Abstract
Background
Data on the link between anxiety and body composition in youth are mixed. Yet, anxiety and disordered eating are highly correlated. One pathway between anxiety and excess body weight and fat mass may be through loss of control (LOC) eating. We examined whether LOC eating mediated the relationship between anxiety and body composition in youth with and without overweight.
Method
Non-treatment-seeking youth (8–17 years) participated in studies examining weight and eating behaviors. Anxiety (child- and parent-report of child) and LOC eating were assessed by self-report questionnaires and interviews, respectively. Fat mass was assessed by dual-energy x-ray absorptiometry or air displacement plethysmography. Cross-sectional mediation models with bias-corrected bootstrap confidence intervals (CI) were conducted.
Results
257 youth (12.91±2.76 years; 52.5% female; BMI-z 0.93±1.07) were studied. There was a significant indirect path between child-reported anxiety and both BMI-z (ab=. 005, SE=.003, 95% CI=.001–.01) and body fat mass (ab=.001, SE=.001, 95% CI=<.001–.003) through the number of LOC episodes in the past month. No significant indirect paths through the number of LOC episodes was observed for parent-report of child anxiety on BMI-z (ab=.004, SE=.01, 95% CI= −.01–.03) or body fat mass (ab=.001, SE=.002, 95% CI= −.002–.01). No direct paths were observed between anxiety and body composition regardless of the informant.
Discussion
LOC eating appears to mediate the relationship of child-reported anxiety with body composition in non-treatment seeking boys and girls. Prospective data are needed to determine if anxiety promotes LOC eating that results in increased risk for excess body weight and fat gain.
Keywords: loss of control eating, anxiety, adiposity, children and adolescents
1. Introduction
Anxiety disorders are among the most common psychiatric problems during childhood and adolescence (Merikangas, et al., 2010) and are particularly common in both treatment and non-treatment seeking youth (i.e., children and adolescents) with overweight (Van Vlierberghe, Braet, Goossens, & Mels, 2009). Data from a nationally representative sample indicate that youth with overweight are 1.6 times more likely to report internalizing problems (e.g., anxiety) compared to youth without overweight (BeLue, Francis, & Colaco, 2009). Additionally, youth with overweight and obesity who experience clinical anxiety have worse psychosocial functioning compared to their peers without clinical anxiety (Lim, Espil, Viana, & Janicke, 2015). Although a meta-analysis concluded that anxiety is associated with excess weight in youth, the reported effect size was small (r=. 08) (Burke & Storch, 2015). Indeed, cross-sectional studies have shown mixed findings to support the relationship between anxiety and weight status in adolescents and young adults; while some studies demonstrate a clear association (Dreber, et al., 2017; Hillman, Dorn, & Huang, 2010; Young-Hyman, et al., 2006), others do not (Lamertz, Jacobi, Yassouridis, Arnold, & Henkel, 2002). Extant prospective data found that anxiety disorders among adolescent females are associated with significant increases in body mass index (BMI) over time (Anderson, Cohen, Naumova, & Must, 2006; Rofey, et al., 2009). By contrast, another study found that adolescent males, but not females, with anxiety disorders were at increased risk for overweight and obesity(Roberts & Duong, 2016). The relationship between anxiety and obesity in youth may also be bidirectional, in that psychological distress may foster weight gain, and being overweight may contribute to social problems due to bullying and teasing that lead to increased anxiety (Puder & Munsch, 2010). Thus, youth with overweight do not necessarily have more social problems than their peers without overweight, but because of society’s negative views toward excess body weight, they are at increased risk for stigma, which promotes anxiety. Indeed, obesity in adolescence has been shown to predict later onset of anxiety disorder diagnosis in girls (Anderson, Cohen, Naumova, Jacques, & Must, 2007). Given the inconsistent findings across studies, the nature of the relationship of anxiety with overweight and obesity during childhood requires further exploration.
One approach to elucidating the link between anxiety and body weight involves identifying mechanisms that may explain the relationship. Considering that anxiety and disordered eating are robustly correlated (Swanson, Crow, Le Grange, Swendsen, & Merikangas, 2011), one pathway between anxiety and obesity may be through loss-of-control (LOC) eating. LOC eating, a hallmark feature of binge eating disorder and bulimia nervosa, is the subjective experience of being unable to stop eating regardless of the amount of food consumed (Tanofsky-Kraff, Marcus, Yanovski, & Yanovski, 2008). Associated with overweight/obesity (Shomaker, et al., 2010; Tanofsky-Kraff, et al., 2004), LOC eating, regardless of episode size is also a prospective risk factor for excess body weight and fat in youth (Sonneville, et al., 2013; Tanofsky-Kraff, et al., 2006; Tanofsky-Kraff, Yanovski, et al., 2009). Notably, presence of LOC eating is associated with greater anxiety symptomatology (Glasofer, et al., 2007; Goossens, Braet, Van Vlierberghe, & Mels, 2009; Morgan, et al., 2002; Shomaker, et al., 2010) and predictive of worsening anxiety symptoms over time (Tanofsky-Kraff, et al., 2011).
