patients were stratified into 4 groups according to age at the time of injury: children under 6, elementary school age (6≤12), intermediate school age (12≤16), and high school age (16–18).
Statistical analyses
Statistical analyses were performed using SPSS, version 17.0 (IBM Corporation, Armonk, NY, USA). Descriptive statistics (means, standard deviations, proportions) were used to describe quantitative and categorical variables. Chi-square and Fisher exact tests were used to compare categorical variables. The Kruskal-Wallis and Mann-Whitney tests were used to compare quantitative measures. Correlations involving nonparametric data were examined with Spearman correlation coefficients. Results with P values of .05 or below were considered statistically significant.
RESULTS
Patient demographics
A total of 8941 trauma patients were identified during the study period, and 3796 of these patients were at or below 18 years of age. Of these younger patients, 120 had sustained a spine injury (3.2% of all pediatric trauma cases). These patients had a total of 141 spinal fractures. The mean age was 13.5 (range 2–8). Injuries were most frequent in the age group of 16 to 18 years old (49.2%, Table 1). Males were affected significantly more frequently (83.8%, P=.003) across all age groups, and this pattern was particularly evident for those older than 12 years of age (P=.0001).
Table 1.
Characteristics of study population (actual patient numbers).
| Age group (y) | Total | P value | ||||
|---|---|---|---|---|---|---|
| >6 y | 6–11.9 | 12–15.9 | 16–18 | |||
|
| ||||||
| Number of patients (%) | 13 (10.8%) | 19 (15.8%) | 29 (24.2%) | 59 (49.2%) | 120 | |
| Sex | ||||||
| Male | 8 | 12 | 27 | 53 | 100 (83.3%) | .003 |
| Female | 5 | 7 | 2 | 6 | 20 (16.7%) | |
| Mean ISS (SD) | 13.9 (22.3) | 10.0 (6.2) | 17.7 (14.1) | 15.6 (11.6) | 15.0 (13.2) | .051 |
| Mean GCS (SD) | 12.4 (4.7) | 13.8 (2.5) | 10.9 (5.3) | 11.9 (4.4) | 12.0 (4.4) | .395 |
| Spine injury level | ||||||
| Cervical | 13 | 17 | 11 | 26 | 67 (55.8%) | .0001 |
| Thoracic | 1 | 1 | 16 | 29 | 47 (39.2%) | .0001 |
| Lumbosacral | 0 | 2 | 11 | 22 | 35 (29.2%) | .009 |
| Associated injuries | ||||||
| Spinal cord | 3 | 2 | 2 | 5 | .821 | |
| Head | 2 | 4 | 3 | 12 | 12 | |
| Body | 0 | 3 | 6 | 17 | 21 | |
| Head and body | 3 | 6 | 7 | 12 | 26 | |
| Spinal cord and head | 0 | 0 | 2 | 1 | 283 | |
| Spinal cord and body | 0 | 1 | 2 | 3 | 6 | |
| Spinal cord, head and body | 0 | 0 | 1 | 1 | 2 | |
| All spinal cord patients | 3 | 3 | 7 | 10 | 23 | |
| Outcome | ||||||
| Mortality | 3 | 1 | 3 | 3 | 10 (8.5%) | .143 |
| Neurological deficit | 2 | 0 | 9 | 14 | 25 (21.2%) | .065 |
| Full recovery | 7 | 18 | 17 | 41 | 83 (70.3%) | .043 |
| Transportation to hospital | ||||||
| Ambulance | 5 | 8 | 17 | 45 | 75 (63%) | .01 |
| Private vehicle | 8 | 11 | 11 | 14 | 44 (37%) | |
ISS: Injury severity score, GCS: Glasgow coma scale.
