Abstract
Acetabular bone cyst is usually associated with dysplastic secondary osteoarthritis of the hip joint. Acetabular reorientation osteotomy is one of the most common therapeutic options for treating patients with hip dysplasia. However, it may be too invasive for athletes and can also lead to some complications including intraoperative fracture and postoperative bone necrosis especially in patients with acetabular large bone cysts. Endoscopic shelf acetabuloplasty offers a less invasive option for athletic patients with dysplasia of severity greater than those indicated for isolated hip arthroscopy. This Technical Note demonstrates endoscopic shelf acetabuloplasty with bone grafting, simultaneously addressing a large bone cyst and acetabular undercoverage, as part of a comprehensive approach addressing chondrolabral pathology while restoring capsular integrity in an athlete with moderate dysplasia.
Developmental dysplasia of the hip (DDH) is the most common cause of secondary osteoarthritis (OA) of the hip in the Asian population.1, 2 The pathomechanism involves increased stress loading of the hypovolemic socket at the acetabular rim with chondrolabral damage and subsequent OA.3, 4
High-impact athletic activities have been associated with hip OA. Vigdorchik et al.,5 in a systematic review, reported that male athletes participating in elite high-impact sports are at an increased risk of developing hip OA. In our practice, we often see young athletes with OA of the dysplastic hip.
Current surgical interventions for symptomatic hip dysplasia include reorientation osteotomies (e.g., periacetabular osteotomy [PAO] or rotational acetabular osteotomy [RAO]) and hip arthroscopy. The reorientation osteotomies have been successful6, 7 but are associated with some major complications including but not limited to intra-articular fracture and acetabular osteonecrosis.8, 9 Hip arthroscopy's role in dysplasia, while evolving, appears to yield encouraging outcomes approaching those for femoroacetabular impingement when limited to borderline or mild dysplasia and with less risk than PAO or RAO.
In the athletic patient population, PAO or RAO may compromise return to sport as the open surgeries involve significant muscle dissection with commensurately long postoperative rehabilitation. Hip arthroscopy is an attractive less invasive alternative, but many athletes may have dysplasia of greater severity than is currently shown to have successful arthroscopic outcomes.
Endoscopic shelf acetabuloplasty may address the intra-articular chondrolabral pathology, associated cam femoroacetabular impingement, and anterolateral acetabular undercoverage. Shelf acetabuloplasty can theoretically decrease edge loading by increased bony support of the anterosuperior aspect of the shallow acetabulum for treating patients with DDH.10 Uchida et al.11 have developed a comprehensive endoscopic approach including labral repair, cam osteoplasty, capsular plication, and shelf acetabuloplasty. In a series of 32 active patients, endoscopic shelf acetabuloplasty provided promising clinical outcomes and a high rate of return to play sports-related activities.12
Acetabular cysts often accompany dysplasia,13 typically involving the anterolateral rim, and are often quite large. Bone cysts may be treated with bone grafting from various sources (autograft, allograft, orthobiologic). Small anterolateral rim cysts may be removed via rim trimming, but this is not a viable option in the already shallow dysplastic socket. We present a hip arthroscopic technique including the application of endoscopic shelf acetabuloplasty to provide autologous bone grafting of the cyst and concurrent osseous support at the deficient anterolateral rim.
Indications
Basically, indications for this procedure are the same as those of Uchida et al.11's report on endoscopic shelf acetabuloplasty (Table 1). The investigators noted that this procedure is not indicated for OA. However, this technique may potentially apply for OA cases (Tönnis grade 2) with cysts limited to the anterior acetabulum (Table 1).
Table 1.
