Abstract
Aims
To develop Swahili versions of the Alcohol Use Disorders Identification Test (AUDIT) and CAGE questionnaires and evaluate their psychometric properties in a traumatic brain injury (TBI) population in Tanzania.
Methods
Swahili versions of the AUDIT and CAGE were developed through translation and back-translation by a panel of native speakers of both English and Swahili. The translated instruments were administered to a sample of Tanzanian adults from a TBI registry. The validity and reliability were analyzed using standard statistical methods.
Results
The translated versions of both the AUDIT and CAGE questionnaires were found to have excellent language clarity and domain coherence. Reliability was acceptable (>0.85) for all tested versions. Confirmatory factor analysis of one, two and three factor solution for the AUDIT and one factor solution for the CAGE showed adequate results. AUDIT and CAGE scores were strongly correlated to each other (R > 0.80), and AUDIT scores were significantly lower in non-drinkers compared to drinkers.
Conclusions
This article presents the first Swahili and Tanzanian adaptations of the AUDIT and CAGE instruments as well as the first validation of these questionnaires with TBI patients. Both instruments were found to have acceptable psychometric properties, resulting in two new useful tools for medical and social research in this setting.
INTRODUCTION
Excessive alcohol use, both binge drinking and chronic use, has been associated with many high risk behaviors for injuries such as crime, aggressive driving, interpersonal violence, unintentional injuries and self-inflicted injury (Organization, 2015). Alcohol use is an important contributor to morbidity and mortality for many diseases worldwide, accounting for 6% of all deaths and 9.6% of disability adjusted life years (DALYS) (Whiteford et al., 2013; Molina et al., 2015; World Health Organization, 2017; Ogeil et al., 2016; Lhachimi et al., 2016; Praud et al., 2016; Nadkarni et al., 2016; Popova et al., 2016; Younossi and Henry, 2016; Unsworth and Mathias, 2017). In sub-Saharan Africa, research estimates that ~40% of all alcohol-attributable deaths and 40% of DALYs in men are due to injury; for women, estimates are ~10% deaths and more than 14% of DALYs. (Ferreira-Borges et al., 2016).
Of all injuries, traumatic brain injuries (TBIs) are responsible for the most death and disability globally (Hyder et al., 2007; Staton et al., 2017); TBIs are also the leading cause of disability in people <40 years of age (Bruns and Hauser, 2003; Fleminger and Ponsford, 2005). In Tanzania, the estimated burden of TBI at a regional referral hospital is ~6% of all emergency department visits, or ~1000 patients annually (Staton et al., 2017). Of acute TBI patients seen at this hospital, almost 30% of them presenting for care to the emergency department had alcohol use prior to their injury (Staton et al., 2017). Both globally and in Tanzania, of those who survive their debilitating injury, many (nearly 30%) either continue to suffer from or have a new substance use disorder (Zatzick et al., 2002; Vissoci et al., 2016).
Given the important role alcohol plays in many health outcomes, especially for injury and TBI patients, developing tools to screen for alcohol misuse has become essential in both clinical practice and public health research. Two of the most frequently used tools are the Alcohol Use Disorders Identification Test (AUDIT) and CAGE questionnaires, but neither have been cross-culturally validated to Swahili nor have been psychometrically evaluated with a TBI population. As the leading cause of the most socially and functionally disabling injuries (Schultheis and Whipple, 2014; von Steinbuechel et al., 2016), TBI patients are the most likely to need alcohol use disorder assessments, yet the validity of these instruments for this population is unknown.
AUDIT was originally developed by the WHO and consists of 10 questions assessing alcohol use, dependence and harmful behavior (Saunders et al., 1993). Since its publication, the AUDIT tool has been translated into numerous languages and validated among many different populations. The tool has been shown to have acceptable validity and reliability across a wide range of settings, including Sweden (Bergman and Kallmen, 2002), Korea (Kim et al., 1999), Nepal (Pradhan et al., 2012), Brazil (Moretti-Pires and Corradi-Webster, 2011), Japan (Kawada et al., 2011), Chile (Alvarado et al., 2009), the United Arab Emirates (AlMarri et al., 2009), Spain (de Torres et al., 2009), Germany (Dybek et al., 2006), France (Gache et al., 2005), India (Pal et al., 2004) and Hong Kong (Leung and Arthur, 2000), among others. Specifically for TBI populations, studies have looked into the criterion validity (Bryce et al., 2015), but not other measures of validity.
Although Kenya was one of the six international sites where the English language AUDIT tool was originally developed and validated (Saunders et al., 1993), there is limited rigorous evaluation of the psychometric properties of the AUDIT tool elsewhere on the continent. The AUDIT questionnaire has been used to assess prevalence of alcohol use disorders in various sub-Saharan African populations, but the majority has occurred without formal cultural cross-validation of the translated instrument in the local setting (Zetola et al., 2012; Soboka et al., 2014; Francis et al., 2015; Schwitters et al., 2015; Seth et al., 2015; Wandera et al., 2015; Fekadu et al., 2016; Lancaster et al., 2016; Thakarar et al., 2016; Weiss et al., 2016). Preliminary studies assessing usage of the AUDIT in Nigeria, South Africa and Zambia found the tool to be a valid screening instrument when compared to ICD-10 or Mini International Neuropsychiatric Interview questionnaire (MINI) criteria for alcohol misuse, with areas under the curve ranging from 0.75 to 0.98 (Adewuya, 2005; Myer et al., 2008; Chishinga et al., 2011). The reliability of AUDIT has also been assessed among subpopulations in South Africa (Young and Mayson, 2010; Peltzer et al., 2011; Pengpid et al., 2011), Zambia (Chishinga et al., 2011) and Rwanda (Kanyoni et al., 2015), where the tool was found to have excellent reliability, with Cronbach's alpha ranging from 0.83 to 0.98. However, beyond criterion validity and reliability, the broader spectrum of psychometric properties of AUDIT across sub-Saharan Africa, including Tanzania, have not been fully explored; furthermore, validated translations of the questionnaire in widely used local languages such as Swahili are sorely lacking. Although the AUDIT has consistently shown good reliability across cultures and good validity for screening for alcohol-use disorder, its internal structure, specifically the ability to differentiate an alcohol use disorder (i.e. unidimensional, two dimensions) displays diverse results in different cultures and populations and has not been tested in Swahili or TBI patients.
