Abstract
Environmental chemicals termed “obesogens” disrupt the endocrine system to promote adipogenesis and obesity. Tetrabromobisphenol-A (TBBPA) has been reported to increase adipogenesis; however, the mechanism(s) of action are unclear. Thy1 (CD90) is a glycophosphatidylinositol-anchored membrane protein that serves as a marker for stem cells and also plays an important role in regulating adipogenesis and obesity. We investigated whether or not TBBPA promotes adipogenesis in human and mouse cells by reducing Thy1 levels. We further sought to identify the molecular mechanism(s) whereby TBBPA targets Thy1 expression. Mouse and human cells were exposed to TBBPA, and Thy1 expression was analyzed using flow cytometry, Western blotting, and qPCR. We tested whether microRNAs predicted to target Thy1 (miR-103 and miR-107) were upregulated by TBBPA using quantitative PCR assays. We also determined if Thy1 mRNA was a bona fide miR-103/107 target. Our results show that Thy1 expression was reduced in both human and mouse cells after exposure to TBBPA. Both Thy1 mRNA and protein levels were decreased by low-dose TBBPA exposure. TBBPA reduced Thy1 levels and further increased adipogenesis when an adipogenic medium was used. Mechanistically, we show that miR-103 and miR-107 are induced by TBBPA and that miR-103 targets Thy1 to reduce its expression. Our results reveal for the first time that Thy1 is a target of TBBPA. Furthermore, our data support the concept that Thy1 is a key marker targeted by environmental chemicals that promote adipogenesis and obesity.
Keywords: Thy1 (CD90), Tetrabromobisphenol-A (TBBPA), endocrine disruptor, obesogen, adipogenesis, obesity, microRNA, mesenchymal stem cells
Obesity has risen dramatically over the last 30 years. In the U.S. alone, 60 million people are defined as clinically obese (Juonala et al., 2011). The main causes of the current obesity epidemic are thought to be a high-caloric intake, sedentary behavior, and lack of exercise. However, exposure to persistent chemicals in the environment may also be involved (Baillie-Hamilton, 2002). Obesogens are a class of endocrine disrupting chemicals that increase obesity and adipogenesis. Some obesogens are lipophilic, persistent organic pollutants that accumulate in human blood, milk, and adipose tissues. Obesogens can function in many ways including modulating adipocyte differentiation and size, lipid homeostasis, and/or regulation of appetite (Heindel et al., 2015; Janesick and Blumberg, 2016; La Merrill and Birnbaum, 2011). A large knowledge gap is the mechanism of action and molecular targets of obesogens. Tributyltin (TBT), an organotin used as a fungicide, bisphenol-A diglycidyl ether, a compound used in food container linings, and tetrabromobisphenol-A (TBBPA), the most widely used flame retardant in electronics and other materials, have been reported to increase adipogenesis and obesity (Chamorro-Garcia et al., 2012; Janesick and Blumberg, 2011; Riu et al., 2011a; Vafeiadi et al., 2015). In addition, TBBPA was shown to act as an obesogen in zebrafish, promoting lipid accumulation and weight gain in zebrafish exposed to the compound at several stages of development (Riu et al., 2014). TBBPA also adversely affects multiple pathways in neuronal cells in the low micromolar range, which is lower than reported human serum concentrations (Hendriks et al., 2012). The mechanism(s) by which these chemicals function to disrupt the endocrine system and increase obesity require active investigation.
Adipogenesis requires activation of the ligand-activated transcription factor, peroxisome proliferator activated receptor gamma (PPARγ) (Tontonoz and Spiegelman, 2008). PPARγ is the master regulator of adipogenesis, inducing expression of key adipogenic genes such as perilipin and fatty acid binding protein 4 (FABP4). Recently, TBT and TBBPA have been reported to increase adipogenesis by serving as PPARγ ligands (Janesick and Blumberg, 2011; Watt and Schlezinger, 2015).
Thy1, formally called CD90, is an N-glycosylated, glycophosphatidylinositol (GPI)-anchored membrane protein that was originally identified as a marker for mouse T cells. It also serves as a marker for identifying some types of stem cells, including mouse and human mesenchymal stem cells (MSCs) which are also sometimes called multipotent stromal cells (Nery et al., 2013). Our recent work supports a direct role for Thy1 function in controlling adipogenesis as we have shown that: depletion of Thy1 using Thy1 siRNA increases adipogenesis, introduction of Thy1 into an in vitro model of adipogenesis (mouse 3T3-L1 pre-adipocytes) dramatically reduces adipocyte formation and introduction of Thy1 reduces expression of a PPARγ-dependent reporter gene (Lehmann et al., 2010; Woeller et al., 2015a). These data support the concept that Thy1 is important for regulating PPARγ and adipogenesis. The mechanisms whereby Thy1 expression is regulated in MSCs are currently unknown.
MicroRNAs (miRNAs) are endogenous, small RNAs that regulate genes by suppressing target mRNA translation or increasing target mRNA degradation (Bartel, 2009). Recent work links expression of certain miRNAs with adipogenesis and obesity (Alexander et al., 2011; Deiuliis, 2016; Heneghan et al., 2010; Xie et al., 2009). The miR-103/107 family of miRNA has been shown to be dysregulated in obesity and type 2 diabetes (Perri et al., 2012; Trajkovski et al., 2011). Furthermore, miR-103 can regulate insulin sensitivity (Vatandoost et al., 2015; Vienberg et al., 2016). Herein, we investigated whether or not TBBPA promotes adipogenesis in human and mouse cells by targeting Thy1. We further sought to uncover the mechanism(s) whereby TBBPA targets Thy1 expression. Specifically, we hypothesized that miRNAs predicted to target Thy1 are involved in TBBPA mediated Thy1 suppression.
MATERIALS AND METHODS
Chemicals
3,3′,5,5′-TBBPA, 3-isobutyl-1-methylxanthine (IBMX), dexamethasone, and human recombinant insulin were purchased from Sigma-Aldrich (St. Louis, Missouri). Rosiglitazone was purchased from Cayman Chemical (Ann Arbor, Michigan).
Cell culture
3T3-L1 (ATCC CL-173) pre-adipocytes and C3H10T1/2 (ATCC CCL-226) multipotent cells were obtained from the American Type Culture Collection (Rockville, Maryland). Human adipose-derived primary MSCs were purchased from Millipore (Billerica, Massachusetts), Invitrogen (Carlsbad, California), or Thermo Fisher (Waltham, Massachusetts). Alternatively, human adipose-derived cells were isolated from fat tissue as described below. All media and supplements were purchased from Gibco (Carlsbad, California). MSCs were cultured and maintained in MesenPro RS medium while 3T3-L1 and C3H10T1/2 cells were maintained in 10% calf serum supplemented DMEM. All cells were incubated at 37°C with 7% humidified CO2. Adipogenesis was induced in all 3T3-L1 pre-adipocytes using adipogenic medium that contained 0.5 mM IBMX, 0.5 μM dexamethasone, and 2 μg/ml insulin in 10% FBS supplemented DMEM for 2 days. After 2 days, fresh adipogenic medium lacking IBMX was added. Medium was replaced every 3 days until the experiment was finished. Differentiation of C3H10 T1/2 cells and MSCs was done with the same adipogenic medium except 3% FBS supplemented DMEM was used (instead of 10%). Adipogenesis was induced only after cultures became confluent. TBBPA (1–10 μM) or the potent PPARγ ligand, rosiglitazone (2 μM) were added to the adipogenic medium as described. Cells were analyzed for lipid accumulation and adipogenesis as previously described (Woeller et al., 2015a). In brief, for immunofluorescent staining, cells were stained with LipidToxRed and the nucleic acid stain DAPI (Thermo Fisher) and visualized on an EVOS-FL Cell Imaging System (Thermo Fisher). Quantification of lipid levels was performed using the fluorescent AdipoRed assay and fluorescence was measured on a Varioskan plate reader (Thermo Fisher).
Isolation of human multipotent stromal cells from adipose tissue
Abdominal fat surgical waste was obtained with IRB approval from the Department of Pathology and Laboratory Medicine after unique patient identifiers were removed. All fat tissue was washed in ice cold PBS and cut into 2–3 mm pieces and then placed in DMEM containing 280 units/ml collagenase. The collagenase mixture was incubated at 37°C for 1.5 h with gentle agitation. Fractions were separated by centrifugation at 1000 × g for 5 min. MSCs were collected from the pellet, plated, and allowed to attach to culture dishes and passaged two times before being characterized by flow cytometry for CD90, CD105, and CD73 and CD45 negative as described (Bernacki et al., 2008; Nery et al., 2013).
Animal studies
C57BL/6 mice were housed in colony cages with a 12-h light/12-h dark cycle and fed ad libitum. During the study, 8-week-old male mice were injected intraperitoneally (three times per week) with Vehicle (corn oil) or TBBPA (either 1 or 100 mg/kg) for 5 weeks (n = 3 animals per group). After 5 weeks, mice were euthanized and the perigonadal visceral adipose tissue was collected and digested with collagenase as described previously (Woeller et al., 2015a). The stromal cell fraction was analyzed by flow cytometry for Thy1 expression. All animal experiments were performed with approval of the University Committee on Animal Resources at the University of Rochester School of Medicine and Dentistry.
Introduction of miRNA into MSCs
Cells were seeded at 5–8×104 or 1×105 cells/cm2 into 24-well or 6-well cell culture plates (Corning, Corning, New York), respectively, and subsequently transiently transfected with 50–200 nM of either a nonspecific control miRNA mimic or a mature miR-103 mimic (Ambion) using Lipofectamine 2000 (Invitrogen, Carlsbad, California) following the manufacture’s protocol. Cells were incubated with miRNA for 1–4 days before being subjected to analysis by Western blotting, flow cytometry and/or qPCR.
Transient transfection by electroporation
2 × 106 cells were collected and resuspended in 100 μl of Ingenio electroporation solution (Mirus Bio, Madison, Wisconsin) containing appropriate DNA-miRNA antagomir complexes and electroporated with program U-023 on an Amaxa Nucleofector instrument (Lonza, Cologne, Germany) following the instructions from the manufacturer.