Surgical Indications and Contraindications
| Indications | Contraindications |
|---|---|
| Mild to moderate dysplasia (lateral center-edge angle >5° but <20° and vertical center anterior angle >5°but <20°) with cysts at anterior acetabulum No evidence of severe chondral damage |
Presence of severe acetabular shallowness (lateral center-edge angle <5° and vertical center anterior <5°) Dysplasia with additional severe femoral deformities Severe chondral damage Osteoarthritis (greater than Tönnis grade 2) except for cysts at anterior acetabulum (detected by preoperative computed tomography) Skeletally immature patients (age <12 years) |
Preoperative Evaluation and Radiographic Imaging
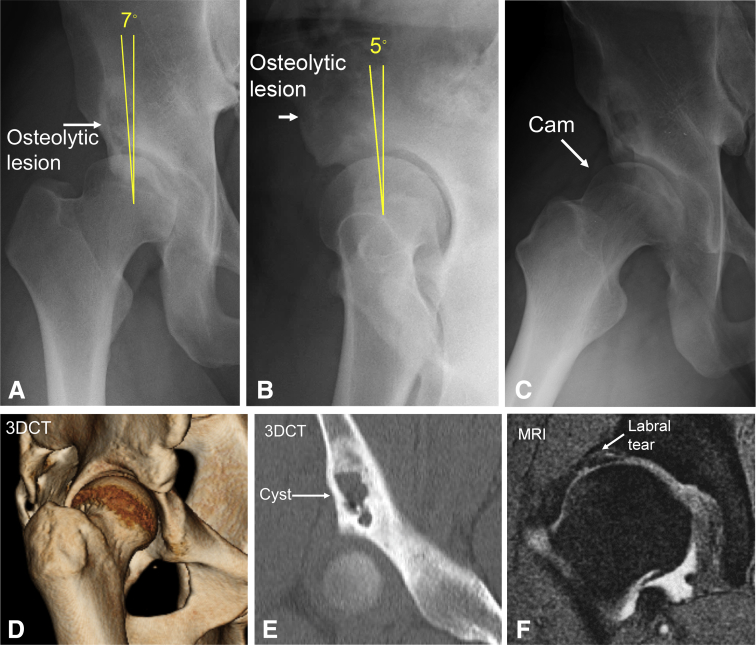
Commonly, the patient complains of hip pain associated with limitation in range of motion. Lateral center edge angle (LCEA) and vertical center anterior (VCA) angle should be measured on the anteroposterior (AP) pelvis (Fig 1A) and false profile view (Fig 1B), respectively. An AP pelvic radiograph will confirm lateral acetabular shallowness (Fig 1A). A round osteolytic lesion will be identified at the superior acetabulum (Fig 1A). A modified Dunn view can show cam morphology (Fig 1C). A false profile view will show large osteolytic lesion at anterior-superior acetabulum and anterior acetabular deficiency (Fig 1B). A 3-dimensional computed tomography (3DCT) will show insufficient lateral and anterior coverage of acetabulum (Fig 1D), and a coronal view will demonstrate a large bone cyst at the anterosuperior acetabulum (Fig 1E). A T2 weighted coronal view on magnetic resonance imaging will reveal a high-intensity area in the anterosuperior labrum (Fig 1F).
Fig 1.
(A) Preoperative anteroposterior radiograph of a right hip showing dysplastic acetabulum and a round shaped osteolytic lesion at superior acetabulum. The lateral center-edge angle is 7°, and the sharp angle was 40°. (B) Preoperative modified Dunn view of a right hip showing cam lesion. The alpha angle is 73°, and the offset ratio is 0.09. (C) Preoperative false profile view of a right hip showing anterior acetabular shallowness. The vertical center anterior angle is 5°. (D) Three-dimensional computed tomography of a right hip showing insufficient coverage of acetabulum. (E) A coronal view of computed tomography showing a large cyst at anterior-superior acetabulum. (F) T2-weighted coronal view of magnetic resonance image after arthrography showing torn anterosuperior labrum.