Mechanisms and timings of injuries
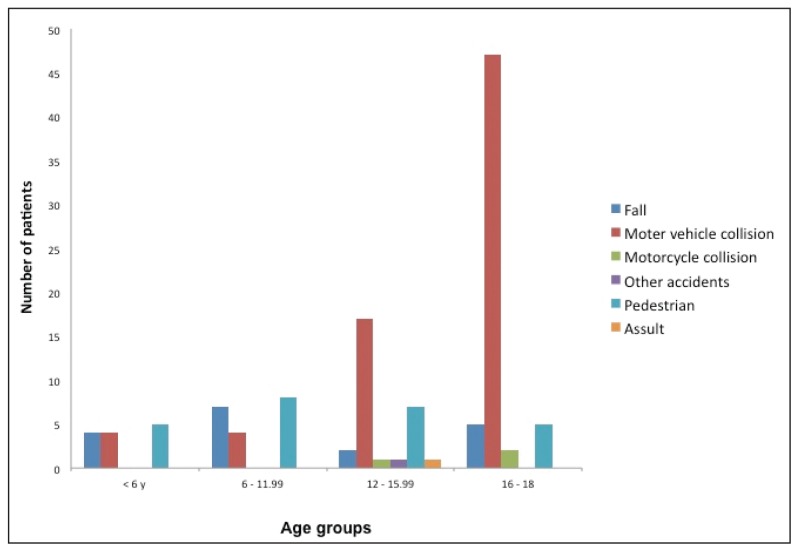
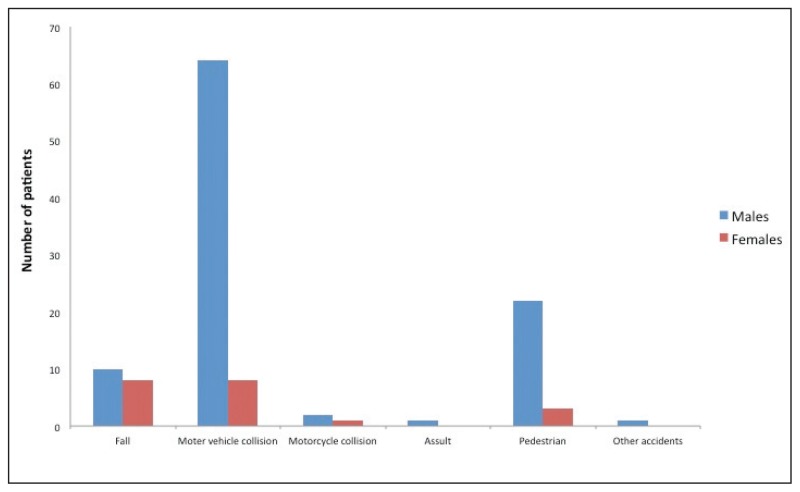
Overall, MVC was the commonest mechanism of spine injury (60.8%) followed by pedestrian injuries (20.8%), fall-related injuries (15%), and other miscellaneous injuries (3.4%, injuries related to motorcycles, assaults, or unspecified). The mechanisms of injury varied significantly across the age groups (P=.0001, Figure 1). Patients younger than 12 years old experienced pedestrian (40.6%) and fall-related (34.4%) injuries. Among the older patients (12–18 years), injuries were mostly caused by MVC (72.7%). The mechanisms of spine injury were significantly different between males and females (P=.013). Among females, injuries were caused equally by falls and MVC (40% each); however, MVC was the main cause of injuries (64%) in males followed by pedestrian injuries (22%) (Figure 2).
Figure 1.
Mechanism of injury by age group.
Figure 2.
Mechanism of injury by gender.
Injuries reached their peak during the day at 10 o’clock (9.2%) in the morning followed by 8 o’clock (7.5%) in the evening. Across the study period, more spine injuries occurred in 2005 (21.7%) than in any other year in our cohort.
Seat belt usage status was known in 32 of 72 MVC cases (44.5%). Of the cases with known seat belt statuses, seat belts were used in only 3 cases (9.4%).
Transportation to the hospital
The methods by which patients were transferred to the hospital included ambulances (63%) and private vehicles (37%, Table 1). The average age at transfer by a private vehicle was 11 years, and the average age at transfer by an ambulance was 14.7 years (P=.0001). Regarding age categories, patients under 12 years old were most likely to be transferred to the hospital in a private vehicle (59.4%), and patients older than 12 years were most likely to be transferred in an ambulance (71.3%, P=.002). Regarding gender, males were most likely to be transferred by an ambulance (67%), and females were most likely to be transferred by private vehicles (60%, P=.019).