Similar to the AUDIT, the CAGE survey is designed to screen for alcohol dependence and abuse (Ewing, 1984). The CAGE questionnaire has also been translated into many different languages and validated in settings across the globe such as Korea (So and Sung, 2013), Brazil (Meneses-Gaya et al., 2010), Taiwan (Wu et al., 2008) and France (Gache et al., 2005). As with AUDIT, few studies have investigated the psychometric properties of the CAGE tool in sub-Saharan Africa, and none have been conducted among TBI patients. The CAGE questionnaire has been used in several studies to assess prevalence of alcohol abuse in various sub-Saharan African populations, but frequently without prior validation of the translated instrument for the local setting (Alem et al., 1999; Kebede and Alem, 1999; Siegfried et al., 2001; Okulate and Odunaike, 2005; Mitsunaga and Larsen, 2008; Ghebremichael et al., 2009; Kullgren et al., 2009; Namagembe et al., 2010; Ao et al., 2011; Mongi et al., 2013; Opio et al., 2013; Weiss et al., 2016). To our knowledge, only one study has formally assessed the validity of CAGE in the sub-Saharan region. This was conducted in a single rural South African community, where CAGE was found to have acceptable sensitivity and specificity when compared to the DSM-IV definition of alcohol dependence (100 and 78%, respectively) with adequate reliability (Cronbach's alpha = 0.7) (Claassen, 1999). The psychometric properties of CAGE elsewhere in the sub-Saharan continent are otherwise unknown, and validated translations of the tool in local languages such as Swahili for TBI patients are utterly absent.
Despite the recognized importance of the relationship between alcohol use disorders and injury in sub-Saharan Africa, validated tools for measuring alcohol misuse such as the CAGE and AUDIT are unavailable in most African communities (de Meneses-Gaya et al., 2009; Francis et al., 2014). Thus, there is a pressing need to develop such reliable objective measures to inform practice and policy, particularly among TBI patients among whom alcohol use has been shown to be a significant contributor to morbidity and mortality (Molina et al., 2015). There are no validated versions of these tools in Swahili, a common language spoken across East Africa, and no formal validation studies have been performed in Tanzania, where Swahili is the primary language. Therefore, the aims of this study were to (a) develop the first translation and adaptation of both AUDIT and CAGE in Swahili and (b) to perform the analysis of their psychometric properties in Tanzanian TBI patients, including evidence of reliability, internal structure and external validity.
METHODS
Participants
The study sample was composed of 190 adults who were part of a TBI patient registry and post-hospitalization cohort study in northern Tanzania. Participants were included if they sought acute care for a TBI of any severity, as long as they were admitted for continued care, were at least 18 years of age, spoke Swahili, were able to understand and respond to questions appropriately and consented to participate prior to hospital discharge.
Instrument
The original scales used were the AUDIT (Saunders et al., 1993) and CAGE (Ewing, 1984) questionnaires. The AUDIT tool consists of 10 questions across three domains (alcohol use, alcohol abuse and harmful behavior) and an overall score ranging from 0 to 40. The answer to each question is scored on a 5-point Likert-type scale, with assigned point values ranging from 0 to 4. The CAGE questionnaire consists of four dichotomous questions, each of which is scored as 1 for ‘yes’ and 0 for ‘no’. Higher scores on both scales are correlated with increasing probability of alcohol misuse and dependence. Alcohol use questions covered alcohol consumption over the past 12 months; non-drinkers were defined as those who had consumed no alcohol over the preceding year. In terms of quantifying the number of drinks consumed, the National Institute on Alcohol Abuse and Alcoholism recommended guidelines for standard drinks was used (2017).
Ethical statement
The study was approved by the Institutional Review Board of the Duke University (IRB #Pro000061652), the Ethics Committee of the Kilimanjaro Christian Medical Center, Moshi, Tanzania.
Translation and adaptation
A translation and cross-cultural adaptation committee of five judges (physicians, nurses and researchers) oversaw the translation, adaptation and content validation process. After finalizing content validation, a pilot study was conducted with a convenience sample of 20 Tanzanian adults to assess the quality of instrument questions and coherence of language and content.
The instrument was translated through independent back translation methods, as suggested by the WHO for health outcomes translation (Erkut, 2010). Initially, a Swahili translator was hired to translate AUDIT and CAGE questionnaires into Swahili. Subsequently, another bilingual translator converted the Swahili version back into English. English translated versions were compared with the original version of the instrument and checked for inconsistencies by four independent bilingual research nurses. Issues with semantics were discussed and adjustments made by the researchers and the judges committee.
To perform theoretical and content evaluation of the translated instrument, we employed a five-point Likert scale with the aim of verifying: (a) practical relevance, (b) language clarity of the translated instrument and (c) theoretical coherence of the item, as determined by the judges. These scales allowed for an evaluation of the consistency of the judges’ opinions in relation to the items of the instrument. The experts’ opinions were initially collected individually with the scale and later discussed collectively in focus group sessions to improve the quality of the translations and discuss any discordances.
Data collection
Patients in the Kilimanjaro Christian Medical Center TBI registry were screened for inclusion in a follow-up cohort project. They were offered enrollment after informed consent and subsequently enrolled prior to hospital discharge. The patient had the AUDIT and CAGE questions administered at the bedside as a part of a 45-min interview that served as a baseline for future follow-up evaluations. All responses were collected by hand and entered into an Internet based dataset (REDCAPS); additionally, the principal investigator (C.A.S.) conducted a quality control evaluation for all data entered.
Data analysis
Sociodemographic data were presented as means with standard deviations, medians with interquartile range, or absolute and relative frequencies. All analyses were conducted with R Language for Statistical Computing (R foundation, Vienna).
Evidence of validity
Content validity was evaluated by a content validity coefficient for each item of the instrument (CVCi) and for the questionnaire as a whole (CVCt) (Hernandez-Nieto, 2002), with a cutoff of 0.80 deemed to be acceptable. To analyze the concordance index between judges for the theoretical dimensions of the items, the Kappa coefficient was used.