Surgical Technique
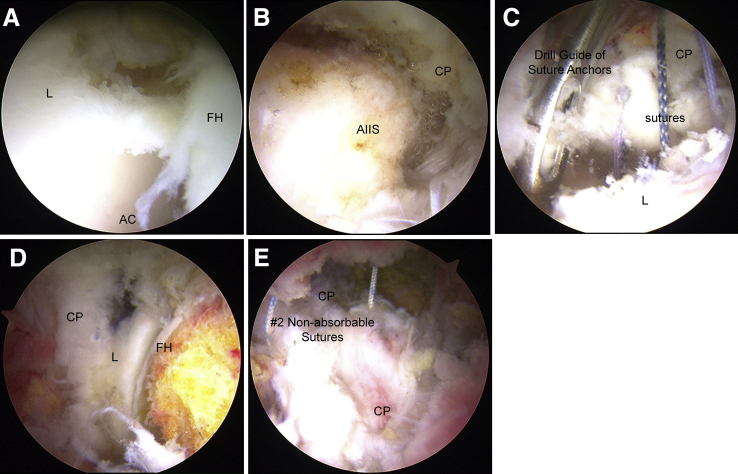
Supine hip arthroscopy is performed on a traction table under general anesthesia. Anterolateral portal, midanterior portal, and proximal mid-anterior portal are established. After traction is applied, a 70° arthroscope is introduced through the anterolateral portal. After interportal capsulotomy, intra-articular evaluation is performed. Delamination of the chondrolabral complex is observed at the anterosuperior aspect of the acetabulum adjacent to the large acetabular bone cyst (Fig 2A). A prominent AIIS is observed adjacent to a torn anterosuperior labrum (Fig 2B). Subspine decompression is performed using a motorized round burr (Smith and Nephew, Andover, MA). Conservative osteoplasty is done to preserve the bone cyst. Labral fixation with suture anchors (Gryphon BR anchor, DePuy Synthes, Raynham, MA; Osteoraptor anchor, Smith and Nephew) is performed (Fig 2C). After releasing the traction and confirming perimetric labral fluid seal, peripheral compartment arthroscopy and cam osteoplasty are performed without incident (Fig 2D). Capsular plication with 5 no. 2 nonabsorbable sutures (Fiberwire; Arthrex, North Naples, FL) is then performed (Fig 2E).
Fig 2.
(A) Arthroscopic findings from anterolateral portal on a right hip showing complete labral tear and acetabular labral-chondral delamination. (B) Arthroscopic view from anterolateral portal on a right hip showing AIIS protrusion. (C) Arthroscopic view from anterolateral portal on a right hip showing that labrum is repaired with suture anchors. (D) Peripheral compartment view from anterolateral portal on a right hip showing cam osteochondroplasty. (E) Endoscopic extra-articular view on a right hip showing capsular plication with strong sutures. (AC, acetabulum; AIIS, anterior inferior iliac spine; CP, capsule; FH, femoral head; L, labrum.)
After complete capsular closure, the 30° arthroscope is positioned into the extracapsular space under the AP fluoroscopic guidance. Arthroscopic debridement using a motorized shaver (Smith and Nephew) and radiofrequency ablator (Ambient Hipvac 50, Smith and Nephew) enables good visualization and a secure working space for shelf acetabuloplasty.
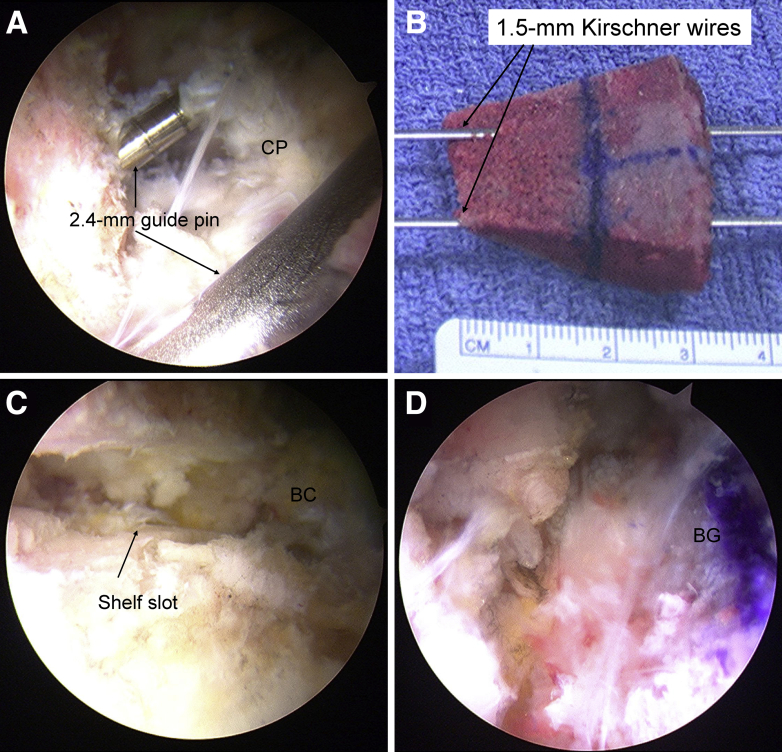
Three parallel 2.4-mm guide wires are introduced using a drill guide through the midanterior portal, along the anterosuperior acetabular rim adjacent to the capsule (Fig 3A). The transverse slot is enlarged with the use of a 10-mm wide osteotome to measure approximately 5 to 6 mm in height and 25 mm in width.