Quantitative real-time PCR (qPCR) detection of mRNA and miRNA levels
Total cell RNA was extracted using the miRNeasy Kit (Qiagen, Valencia, California) according to the manufacturers’ instructions. Purified RNA concentrations were measured with a NanoDrop 1000 spectrophotometer (Thermo Scientific, Wilmington, Delaware). 50–150 ng of total RNA was used to generate cDNA using an iScript reverse transcription kit (Bio-Rad). Gene expression was quantified via real-time PCR with gene specific primers, a universal SsoFast Evergreen PCR master mix (Bio-Rad) using a CFX Connect Real Time PCR Detection System (Bio-Rad). To analyze relative gene expression we used the comparative ΔΔCt method as described by Schmittgen and Livak (2008). Forward and reverse gene-specific primers are as follows: human THY1: ATCTCCTCCCAGAACGTC and ATCTCTGCACTGGAACTTG; human 18S rRNA: TGAGAAACGGCTACCACATC and ACTACGAGCTTTTTAACTGC; human GAPDH mRNA: ATG GAA ATC CCA TCA CCA TCT T and CGG CCC ACT TGA TTT TGG; mouse Thy1: CCTTACCCTAGCCAACTTCAC and AGGATGTGTTCTGAACCAGC; mouse fabp4: ATGTGTGATGCCTTTGTGGGAAC and TCATGTTGGGCTTGGCCATG; mouse Gapdh: AGCCTCGTCCCGTAGACAAA and CCTTGACTGTGCCGTTGAAT; mouse 18S rRNA: GTAACCCGTTGAACCCCATT and CCATCCAATCGGTAGTAGCG. To analyze changes in Thy1 mRNA levels, we normalized Thy1 levels to both 18S rRNA and GAPDH mRNA levels. MiRNA cDNA was generated from 10 to 100 ng of total RNA using TaqMan microRNA reverse transcription kit (Applied Biosystems) and miRNA qPCR was performed using TaqMan Universal PCR master mix (Applied Biosystems). TaqMan based miRNA primers which recognize both human and mouse miRNA were purchased from Applied Biosystems (miR-103: 4427975 “000439”, miR-107: 4427975 “000443”, and U6: 4395470 “001973”).
Western blot analysis
Protein was isolated from 1 to 2 × 106 cells and lysed in 60 mM Tris, pH 6.8, 2% SDS containing 1× protease inhibitor cocktail (Sigma-Aldrich). Total protein (1–10 μg per lane) was subjected to SDS-PAGE. Protein gels were transferred to 0.45 μm Immobilon-PVDF membrane (Millipore, Temecula, California) and blocked with 5% non-fat dry milk in 0.1% Tween 20 in 1× PBS. Antibodies targeting: Thy1 (rabbit anti-Thy1, cat #9798, Cell Signaling Technology, Danvers, Massachusetts), FABP4 (rabbit anti-FABP4, cat #HP9028, Hycult Biotech, Plymouth Meeting, Pennsylvania), perilipin (rabbit anti-perilipin, cat #9349, Cell Signaling Technology), and β-tubulin (rabbit anti-β-tubulin, cat. # 2146, Cell Signaling Technology), were diluted according to the manufacturers’ instructions. Anti-mouse or anti-rabbit HRP-conjugated secondary antibodies were purchased from Jackson ImmunoResearch Laboratories (West Grove, Pennsylvania). Protein was visualized using Immobilon Western chemiluminescent horseradish peroxidase substrate (Millipore). Chemiluminescent signals were captured using X-ray film (Laboratory Product Sales, Rochester, New York). Film was scanned and densitometry analysis was performed with Image Studio Lite, version 5.2 (Li-Cor Inc., Lincoln, Nebraska).
Flow cytometry
Cells were cultured with TBBPA, rosiglitazone or the pro-adipogenic medium for the indicated times and then collected by trypsinization and washed in 1× PBS before blocking non-specific binding for 30 min with 5% human Fc receptor blocker (Miltenyi Biotech Inc., San Diego, California) in PBS containing 1% bovine serum albumin. The blocked cells were then incubated with anti-mouse Thy1.2-PE conjugated antibody (BD Biosciences, San Jose, California) or anti-human Thy1-PE conjugated antibody (BD Biosciences) for 1–2 h at 4°C. Cells were analyzed on a FACS Canto II flow cytometer running FACSDIVA software (BD Biosciences) using a 488-nm excitation laser and a 585/42-nm band pass detector filter. Subsequent analysis of fluorescence emission data was performed using FlowJo software v10.1 (FlowJo, LLC, Ashland, Oregon).
Generation of constitutively human Thy1 3′UTR reporter construct
The human Thy1 3′UTR was amplified from human MSC (hMSC) cDNA by PCR using KOD polymerase (Novagen, Madison, Wisconsin) using the following primers: THY1 3′UTR fwd: TACTCGAGTGACTGG-TGGGGCCCATGGAGG; THY1 3′UTR rev: TAGCGGCCGCTGGGCAAATGTGTCTCG-TTAGGG, where the underlined nucleotides indicate restriction sites for XhoI and NotI. The 3′UTR sequence was verified by DNA sequencing and then inserted into the psiCheck2 vector (Promega, Madison, Wisconsin) downstream of the Renilla luciferase gene.
Luciferase reporter assays
Luciferase reporter assays were performed as described previously (Woeller et al., 2015b). In brief, the reporter plasmids psiCheck2 empty or psiCheck2-Thy1 3′-UTR along with miRNA mimics (10 nM) or antagomirs (10 nM) (Ambion) were introduced into cells by electroporation as described above. Cells were treated with DMSO (vehicle) or TBBPA at the doses indicated for 24 h. Luciferase activity was then measured using Dual-Glo Luciferase Assay buffer (Promega) read on a Varioskan Flash luminescent plate reader (Thermo Fisher). Luciferase readings were normalized to the control, vehicle-treated samples for statistical analysis.
Statistical analysis
Statistical analyses were performed using Prism (Graphpad). All values are presented as mean ± SD unless otherwise noted. Student’s t test and one-way analysis of variance (ANOVA) with Tukey’s post-test were used for statistical analysis and P values of P < .05, P < .01, P < .001, were considered significant.
RESULTS
TBBPA Exposure Decreases Thy1 Expression and Promotes Adipogenesis
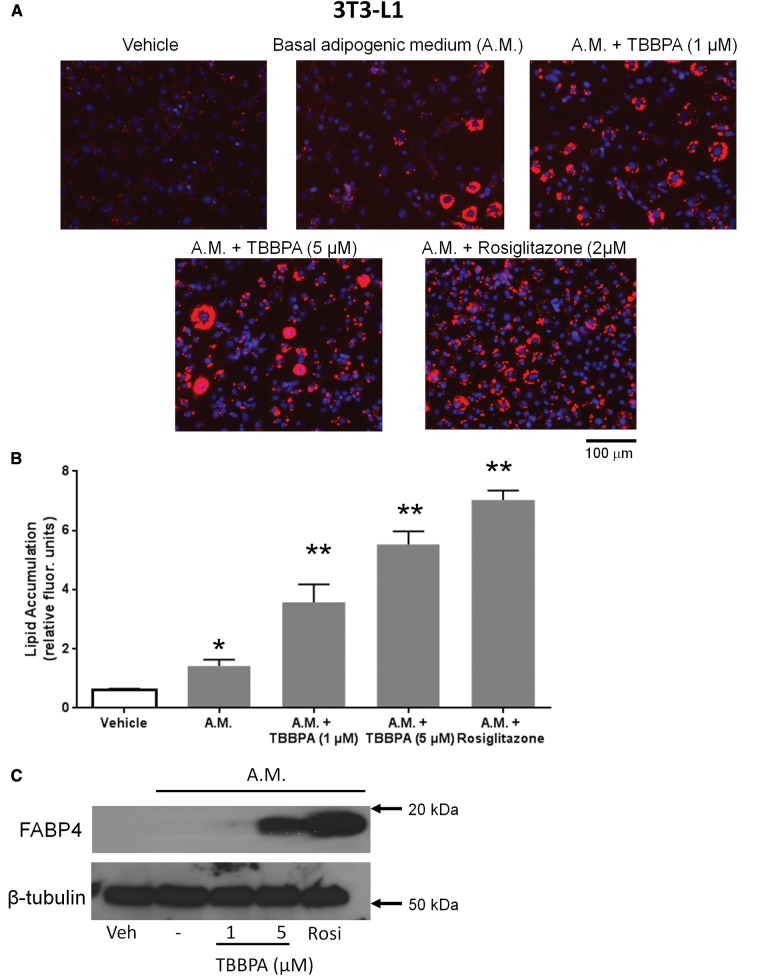
TBBPA is the most widely used brominated flame retardant in the world and can be absorbed through the skin, inhaled, or ingested (Di Napoli-Davis and Owens, 2013; Knudsen et al., 2015; Zhou et al., 2014). TBBPA and TBBPA derivatives are commonly detected in human serum, milk, and adipose tissue (up to 37 ng/g lipid weight) and can bioaccumulate therein (Cariou et al., 2008; Honkisz and Wojtowicz, 2015; Johnson-Restrepo et al., 2008). MSCs or mulitipotent stromal cells present in the microenvironment of fat tissue are therefore continually exposed to environmental TBBPA. TBBPA concentrations present in human serum can reach the low micromolar range and these concentrations also promote lipid accumulation in zebrafish (Hendriks et al., 2012; Riu et al., 2014). Our first goal was to test the hypothesis that TBBPA can promote lipid accumulation and adipogenesis in mouse and human cells. The first model we chose was the 3T3-L1 pre-adipocyte cell line that is the most well-studied model of adipogenesis and can rapidly form adipocytes in an 8-day treatment of adipogenic medium (Green and Kehinde, 1975). Because we wanted to study if TBBPA could enhance adipogenesis, we used a shorter time frame for our analyses to better observe differences in lipid accumulation. We exposed 3T3-L1 cells to adipogenic medium alone or with 1 or 5 µM TBBPA for 5 days. As an additional control, we treated cells with the adipogenic medium plus the potent PPARγ ligand, rosiglitazone. After 5 days, cells were analyzed for lipid accumulation and adipogenesis by three different methods (Figure 1). First, some wells were fixed and stained with the lipid binding dye, LipidToxRed and nucleic acid binding dye, DAPI, and then visualized by fluorescent microscopy (Figure 1A). While the adipogenic medium alone does lead to lipid accumulation in some of the cells, there is a clear increase in the number of cells staining with LipidTox when cells are exposed to TBBPA. Rosiglitzone treatment led to the greatest increase in LipidTox positive cells. To better quantify lipid accumulation, some cells were used to measure lipid accumulation with the quantitative AdipoRed assay (Figure 1B). The AdipoRed assay shows that the adipogenic medium does increase lipid accumulation, however, TBBPA leads to a large increase in lipid accumulation, where 1 µM TBBPA increases lipid accumulation by 2-fold and 5 µM TBBPA increases lipid by 3-fold compared with adipogenic medium alone. Rosiglitazone again leads to the largest increase in lipid accumulation (∼6-fold over adipogenic medium alone). As a final test, some cells were used in Western blot analyses for FABP4 expression (Figure 1C). Both 5 µM TBBPA and rosiglitazone lead to a dramatic induction of FABP4 expression at treatment day 5.