Confirmatory factor analysis (CFA) was used to test the internal structure of the AUDIT and the CAGE based on the previous literature looking at the factor structure in different populations. Although the AUDIT was originally conceived to be a three dimensions tool that evaluated alcohol use, dependence and harmful behavior (Babor et al., 2001; de Meneses-Gaya et al., 2009), several reports suggested that a two dimension structure (aggregating the dependence and harmful subscales) would perform better (Doyle et al., 2007; Von Der Pahlen et al., 2008; Rist et al., 2009; Nayak et al., 2015; Tuliao et al., 2016). However, the most common use of the AUDIT is a sum score of all items as a unidimensional scale (Carey et al., 2003; English et al., 2011), from which cutoff points have been established. Therefore, we tested the three existing models based on previous evidence, to verify which structure would best be represented in a TBI population. Our hypothesis was that the unidimensional model would perform better considering the high association between alcohol use and alcohol dependence in the sub-Saharan Africa, making it harder to differentiate the subscales. For the CAGE, we tested for the unidimensional model (Table 1).
Table 1.
Sociodemographic profile of the validation sample
| Variables | |
|---|---|
| Age (years), mean (SD) | 33.87 (13.32) |
| Household size, mean (SD) | 4.43 (2.48) |
| Monthly personal income, USD, mean (SD) | $104.42 (100.08) |
| Monthly family income, USD, mean (SD) | $155.20 (235.52) |
| Male, N (%) | 159 (82.8) |
| Married, N (%) | 104 (54.7) |
| Occupation, N (%) | |
| Business | 44 (21.7) |
| Farming | 41 (22.3) |
| Skilled worker | 23 (12.5) |
| Salaried worker | 67 (36.4) |
| Other | 13 (7.1) |
| Education, N (%) | |
| Some primary education | 112 (59.3) |
| Some secondary education | 44 (23.3) |
| Some university education | 33 (17.5) |
CFA model adequacy was tested using Weighted Least Square Means and Variance Adjusted (WLSMV). Model adjustment was tested through the fit indices (reference of expected values for each index): Chi-square (X2 and P-value), Root Mean Square Error of Approximation (RMSEA < 0.08, I.C. 90%), Tucker–Lewis index (TLI > 0.90) and comparative fit index (CFI > 0.95). These indices aim to assess whether the model shows a good fit to the data, as proposed in the literature (Hu and Bentler, 1999; Kline, 2012). Average variance extracted (AVE) was calculated and values >0.50 were considered acceptable indicators of convergent validity (Hair et al., 2005).
Both measures (AUDIT and CAGE) have been shown to be highly correlated in previous literature (Cremonte et al., 2010). Thus, we tested external validity by correlating both scores. Our hypothesis was that the translated and adapted versions of the AUDIT and CAGE questionnaires to Swahili would also correlate positively, confirming the instrument's ability to behave as expected in relation to the theoretical concept. We also tested external validity by comparing AUDIT scores between injury patients reporting use of alcohol in the past 12 months and injury patients who abstained from alcohol in the past 12 months. Our hypothesis was that AUDIT would be able to differentiate groups by group comparison using Mann–Whitney with a significance of 5%.
Reliability
Reliability is the capacity of an instrument to produce consistent results in different situations. We measured reliability with internal consistency to assess the degree to which all of the items in the instrument refer to the same subject (Devellis, 2003). To measure internal consistency we used the Cronbach's alpha for the AUDIT and the Kuder-Richardson-20 (KR20) for the CAGE, given it is a dichotomous scale. (Kuder and Richardson, 1937) Similarly, composite reliability (CR) and McDonald's Omega coefficient were calculated using CFA results. Each coefficient has its strengths and limitations (Padilla and Divers, 2016); thus, we choose to compare indicators.
RESULTS
Sample characteristics
Most of the participants were male (83%), married (55%) and had some primary education (59%). The average age was 33.87 years old (SD = 13.32), with an average household size of 4.43 (SD = 2.48) individuals. Average personal monthly income among participants was 104.42 USD (Table 1). Most patients (91%) showed mild injury severity, measured by Glasgow Coma Score.
Regarding the alcohol use behavior, 55% of the participants reported having used alcohol in the past 12 months, with ~25% reporting using alcohol on a weekly basis. The majority (78%) of the sample reported consuming one or two units of drinks per drinking day, while almost all (96.3) of the participants reported using a maximum of four drinks per drinking day. Only 4%, approximately, used more than five drinks per drinking day. Relating to alcohol use prior to the injury, 26% of the patients showed positive alcohol use, assessed by the healthcare professionals at arrival to the hospital.
Translation and adaptation
All items obtained language clarity and domain coherence coefficients above 0.80 for both questionnaires (Table 2). These findings indicate that the translated and adapted versions of the AUDIT and CAGE questionnaires are clearly understandable within Tanzanian culture, in addition to being relevant and pertinent. AUDIT and CAGE item classification agreement among judges was also above 0.80, indicating that the evaluators found the items to be consistent with the underlying theoretical conceptualization (Table 2).
Table 2.
Reliability and confirmatory factor analysis model fit indicators
| AUDIT 1 factor model | AUDIT 2 factor modela | AUDIT 3 factor modela | CAGE | |
|---|---|---|---|---|
| Reliability | ||||
| Cronbach's alpha (CI 95%) | 0.85 (0.83;088) | 0.64 (0.57;0.72)/0.79 (0.75;0.83) | 0.64 (0.57;0.72)/ 0.64 (0.56/0.71)/ 0.65 (0.58;0.73) | 0.76 (0.71;0.81) |
| Omega 6 | 0.88 | 0.67/0.79 | 0.67/0.58/0.61 | 0.73 |
| Composite reliability | 0.95 | 0.87/0.93 | 0.87/0.85/0.88 | 0.77 |
| CFA | ||||
| X2 (Df)/P-value | 33.74 (35)/0.529 | 33.35 (34)/0.499 | 36.72 (34)/0.499 | 3.02 (2)/0.221 |
| RMSEA (CI 95%) | 0.00 (0.00;0.05) | 0.00 (0.00;0.05) | 0.00 (0.00;0.06) | 0.05 (0.00;0.06) |
| TLI | 0.99 | 0.99 | 0.99 | 0.98 |
| CFI | 0.99 | 0.99 | 0.99 | 0.99 |
| Average extracted variance | 0.66 | 0.69/0.66 | 0.69/0.66/0.64 | 0.47 |
| Item thresholds range (Item #) | 0.57 (1)–2.01 (8) | |||
aAll paths significant
CFA = confirmatory factor analysis; X2 = chi-square; Df = degree of freedom; RMSEA = root mean square error of approximation; TLI = Tucker–Lewis index; CFI = comparative fit index.