Fig 3.
(A) An arthroscopic view from the anterolateral portal at the extra-articular space on a right hip shows that 2.4-mm guide pins are introduced along the anterior capsule. (B) Free bone graft is harvested from ipsilateral iliac crest, and 2 parallel 1.5-mm Kirschner wires are inserted. (C) An endoscopic finding on a right hip shows that optimum sized shelf slot is made, and bone cyst in the anterior acetabulum is identified at the back of the slot. (D) The autologous bone graft is inserted into the slot through the guide wires with press-fit fixation. (BC, bone cyst; BG, bone graft; CP, capsule.)
Autologous tricortical bone graft is harvested from the ipsilateral iliac crest (Fig 3B). Two 1.5-mm Kirshner wires are introduced in 1.8-mm diameter drill holes, helping to control the graft position during endoscopic insertion into the aforementioned anterosuperior peri-acetabular slot (Fig 3B).
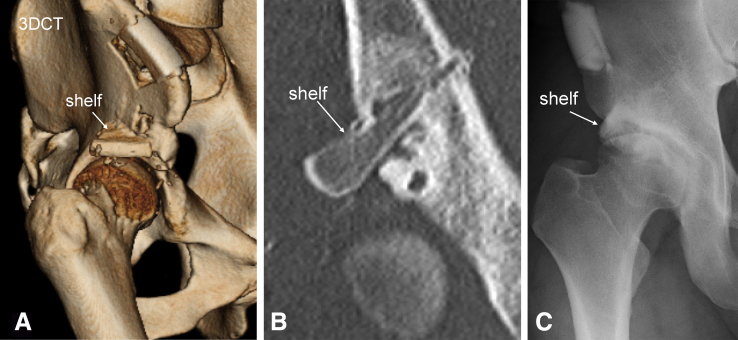
Bone cyst is found in the transverse slot in the acetabulum with the scope. A vertical slot is made to remove the cystic contents (Fig 3C). Corticocancellous bone chips are packed into the cyst cavity. The free autologous bone graft is then secured into the transverse slot (Fig 3D) using the parallel skewer wires (Fig 3B) and secured into position via press fit using a cannulated bone tamp (Meira, Nagoya, Japan).14 Subsequently, several bone wedges are tamped into the vertical slot and cancellous bone chips are placed above the new shelf with a custom-made cannula.14 An example illustrating postoperative pelvic AP radiograph shows proper partial resorption and good remodeling of the shelf graft and elimination of the large bone cyst (Fig 4C; Video 1 with narration).
Fig 4.
Postoperatively, (A) 3-dimensional computed tomography shows enough coverage of acetabulum, (B) a large bone cyst is stuffed with bone grafts on a coronal view of computed tomography, and (C) a pelvic radiograph 3 years after surgery shows good remodeling of shelf graft and bone cyst completely disappears.
Postoperative Management and Rehabilitation Protocol
Initial non-weight-bearing ambulation using dual crutches for 4 weeks is advanced to partial weight-bearing status for another 2 weeks. At 6 postoperative weeks, full weight bearing is permitted.
Postoperative 3DCT shows improved anterosuperior acetabular coverage (Fig 4A), and coronal view shows bone graft incorporation and fill of the bone cyst (Fig 4B).
Discussion
This Technical Note describes an endoscopic autologous bone graft combined with shelf acetabuloplasty for the treatment of DDH with large bone cyst.
Patients with DDH have conventionally undergone acetabular reorientation osteotomies,6, 7 but it has been difficult for athletes with DDH to be candidates for these more invasive procedures because they require return to preinjury level quickly.11 RAO for DDH with giant acetabular bone cysts can also cause catastrophic complications, such as fracture of the acetabulum during or after surgery and bone necrosis after the operation.8, 9 However, our surgical technique can be simultaneously performed for not only the improvement of the acetabular coverage but also the treatment of anterior acetabular bone cysts without severe complications13 (Table 2).