FIG. 1.
TBBPA promotes adipogenesis in 3T3-L1 pre-adipocytes. Adipogenesis was induced in confluent 3T3-L1 pre adipocytes using adipogenic medium that contained 0.5 mM IBMX, 0.5 μM dexamethasone, and 2 μg/ml insulin in 10% FBS supplemented DMEM for 2 days. After 2 days, fresh adipogenic medium lacking IBMX was added for 3 days. In addition to adipogenic medium, some cells received 1 or 5 µM TBBPA or 2 µM rosiglitazone for the entire 5-day experiment. (A) Representative LipidToxRed staining of cells treated with vehicle, TBBPA, or rosiglitazone is shown. (B) Lipid accumulation of 3T3-L1 cells was quantified using the fluorescent AdipoRed assay. The results shown are a result of three different experiments with three replicate wells measured for each experiment. The data were analyzed by a one-way ANOVA with Tukey’s post-test for significance (**P < 0.01). (C) Western blot analysis of FABP4 expression in 3T3-L1 cells treated as above. β-tubulin serves as a loading control. This Western blot is a representative blot from three different experiments that were performed.
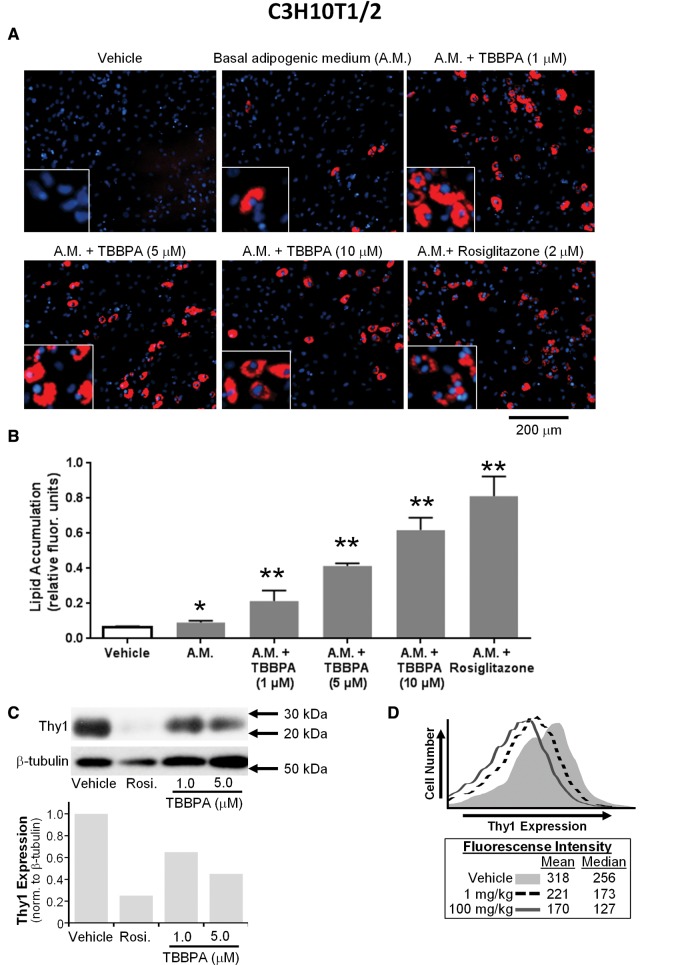
We also used multipotent mesenchymal C3H10T1/2 cells to test the ability of TBBPA to promote adipogenesis. C3H10T1/2 cells have the ability to form adipocytes, osteoblasts, or chondrocytes if given the appropriate stimuli (Hisada et al., 2013). Here, confluent C3H10T1/2 cells were treated with a basal adipogenic medium and either vehicle (DMSO), TBBPA (at 1, 5, or 10 μM) or rosiglitazone (2 μM) as described in Materials and Methods section for 8 days. After treatment, some cells were fixed and stained with LipidToxRed and counterstained with DAPI and then visualized by fluorescent microscopy (Figure 2A). Lipid accumulation was also quantified using the AdipoRed assay (Figure 2B). The basal adipogenic medium resulted in minor lipid accumulation. However, TBBPA significantly induced formation of large lipid droplets that stained with LipidToxRed. Rosiglitazone treatment also dramatically increased lipid accumulation in C3H10T1/2 cells. Since we have previously shown that Thy1 expression can prevent lipid accumulation and that Thy1 expression is normally lost during adipogenesis (Woeller et al., 2015a), we determined if Thy1 expression was altered by rosiglitazone or TBBPA treatment even without progression through adipogenesis. To test this, C3H10T1/2 cells were cultured with vehicle, rosiglitazone, or TBBPA (1 or 5 μM) for 4 days without adipogenic medium and Thy1 expression was analyzed by Western blot (Figure 2C). Both rosiglitazone and TBBPA exposure decreased Thy1 expression. While Thy1 expression is decreased by TBBPA in vitro, we also tested if TBBPA could act on Thy1 in vivo. To do this, we performed an experiment in which we gave mice vehicle (corn oil), 1or 100 mg/kg TBBPA intraperitoneally three times per week for a total of 5 weeks. At the end of the experiment, visceral adipose tissue was isolated and digested with collagenase as described in Materials and Methods section. We analyzed surface expression of Thy1 in the stromal fraction of cells using flow cytometry (Figure 2D). Interestingly, Thy1 expression was reduced by TBBPA treatment in vivo.
FIG. 2.
TBBPA promotes adipogenesis and reduces Thy1 expression. (A) C3H10T1/2 cells were plated and allowed to reach confluence before being treated with vehicle or adipogenic medium that contained 0.5 mM IBMX, 0.5 μM dexamethasone, and 2 μg/ml insulin in 3% FBS supplemented DMEM for 2 days. After 2 days, fresh adipogenic medium lacking IBMX was added every 3 days. In addition to adipogenic medium, some cells received 1, 5, or 10 µM TBBPA or 2 µM rosiglitazone for the entire 8-day experiment. Representative LipidToxRed staining is shown. (B) Lipid accumulation in C3H10T1/2 cells was quantified using the fluorescent AdipoRed assay. The results shown are a result of three different experiments with three replicate wells measured for each experiment. The data were analyzed by a one-way ANOVA with Tukey’s post-test for significance (*P < .05 and **P < .01). (C) Western blot analysis of Thy1 expression in C3H10 T1/2 cells treated with rosiglitazone or TBBPA (1 or 5 μM) for 4 days without adipogenic medium. β-tubulin serves as a loading control. Densitometry analysis of the representative Western blot is shown below the blot. (D) Male C57Bl/6 mice were injected intraperitoneally (three times per week) with Vehicle (corn oil) or TBBPA (either 1 or 100 mg/kg) for 5 weeks, then visceral adipose tissue was harvested and dissociated with collagenase as described in Material and Methods section to liberate stromal cells. Cells were stained with an anti-Thy1 antibody and stromal cells were gated on and analyzed for Thy1 expression. Thy1 expression was decreased by TBBPA. (n = 3 animals/group, representative animals shown).
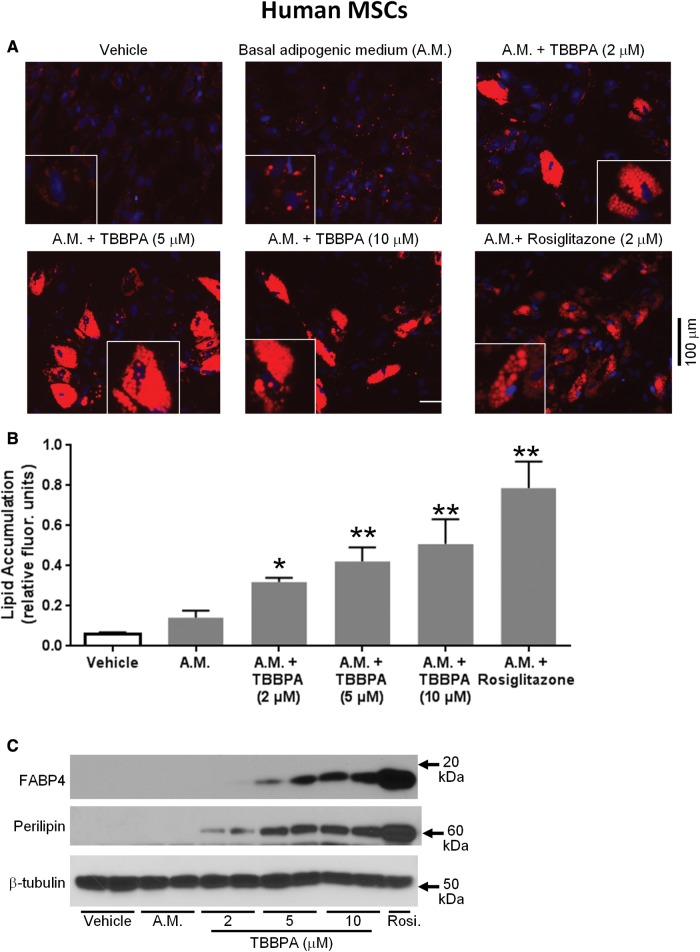
Since TBBPA exposure promoted adipogenesis and reduced Thy1 expression in mouse cells in vitro and in vivo, we tested the ability of TBBPA to function in human MSCs. MSCs are variably called multipotent stromal cells but all of these cells have the potential to form adipocytes, chondrocytes, or osetocytes when provoked with the appropriate stimuli (Biemann et al., 2014; Yamamoto et al., 2007). Here, human MSCs were treated with or without a basal adipogenic medium containing insulin and dexamethasone. Cells were additionally exposed to vehicle (DMSO), TBBPA (2, 5, or 10 μM), or rosiglitazone. After incubation for 12 days, hMSCs were analyzed for lipid accumulation and adipocyte differentiation using LipidToxRed (Figure 3A), the AdipoRed assay (Figure 3B) and expression of the adipocyte markers, perilipin, and FABP4 (Figure 3C). While the basal adipogenic medium induced some lipid accumulation, TBBPA significantly enhanced adipogenesis, lipid accumulation, perilipin, and FABP4 expression in hMSCs. Likewise, rosiglitazone significantly induced adipogenesis of hMSCs as shown by lipid droplet accumulation, perilipin expression, and FABP4 expression (Figure 3).