Affect-related theories provide a relevant framework for examining the relationships between anxiety, LOC eating, and subsequent weight gain. The emotion regulation model posits that LOC eating develops into a maladaptive coping strategy for regulating negative emotions either by means of a “trade off” or through escape (Hawkins & Clement, 1984; Kenardy, Arnow, & Agras, 1996). Relief from a negative mood is reinforcing, albeit short-lived. Thus, increased bouts of LOC eating are necessary to sustain the improvements in mood (Stein, et al., 2007). In support of affect regulation models of LOC eating are data that have identified negative affect as an antecedent to a LOC episode in youth (Goldschmidt, Tanofsky-Kraff, & Wilfley, 2011; Ranzenhofer, et al., 2013; Tanofsky-Kraff, et al., 2007; Tanofsky-Kraff, McDuffie, et al., 2009). For example, one study found that youth with LOC had greater post-meal negative affect during a laboratory test meal compared to youth without reported LOC (Tanofsky-Kraff, McDuffie, et al., 2009).
There are also data to suggest that anxiety may be particularly relevant in regard to the relationship between LOC eating and adiposity. Anxiety may promote LOC eating, which may in turn drive weight and fat gain. A laboratory study that examined mediators of the relationship between social problems and palatable food intake at a test meal designed to model a LOC episode found that only anxiety, but not anger, confusion, depression, fatigue, served as a significant mediator. Moreover, socio-emotional neural circuits that commonly distinguish youth with anxiety from healthy controls may be relevant for youth who report LOC eating. Girls with overweight or obesity with reported LOC eating showed less activity in the ventromedial prefrontal cortex compared to girls without LOC eating (Shank, et al., 2017). Furthermore, a relationship between fusiform face activation and greater energy intake after exposure to peer rejection was observed only among those with LOC eating (Jarcho, et al., 2015). Lastly, in a trial aimed at preventing excess weight gain in adolescent girls with LOC eating, baseline anxiety symptoms moderated outcome, such that greater anxiety was associated with the most improved BMI-z and adiposity trajectories among girls who received the experimental intervention, which focused on improving mood states through addressing social functioning (Jarcho, et al., 2015).
To extend existing data and clarify how anxiety and LOC eating are involved in promoting excess body weight and fat, we examined anxiety, LOC eating, and body weight and fat in a non-treatment seeking sample of boys and girls. Exploring these associations in a non-treatment sample is an important step in identifying those at particular risk for obesity so that early preventive interventions may be developed. Based on affect regulation theory (Hawkins & Clement, 1984; Kenardy, et al., 1996), and recent data (Jarcho, et al., 2015; Shank, et al., 2017; Tanofsky-Kraff, et al., 2016) we hypothesized that LOC eating would mediate the association between child- and parent-report of child anxiety and body weight/fat. Specifically, those who experience high levels of anxiety would be more likely to engage in LOC eating that would be associated with greater body weight/fat.
2. Material and methods
2.1. Participants and recruitment
Participants were a convenience sample of healthy volunteers (ages 8–17 years) recruited for two separate non-intervention studies that examined eating patterns in children and adolescents (Clinicaltrials.gov. ID: NCT00320177, NCT02390765). Children and adolescents were recruited through mailings to families in the greater Washington, DC metropolitan area; flyers posted at the National Institutes of Health (NIH) and throughout local community facilities; and direct recruitment of children who had already endorsed LOC eating or overeating in previous studies. Boys and girls were deemed eligible to participate if their BMI was ≥ 5th percentile for their age and sex according to the Centers for Disease Control and Prevention 2000 US standards (Centers for Disease Control and Prevention, 2000) and were in good general health based on a physical examination. Participants were excluded if they were seeking treatment for a major medical or psychiatric illness; were taking medication that affected body weight or eating behavior; were taking medication that affected body weight or eating behavior; endorsed regular use of alcohol, tobacco products, or other substances; had lost 5% of their body weight in the past three months; or were currently pregnant or had a history of pregnancy. Parents of children and adolescents were encouraged to participate in both protocols but were not required. At the time of recruitment, a total of 35 participants did not meet eligibility criteria at the screening visits, and 9 withdrew due to lack of interest. Both protocols were approved by the Institutional Review Board at the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
2.2. Procedure
Written consent and assent were provided by parents/guardians and children, respectively. All procedures were carried out at outpatient visits conducted at the Hatfield Clinical Research Center of the NIH.