Following injuries on the road, 29% of patients were transferred in a private vehicle. Two patients were injured at home and transferred in a private vehicle, and 1 patient was injured at school and transferred in an ambulance. Private vehicles were used to transfer 48.5% of patients with cervical injuries (P=.004), 34% of patients with thoracic injuries (P=.592), and 23% of patients with lumbosacral injuries (P=.039). Patients transferred by an ambulance were more severely injured as indicated by a lower GCS (mean 11, P=.0001) and a trend toward a higher ISS (mean 16.5, P=.06). The statuses of spine-injury precautions taken during a private vehicle transfer are unknown.
Injury assessments and hospital stays
Across the different age groups, there were no significant differences in ISS (P=.246), lengths of stay in the hospital (P=.264), or GCS (P=.174) (Table 1). The mean length of hospital stay was 29.3 (60) days, and the maximum length of stay was 444 days. GCS was negatively correlated with both ISS (P=.001) and length of hospital stay (rs=−0.32, P=.0001). A positive correlation was observed between ISS and length of hospital stay (rs=0.44, P=.001). Injuries tended to be more severe in males as demonstrated by a higher mean ISS (16 vs 10 for males and females, respectively, P=.062) and a lower mean GCS (11.6 vs 14 for males and females, respectively, P=.059). No significant gender difference was recorded in length of hospital stay (P=.97). Pedestrian injuries were the most severe in terms of both ISS (mean 20.16, P=.006) and GCS (mean 10.08, P=.012). Surgical interventions were performed in 45.8% of all cases. Of these, 40.7% underwent spine surgery.
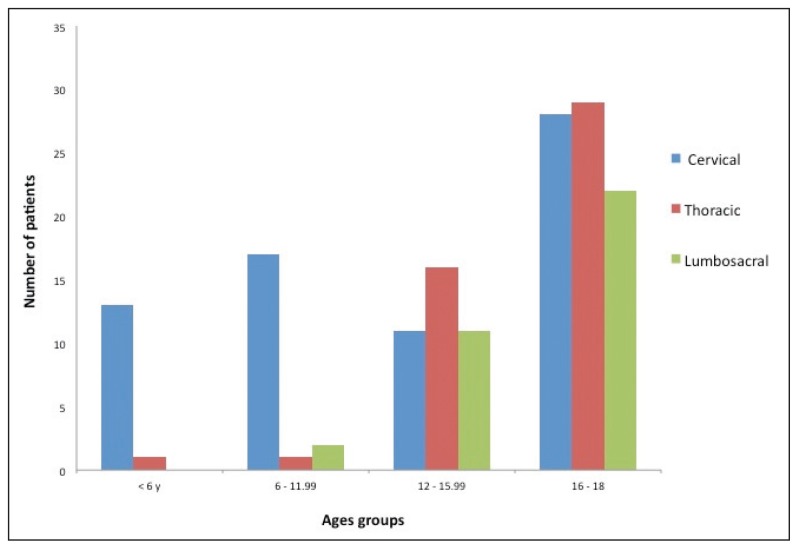
Spine and spinal cord injury
Overall, the spine was most commonly affected at the cervical level (55.8%, Table 1). More than 1 spinal region was affected in 23.3% of cases. Most of the younger patients (<12 years) sustained cervical injuries (88%), and thoracic involvement followed by cervical involvement was more common in the older cases (Figure 3).
Figure 3.
Mechanism of injury by spinal injury level.
SCI, alone or in combination with other injuries, was found in 23 patients (19.2%) (Table 1). The average age at SCI was 13.7 (4.5) years, and SCI was more common in males (74%). SCIs were most likely to be caused by MVC (56.5%) followed by fall injuries (35%), and others (8.6%). Seat belts were not used by any of the 6 patients (out of the 23) with SCI for whom seat belt status was known. Patients with SCI had a mean ISS of 10.2 (8.3) and a mean GCS of 13.4 (3.7). SCI was associated with cervical injury in 9 patients (39%), thoracic injury in 11 patients (47.8%), and lumbosacral injury in 10 patients (43.5%). None of the SCI patients died. Neurological deficits at discharge were present in 6 of the SCI patients (26%), and the other SCI patients achieved full recoveries (74%).