FIG. 3.
TBBPA promotes adipogenesis in human mesenchymal stem cells (hMSCs). Adipogenesis was induced in confluent MSCs using adipogenic medium that contained 0.5 mM IBMX, 0.5 μM dexamethasone, and 2 μg/ml insulin in 3% FBS supplemented DMEM for 2 days. After 2 days, fresh adipogenic medium lacking IBMX was added for ten additional days with medium changes every 3 days. In addition to adipogenic medium, some cells received 2, 5, or 10 µM TBBPA or 2 µM rosiglitazone for the entire experiment. (A) Representative LipidToxRed staining is shown. (B) Lipid accumulation in hMSCs was quantified using the fluorescent AdipoRed assay. The results shown are a result of three different experiments with three replicate wells measured for each experiment. The data were analyzed by a one-way ANOVA with Tukey’s post-test for significance (*P < .05 and **P < .01). (C) Western blot analysis of FABP4 and perilipin expression in hMSCs treated as above. β-tubulin serves as a loading control. The blot shown is representative of three different experiments performed.
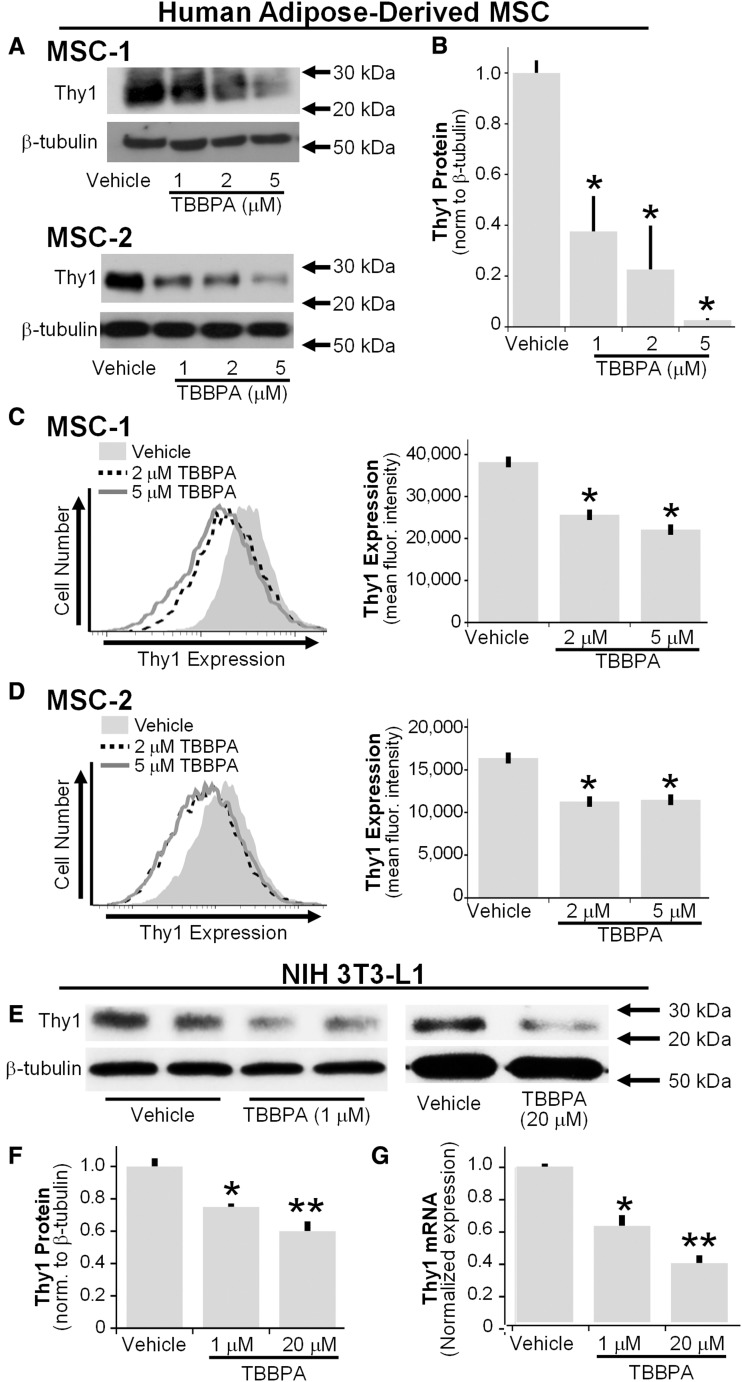
To test if TBBPA targets Thy1 in hMSCs, cells were cultured in 0.05% FBS supplemented DMEM in the presence of vehicle or TBBPA (1, 2, or 5 μM) for 7 days. Thy1 protein levels were analyzed by Western blot (Figs. 4A and B) and surface Thy1 levels were analyzed by flow cytometry (Figs. 4C and D). Both total Thy1 and surface Thy1 levels were dose-dependently decreased by TBBPA in hMSCs (representative strains MSC-1 and MSC-2 are shown).
FIG. 4.
Thy1 levels are reduced by TBBPA. (A) hMSCs were cultured in 0.05% FBS supplemented DMEM in the presence of vehicle or TBBPA (1, 2, or 5 μM) for 7 days. Thy1 protein levels were analyzed by Western blot (tubulin serves as a loading control). (B) Densitometry analysis of Western blots run with MSCs treated with TBBPA. The results shown are a result of three different experiments with three replicate wells measured for each experiment. The data were analyzed by a one-way ANOVA with Tukey’s post-test for significance (*P < .05 and **P < .01). (C, D) Surface Thy1 levels of hMSCs treated as in (A) were analyzed by flow cytometry (representative strains MSC-1 and MSC-2 are shown). The right hand panels show mean fluorescent intensity of Thy1 surface staining. (E) Western blot analysis of Thy1 expression in 3T3-L1 cells treated with vehicle or TBBPA (1 or 20 μM) for 4 days. Tubulin serves as a loading control. (F) Densitometry analysis of Western blots is shown. (G) The mRNA level of Thy1 was quantified (and normalized to 18S rRNA and gapdh mRNA) by qPCR. The data were analyzed by a one-way ANOVA with Tukey’s post-test for significance (*P < .05 and **P < .01).
We further evaluated the effects of TBBPA on 3T3-L1 cells without an adipogenic medium. Here, we treated subconfluent 3T3-L1 cells with TBBPA (1–20 μM) for 4 days without addition of other pro-adipogenic stimuli (Figure 4E). TBBPA exposure decreased Thy1 protein levels in 3T3-L1 cells (Figure 4F). TBBPA also decreased Thy1 mRNA (Figure 4G) and protein levels in a dose-dependent manner, where 1 μM TBBPA decreased Thy1 protein and mRNA by 20% and 20 μM TBBPA decreased Thy1 protein and mRNA by 50% in 3T3-L1 cells (Figs. 4E–G).
Pre-Exposure to TBBPA Increases Adipogenesis
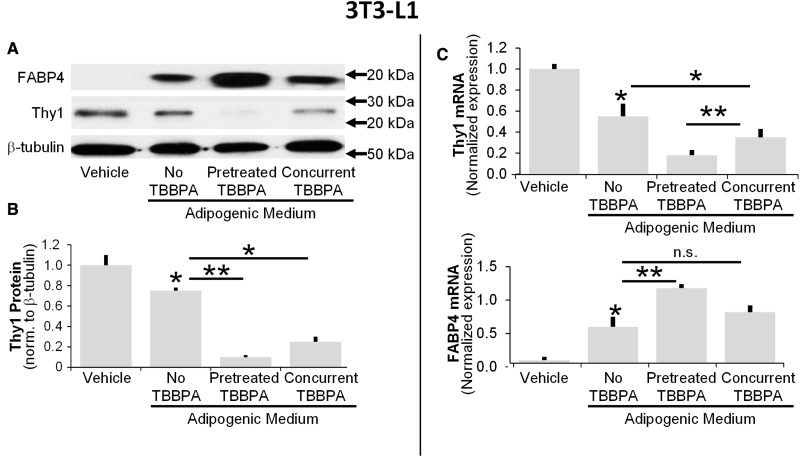
Since we observed that TBBPA could decrease Thy1 expression in hMSCs, multipotent mesenchymal cells, and 3T3-L1 cells, we tested if pre-exposure to TBBPA could further enhance adipogenesis. Here, we exposed subconfluent 3T3-L1 cells to TBBPA (5 μM) for 4 days prior to initiation of adipogenesis with the standard pro-adipogenic medium (Figure 5). After 4 days, the cells became confluent and were then cultured in adipogenic medium for another 4 days before harvest. Cells were collected and analyzed for expression of Thy1 and FABP4 by Western blot and qPCR. Adipogenic medium alone induced expression of FABP4, however, pre-treatment with TBBPA significantly enhanced expression of FABP4 (Figs. 5A and C). Concomitant treatment with TBBPA also increased FABP4 expression, though not to the same degree as TBBPA pre-treatment. Thy1 mRNA was significantly decreased by 4 days of adipogenic medium treatment, but both co-treatment and pre-treatment with TBBPA further decreased Thy1 protein and mRNA (Figs. 5B and C). These results further support that loss of Thy1 is an early step in adipogenic commitment and that TBBPA can target Thy1 to promote adipogenesis.