2.3. Measures
2.3.1. Body Composition
Height (cm) was measured in triplicate by stadiometer, and fasting weight (kg) was measured by a calibrated scale to the nearest 0.1 kg. BMI (kg/m2) was then calculated using the average height. Age and sex-adjusted BMI-z was calculated based on the Centers for Disease Control and Prevention growth standards (Centers for Disease Control and Prevention, 2000). Body fat mass (kg) was measured using either dual-energy x-ray absorptiometry (DXA; iDXA system, GE Healthcare, Madison WI) and analyzed with GE Encore 15, SP 2 software or via air displacement plethysmography (Bod Pod; Life Measurement Inc. Concord, CA) as previously described (Nicholson, et al., 2001). As DXA and Bod Pod are cost-prohibitive assessments of body fat mass, we included two measures of body composition (i.e., BMI-z and body fat mass) for the purpose of study replication.
2.3.2 Anxiety Symptoms
Child report of anxiety was measured using the trait scale of the State-Trait Anxiety Inventory for Children (Spielberger, 1973), a widely used and well-validated 20-item self-report measure (Muris, Merckelbach, Ollendick, King, & Bogie, 2002). The trait scale is not a clinical measure of anxiety, but rather assesses general proneness to anxious behaviors. Children and adolescents reported the extent to which they “usually feel” 20 anxiety-related symptoms, based on a 3-point scale, ranging from 1= “Hardly ever, 2= “Sometimes”, or 3= “Often”. The possible total score range for the Trait scale is 20–60. The total score was used for analyses, with higher scores corresponding to greater symptoms of anxiety. The trait scale demonstrates good internal consistency among non-treatment seeking children and good test-retest reliability over the course of two months (Spielberger, 1972). Cronbach’s alpha for the 20 items in the present study was α=.88.
Parent-report of child anxiety was measured using the DSM-IV Child Behavior Checklist Anxiety Problem scale (Achenbach, Dumenci, & Rescorla, 2003). The Anxiety Problem scale comprises six features of anxiety that experts deemed consistent with DSM-IV constructs of generalized anxiety disorder, specific phobia, and separation anxiety disorder. The items include: “Dependent,” “Fears,” “Fears school,” “Nervous,” “Fearful,” and “Worries.” Responses are recorded on a scale ranging from 0=Not True, 1=Somewhat or Sometimes True, and 2=Very True or Often True, yielding a possible total raw score range from 0–12. The total score was used for analyses, with higher scores indicating greater parent-report of child anxiety symptoms. The scales have shown good internal consistency, test-retest reliability, and cross-informant agreement (Achenbach, et al., 2003). Cronbach’s alpha for the six items in the present study was α=. 61. The Anxiety Problem scale is also consistent with DSM-IV nosology of anxiety disorders in both clinical and non-clinical samples of youth (Ferdinand, 2008; Price, et al., 2013).
2.3.3 Depressive Symptoms
Report of child depressive symptoms was measured using the Children’s Depression Inventory,(Kovacs, 1992), a 27-item measure that assesses depressive behaviors and cognitions in the past two weeks. The items from the Children’s Depression Inventory are summed into a total raw score with ranges from 0–54. Higher scores indicate greater depressive symptoms. A cut-off of 19–20 is typically used in non-clinical samples as an indicator of heightened depressive symptoms (Kovacs, 1992). The Children’s Depression Inventory was included as a covariate in all mediation models due to the comorbidity of anxiety and depression (Cummings, Caporino, & Kendall, 2014) and depression and obesity (Blaine, 2008) in youth. The Children’s Depression Inventory demonstrates good internal consistency and convergent and discriminant validity (Carey, Gresham, Ruggiero, Faulstich, & Enyart, 1987) and has been used to assess depression in samples of youth at risk for adult obesity (Shomaker, et al., 2011). The sum score was used for the purpose of the analyses. Cronbach’s alpha for the 27 items in the present study was α=.84.
2.3.4. LOC Eating
As described in other studies (Tanofsky-Kraff, et al., 2007; Tanofsky-Kraff, et al., 2004), the number of LOC eating episodes in the past 28 days was measured using the Eating Disorder Examination version 12OD/C.2 (Fairburn & Cooper, 1993) or the adapted version for children (Bryant-Waugh, Cooper, Taylor, & Lask, 1996). Participants reporting at least one instance of overeating with LOC or LOC with subjective interpretation of the episode as large by the participant were categorized as having LOC eating. Report of ≥12 binge episodes (overeating with LOC) in the past three months is considered clinically significant. The Eating Disorder Examination has demonstrated good inter-rater reliability and discriminant validity in pediatric samples with and without overweight (Glasofer, et al., 2007; Tanofsky-Kraff, et al., 2004) and the adult and child versions have been successfully used together for samples of youth ages 8–18 (Tanofsky-Kraff, et al., 2007).