Internal structure
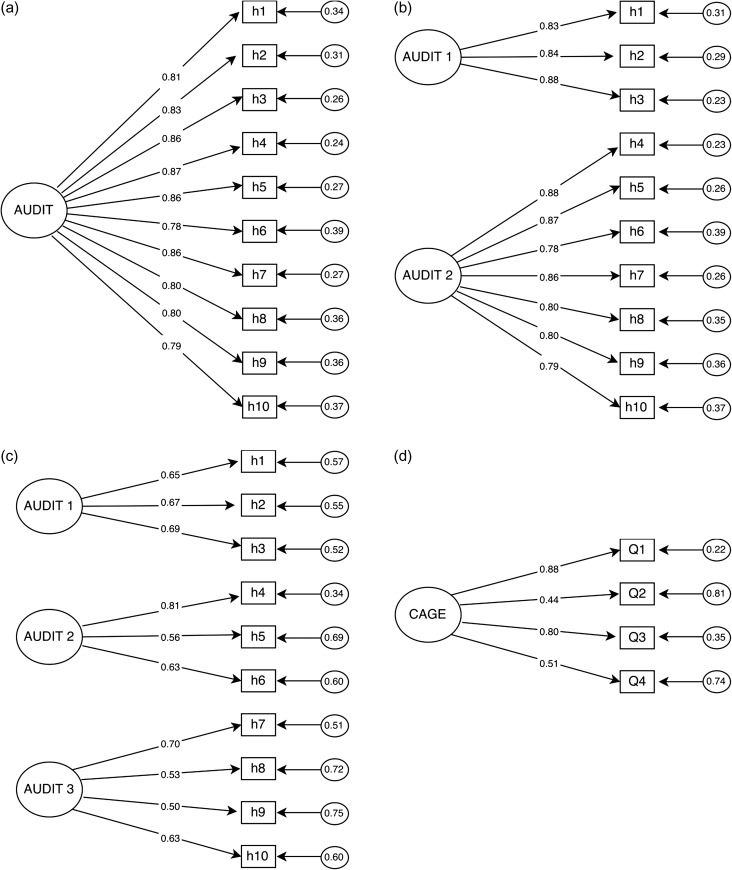
All AUDIT CFA models (one, two and three factor models) performed well, showing all items with factor loadings ranging from 0.41 to 0.71 (Fig. 1). All AUDIT models showed adequate fit indicators (Table 2). CAGE's CFA model showed adequate fit indicators and individual item reliability (Table 2 and Fig. 1).
Fig. 1.
Confirmatory factor analysis diagram, factor loadings for the AUDIT's (a) one factor model, (b) two factor model, (c) three factor model and CAGE (d) one factor model.
Reliability
Reliability were considered adequate with values above 0.80 for the unidimensional AUDIT and above 0.70 for CAGE in all reliability measurements, indicating strong internal consistency for both questionnaires (Table 2). When looking at the possible two and three dimensions structures for the AUDIT, both showed acceptable reliability values (~0.70) in all dimensions. However, reliability performance was worse than the AUDIT 1D model.
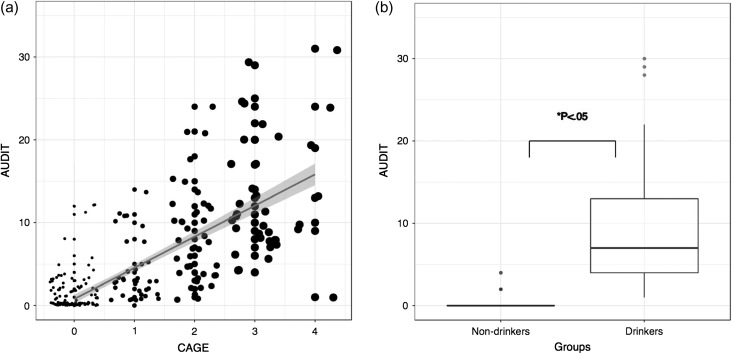
Validity evidences
AUDIT and CAGE scores showed a strong positive correlation (R = 0.78, P = 0.01), showing that both tools agreed and performed as expected. Both scales also behaved as anticipated when comparing groups of drinkers and non-drinkers (Fig. 2). Group comparison showed significantly lower AUDIT scores (P < 0.05) for participants reporting not having used alcohol in the past 12 months than those who reported alcohol use (Fig. 2).
Fig. 2.
Correlation between AUDIT score and CAGE and known group comparison.
DISCUSSION
To our knowledge, current validation studies of AUDIT and CAGE performed elsewhere in sub-Saharan Africa have only assessed the diagnostic ability of the scales, comparing these instruments to either MINI criteria, the DSM-IV criteria or ICD-10 criteria for alcohol misuse or dependence (Claassen, 1999; Adewuya, 2005; Myer et al., 2008; Chishinga et al., 2011). This study incorporated an analysis of several other measures of validity and reliability relevant to provide evidence on the psychometric properties of AUDIT and CAGE. This is the first study to conduct a cross-cultural adaptation of the AUDIT and CAGE questionnaires in Swahili in Tanzania, and is also the first study to assess the validity of AUDIT and CAGE in a TBI population in sub-Saharan Africa. Both questionnaires, in their translated versions, performed as expected in unidimensional models and showed similar psychometric properties in relation to other languages and other populations. No specific modifications were needed for our TBI population, suggesting that the Swahili version of the AUDIT and CAGE can be used to evaluate alcohol use in this specific injury population.
The AUDIT questionnaire was originally designed to have three dimensions: one dealing with frequency of alcohol use, one with alcohol dependence, and one with risky behavior related to alcohol use (Saunders et al., 1993). However, multiple previous psychometric analyses have shown that AUDIT's internal structure is most consistent with a 2D model (Bergman and Kallmen, 2002; Cook et al., 2011). Functionally, however, the AUDIT is typically used in a unidimensional fashion, where a single total score is used to provide a global assessment of alcohol misuse. In our analysis of the internal structure of the Swahili version of AUDIT, an analysis of one, two and three dimensions models all demonstrated excellent fit, suggesting that any of these three models are acceptable. The apparent equivalence of the one, two and three dimensions models in this study may be a reflection of the close correlation between frequency of alcohol use, alcohol dependence, and risky behavior in this patient population (Kallmen et al., 2014). The CAGE questionnaire was found to have a unidimensional internal structure in our analysis, consistent with its original design (Ewing, 1984).