Table 2.
Advantages and Disadvantages
| Advantages | Disadvantages |
|---|---|
| Minimally invasive Fewer severe complications Accessibility to large cysts at anterior acetabulum with the same approach as shelf acetabuloplasty Early rehabilitation Quick recovery |
Technically demanding Possibility of all complications of hip arthroscopic surgery Shelf bone graft fracture Shelf bone graft displacement |
Sabokbar and his colleagues described that increased mechanical stress might cause subchondral acetabular cyst formation and/or enlargement in osteoarthritic hips.14 Hipp et al.15 have shown that joint contact areas were smaller and joint contact pressures were higher in the dysplastic hips compared with the normal hips. We believe that a large acetabular bone cyst in this case healed because the shelf procedure could alleviate the joint contact pressure16 coupled with the effect of local autologous bone grafting.
This surgical technique has several advantages and disadvantages as summarized in Table 2. This entirely endoscopic procedure is especially beneficial to athletes with DDH who must return to sports quickly because it is less invasive and has fewer major complications. The procedure is technically challenging, which is a disadvantage, limiting its use to surgeons with a high level of expertise and experience in hip arthroscopy (Table 2). General complications of hip arthroscopic surgery including traction-related complications such as nerve injury or skin injury may occur (Table 2). Surgical pearls and pitfalls for this technique are detailed in Table 3.
Table 3.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| Preoperative evaluation and planning with computed tomography is indispensable. Use the 30° arthroscope at the time of working in the extracapsular space under the guidance of an image intensifier. Confirming the exact location of shelf graft and acetabular cysts under fluoroscopic visualization is crucial. Bone cyst is identified in the transverse slot with the scope. A vertical slot is useful to remove the cystic contents and stuff corticocancellous bone tips into the cystic cavity. |
Difficulty of treating cysts at posterior acetabulum with the same portal as shelf acetabuloplasty. |
Long-term clinical and radiographic outcomes from multiple cases will be required to substantiate the benefits of this procedure. Until such time, we believe endoscopic shelf acetabuloplasty may offer a less invasive procedure to simultaneously address even large bone cysts in dysplasia while theoretically decreasing edge loading by providing increased albeit focal anterolateral rim bony coverage. When combined with a comprehensive arthroscopic approach addressing concurrent cam femoroacetabular impingement, chondrolabral pathology, and capsular closure, we submit that endoscopic shelf acetabuloplasty may be a viable procedure, particularly in the athletic patient with moderate dysplasia and large acetabular cyst.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: S.U. is a consultant for Smith and Nephew and Zimmer-Biomet and receives research funds from Smith and Nephew, Pfizer, and Johnson and Johnson. This article is unrelated to any funds. The authors report no other conflicts of interest to disclose that may affect the information and recommendations presented in the manuscript. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article. Informed consent has been obtained from the patient. The patient approved the use of her data for the publication of this manuscript.