FIG. 5.
Pretreatment with TBBPA enhances adipogenesis and results in a further reduction of Thy1. Subconfluent cultures of 3T3-L1 cells were treated with vehicle or 5-μM TBBPA for 4 days prior to induction of adipogenesis. After 4 days, the cultures became confluent and adipogenesis was induced using adipogenic medium that contained 0.5 mM IBMX, 0.5 μM dexamethasone, and 2 μg/ml insulin in 10% FBS supplemented DMEM for 2 days. After 2 days, fresh adipogenic medium lacking IBMX was added for 2 days. Some of the cells were treated with 5 μM TBBPA during the adipogenic treatment. After the 8-day experiment, cells were collected and analyzed. (A) Western blot analysis of Thy1, FABP4, and β-Tubulin (loading control). (B) Densitometry analysis of Thy1 protein levels. (C) The mRNA levels of the adipogenic marker FABP4 and Thy1 were quantified (and normalized to 18S rRNA and gapdh mRNA) by qPCR. The data were analyzed by a one-way ANOVA with Tukey’s post-test for significance (*P < .05 and **P < .01).
Thy1 Expression Is Regulated by miR-103
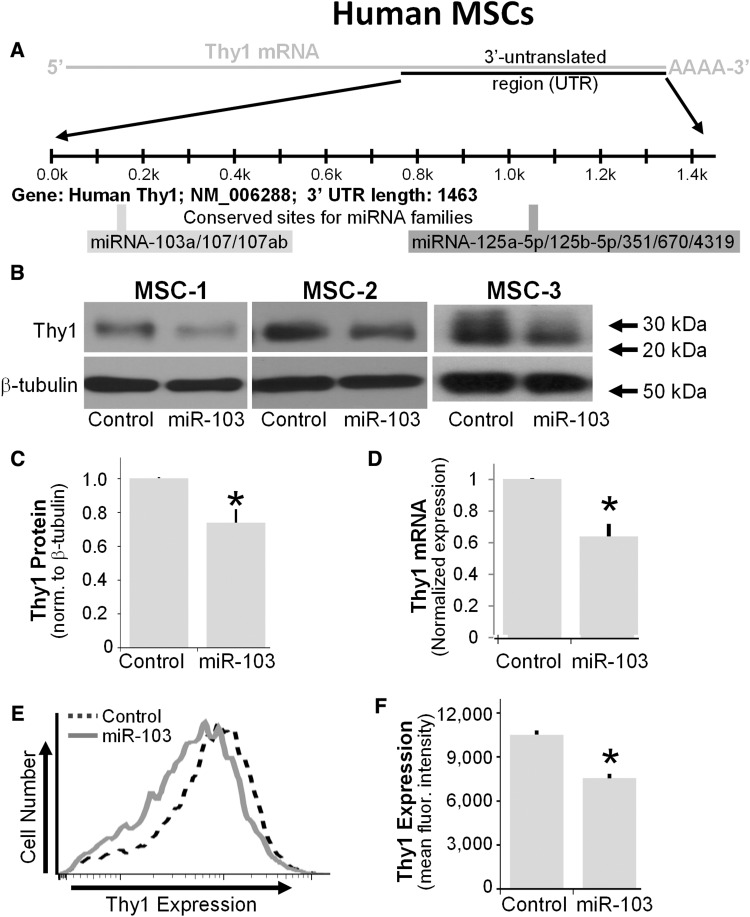
While Thy1 is highly expressed in hMSCs, almost nothing is known about how Thy1 expression is controlled. One potential mechanism whereby TBBPA could target Thy1 expression is through upregulation of key miRNA that target Thy1. Using TargetScan software (Agarwal et al., 2015), we discovered that the Thy1 mRNA is a predicted target of multiple miRNAs, including the miR-103/107 family (Figure 6A). The consensus seed sequence for the miR-103/107 family is conserved between human and mouse Thy1 mRNA. We tested whether miR-103 blocks Thy1 expression in hMSCs. To accomplish this, a non-specific control miRNA mimic, or a miR-103 mimic were introduced into hMSCs. After 3 days of treatment, Thy1 protein levels (Figs. 6B and C), Thy1 mRNA levels (Figure 6D) and Thy1 surface levels were analyzed (Figs. 6E and F). Interestingly, in all three hMSCs strains tested, Thy1 protein, and mRNA levels were significantly reduced by exogenous miR-103 expression.
FIG. 6.
Thy1 is a target of miR-103 in human MSCs. (A) Depiction of human Thy1 mRNA showing a conserved seven nucleotide consensus binding site for the miR-103/107 miRNA family. (B) Control miRNA mimic or miR-103 mimic were introduced into hMSCs and after 3 days or treatment, Thy1 levels were analyzed by Western blot (tubulin serves as a loading control). (C) Densitometry analyses of results in (B). (D) Thy1 mRNA levels from experiment described in (B) were analyzed (and normalized to 18S rRNA) by qPCR. The data were analyzed by Student’s t test (*P < .05). Results are an average of experiments performed in five different MSC cell lines with representative blots shown. (E) Flow cytometry of Thy1 levels from MSCs treated with control or miR-103 mimics. (F) Mean fluorescent intensity of Thy1 levels from E shows a reduction in Thy1 surface levels (*P < .05).
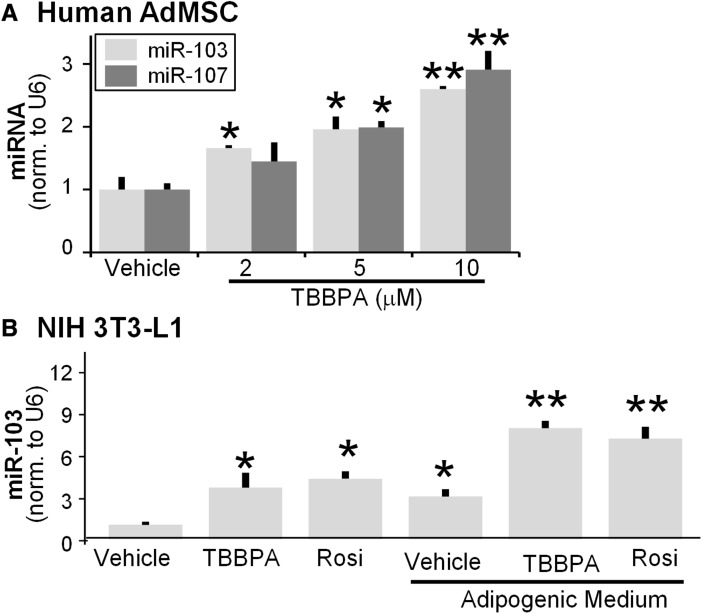
TBBPA Increases Expression of miR-103 and miR-107 in Human MSCs and 3T3-L1 Cells
Since Thy1 is potentially a target of miR-103/107, we tested whether or not TBBPA could alter miRNA expression in human and mouse cells. We treated hMSCs with vehicle or TBBPA (2, 5, or 10 μM) for 4 days before collecting cells for miRNA expression analyses using TaqMan miRNA qPCR assays. Interestingly, expression of miR-103 and miR-107 were increased by TBBPA exposure. After a 4-day exposure to 10-μM TBBPA, both miR-103 and miR-107 were increased ∼3-fold in hMSCs (Figure 7A).
FIG. 7.
TBBPA induces expression of miR-103 in mouse and human cells. (A) Human adipose-derived MSCs were treated with vehicle (DMSO) or 5 μM TBBPA for 4 days and small RNA was isolated. MiR-103 and miR-107 were detected by qPCR. MiRNA levels were normalized to U6 snRNA. MiR-103 was detected by qPCR. MiR-103/107 levels were normalized to U6 snRNA. (B) 3T3-L1 pre-adipocytes were treated with TBBPA (5 μM) or rosiglitazone (2 μM) with or without adipogenic medium. After 4 days of treatment, miRNA was isolated and miR-103 expression was analyzed using TaqMan qPCR assays. The results shown are a result of three different experiments with three replicate wells measured for each experiment. The data were analyzed by a one-way ANOVA with Tukey’s post-test for significance (*P < .05 and **P < .01).
The expression of miR-103 has been shown to be induced during adipogenesis of 3T3-L1 cells and this upregulation has been shown to be PPARγ dependent (John et al., 2012; Li et al., 2015). Here, we treated 3T3-L1 cells with TBBPA (5 μM) or rosiglitazone (2 μM) with or without adipogenic medium. After 4 days of treatment, miRNA was isolated and miR-103 expression was analyzed using TaqMan qPCR assays. TBBPA treatment alone increased expression of miR-103 by 4-fold in 3T3-L1 cells (Figure 7B). Likewise, rosiglitazone also induced miR-103 expression more than 4-fold suggesting again that the increase in miR-103 is PPARγ activation dependent. Addition of adipogenic medium containing dexamethasone and insulin also increased miR-103 expression over vehicle treated cells by ∼3-fold. Concomitant treatment with either TBBPA or rosiglitazone resulted in a 7-fold increase in miR-103 levels (Figure 7B). These results show that miR-103 and miR-107 are significantly elevated by TBBPA treatment in hMSCs and miR-103 is elevated by TBBPA, rosiglitazone and adipogenic medium in 3T3-L1 cells suggesting a PPARγ-dependent mechanism.