The AUDIT was found to have excellent internal consistency in our study (Table 1), similar to the findings of studies performed in South Africa, Zambia and Rwanda. (Young and Mayson, 2010; Chishinga et al., 2011; Peltzer et al., 2011; Pengpid et al., 2011; Kanyoni et al., 2015) CAGE also had acceptable internal reliability in our study (Table 1), similar to the value reported by in South Africa (Claassen, 1999). However, Cronbach's alpha has been repeatedly criticized in the specialized literature (Padilla and Divers, 2016); thus, results for the CR and Omega coefficients, which have shown less bias, were also calculated. Interestingly, all reliability coefficients (Alpha, CR and Omega) were consistent for both the AUDIT and the CAGE, which confirms a good reliability of the Swahili translated versions considering item-item correlation, factor loading distribution (Padilla and Divers, 2016). However, the reliability of the AUDIT's two and three factor models was not as good as the one factor model (Table 1).
In this study, AUDIT and CAGE scores were noted to be significantly higher among drinkers than non-drinker as expected, suggesting that these instruments are able to discriminate the population exposed to alcohol use. Additional research will likely be needed to compare the performance of the validated Swahili versions of AUDIT and CAGE presented here to other measures of alcohol abuse. Validation studies of AUDIT and CAGE elsewhere have assessed external validity by comparing the performance of these tools to other instruments such as the MINI criteria for alcohol abuse of the DSM-IV criteria for alcohol dependence (Claassen, 1999; Myer et al., 2008; Chishinga et al., 2011). No such comparison was performed in this study, partly because there is no clear gold standard tool for measuring alcohol misuse and so any such analyses of areas under the curve would be difficult to interpret.
Results of this study should be taken in context of its limitations. One limitation is related to our sample. The participants in this study were drawn from a sample of patients participating in a TBI registry and longitudinal cohort who were able to respond to survey questions. Such sampling allowed for validation of the AUDIT and CAGE questionnaires in a TBI population; since TBI is the leading cause of death and disability due injury at our hospital, this is an important first step in understanding the interplay between alcohol use and traumatic injury in Tanzania. While our population is composed of mostly mild TBI patients, this represents the majority of patients treated at our hospital, and those who will survive with good function; this resource limited setting with extensive access to care issues is typical for other low and middle income referral hospital settings (Staton et al., 2017). However, the TBI population is unlikely to be representative of the entire adult Tanzanian population; therefore, additional research will be needed to validate AUDIT and CAGE in a more diverse patient population before using these tools in other Tanzanian groups.
Similarly, in Tanzania and globally, both alcohol use as well as TBI in Tanzania disproportionately affects males which is reflected in our unbalanced sample. Therefore, although it has been previously reported that gender influences the performance of the AUDIT and CAGE (de Meneses-Gaya et al., 2009; Staton et al., 2017 Tanzania: challenges and the way forward), we were not able to gather enough patients to compare across gender. Generalization in the usage of the scale should be considered carefully when applying to gender based comparisons. Further studies should look into the influence of gender in the performance of Swahili translated AUDIT and CAGE. A second limitation of this study is the absence of criterion validity analysis in our study, which would have allowed for a calculation of sensitivity and specificity and cutoff points of the validated instruments presented here. Tanzania, currently, has no psychiatric human resources available to support an adequate DSM-IV screening, or to train healthcare providers to do so. As a step to a broader project about the psychiatric assessment of substance use, this project aimed specifically at evaluating the translation and adaptation of the AUDIT and CAGE to Swahili. Assuring that the current version of the instruments are psychometric adequate, we suggest that the criterion validity should be the subject of future work. A third limitation refers to our sample's post injury cognitive functioning. We could not find a validated measurement of cognitive functioning to Swahili and Tanzania, which would be a full project on its own. Our sample was enrolled with informed consent, therefore requiring decision making capacity and cognitive functioning. While for some patients we used legal authorized representative's consent, those patients ultimately regained capacity to consent as determined by their healthcare provider and were enrolled. Therefore, our sample represents mostly mild injury patients (Table 1). But, this pattern is also representative of those who survive an injury in a limited resource setting, as well as those who would be most likely to have persistent harmful alcohol use behavior (Staton et al., 2017).
In conclusion, this article presents the first validation of Swahili versions of AUDIT and CAGE for TBI patients in Tanzania. These instruments provide clinicians, researchers and public health officials with a rigorously validated tool to evaluate the prevalence of alcohol misuse in Tanzania and measure its effects on health outcomes. Such data could help drive evidence-based interventions to reduce alcohol-related morbidity and mortality and shape policy. Additional research is needed to validate the AUDIT and CAGE tools in a wider Tanzanian population as well as to establish specific cutoff values for defining alcohol misuse for both instruments in Tanzania. Although this study addressed the need for Swahili versions of AUDIT and CAGE in Tanzania, there are many other languages and communities in which validated versions of these questionnaires are still lacking. Clearly, more research is needed to develop validated translations of these tools in other languages and in other settings across sub-Saharan Africa.
FUNDING
This project was made possible by the Mentored Research Training Program in collaboration with the HRSA-funded KCMC MEPI grant # T84HA21123-02; U.S. National Institutes of Health and the Duke Division of Emergency Medicine. Dr Staton would like to acknowledge salary support provided by the Fogarty International Center of the National Institutes of Health under Award Number K01TW010000 (PI, Staton).
CONFLICT OF INTEREST STATEMENT
None declared.
AUTHOR CONTRIBUTIONS
J.R.N.V. and C.A.S. thought of the scientific basis and rationale for this project. J.R.N.V., J.H. and D.E. were responsible for the writing, literature review and article preparation. C.A.S. and M.M. supervised the manuscript preparation. B.T.M. and M.M. were responsible for data collection. J.R.N.V., J.R.A., L.P.O. and J.F.C. contributed to the data analysis interpretation of the results. All authors critically reviewed the contents and approved the final version of the article.
ACKNOWLEDGMENTS
We would like to acknowledge our KCMC/Duke ED Research Team without whom none of our research would be possible.