Outcome
Twenty-five patients (22.7% of alive patients) were discharged with neurological deficits, and 6 of cases (5.5%) were secondary to SCI. There were no significant gender (P=.054) or age differences between the patients with neurological deficits (mean age 14.7 years) and those who recovered fully (83 patients, mean age 13.6 years, P=.2). However, when the age groups were considered, 92% of the patients with neurological deficits were older than 12 years (P=.019). MVC was responsible for greatest proportion of cases of neurological deficit (68%) followed by fall and pedestrian injuries (16% each). Patients with neurological deficits exhibited higher ISSs (mean 18.7, P=.001) and lower GCSs (mean 10, P=.007). Of the 25 patients with neurological deficits, 11 sustained cervical injuries (P=.3), 14 sustained thoracic injuries (P=.045), and 10 sustained lumbosacral injuries (P=.24).
There were 10 deaths (8.3%) in the study population. Nine patients died during their hospital stays, and 1 died after discharge. The average age at death was 11 years. There was no difference in mortality across the different age groups (P=.143) and no effect of gender (P=.5). Five of the deaths (50%) were secondary to pedestrian injury, which represented 20% of all pedestrian spinal injuries in our sample. Three deaths were secondary to MVC (4% of all MVC injuries), 1 death was the result of a motorcycle accident, and 2 death was related to a fall injury. As expected, mortality cases exhibited higher ISSs (mean 38.8, P=.0001) and lower GCSs (mean 5.5, P=.0001). Out of the 10 patients who died, 9 sustained cervical injuries (P=.02), 4 suffered thoracic injuries (P=.59), and 1 suffered a lumbosacral injury (P=.16). Two of the mortality cases underwent spinal surgery and 2 underwent non-spinal surgery.
DISCUSSION
The current study is the largest in Saudi Arabia that has addressed traumatic spine injuries in children and adolescents. Spine injuries were involved in 3.2% of all admitted pediatric trauma cases, and this proportion is similar to published figures.5,8,11,12,32,33 Adolescent boys were the most likely to be affected,1,3–5,17,18,34 which is likely attributable to the increased exposure to outdoor activities and risk-taking behavior of males.35 Alternately, this finding may be due to the greater exposure of male to MVC because women do not drive in Saudi Arabia.
Mechanism of injury
As in previous reports, MVC was the main cause of TSI in the current report.3,5,8 However, the percentage of injuries caused by MVC in our study (60.8%) was much higher than international figures (25%–30%).8,18,36,37 The inclusion of the 16 to 18 year age category (i.e., the age of driving) may have contributed to the elevation in MVC-caused injuries observed in the current study. Traffic laws and regulations should be vigorous and carefully enforced to limit the frequency of these injuries, particularly because of increases in traffic activity that are related to rapid economic development.24,38 Obviously, the use of seat belts should be encourage because only 9% of those with known seat belt statuses (43.8% of total study population) were wearing their seat belts.
Pedestrian injury presents a challenge in the developing world both in terms of frequency and severity. In the current paper, pedestrian-related TSI among children and adolescents was more prevalent (20.8%) than published figures (10%).8 Pedestrian injuries were the most common cause of injury to patients under 12 years of age. Similar findings have been reported regarding head injury in the same patient group.23 Pedestrian injuries tend to be more severe and are associated with multiple organ injuries.8 The pedestrians in the current study sustained more severe injuries (i.e., worse ISS and GCS scores) and constituted 50% of all deaths. This is public health concern particularly because most injuries occurred approximately 10 am or 8 pm. These time periods are related to the timing of morning and evening school activities. Strict traffic rules and enhanced parent education have reduced the accident rates among children and adolescents in more developed countries.3 Direct adult supervision of the younger age group is required because these children lack the knowledge and cognitive and behavioral skills necessary to ensure their safety.3,39
Spine injury
The anatomic and biomechanical features of the developing pediatric spine predispose younger people to cervical injury. Similar to previous reports, the current study showed that most injuries affected the cervical spine (60%–80%).5,15,37,38,40 However, the involvement of the cervical spine was more frequent among the children younger than 12 years (94%) compared to the older patients (42%). In a population-based study by Puisto et al, 64% of younger children (<8 years) had cervical injuries compared to 25% of children over 8 years old.5 As demonstrated in the current and previous reports,5 as children age, the level of injury moves to the thoracic and lumbar areas.