Supplementary Data
This movie shows a surgical technique for endoscopic shelf acetabuloplasty for treating acetabular large bone cyst in a patient with hip dysplasia. A 23-year-old male professional rugby player presented with a 10-year-history of right hip pain. Physical examination showed limited range of motion and positive impingement sign and dial test. The lateral center edge angle is 7°, and the vertical center anterior angle is 5°, suggesting anterolateral uncoverage of the socket. A round osteolytic lesion is found at the anterosuperior aspect of the right acetabulum. Using a scope view from the anterolateral portal on the right hip, anterosuperior and posterior labral tear and cartilage delamination (MAHORN grade 4) are observed. A prominent AIIS is observed adjacent to a torn anterosuperior labrum. Subspine decompression and tiny rim refreshing are performed using a motorized round burr. Using a scope view from the anterolateral portal on the right hip, anterosuperior labral repair with suture anchor is performed with the lasso loop technique. Using a scope view from the midanterior portal, posteriorsuperior labral refixation is performed. After releasing the traction and confirming labral sealing, peripheral compartment arthroscopy and cam osteoplasty are performed. Complete capsular plication with 5 no. 2 nonabsorbable sutures is then performed. After capsular plication, the 30° arthroscope is positioned into the extracapsular space through the anterolateral portal. Endoscopic soft-tissue debridement enables good visualization and a secure working space for shelf acetabuloplasty. Three parallel 2.4-mm guide wires are introduced using a drill guide through the midanterior portal along the anterosuperior aspect of the acetabular rim adjacent to the capsule. The transverse slot is made with the use of a 10-mm wide osteotome that is introduced along with 3 guide wires. A vertical slot is made using a Kirshner wire and an osteotome to access bone cyst, and then the bone cyst is found through the vertical and transverse slots. The cystic contents are removed by a forceps and shaver. We confirm the optimum width and depth using a custom-made dilator. Corticocancellous bone chips are packed into the bony cyst cavity. A free autologous tricortical bone graft is harvested from the ipsilateral iliac crest. Two 1.5-mm Kirshner wires are introduced, which helps to control the graft position during endoscopic insertion into the transverse slot. The bone graft is then secured into the transverse slot using the parallel skewer wires and secured into position via press fit. Postoperative 3-dimensional computed tomography scan shows enough coverage of the acetabulum, and a large bone cyst is stuffed with bone grafts. Pelvic radiographs show good remodeling of shelf graft, and the bone cyst completely disappears.
References
- 1.Jingushi S., Ohfuji S., Sofue M. Multiinstitutional epidemiological study regarding osteoarthritis of the hip in Japan. J Orthop Sci. 2010;15:626–631. doi: 10.1007/s00776-010-1507-8. [DOI] [PubMed] [Google Scholar]
- 2.Jingushi S., Ohfuji S., Sofue M. Osteoarthritis hip joints in Japan: Involvement of acetabular dysplasia. J Orthop Sci. 2011;16:156–164. doi: 10.1007/s00776-011-0025-7. [DOI] [PubMed] [Google Scholar]
- 3.Mavcic B., Pompe B., Antolic V., Daniel M., Iglic A., Kralj-Iglic V. Mathematical estimation of stress distribution in normal and dysplastic human hips. J Orthop Res. 2002;20:1025–1030. doi: 10.1016/S0736-0266(02)00014-1. [DOI] [PubMed] [Google Scholar]
- 4.Wenger D.R. Is there a role for acetabular dysplasia correction in an asymptomatic patient? J Pediatric Orthop. 2013;33(Suppl 1):S8–12. doi: 10.1097/BPO.0b013e3182771764. [DOI] [PubMed] [Google Scholar]
- 5.Vigdorchik J.M., Nepple J.J., Eftekhary N., Leunig M., Clohisy J.C. What is the association of elite sporting activities with the development of hip osteoarthritis? Am J Sports Med. 2017;45:961–964. doi: 10.1177/0363546516656359. [DOI] [PubMed] [Google Scholar]
- 6.Ganz R., Klaue K., Vinh T.S., Mast J.W. A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop Relat Res. 1988:26–36. [PubMed] [Google Scholar]
- 7.Ninomiya S., Tagawa H. Rotational acetabular osteotomy for the dysplastic hip. J Bone Joint Surg Am. 1984;66:430–436. [PubMed] [Google Scholar]
- 8.Morishima Y., Yamada H., Morita M. Hip-shelf procedure in the treatment of osteonecrosis of the transpositioned acetabulum after rotational acetabular osteotomy. J Orthop Sci. 2001;6:435–438. doi: 10.1007/s007760170011. [DOI] [PubMed] [Google Scholar]
- 9.Morita M., Yamada H., Hemmi O., Fujikawa K. Rotational acetabular osteotomy for acetabular dysplasia of the hip with a giant acetabular bone cyst: A case report. J Orthop Sci. 2004;9:99–102. doi: 10.1007/s00776-003-0742-7. [DOI] [PubMed] [Google Scholar]