REFERENCES
- Adewuya AO. (2005) Validation of the alcohol use disorders identification test (audit) as a screening tool for alcohol-related problems among Nigerian university students. Alcohol Alcohol 40:575–7. [DOI] [PubMed] [Google Scholar]
- Alem A, Kebede D, Kullgren G (1999) The epidemiology of problem drinking in Butajira, Ethiopia. Acta Psychiatr Scand Suppl 397:77–83. [DOI] [PubMed] [Google Scholar]
- AlMarri TS, Oei TP, Amir T (2009) Validation of the alcohol use identification test in a prison sample living in the Arabian Gulf region. Subst Use Misuse 44:2001–13. [DOI] [PubMed] [Google Scholar]
- Alvarado ME, Garmendia ML, Acuna G, et al. (2009) [Assessment of the alcohol use disorders identification test (AUDIT) to detect problem drinkers]. Rev Med Chil 137:1463–8. [PubMed] [Google Scholar]
- Ao TT, Sam N, Kiwelu I, et al. (2011) Risk factors of alcohol problem drinking among female bar/hotel workers in Moshi, Tanzania: a multi-level analysis. AIDS Behav 15:330–9. [DOI] [PubMed] [Google Scholar]
- Babor T, Higgins-Biddle J, Saunders J, et al. (2001) AUDIT the Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Care, 2nd edn Geneva: World Health Organization. [Google Scholar]
- Bergman H, Kallmen H (2002) Alcohol use among Swedes and a psychometric evaluation of the alcohol use disorders identification test. Alcohol Alcohol 37:245–51. [DOI] [PubMed] [Google Scholar]
- Bruns J Jr, Hauser WA (2003) The epidemiology of traumatic brain injury: a review. Epilepsia 44:2–10. [DOI] [PubMed] [Google Scholar]
- Bryce S, Spitz G, Ponsford J (2015) Screening for substance use disorders following traumatic brain injury: examining the validity of the AUDIT and the DAST. J Head Trauma Rehabi 30:E40–8. [DOI] [PubMed] [Google Scholar]
- Carey K, Carey M, Chandra P (2003) Psychometric evaluation of the Alcohol Use Disorders Identification Test and short Drug Abuse Screening Test with psychiatric patients in India. J Clin Psychiatry 64:767–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chishinga N, Kinyanda E, Weiss HA, et al. (2011) Validation of brief screening tools for depressive and alcohol use disorders among TB and HIV patients in primary care in Zambia. BMC Psychiatry 11:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Claassen JN. (1999) The benefits of the CAGE as a screening tool for alcoholism in a closed rural South African community. S Afr Med J 89:976–9. [PubMed] [Google Scholar]
- Cook T, Woodall N, Harper J, et al. Fourth National Audit Project (2011) Major complications of airway management in the UK: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 2: intensive care and emergency departments. Br J Anaesth 106:632–42. [DOI] [PubMed] [Google Scholar]
- Cremonte M, Ledesma R, Cherpitel C, et al. (2010) Psychometric properties of alcohol screening tests in the emergency department in Argentina, Mexico and the United States. Addict Behav 35:818–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Meneses-Gaya C, Zuardi A, Loureiro S, et al. (2009) Alcohol Use Disorders Identification Test (AUDIT): an updated systematic review of psychometric properties. Psychology & Neuroscience [Online], 2:83–97. [Google Scholar]
- de Torres LA, Rebollo EM, Ruiz-Moral R, et al. (2009) Diagnostic usefulness of the Alcohol Use Disorders Identification Test (AUDIT) questionnaire for the detection of hazardous drinking and dependence on alcohol among Spanish patients. Eur J Gen Pract 15:15–21. [DOI] [PubMed] [Google Scholar]
- Devellis R. (2003) Scale Development: Theory and Applications. Thousand Oaks, CA: Sage. [Google Scholar]
- Doyle S, Donovan D, Kivlahan D (2007) The factor structure of the alcohol use disorders 14 identification test (AUDIT). J Stud Alcohol Drugs 68:474–9. [DOI] [PubMed] [Google Scholar]
- Dybek I, Bischof G, Grothues J, et al. (2006) The reliability and validity of the Alcohol Use Disorders Identification Test (AUDIT) in a German general practice population sample. J Stud Alcohol 67:473–81. [DOI] [PubMed] [Google Scholar]
- English C, Rey JA, Schlesselman LS (2011) Prevalence of hazardous alcohol use among pharmacy students at nine U.S. schools of pharmacy. Pharm Pract (Granada)9:162–8. [PMC free article] [PubMed] [Google Scholar]
- Erkut S. (2010) Developing Multiple Language Versions of Instruments for Intercultural Research. Child Dev Perspect 4:19–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ewing JA. (1984) Detecting alcoholism. The CAGE questionnaire. Jama 252:1905–7. [DOI] [PubMed] [Google Scholar]
- Fekadu A, Medhin G, Selamu M, et al. (2016) Non-fatal suicidal behaviour in rural Ethiopia: a cross-sectional facility- and population-based study. BMC Psychiatry 16:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferreira-Borges C, Rehm J, Dias S, et al. (2016) The impact of alcohol consumption on African people in 2012: an analysis of burden of disease. Trop Med Int Health 21:52–60. [DOI] [PubMed] [Google Scholar]
- Fleminger S, Ponsford J (2005) Long term outcome after traumatic brain injury. BMJ 331:1419–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francis J, Grosskurth H, Changalucha J, et al. (2014) Systematic review and meta-analysis: prevalence of alcohol use among young people in eastern Africa. Trop Med Int Health 19:476–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francis JM, Weiss HA, Mshana G, et al. (2015) The epidemiology of alcohol use and alcohol use disorders among young people in northern Tanzania. PLoS One 10:e0140041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gache P, Michaud P, Landry U, et al. (2005) The Alcohol Use Disorders Identification Test (AUDIT) as a screening tool for excessive drinking in primary care: reliability and validity of a French version. Alcohol Clin Exp Res 29:2001–7. [DOI] [PubMed] [Google Scholar]
- Ghebremichael M, Paintsil E, Larsen U (2009) Alcohol abuse, sexual risk behaviors, and sexually transmitted infections in women in Moshi urban district, northern Tanzania. Sex Transm Dis 36:102–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hair J, Black W, Babin B, et al. (2005) Multivariate Data Analysis. New Jersey: Pearson Educational. [Google Scholar]
- Hernandez-Nieto R. (2002) Contributions to Statistical Analysis. Merida: Universidad de Los Andes. [Google Scholar]