The rate of spinal cord injury was higher than that reported previously in the published studies (19.2% vs 2.3%).3 However, direct comparisons are difficult due to differences in the study populations. A portion of this difference may be attributable to the comparison to countries in which more developed prevention programs have been established.3 The prognoses of children with spinal cord injuries have been reported to be more favorable than those of adults.41 One quarter of our patients exhibited enduring neurological deficits. However, in the current study, final conclusions regarding recovery from spinal cord injury are not possible due to the lack of a standard neurological assessment method.
According to recent guidelines on acute cervical spine and spinal cord injuries, patients with spinal injury or suspected spinal injury should be transported to the hospital by experienced personnel in conditions of full spine immobilization.42 Important steps taken by emergency responders include careful patient assessment, spinal immobilization (cervical collar and rigid board), and appropriate airway management.43 These precautions should also be employed for very young children. Kim et al examined the use of spinal immobilization techniques in children of different age groups with and without traumatic cervical spinal injury in the US and found inconsistencies in the application of full spinal immobilization to children, particularly younger children, and this finding is similar to those of the current study.44
Outcomes
While spinal injuries are relatively uncommon in children, they can be associated with devastating outcomes.45 Ten of the patients (8.3%) in our sample died. In contrast to previous reports in which death was most frequently related to traffic accidents, 50% of deaths in the current series were related to pedestrian injuries. Although the direct causes of death in our series were not clearly defined, those who died exhibited higher impact injuries (as measured with the ISS), more severe head injuries (i.e., lower GCS scores) and more cervical injuries. In addition to the cervical involvement, mortality was also related to associated body and head injuries.8,46
Limitations
While the current study provides valuable insight into spine injuries in children and adolescents, population-based studies are required for proper injury prevention strategies. This study did not include patients with minor injuries who did not go to a hospital local primary care facility. Although this study was carried out in a large metropolitan area, the prevalences and outcomes of spinal cord injuries may be different in more rural areas of Saudi Arabia, and this issue should be assessed in future studies. Another limitation of this study is the lack of detailed neurological assessments after injury. Additionally, the data regarding the injury prevention methods that the patients could have used were incomplete.
The current study demonstrated the unique features of traumatic spine injury in children and adolescents. There was more cervical involvement in the younger age group and more thoracic involvement among the older patients. These findings raise significant concerns regarding spine trauma in children and adolescents. The majority of spine injuries were secondary to MVC. Appropriate traffic rules, child positioning in vehicles, and seatbelt use are important injury prevention strategies that should be utilized. Regarding pedestrian injuries, measures should be taken to address the safety of road crossing, especially during peak times. Additionally, appropriate care should be utilized during patient transfer to the hospital after injury.