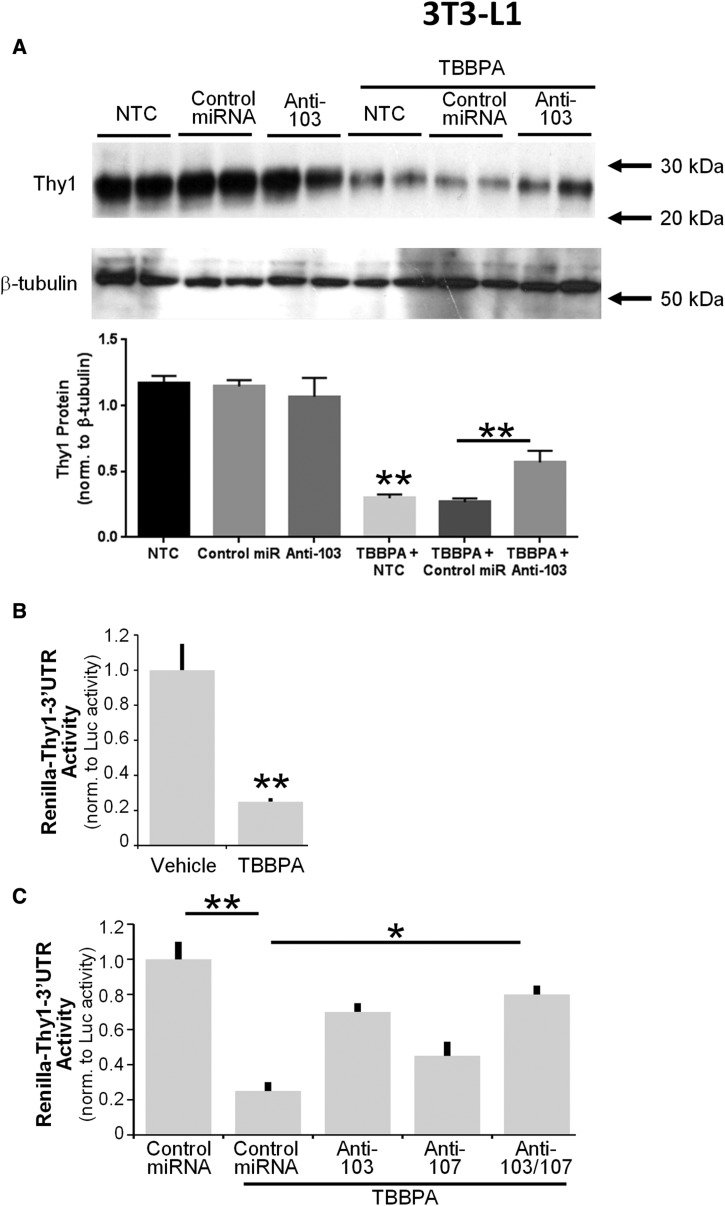
Inhibition of miR-103/107 Function Attenuates the Ability of TBBPA to Target Thy1 Expression
To further test if Thy1 expression is indeed regulated by TBBPA induced miR-103 levels, we introduced either nothing (no transfection control, NTC), a non-specific miRNA inhibitor (control miRNA), or a specific miR-103 inhibitor (anti-103) into 3T3-L1 cells that were treated with vehicle (DMSO) or TBBPA (5 μM) for 4 days. After 4 days of culture, cells were collected and Thy1 protein expression was analyzed by Western blot (Figure 8A). TBBPA reduced Thy1 expression by ∼60% in the NTC and control miRNA inhibitor treatments. Excitingly, the reduction in Thy1 expression was significantly attenuated (∼50% restoration) by addition of a miRNA-103 inhibitor. These data suggest that TBBPA induces miR-103 to reduce Thy1 expression.
FIG. 8.
TBBPA decreases Thy1 levels by increasing miR-103 levels. (A) Either nothing (no transfection control, NTC), a non-specific miRNA inhibitor (control miRNA) or a specific miR-103 inhibitor (anti-103) were introduced into 3T3-L1 cells. Then cells were treated with vehicle (DMSO) or TBBPA (5 μM) for 4 days. After 4 days of culture, cells were collected and Thy1 protein expression was analyzed by Western blot (tubulin serves as a loading control). Densitometry of Western blot analyses is shown below the representative blot. The results shown are a result of three different experiments with three replicate wells measured for each experiment. The data was analyzed by a one-way ANOVA with Tukey’s post-test for significance (*P < .05 and **P < .01). (B) The psiCheck-2 Thy1 3′UTR reporter construct was introduced into 3T3-L1 cells that had been treated in the presence or absence of 5 μM TBBPA for 24 h. 48 h after the addition of the reporter plasmid, cells were lysed and luciferase activity was measured. Normalized luciferase activity is shown. (C) A similar experiment as in (B), however, negative control, anti-103, anti-107 or anti-103/107 miRNA antagomirs were also introduced. After 48 h, luciferase activity was measured. (*P < .05 **P < .001, ANOVA, Tukey’s post test.).
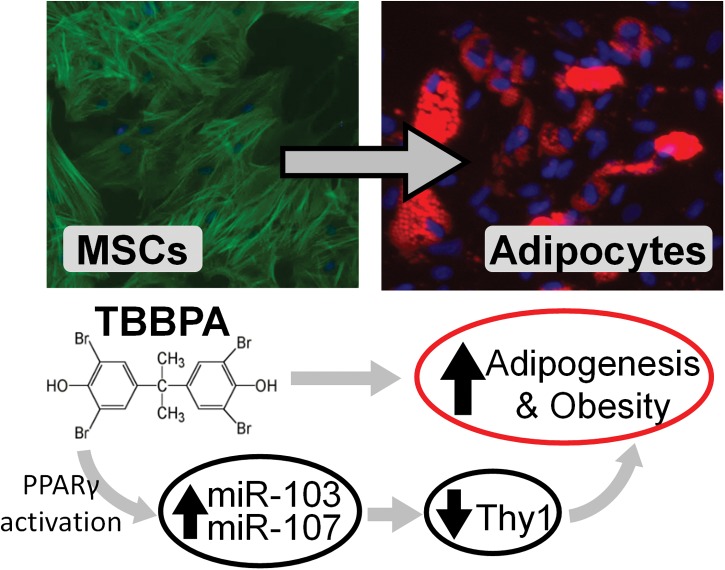
Next, we inserted the human Thy1 3′-untranslated region (3′-UTR), which harbors the miR-103/107 seed sequence, downstream of a Renilla luciferase gene in the psiCheck2 reporter plasmid. The psiCheck2 plasmid also contains a constitutive Firefly luciferase gene which controls for transfection efficiency and can serve to normalize Renilla luciferase reporter activity. When this plasmid was introduced into 3T3-L1 cells, a robust signal of both Renilla and Firefly luciferase activity was detected (Figure 8B). Interestingly, when cells were treated with TBBPA, a 70% reduction in Renilla-Thy1-3′UTR activity was observed. To prove whether or not this reduction was mediated by miR-103/107, specific miRNA inhibitors (antagomirs) to miR-103 and miR-107 or a non-specific control antagomir were introduced. When the non-specific control antagomir was added, a significant reduction in Renilla activity was still observed (Figure 8B). However, when a miR-103 antagomir was used, the ability of TBBPA to silence in Renilla-Thy1-3′UTR activity was significantly attenuated. The addition of a miR-107 antagomir trended to increase Renilla activity but the observation was not significant. However, with the addition of both miR-103 and miR-107 antagomirs, the ability of TBBPA to decrease in Renilla-Thy1-3′UTR activity was further significantly mitigated (Figure 8C). Taken together these results demonstrate that TBBPA promotes adipogenesis and obesity at least in by decreasing Thy1 expression through inducing expression of miR-103/107 (Figure 9).
FIG. 9.
Potential mechanism(s) of action of the environmental chemical TBBPA on adipogenesis and obesity. TBBPA activates PPARγ which induces the expression of miR-103 which in turn leads to a reduction in Thy1 expression. The reduction in Thy1 predisposes MSCs and other progenitor cells toward the adipogenic lineage, thereby promoting adipogenesis and obesity.
DISCUSSION
Obesity and related disorders, such as type 2 diabetes, fatty liver disease, and cardiovascular disease have emerged as one of the most significant public health problems facing the USA and in fact the entire globe (Flegal et al., 2010). Especially concerning is the near outbreak rate of childhood obesity (Ludwig, 2007). If unabated, the “Globesity” epidemic will result in 2.7 billion obese adults by 2025 (Swinburn et al., 2015). In addition to diet and an inactive lifestyle, environmental chemicals may play a role in the current obesity epidemic. TBBPA is currently the most widely used brominated flame retardant (Knudsen et al., 2015). TBBPA can be absorbed through the skin, inhaled, or ingested (Zhou et al., 2014). TBBPA has been detected in human adipose tissue, serum, and in breast milk (Cariou et al., 2008; Johnson-Restrepo et al., 2008) supporting the concept that adipocyte progenitor cells such as MSCs from adults and infants could be chronically exposed to TBBPA. Thus, it is essential that we understand the consequences of TBBPA exposure on MSCs. Here, we present evidence that hMSCs exposed to TBBPA at levels detected in human serum and tissues display signs of enhanced adipogenesis, decreased expression of Thy1 and increased expression of miR-103 and miR-107.
While we show for the first time that the endocrine disruptor, TBBPA decreases Thy1 to enhance adipogenesis, there are potentially hundreds of other endocrine disrupting chemicals that could also target Thy1. For example, TBT is another molecule with similar modes of action to TBBPA that would be a prime candidate to test for its ability to dampen Thy1 levels. The Blumberg group has shown that TBT increases adipogenesis in vivo and in mouse MSCs (Chamorro-Garcia et al., 2013; Grun et al., 2006).
Several recent studies show that TBBPA is a ligand for PPARγ (Riu et al., 2011a, b; Zhuang et al., 2014). We also show here for the first time that, in addition to TBBPA decreasing Thy1 expression, rosiglitazone also potently reduces Thy1 expression. These data suggest that while rosiglitazone beneficially increases insulin sensitivity, it can also be considered to be an obesogen. A recent study demonstrated that rosiglitazone treatment increased the differentiation of adipocyte progenitors into mature adipocytes (Tang et al., 2011). In addition, other studies have documented increased fat deposits and weight gain in both humans and animals treated with rosiglitazone (Chaput et al., 2000; Kang et al., 2010; Ratziu et al., 2008). One mechanism that leads to this increased adipocyte formation may be rosiglitazone mediated reduction in Thy1 expression.