- Hu L, Bentler P (1999) Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling 6:1–5. [Google Scholar]
- Hyder A, Wunderlich C, Puvanachandra P, et al. (2007) The impact of traumatic brain injuries: a global perspective. Neurorehabilitation 22:341–53. [PubMed] [Google Scholar]
- Kallmen H, Wennberg P, Ramstedt M, et al. (2014) The psychometric properties of the AUDIT: a survey from a random sample of elderly Swedish adults. BMC Public Health 14:672, 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanyoni M, Gishoma D, Ndahindwa V (2015) Prevalence of psychoactive substance use among youth in Rwanda. BMC Res Notes 8:190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawada T, Inagaki H, Kuratomi Y (2011) The alcohol use disorders identification test: reliability study of the Japanese version. Alcohol 45:205–7. [DOI] [PubMed] [Google Scholar]
- Kebede D, Alem A (1999) The epidemiology of alcohol dependence and problem drinking in Addis Ababa, Ethiopia. Acta Psychiatr Scand Suppl 397:30–4. [DOI] [PubMed] [Google Scholar]
- Kim J, Oh M, Park B, et al. (1999) Screening criteria of alcoholism by alcohol use disorders identification test (AUDIT) in Korea. J Korean Acad Fam Med 20:1152–9. [Google Scholar]
- Kline R. (2012) Principles and Practice of Structural Equation Modeling. New York: The Guilford Press. [Google Scholar]
- Kuder G, Richardson M (1937) The theory of the estimation of test reliability. Psychometrika 2:151–60. [Google Scholar]
- Kullgren G, Alibusa S, Birabwa-Oketcho H (2009) Problem drinking among patients attending primary healthcare units in Kampala, Uganda. Afr J Psychiatry (Johannesbg) 12:52–8. [DOI] [PubMed] [Google Scholar]
- Lancaster KE, Go VF, Lungu T, et al. (2016) Substance use and HIV infection awareness among HIV-infected female sex workers in Lilongwe, Malawi. Int J Drug Policy 30:124–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung SF, Arthur D (2000) The alcohol use disorders identification test (AUDIT): validation of an instrument for enhancing nursing practice in Hong Kong. Int J Nurs Stud 37:57–64. [DOI] [PubMed] [Google Scholar]
- Lhachimi SK, Nusselder WJ, Smit HA, et al. (2016) Potential health gains and health losses in eleven EU countries attainable through feasible prevalences of the life-style related risk factors alcohol, BMI, and smoking: a quantitative health impact assessment. BMC Public Health 16:734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meneses-Gaya C, Zuardi AW, Loureiro SR, et al. (2010) Is the full version of the AUDIT really necessary? Study of the validity and internal construct of its abbreviated versions. Alcohol Clin Exp Res 34:1417–24. [DOI] [PubMed] [Google Scholar]
- Mitsunaga T, Larsen U (2008) Prevalence of and risk factors associated with alcohol abuse in Moshi, northern Tanzania. J Biosoc Sci 40:379–99. [DOI] [PubMed] [Google Scholar]
- Molina PE, Katz PS, Souza-Smith F, et al. (2015) Alcohol's burden on immunity following burn, hemorrhagic shock, or traumatic brain injury. Alcohol Res 37:263–78. [PMC free article] [PubMed] [Google Scholar]
- Mongi AS, Baisley K, Ao TT, et al. (2013) Factors associated with problem drinking among women employed in food and recreational facilities in northern Tanzania. PLoS One 8:e84447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moretti-Pires RO, Corradi-Webster CM (2011) [Adaptation and validation of the Alcohol Use Disorders Identification Test (AUDIT) for a river population in the Brazilian Amazon]. Cad Saude Publica 27:497–509. [DOI] [PubMed] [Google Scholar]
- Myer L, Smit J, Roux LL, et al. (2008) Common mental disorders among HIV-infected individuals in South Africa: prevalence, predictors, and validation of brief psychiatric rating scales. AIDS Patient Care STDS 22:147–58. [DOI] [PubMed] [Google Scholar]
- Nadkarni A, Weiss HA, Naik A, et al. (2016) The six-year outcome of alcohol use disorders in men: a population based study from India. Drug Alcohol Depend 162:107–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Namagembe I, Jackson LW, Zullo MD, et al. (2010) Consumption of alcoholic beverages among pregnant urban Ugandan women. Matern Child Health J 14:492–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nayak M, Bond J, Greenfield T (2015) Evaluating shortened versions of the AUDIT as screeners for alcohol use problems in a general population study. Subst Use Misuse 50:1579–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogeil RP, Gao CX, Rehm J, et al. (2016) Temporal changes in alcohol-related mortality and morbidity in Australia. Addiction 111:626–34. [DOI] [PubMed] [Google Scholar]
- Okulate GT, Odunaike A (2005) Alcohol use and abuse among medical and surgical in-patients in a general hospital. Niger Postgrad Med J 12:77–80. [PubMed] [Google Scholar]
- Opio CK, Seremba E, Ocama P, et al. (2013) Diagnosis of alcohol misuse and alcoholic liver disease among patients in the medical emergency admission service of a large urban hospital in Sub-Saharan Africa; a cross sectional study. Pan Afr Med J 15:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padilla MA, Divers J (2016) A comparison of composite reliability estimators: coefficient omega confidence intervals in the current literature. Educ Psychol Meas 76:436–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pal HR, Jena R, Yadav D (2004) Validation of the Alcohol Use Disorders Identification Test (AUDIT) in urban community outreach and de-addiction center samples in north India. J Stud Alcohol 65:794–800. [DOI] [PubMed] [Google Scholar]
- Peltzer K, Davids A, Njuho P (2011) Alcohol use and problem drinking in South Africa: findings from a national population-based survey. Afr J Psychiatry (Johannesbg) 14:30–7. [DOI] [PubMed] [Google Scholar]
- Pengpid S, Peltzer K, Van Der Heever H (2011) Prevalence of alcohol use and associated factors in urban hospital outpatients in South Africa. Int J Environ Res Public Health 8:2629–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Popova S, Lange S, Burd L, et al. (2016) The economic burden of fetal alcohol spectrum disorder in Canada in 2013. Alcohol Alcohol 51:367–75. [DOI] [PubMed] [Google Scholar]