REFERENCES
- 1.Galvin J, Scheinberg A, New PW. A retrospective case series of pediatric spinal cord injury and disease in Victoria, Australia. Spine. 2013;38(14):E878–82. doi: 10.1097/BRS.0b013e318294e839. [DOI] [PubMed] [Google Scholar]
- 2.Rozzelle CJ, Aarabi B, Dhall SS, Gelb DE, Hurlbert RJ, Ryken TC, et al. Spinal cord injury without radiographic abnormality (SCIWORA) Neurosurgery. 2013;72(Suppl 2):227–33. doi: 10.1227/NEU.0b013e3182770ebc. [DOI] [PubMed] [Google Scholar]
- 3.Augutis M, Levi R. Pediatric spinal cord injury in Sweden: incidence, etiology and outcome. Spinal cord. 2003;41(6):328–36. doi: 10.1038/sj.sc.3101478. [DOI] [PubMed] [Google Scholar]
- 4.Chien LC, Wu JC, Chen YC, Liu L, Huang WC, Chen TJ, et al. Age, sex, and socio-economic status affect the incidence of pediatric spinal cord injury: an eleven-year national cohort study. PloS one. 2012;7(6):e39264. doi: 10.1371/journal.pone.0039264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Puisto V, Kaariainen S, Impinen A, Parkkila T, Vartiainen E, Jalanko T, et al. Incidence of spinal and spinal cord injuries and their surgical treatment in children and adolescents: a population-based study. Spine. 2010;35(1):104–7. doi: 10.1097/BRS.0b013e3181c64423. [DOI] [PubMed] [Google Scholar]
- 6.Lee JH, Sung IY, Kang JY, Park SR. Characteristics of pediatric-onset spinal cord injury. Pediatrics international : official journal of the Japan Pediatric Society. 2009;51(2):254–7. doi: 10.1111/j.1442-200X.2008.02684.x. [DOI] [PubMed] [Google Scholar]
- 7.Klimo P, Jr, Ware ML, Gupta N, Brockmeyer D. Cervical spine trauma in the pediatric patient. Neurosurgery clinics of North America. 2007;18(4):599–620. doi: 10.1016/j.nec.2007.09.004. [DOI] [PubMed] [Google Scholar]
- 8.Cirak B, Ziegfeld S, Knight VM, Chang D, Avellino AM, Paidas CN. Spinal injuries in children. Journal of pediatric surgery. 2004;39(4):607–12. doi: 10.1016/j.jpedsurg.2003.12.011. [DOI] [PubMed] [Google Scholar]
- 9.McGrory BJ, Klassen RA, Chao EY, Staeheli JW, Weaver AL. Acute fractures and dislocations of the cervical spine in children and adolescents. The Journal of bone and joint surgery American volume. 1993;75(7):988–95. doi: 10.2106/00004623-199307000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Roche C, Carty H. Spinal trauma in children. Pediatric radiology. 2001;31(10):677–700. doi: 10.1007/s002470100532. [DOI] [PubMed] [Google Scholar]
- 11.Hamilton MG, Myles ST. Pediatric spinal injury: review of 61 deaths. Journal of neurosurgery. 1992;77(5):705–8. doi: 10.3171/jns.1992.77.5.0705. [DOI] [PubMed] [Google Scholar]
- 12.Hamilton MG, Myles ST. Pediatric spinal injury: review of 174 hospital admissions. Journal of neurosurgery. 1992;77(5):700–4. doi: 10.3171/jns.1992.77.5.0700. [DOI] [PubMed] [Google Scholar]
- 13.Alper G, Crumrine PK, Hamilton RL, Albright AL, Wald ER. Unusual case of inflammatory spinal epidural mass (Castleman syndrome) Pediatric neurology. 1996;15(1):60–2. doi: 10.1016/0887-8994(96)00090-2. [DOI] [PubMed] [Google Scholar]
- 14.Hood C, Kron T, Hamilton C, Callan S, Howlett S, Alvaro F, et al. Correlation of 3D-planned and measured dosimetry of photon and electron craniospinal radiation in a pediatric anthropomorphic phantom. Radiotherapy and oncology : journal of the European Society for Therapeutic Radiology and Oncology. 2005;77(1):111–6. doi: 10.1016/j.radonc.2005.06.035. [DOI] [PubMed] [Google Scholar]