- 10.Nishimatsu H., Iida H., Kawanabe K., Tamura J., Nakamura T. The modified Spitzy shelf operation for patients with dysplasia of the hip. A 24-year follow-up study. J Bone Joint Surg Br. 2002;84:647–652. doi: 10.1302/0301-620x.84b5.12732. [DOI] [PubMed] [Google Scholar]
- 11.Uchida S., Wada T., Sakoda S. Endoscopic shelf acetabuloplasty combined with labral repair, cam osteochondroplasty, and capsular plication for treating developmental hip dysplasia. Arthrosc Techn. 2014;3:e185–e191. doi: 10.1016/j.eats.2013.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Uchida S, Hatakeyama A, Kanezaki S, et al. Endoscopic shelf acetabuloplasty can improve clinical outcomes and achieve return to sports-related activity in active patients with hip dysplasia[published online November 28, 2017]. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-017-4787-0. [DOI] [PMC free article] [PubMed]
- 13.Yoshida M., Konishi N. Subchondral cysts arise in the anterior acetabulum in dysplastic osteoarthritic hips. Clin Orthop Relat Res. 2002:291–301. doi: 10.1097/00003086-200211000-00044. [DOI] [PubMed] [Google Scholar]
- 14.Sabokbar A., Crawford R., Murray D.W., Athanasou N.A. Macrophage-osteoclast differentiation and bone resorption in osteoarthrotic subchondral acetabular cysts. Acta Orthop Scand. 2000;71:255–261. doi: 10.1080/000164700317411843. [DOI] [PubMed] [Google Scholar]
- 15.Hipp J.A., Sugano N., Millis M.B., Murphy S.B. Planning acetabular redirection osteotomies based on joint contact pressures. Clin Orthop Relat Res. 1999;364:134–143. doi: 10.1097/00003086-199907000-00018. [DOI] [PubMed] [Google Scholar]
- 16.Fu M., Xiang S., Zhang Z. The biomechanical differences of rotational acetabular osteotomy, Chiari osteotomy and shelf procedure in developmental dysplasia of hip. BMC Musculoskel Disord. 2014;15:47. doi: 10.1186/1471-2474-15-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This movie shows a surgical technique for endoscopic shelf acetabuloplasty for treating acetabular large bone cyst in a patient with hip dysplasia. A 23-year-old male professional rugby player presented with a 10-year-history of right hip pain. Physical examination showed limited range of motion and positive impingement sign and dial test. The lateral center edge angle is 7°, and the vertical center anterior angle is 5°, suggesting anterolateral uncoverage of the socket. A round osteolytic lesion is found at the anterosuperior aspect of the right acetabulum. Using a scope view from the anterolateral portal on the right hip, anterosuperior and posterior labral tear and cartilage delamination (MAHORN grade 4) are observed. A prominent AIIS is observed adjacent to a torn anterosuperior labrum. Subspine decompression and tiny rim refreshing are performed using a motorized round burr. Using a scope view from the anterolateral portal on the right hip, anterosuperior labral repair with suture anchor is performed with the lasso loop technique. Using a scope view from the midanterior portal, posteriorsuperior labral refixation is performed. After releasing the traction and confirming labral sealing, peripheral compartment arthroscopy and cam osteoplasty are performed. Complete capsular plication with 5 no. 2 nonabsorbable sutures is then performed. After capsular plication, the 30° arthroscope is positioned into the extracapsular space through the anterolateral portal. Endoscopic soft-tissue debridement enables good visualization and a secure working space for shelf acetabuloplasty. Three parallel 2.4-mm guide wires are introduced using a drill guide through the midanterior portal along the anterosuperior aspect of the acetabular rim adjacent to the capsule. The transverse slot is made with the use of a 10-mm wide osteotome that is introduced along with 3 guide wires. A vertical slot is made using a Kirshner wire and an osteotome to access bone cyst, and then the bone cyst is found through the vertical and transverse slots. The cystic contents are removed by a forceps and shaver. We confirm the optimum width and depth using a custom-made dilator. Corticocancellous bone chips are packed into the bony cyst cavity. A free autologous tricortical bone graft is harvested from the ipsilateral iliac crest. Two 1.5-mm Kirshner wires are introduced, which helps to control the graft position during endoscopic insertion into the transverse slot. The bone graft is then secured into the transverse slot using the parallel skewer wires and secured into position via press fit. Postoperative 3-dimensional computed tomography scan shows enough coverage of the acetabulum, and a large bone cyst is stuffed with bone grafts. Pelvic radiographs show good remodeling of shelf graft, and the bone cyst completely disappears.