Pemphigoid nodularis (PN) is a rare variant of bullous pemphigoid (BP), manifesting with clinical features of prurigo nodularis with an autoantibody profile of BP.1 Psoralen ultraviolet A (PUVA) can induce blister formation acrally and in areas with friction or trauma.2 While this is generally distinct from BP,3 these blisters represent the initial manifestation of BP in some patients, and are thus considered PUVA-induced BP.4
A 73-year-old East Asian man presented with a vesiculobullous eruption following four treatments of oral PUVA for recalcitrant pruritus with prurigo nodules. Other than prurigo nodules and excoriations, the patient originally lacked other cutaneous manifestations. The initial cause of the patient’s pruritus was unclear. He had previously been prophylactically treated with permethrin, topical corticosteroids, pramoxine and gabapentin with little improvement. The patient’s other medications included amlodipine, aspirin, atorvastatin, apixaban, escitalopram and metoprolol. He had not had a biopsy taken prior to the start of his PUVA treatment and basic laboratory investigations at the time were unremarkable.
On physical examination, the patient was found to have prurigo nodules and excoriations (Fig. 1), along with numerous coalescing vesicles and tense bullae on his hands, trunk and thighs.
Figure 1.

Scattered excoriated prurigo nodules with an absence of typical bullous or urticarial lesions of bullous pemphigoid.
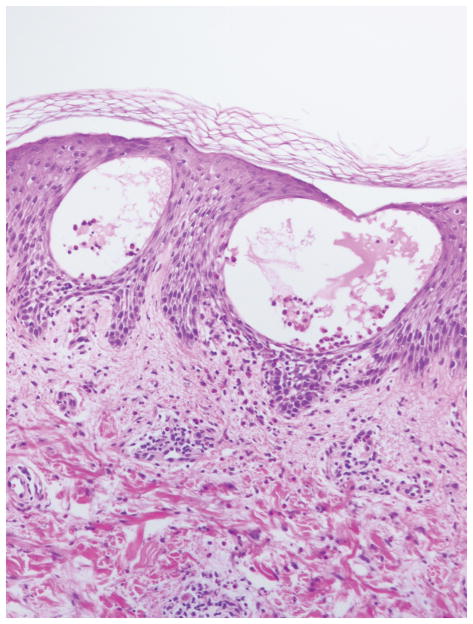
Histological examination of a biopsy taken from an intact vesicle demonstrated vesicular spongiotic dermatitis with numerous eosinophils (Fig. 2).
Figure 2.
Biopsy of an intact vesicle demonstrating spongiosis with vesicle formation, and a perivascular infiltrate of lymphocytes admixed with eosinophils 10x.
Indirect immunofluorescence demonstrated linear staining for IgG along the basement membrane zone (BMZ) at a titre of 1 : 40 960 on monkey oesophagus, and an epidermal staining pattern on salt-split skin at a dilution of 1 : 5120. ELISA results for IgG to BP180 and BP230 were 114 and 59 ELISA units/mL, respectively, with a reference range of 9 ELISA units/mL for both tests.
Therefore, a diagnosis of PN was made. The patient was successfully treated with a combination of a slow prednisone taper, intravenous IgG 2 g/kg/month, minocycline 100 mg twice daily, niacinamide 500 mg three times daily, and mycophenolate mofetil 1 g twice daily, as is standard in our immunobullous clinic to achieve durable remissions. The patient was successfully weaned off prednisone, and his other medications were continued.
PN is a rare variant of BP. Although patients demonstrate an immunological phenotype of BP, some do not develop blisters. Similar nonbullous phenomena occur in patients with significant levels of BP antibodies in other pruritic disorders of the elderly, and PN is thus considered by some to represent a preclinical form of BP.5 Histopathology of PN is not always suggestive of BP, owing to an absence of eosinophils in many cases.6 However, the characteristic immunofluorescence of BP is always present. The cutaneous lesions of PN and the associated pruritus are often recalcitrant to high-potency topical corticosteroids, necessitating treatment with oral corticosteroids and steroid-sparing immunosuppressants.1
PUVA-induced blistering can be divided into two types: PUVA-induced acrobullous dermatosis and PUVA-induced BP.3 These can be differentiated histologically, as PUVA-induced acrobullous dermatosis is characterized by intracellular oedema and vacuolization with destruction of keratinocytes. ‘Sunburn cells’ are also seen. These findings are in contrast to the traditional eosinophilic spongiosis seen in PUVA-induced BP.2 PUVA-induced acrobullous dermatosis can also exhibit junctional C3 deposition, but it lacks the characteristic IgG deposition of BP.
In conclusion, we describe a case of PUVA-aggravated PN, a previously undescribed combination of two rare entities in immunobullous disease: PN and PUVA-induced BP. It is possible that the PUVA facilitated an advance of the patient’s disease from a nodular to a vesiculobullous stage. While the possibility cannot be excluded that the patient did not in fact have idiopathic PN with the subsequent development of PUVA-induced BP, his robust anti-BMZ titre, the acute development of the bullae with PUVA and the resolution of prurigo nodules following treatment for BP make this highly unlikely. Thus, PN should be suspected in patients with recalcitrant prurigo nodularis and in those developing blistering during PUVA treatment. Likewise, PN should be excluded prior to treatment with PUVA for prurigo.
Footnotes
Conflict of interest: the authors declare that they have no conflicts of interest.
References
- 1.Cliff S, Holden CA. Pemphigoid nodularis: a report of three cases and review of the literature. Br J Dermatol. 1997;136:398–401. [PubMed] [Google Scholar]
- 2.Friedmann PS, Coburn P, Dahl MG, et al. PUVA-induced blisters, complement deposition, and damage to the dermoepidermal junction. Arch Dermatol. 1987;123:1471–7. [PubMed] [Google Scholar]
- 3.Robinson JK, Baughman RD, Provost TT. Bullous pemphigoid induced by PUVA therapy. Is this the aetiology of the acral bullae produced during PUVA treatment? Br J Dermatol. 1978;99:709–13. doi: 10.1111/j.1365-2133.1978.tb07067.x. [DOI] [PubMed] [Google Scholar]
- 4.George PM. Bullous pemphigoid possibly induced by psoralen plus ultraviolet A therapy. Photodermatol Photoimmunol Photomed. 1996;11:185–7. doi: 10.1111/j.1600-0781.1995.tb00166.x. [DOI] [PubMed] [Google Scholar]
- 5.Schmidt T, Sitaru C, Amber K, et al. BP180- and BP230-specific IgG autoantibodies in pruritic disorders of the elderly: a preclinical stage of bullous pemphigoid? Br J Dermatol. 2014;171:212–19. doi: 10.1111/bjd.12936. [DOI] [PubMed] [Google Scholar]
- 6.Powell AM, Albert S, Gratian MJ, et al. Pemphigoid nodularis (non-bullous): a clinicopathological study of five cases. Br J Dermatol. 2002;147:343–9. doi: 10.1046/j.1365-2133.2002.04754.x. [DOI] [PubMed] [Google Scholar]