- 15.Dietrich AM, Ginn-Pease ME, Bartkowski HM, King DR. Pediatric cervical spine fractures: predominantly subtle presentation. Journal of pediatric surgery. 1991;26(8):995–9. doi: 10.1016/0022-3468(91)90850-s. discussion 9–1000. [DOI] [PubMed] [Google Scholar]
- 16.Farley FA, Hensinger RN, Herzenberg JE. Cervical spinal cord injury in children. Journal of spinal disorders. 1992;5(4):410–6. doi: 10.1097/00002517-199212000-00005. [DOI] [PubMed] [Google Scholar]
- 17.Valerio G, Galle F, Mancusi C, Di Onofrio V, Colapietro M, Guida P, et al. Pattern of fractures across pediatric age groups: analysis of individual and lifestyle factors. BMC public health. 2010;10:656. doi: 10.1186/1471-2458-10-656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Abbas AK, Hefny AF, Abu-Zidan FM. Seat belts and road traffic collision injuries. World journal of emergency surgery : WJES. 2011;6(1):18. doi: 10.1186/1749-7922-6-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Platzer P, Jaindl M, Thalhammer G, Dittrich S, Kutscha-Lissberg F, Vecsei V, et al. Cervical spine injuries in pediatric patients. The Journal of trauma. 2007;62(2):389–96. doi: 10.1097/01.ta.0000221802.83549.46. discussion 94–6. [DOI] [PubMed] [Google Scholar]
- 20.Hofbauer M, Jaindl M, Hochtl LL, Ostermann RC, Kdolsky R, Aldrian S. Spine injuries in poly-traumatized pediatric patients: characteristics and experience from a Level I trauma center over two decades. The journal of trauma and acute care surgery. 2012;73(1):156–61. doi: 10.1097/TA.0b013e31824e32b5. [DOI] [PubMed] [Google Scholar]
- 21.Viccellio P, Simon H, Pressman BD, Shah MN, Mower WR, Hoffman JR, et al. A prospective multicenter study of cervical spine injury in children. Pediatrics. 2001;108(2):E20. doi: 10.1542/peds.108.2.e20. [DOI] [PubMed] [Google Scholar]
- 22.Basu S. Spinal injuries in children. Frontiers in neurology. 2012;3:96. doi: 10.3389/fneur.2012.00096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alhabdan S, Zamakhshary M, AlNaimi M, Mandora H, Alhamdan M, Al-Bedah K, et al. Epidemiology of traumatic head injury in children and adolescents in a major trauma center in Saudi Arabia: implications for injury prevention. Annals of Saudi medicine. 2013;33(1):52–6. doi: 10.5144/0256-4947.2013.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Crankson SJ. Motor vehicle injuries in childhood: a hospital-based study in Saudi Arabia. Pediatric surgery international. 2006;22(8):641–5. doi: 10.1007/s00383-006-1715-7. [DOI] [PubMed] [Google Scholar]
- 25.Ansari SA, Mandoorah M, Abdalrahim M, Al Moutaery KR. Dorsal spine injuries in Saudi Arabia--an unusual cause. Surgical neurology. 2001;56(3):181–4. doi: 10.1016/s0090-3019(01)00517-1. [DOI] [PubMed] [Google Scholar]
- 26.Ansari S, Ashraff Ali KS. Camel collision as a major cause of low cervical spinal cord injury. Spinal Cord. 1998;36:415–417. doi: 10.1038/sj.sc.3100530. [DOI] [PubMed] [Google Scholar]; Spinal cord. 1998;36(11):804. doi: 10.1038/sj.sc.3100748. [DOI] [PubMed] [Google Scholar]
- 27.all-Sebai MW, al-Zahrani S. Cervical spinal injuries caused by collision of cars with camels. Injury. 1997;28(3):191–4. doi: 10.1016/s0020-1383(96)00191-x. [DOI] [PubMed] [Google Scholar]
- 28.Central Department for Statistics and Information. Annual Statistical Books. 2007. [cited 2009 31 July]. Available from: http://www.cdsi.gov.sa/showsection.aspx?lid=26&id=318.