- Pradhan B, Chappuis F, Baral D, et al. (2012) The alcohol use disorders identification test (AUDIT): validation of a Nepali version for the detection of alcohol use disorders and hazardous drinking in medical settings. Subst Abuse Treat Prev Policy 7:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Praud D, Rota M, Rehm J, et al. (2016) Cancer incidence and mortality attributable to alcohol consumption. Int J Cancer 138:1380–7. [DOI] [PubMed] [Google Scholar]
- Rist F, Glockner-Rist A, Demmel R (2009) The Alcohol Use Disorders Identification Test revisited: establishing its structure using nonlinear factor analysis and identifying subgroups of respondents using latent class factor analysis. Drug Alcohol Depend 100:71–82. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, et al. (1993) Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on early detection of persons with harmful alcohol consumption—II. Addiction 88:791–804. [DOI] [PubMed] [Google Scholar]
- Schultheis M, Whipple E (2014) Driving after traumatic brain injury: evaluation and rehabilitation interventions. Curr Phys Med Rehabil Rep 2:176–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwitters A, Sabatier J, Seth P, et al. (2015) HIV and alcohol knowledge, self-perceived risk for HIV, and risky sexual behavior among young HIV-negative men identified as harmful or hazardous drinkers in Katutura, Namibia. BMC Public Health 15:1182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seth P, Glenshaw M, Sabatier JH, et al. (2015) AUDIT, AUDIT-C, and AUDIT-3: drinking patterns and screening for harmful, hazardous and dependent drinking in Katutura, Namibia. PLoS One 10:e0120850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegfried N, Parry CD, Morojele NK, et al. (2001) Profile of drinking behaviour and comparison of self-report with the CAGE questionnaire and carbohydrate-deficient transferrin in a rural Lesotho community. Alcohol Alcohol 36:243–8. [DOI] [PubMed] [Google Scholar]
- Soboka M, Tesfaye M, Feyissa GT, et al. (2014) Alcohol use disorders and associated factors among people living with HIV who are attending services in south west Ethiopia. BMC Res Notes 7:828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- So K, Sung E (2013) A validation study of the brief Alcohol Use Disorder Identification Test (AUDIT): a brief screening tool derived from the AUDIT. Korean J Fam Med 34:11–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staton C, Msilanga D, Kiwango G, et al. (2017) A prospective registry evaluating the epidemiology and clinical care of traumatic brain injury patients presenting to a regional referral hospital in Moshi, Tanzania: challenges and the way forward. Int J Inj Contr Saf Promot 24:69–77. [DOI] [PubMed] [Google Scholar]
- Thakarar K, Asiimwe SB, Cheng DM, et al. (2016) Alcohol consumption in Ugandan HIV-infected household-brewers versus non-brewers. AIDS Behav 20:2408–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuliao A, Landoy B, Mcchargue D (2016) Factor structure and invariance test of the alcohol use disorder identification test (AUDIT): comparison and further validation in a US and Philippines college student sample. J Ethn Subst Abuse 15:127–43. [DOI] [PubMed] [Google Scholar]
- Unsworth D, Mathias J (2017) Traumatic brain injury and alcohol/substance abuse: a Bayesian meta-analysis comparing the outcomes of people with and without a history of abuse. J Clin Exp Neuropsychol 39:547–62. [DOI] [PubMed] [Google Scholar]
- Vissoci J, Meier B, Staton C (2016) Effect of Pre-morbid Mental Health Conditions on Traumatic Brain Injury Clinical Outcomes. Moshi, Tanzania: Kilimanjaro Christian Medical Center. [Google Scholar]
- Von Der Pahlen B, Santtila P, Witting K, et al. (2008) Factor structure of the Alcohol Use Disorders Identification Test (AUDIT) for men and women in different age groups. J Stud Alcohol Drugs 69:616–21. [DOI] [PubMed] [Google Scholar]
- von Steinbuechel N, Covic A, Polinder S, et al. (2016) Assessment of Health-Related Quality of Life after TBI: comparison of a Disease-Specific (QOLIBRI) with a Generic (SF-36) Instrument. Behav Neurol. 1–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wandera B, Tumwesigye NM, Nankabirwa JI, et al. (2015) Alcohol consumption among HIV-infected persons in a large urban HIV clinic in Kampala Uganda: a constellation of harmful behaviors. PLoS One 10:e0126236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss HA, Vandepitte J, Bukenya JN, et al. (2016) High levels of persistent problem drinking in women at high risk for HIV in Kampala, Uganda: a prospective cohort study. Int J Environ Res Public Health 13:153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- What is a standard drink? (2017, August 15). https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/what-standard-drink. [Google Scholar]
- Whiteford HA, Degenhardt L, Rehm J, et al. (2013) Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet 382:1575–86. [DOI] [PubMed] [Google Scholar]
- World Health Organization (2017) Process of translation and adaptation of instruments [online]. http://www.who.int/substance_abuse/research_tools/translation/en/ (22 September 2017, date last accessed).
- Wu SI, Huang HC, Liu SI (2008) Validation and comparison of alcohol-screening instruments for identifying hazardous drinking in hospitalized patients in Taiwan. Alcohol Alcohol 43:577–82. [DOI] [PubMed] [Google Scholar]
- Young C, Mayson T (2010) The Alcohol Use Disorders Identification Scale (AUDIT) normative scores for a multiracial sample of Rhodes University residence students. J Child Adolesc Ment Health 22:15–23. [DOI] [PubMed] [Google Scholar]
- Younossi Z, Henry L (2016) Contribution of alcoholic and nonalcoholic fatty liver disease to the burden of liver-related morbidity and mortality. Gastroenterology 150:1778–85. [DOI] [PubMed] [Google Scholar]
- Zatzick D, Jurkovich G, Gentilello L, et al. (2002) Posttraumatic stress, problem drinking, and functional outcomes after injury. Arch Surg 137:200–5. [DOI] [PubMed] [Google Scholar]
- Zetola NM, Modongo C, Kip EC (2012) Alcohol use and abuse among patients with multidrug-resistant tuberculosis in Botswana. Int J Tuberc Lung Dis 16:1529–34. [DOI] [PMC free article] [PubMed] [Google Scholar]