Here, we reveal that miR-103 expression is induced by TBBPA and that induction of this miRNA leads to a reduction of Thy1 expression. While little is known about the regulation of miR-103, one study which integrated data from several large datasets revealed that miR-103 is a PPARγ-dependent miRNA (John et al., 2012). Both miR-103 and miR-107 are intergenic miRNA, being located in introns of pantothenate kinase genes (PANK3 for miR-103, PANK1 for miR-107) (Wilfred et al., 2007). Indeed, both miR-103 and Pank3 expression have been shown to be increased by rosiglitazone in 3T3-L1 pre-adipocytes (John et al., 2012). These data further suggest that TBBPA induces expression of miR-103 through a PPARγ-dependent mechanism.
Interestingly, miR-103 is up-regulated in obesity and in insulin resistance (Trajkovski et al., 2011) suggesting a further link regarding Thy1 expression, TBBPA and obesity. While Thy1 may be one key target of miR-103, there are several hundred predicted targets of this miRNA family. Li et al. (2015) showed that exogenous miR-103 expression promoted adipogenesis in 3T3-L1 cells and one key target of miR-103 was myocyte enhancer factor 2D (MEF2D) which prevented adipogenesis by blocking PI3K/Akt signaling. An additional target of miR-103 is caveolin-1, which regulates insulin receptor function (Trajkovski et al., 2011). Both caveolin-1 and Thy1 are plasma membrane associated proteins and have been shown to interact with the Src family kinase, Fyn (Cohen et al., 2009; Sanguinetti et al., 2003). We have shown that Thy1 regulates Fyn activity to blunt adipogenesis (Woeller et al., 2015a) while others have shown that Caveolin-1 is a phospho-target of Fyn (Sanguinetti et al., 2003). Thus, it would be interesting to determine if there is a combined relationship of Thy1-Fyn-Caveolin-1 signaling that is altered by TBBPA to further enhance adipogenesis.
Another key aspect of this study is that pretreatment with TBBPA further enhanced adipogenesis in cells treated with a pro-adipogenic medium. This suggests that TBBPA may alter the balance of MSC fate. MSCs have the ability to form several effector cell lineages including adipocytes, osteocytes, and scar-forming myofibroblasts (Nery et al., 2013; Scott et al., 2011). In promoting adipogenesis, TBBPA may prevent other MSC-derived cells from forming. PPARγ signaling is implicated in tipping the balance between MSC differentiation into adipocytes or osteocytes (Hong et al., 2005; Xu et al., 2016). In addition, TBBPA exposure to adipose MSCs may cause unwanted or ill-timed initiation of adipogenesis. While there needs to be a constant supply of resident MSCs to form adipocytes or repair adipose tissue when needed, premature formation of adipocytes may exhaust the pool of adipose derived MSCs causing fat storage problems or impairments in tissue repair. In support of this, MSCs obtained from obese individuals show a pronounced lack of “stemness” and have limited ability to form multiple effector cell types but can still form adipocytes (Onate et al., 2013). Interestingly, an earlier report by the same group revealed that Thy1 levels were significantly reduced in MSCs isolated from obese individuals compared with non-obese individuals (Onate et al., 2012). This further supports a role for loss of Thy1 in adipogenesis and obesity and provides additional support for the concept that environmental exposure to TBBPA can increase adipogenesis and obesity in humans.
CONCLUSION
Herein, we provide strong evidence that TBBPA decreases Thy1 expression and promotes adipogenesis in human and mouse cells. Furthermore, TBBPA reduces Thy1 expression by increasing expression of miR-103, which targets Thy1 mRNA. This study reveals a novel molecular mechanism of TBBPA action and how it contributes to adipogenesis and obesity. Finally, this study supports the idea that chemicals should be tested for obesogenic activity using Thy1 as an important readout.
FUNDING
NIH (R21 ES023032, ES027767, R25GM64133), NIEHS Center Grant ES001247 and University of Rochester Institutional Funds.
CONFLICT OF INTEREST
There is not a conflict of interest for authors.
REFERENCES
- Agarwal V., Bell G. W., Nam J. W., Bartel D. P. (2015). Predicting effective microRNA target sites in mammalian mRNAs. Elife 4, e05005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander R., Lodish H., Sun L. (2011). MicroRNAs in adipogenesis and as therapeutic targets for obesity. Expert. Opin. Ther. Targets 15, 623–636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baillie-Hamilton P. F. (2002). Chemical toxins: a hypothesis to explain the global obesity epidemic. J. Altern. Complement Med. 8, 185–192. [DOI] [PubMed] [Google Scholar]
- Bartel D. P. (2009). MicroRNAs: target recognition and regulatory functions. Cell 136, 215–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernacki S. H., Wall M. E., Loboa E. G. (2008). Isolation of human mesenchymal stem cells from bone and adipose tissue. Methods Cell Biol. 86, 257–278. [DOI] [PubMed] [Google Scholar]
- Biemann R., Fischer B., Bluher M., Navarrete Santos A. (2014). Tributyltin affects adipogenic cell fate commitment in mesenchymal stem cells by a PPARgamma independent mechanism. Chem. Biol. Interact. 214, 1–9. [DOI] [PubMed] [Google Scholar]
- Cariou R., Antignac J. P., Zalko D., Berrebi A., Cravedi J. P., Maume D., Marchand P., Monteau F., Riu A., Andre F., et al. (2008). Exposure assessment of French women and their newborns to tetrabromobisphenol-A: occurrence measurements in maternal adipose tissue, serum, breast milk and cord serum. Chemosphere 73, 1036–1041. [DOI] [PubMed] [Google Scholar]
- Chamorro-Garcia R., Kirchner S., Li X., Janesick A., Casey S. C., Chow C., Blumberg B. (2012). Bisphenol A diglycidyl ether induces adipogenic differentiation of multipotent stromal stem cells through a peroxisome proliferator-activated receptor gamma-independent mechanism. Environ. Health Perspect. 120, 984–989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chamorro-Garcia R., Sahu M., Abbey R. J., Laude J., Pham N., Blumberg B. (2013). Transgenerational inheritance of increased fat depot size, stem cell reprogramming, and hepatic steatosis elicited by prenatal exposure to the obesogen tributyltin in mice. Environ. Health Perspect. 121, 359–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaput E., Saladin R., Silvestre M., Edgar A. D. (2000). Fenofibrate and rosiglitazone lower serum triglycerides with opposing effects on body weight. Biochem. Biophys. Res. Commun. 271, 445–450. [DOI] [PubMed] [Google Scholar]
- Cohen P. Y., Breuer R., Wallach-Dayan S. B. (2009). Thy1 up-regulates FasL expression in lung myofibroblasts via Src family kinases. Am. J. Respir. Cell Mol. Biol. 40, 231–238. [DOI] [PubMed] [Google Scholar]
- Deiuliis J. A. (2016). MicroRNAs as regulators of metabolic disease: pathophysiologic significance and emerging role as biomarkers and therapeutics. Int. J. Obes. 40, 88–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Napoli-Davis G., Owens J. E. (2013). Quantitation of tetrabromobisphenol-A from dust sampled on consumer electronics by dispersed liquid-liquid microextraction. Environ. Pollut. 180, 274–280. [DOI] [PubMed] [Google Scholar]
- Flegal K. M., Carroll M. D., Ogden C. L., Curtin L. R. (2010). Prevalence and trends in obesity among US adults, 1999-2008. JAMA 303, 235–241. [DOI] [PubMed] [Google Scholar]
- Green H., Kehinde O. (1975). An established preadipose cell line and its differentiation in culture. II. Factors affecting the adipose conversion. Cell 5, 19–27. [DOI] [PubMed] [Google Scholar]
- Grun F., Watanabe H., Zamanian Z., Maeda L., Arima K., Cubacha R., Gardiner D. M., Kanno J., Iguchi T., Blumberg B. (2006). Endocrine-disrupting organotin compounds are potent inducers of adipogenesis in vertebrates. Mol. Endocrinol. 20, 2141–2155. [DOI] [PubMed] [Google Scholar]
- Heindel J. J., Newbold R., Schug T. T. (2015). Endocrine disruptors and obesity. Nat. Rev. Endocrinol. 11, 653–661. [DOI] [PubMed] [Google Scholar]
- Hendriks H. S., van Kleef R. G., van den Berg M., Westerink R. H. (2012). Multiple novel modes of action involved in the in vitro neurotoxic effects of tetrabromobisphenol-A. Toxicol. Sci. 128, 235–246. [DOI] [PubMed] [Google Scholar]
- Heneghan H. M., Miller N., Kerin M. J. (2010). Role of microRNAs in obesity and the metabolic syndrome. Obes. Rev. 11, 354–361. [DOI] [PubMed] [Google Scholar]
- Hisada K., Hata K., Ichida F., Matsubara T., Orimo H., Nakano T., Yatani H., Nishimura R., Yoneda T. (2013). Retinoic acid regulates commitment of undifferentiated mesenchymal stem cells into osteoblasts and adipocytes. J. Bone Miner. Metab. 31, 53–63. [DOI] [PubMed] [Google Scholar]
- Hong J. H., Hwang E. S., McManus M. T., Amsterdam A., Tian Y., Kalmukova R., Mueller E., Benjamin T., Spiegelman B. M., Sharp P. A., et al. (2005). TAZ, a transcriptional modulator of mesenchymal stem cell differentiation. Science 309, 1074–1078. [DOI] [PubMed] [Google Scholar]