- 29.Baker SP, O’Neill B, Haddon W, Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. The Journal of trauma. 1974;14(3):187–96. [PubMed] [Google Scholar]
- 30.Copes WS, Champion HR, Sacco WJ, Lawnick MM, Keast SL, Bain LW. The Injury Severity Score revisited. The Journal of trauma. 1988;28(1):69–77. doi: 10.1097/00005373-198801000-00010. [DOI] [PubMed] [Google Scholar]
- 31.Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2(7872):81–4. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- 32.Krug EG, Sharma GK, Lozano R. The global burden of injuries. American journal of public health. 2000;90(4):523–6. doi: 10.2105/ajph.90.4.523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Anderson JM, Schutt AH. Spinal injury in children: a review of 156 cases seen from 1950 through 1978. Mayo Clinic proceedings Mayo Clinic. 1980;55(8):499–504. [PubMed] [Google Scholar]
- 34.Alshahri SS, Cripps RA, Lee BB, Al-Jadid MS. Traumatic spinal cord injury in Saudi Arabia: an epidemiological estimate from Riyadh. Spinal cord. 2012;50(12):882–4. doi: 10.1038/sc.2012.65. [DOI] [PubMed] [Google Scholar]
- 35.Suris JC, Nebot M, Parera N. Behaviour evaluation for risk-taking adolescents (BERTA): an easy to use and assess instrument to detect adolescent risky behaviours in a clinical setting. European journal of pediatrics. 2005;164(6):371–6. doi: 10.1007/s00431-005-1649-4. [DOI] [PubMed] [Google Scholar]
- 36.Rasouli MR, Rahimi-Movaghar V, Maheronnaghsh R, Yousefian A, Vaccaro AR. Preventing motor vehicle crashes related spine injuries in children. World journal of pediatrics : WJP. 2011;7(4):311–7. doi: 10.1007/s12519-011-0327-z. [DOI] [PubMed] [Google Scholar]
- 37.Leonard M, Sproule J, McCormack D. Paediatric spinal trauma and associated injuries. Injury. 2007;38(2):188–93. doi: 10.1016/j.injury.2006.09.019. [DOI] [PubMed] [Google Scholar]
- 38.Bilston LE, Brown J. Pediatric spinal injury type and severity are age and mechanism dependent. Spine. 2007;32(21):2339–47. doi: 10.1097/BRS.0b013e3181558886. [DOI] [PubMed] [Google Scholar]
- 39.Brown CV, Neville AL, Salim A, Rhee P, Cologne K, Demetriades D. The impact of obesity on severely injured children and adolescents. Journal of pediatric surgery. 2006;41(1):88–91. doi: 10.1016/j.jpedsurg.2005.10.012. discussion 88–91. [DOI] [PubMed] [Google Scholar]
- 40.Kokoska ER, Keller MS, Rallo MC, Weber TR. Characteristics of pediatric cervical spine injuries. Journal of pediatric surgery. 2001;36(1):100–5. doi: 10.1053/jpsu.2001.20022. [DOI] [PubMed] [Google Scholar]
- 41.Wang MY, Hoh DJ, Leary SP, Griffith P, Mc-Comb JG. High rates of neurological improvement following severe traumatic pediatric spinal cord injury. Spine. 2004;29(13):1493–7. doi: 10.1097/01.brs.0000129026.03194.0f. discussion E266. [DOI] [PubMed] [Google Scholar]
- 42.Theodore N, Hadley MN, Aarabi B, Dhall SS, Gelb DE, Hurlbert RJ, et al. Prehospital cervical spinal immobilization after trauma. Neurosurgery. 2013;72(Suppl 2):22–34. doi: 10.1227/NEU.0b013e318276edb1. [DOI] [PubMed] [Google Scholar]
- 43.Bernhard M, Gries A, Kremer P, Bottiger BW. Spinal cord injury (SCI)--prehospital management. Resuscitation. 2005;66(2):127–39. doi: 10.1016/j.resuscitation.2005.03.005. [DOI] [PubMed] [Google Scholar]
- 44.Kim EG, Brown KM, Leonard JC, Jaffe DM, Olsen CS, Kuppermann N, et al. Variability of prehospital spinal immobilization in children at risk for cervical spine injury. Pediatric emergency care. 2013;29(4):413–8. doi: 10.1097/PEC.0b013e318289d743. [DOI] [PubMed] [Google Scholar]
- 45.Turgut M, Akpinar G, Akalan N, Ozcan OE. Spinal injuries in the pediatric age group: a review of 82 cases of spinal cord and vertebral column injuries. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 1996;5(3):148–52. doi: 10.1007/BF00395505. [DOI] [PubMed] [Google Scholar]
- 46.Orenstein JB, Klein BL, Gotschall CS, Ochsenschlager DW, Klatzko MD, Eichelberger MR. Age and outcome in pediatric cervical spine injury: 11-year experience. Pediatric emergency care. 1994;10(3):132–7. doi: 10.1097/00006565-199406000-00003. [DOI] [PubMed] [Google Scholar]