- Honkisz E., Wojtowicz A. K. (2015). The role of PPARgamma in TBBPA-mediated endocrine disrupting effects in human choriocarcinoma JEG-3 cells. Mol. Cell Biochem. 409, 81–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janesick A., Blumberg B. (2011). Minireview: PPARgamma as the target of obesogens. J. Steroid. Biochem. Mol. Biol. 127, 4–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janesick A. S., Blumberg B. (2016). Obesogens: an emerging threat to public health. Am. J. Obstet. Gynecol. 214, 559–565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- John E., Wienecke-Baldacchino A., Liivrand M., Heinaniemi M., Carlberg C., Sinkkonen L. (2012). Dataset integration identifies transcriptional regulation of microRNA genes by PPARgamma in differentiating mouse 3T3-L1 adipocytes. Nucleic Acids Res. 40, 4446–4460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson-Restrepo B., Adams D. H., Kannan K. (2008). Tetrabromobisphenol A (TBBPA) and hexabromocyclododecanes (HBCDs) in tissues of humans, dolphins, and sharks from the United States. Chemosphere 70, 1935–1944. [DOI] [PubMed] [Google Scholar]
- Juonala M., Magnussen C. G., Berenson G. S., Venn A., Burns T. L., Sabin M. A., Srinivasan S. R., Daniels S. R., Davis P. H., Chen W., et al. (2011). Childhood adiposity, adult adiposity, and cardiovascular risk factors. N. Engl. J. Med. 365, 1876–1885. [DOI] [PubMed] [Google Scholar]
- Kang J. G., Park C. Y., Ihm S. H., Yoo H. J., Park H., Rhee E. J., Won J. C., Lee W. Y., Oh K. W., Park S. W., et al. (2010). Mechanisms of adipose tissue redistribution with rosiglitazone treatment in various adipose depots. Metabolism 59, 46–53. [DOI] [PubMed] [Google Scholar]
- Knudsen G. A., Hughes M. F., McIntosh K. L., Sanders J. M., Birnbaum L. S. (2015). Estimation of tetrabromobisphenol A (TBBPA) percutaneous uptake in humans using the parallelogram method. Toxicol. Appl. Pharmacol. 289, 323–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- La Merrill M., Birnbaum L. S. (2011). Childhood obesity and environmental chemicals. Mt. Sinai J. Med. 78, 22–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehmann G. M., Woeller C. F., Pollock S. J., O’Loughlin C., Gupta W. S., Feldon S. E., Phipps R. P. (2010). Novel anti-adipogenic activity produced by human fibroblasts. Am. J. Physiol. Cell Physiol. 299, C672–C681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li M., Liu Z., Zhang Z., Liu G., Sun S., Sun C. (2015). miR-103 promotes 3T3-L1 cell adipogenesis through AKT/mTOR signal pathway with its target being MEF2D. Biol. Chem. 396, 235–244. [DOI] [PubMed] [Google Scholar]
- Ludwig D. S. (2007). Childhood obesity—the shape of things to come. N. Engl. J. Med. 357, 2325–2327. [DOI] [PubMed] [Google Scholar]
- Nery A. A., Nascimento I. C., Glaser T., Bassaneze V., Krieger J. E., Ulrich H. (2013). Human mesenchymal stem cells: from immunophenotyping by flow cytometry to clinical applications. Cytometry A 83, 48–61. [DOI] [PubMed] [Google Scholar]
- Onate B., Vilahur G., Camino-Lopez S., Diez-Caballero A., Ballesta-Lopez C., Ybarra J., Moscatiello F., Herrero J., Badimon L. (2013). Stem cells isolated from adipose tissue of obese patients show changes in their transcriptomic profile that indicate loss in stemcellness and increased commitment to an adipocyte-like phenotype. BMC Genomics 14, 625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onate B., Vilahur G., Ferrer-Lorente R., Ybarra J., Diez-Caballero A., Ballesta-Lopez C., Moscatiello F., Herrero J., Badimon L. (2012). The subcutaneous adipose tissue reservoir of functionally active stem cells is reduced in obese patients. FASEB J. 26, 4327–4336. [DOI] [PubMed] [Google Scholar]
- Perri R., Nares S., Zhang S., Barros S. P., Offenbacher S. (2012). MicroRNA modulation in obesity and periodontitis. J. Dent. Res. 91, 33–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ratziu V., Giral P., Jacqueminet S., Charlotte F., Hartemann-Heurtier A., Serfaty L., Podevin P., Lacorte J. M., Bernhardt C., Bruckert E., et al. (2008). Rosiglitazone for nonalcoholic steatohepatitis: one-year results of the randomized placebo-controlled Fatty Liver Improvement with Rosiglitazone Therapy (FLIRT) trial. Gastroenterology 135, 100–110. [DOI] [PubMed] [Google Scholar]
- Riu A., Grimaldi M., le Maire A., Bey G., Phillips K., Boulahtouf A., Perdu E., Zalko D., Bourguet W., Balaguer P. (2011a). Peroxisome proliferator-activated receptor gamma is a target for halogenated analogs of bisphenol A. Environ. Health Perspect. 119, 1227–1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riu A., le Maire A., Grimaldi M., Audebert M., Hillenweck A., Bourguet W., Balaguer P., Zalko D. (2011b). Characterization of novel ligands of ERalpha, Erbeta, and PPARgamma: the case of halogenated bisphenol A and their conjugated metabolites. Toxicol. Sci. 122, 372–382. [DOI] [PubMed] [Google Scholar]
- Riu A., McCollum C. W., Pinto C. L., Grimaldi M., Hillenweck A., Perdu E., Zalko D., Bernard L., Laudet V., Balaguer P., et al. (2014). Halogenated bisphenol-A analogs act as obesogens in zebrafish larvae (Danio rerio). Toxicol. Sci. 139, 48–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanguinetti A. R., Cao H., Corley Mastick C. (2003). Fyn is required for oxidative- and hyperosmotic-stress-induced tyrosine phosphorylation of caveolin-1. Biochem. J. 376, 159–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmittgen T. D., Livak K. J. (2008). Analyzing real-time PCR data by the comparative C(T) method. Nat. Protoc. 3, 1101–1108. [DOI] [PubMed] [Google Scholar]
- Scott M. A., Nguyen V. T., Levi B., James A. W. (2011). Current methods of adipogenic differentiation of mesenchymal stem cells. Stem Cells Dev. 20, 1793–1804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swinburn B., Dietz W., Kleinert S. (2015). A Lancet Commission on obesity. Lancet 386, 1716–1717. [DOI] [PubMed] [Google Scholar]
- Tang W., Zeve D., Seo J., Jo A. Y., Graff J. M. (2011). Thiazolidinediones regulate adipose lineage dynamics. Cell Metab. 14, 116–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tontonoz P., Spiegelman B. M. (2008). Fat and beyond: the diverse biology of PPARgamma. Annu. Rev. Biochem. 77, 289–312. [DOI] [PubMed] [Google Scholar]
- Trajkovski M., Hausser J., Soutschek J., Bhat B., Akin A., Zavolan M., Heim M. H., Stoffel M. (2011). MicroRNAs 103 and 107 regulate insulin sensitivity. Nature 474, 649–653. [DOI] [PubMed] [Google Scholar]
- Vafeiadi M., Georgiou V., Chalkiadaki G., Rantakokko P., Kiviranta H., Karachaliou M., Fthenou E., Venihaki M., Sarri K., Vassilaki M., et al. (2015). Association of prenatal exposure to persistent organic pollutants with obesity and cardiometabolic traits in early childhood: The Rhea Mother-Child Cohort (Crete, Greece). Environ. Health Perspect. 123, 1015–1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vatandoost N., Amini M., Iraj B., Momenzadeh S., Salehi R. (2015). Dysregulated miR-103 and miR-143 expression in peripheral blood mononuclear cells from induced prediabetes and type 2 diabetes rats. Gene 572, 95–100. [DOI] [PubMed] [Google Scholar]
- Vienberg S., Geiger J., Madsen S., Dalgaard L. T. (2016). MicroRNAs in metabolism. Acta Physiol. 219, 346–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watt J., Schlezinger J. J. (2015). Structurally-diverse, PPARgamma-activating environmental toxicants induce adipogenesis and suppress osteogenesis in bone marrow mesenchymal stromal cells. Toxicology 331, 66–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilfred B. R., Wang W. X., Nelson P. T. (2007). Energizing miRNA research: a review of the role of miRNAs in lipid metabolism, with a prediction that miR-103/107 regulates human metabolic pathways. Mol. Genet. Metab. 91, 209–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woeller C. F., O’Loughlin C. W., Pollock S. J., Thatcher T. H., Feldon S. E., Phipps R. P. (2015a). Thy1 (CD90) controls adipogenesis by regulating activity of the Src family kinase, Fyn. FASEB J. 29, 920–931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woeller C. F., O’Loughlin C. W., Roztocil E., Feldon S. E., Phipps R. P. (2015b). Salinomycin and other polyether ionophores are a new class of antiscarring agent. J. Biol. Chem. 290, 3563–3575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie H., Lim B., Lodish H. F. (2009). MicroRNAs induced during adipogenesis that accelerate fat cell development are downregulated in obesity. Diabetes 58, 1050–1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu C., Wang J., Zhu T., Shen Y., Tang X., Fang L., Xu Y. (2016). Cross-talking between PPAR and WNT signaling and its regulation in mesenchymal stem cell differentiation. Curr. Stem. Cell Res. Ther. 11, 247–254. [DOI] [PubMed] [Google Scholar]
- Yamamoto N., Akamatsu H., Hasegawa S., Yamada T., Nakata S., Ohkuma M., Miyachi E., Marunouchi T., Matsunaga K. (2007). Isolation of multipotent stem cells from mouse adipose tissue. J. Dermatol. Sci. 48, 43–52. [DOI] [PubMed] [Google Scholar]
- Zhou X., Guo J., Zhang W., Zhou P., Deng J., Lin K. (2014). Tetrabromobisphenol A contamination and emission in printed circuit board production and implications for human exposure. J. Hazard. Mater. 273, 27–35. [DOI] [PubMed] [Google Scholar]
- Zhuang S., Zhang C., Liu W. (2014). Atomic insights into distinct hormonal activities of Bisphenol A analogues toward PPARgamma and ERalpha receptors. Chem. Res. Toxicol. 27, 1769–1779. [DOI] [PubMed] [Google Scholar]