2.4. Data analysis
All analyses were performed with SPSS Version 24. Data were screened for outliers and normality, and the number of LOC episodes and fat mass were log-transformed to improve normality. Prior to running mediation models, independent-samples t-test was run to assess differences between those excluded and those included in analyses. Four cross-sectional mediation models were conducted using the PROCESS macro Version 2.16 for SPSS model 4 (Hayes, 2013). Each model examined either child-reported anxiety or parent-report of child anxiety as the independent variable, the number of LOC episodes in the past 28 days as the mediator, and fat mass (adjusting for age, sex, race, height, and depression) or BMI-z (adjusting for age, sex, race, and depression) as the dependent variable. Assessment of fat mass (Bod Pod or DEXA) was adjusted to account for known differences in assessment technique. All models used bias-corrected bootstrapping with 10,000 resamples to estimate the 95% confidence interval (CI) for direct and indirect paths. No statistical test assumptions were violated. All tests were two-tailed. Differences were considered significant when p-values were ≤ .05.
3. Results
3.1. Participant Characteristics
Two hundred fifty-seven youth (52.5% girls) aged 8–17 years (M=12.91, SD=2.76) participated. Sixty individuals (18.9%) were excluded from analyses due to any missing data on the key variables in the models: 55 individuals did not have parent-report measure of child anxiety since parent participation was not mandatory, 1 was missing a measure of adiposity, and 4 were missing depressive symptoms. No significant differences on demographic variables were identified between those included and those excluded from analyses. Youth had an average BMI-z of 0.93 (SD=1.07). One hundred forty-four (56.0%) participants identified as Non-Hispanic White, 82 (31.9%) as Non-Hispanic Black, 14 (5.4%) as Hispanic and 17 (6.6%) as mixed race or another or unknown racial/ethnic group. Sixty-three (25%) participants endorsed at least one LOC episode in the past 28 days (range=1–28 episodes, M=3.60, Mdn=2.00, SD=4.86), and one individual met criteria for binge eating disorder. As findings did not change when this individual was excluded from analyses, we retained this participant’s data. Child anxiety and parent reports of child anxiety were modestly, but significantly correlated (r= .17, p=.01). Participant demographics and questionnaire data are included in Table A.
Table A.
| Age in years, M (SD) | 12.91 (2.76), range: 8.00–17.87 |
| Race, n (%) | |
| Non-Hispanic White | 144 (56.0) |
| Non-Hispanic Black | 82 (32.0) |
| Hispanic | 14 (5.4) |
| Other/Unknown | 17 (6.6) |
| BMI-z score, M (SD) | 0.93 (1.07), range: −1.50–3.83 |
| BMI in kg/m2, M (SD) | 23.74 (8.38), range: 14.40–68.98 |
| Fat Mass (%), M (SD) | 27.88 (11.94), range: 2.60–59.10 |
| LOC Eating Episodes in past 28 days, M (SD) | 3.60 (4.86), range: 1–28 |
| Child-Report of Anxiety, M (SD) | 30.46 (7.02), range: 9.00–53.00 |
| Parent-Report of Child Anxiety, M (SD) | .92, (1.31), range: .00–7.00 |
| Depressive Symptoms, M (SD) | 5.70, (5.33), range: 0–35 |
Note: N=257; LOC, loss of control
3.2. Mediation Models
3.2.1. Child-Report of Anxiety and BMI-z
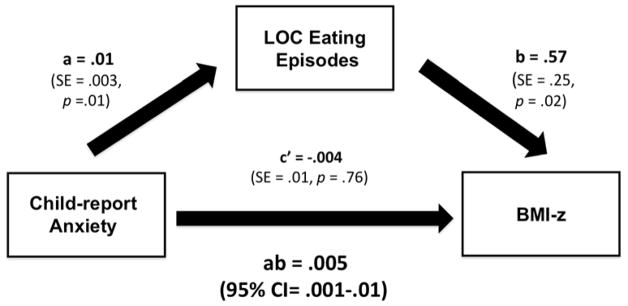
There was no significant total (c=.001, SE=.01, 95% CI= −.02–.03) or direct (c′= −.004, SE=.01, 95% CI= −.03–.02) paths between child-report of anxiety and BMI-z. However, child-report of anxiety was positively associated with the number of LOC eating episodes (a=.01, SE=.003, p =.01), and LOC episode frequency was significantly associated with BMI-z (b=.57, SE=.25, p=.02). Moreover, there was a significant indirect path between child-report of anxiety and BMI-z through LOC episodes (ab=.005, SE=.003, 95% CI= .001–.01; Figure A).
Figure A.
Mediation model examining the relationship between child-report of anxiety, number of loss-of-control (LOC) episodes, and BMI-z. Model adjusted for age, sex, race, and depressive symptoms.
3.2.2. Child-Report of Anxiety and Fat Mass
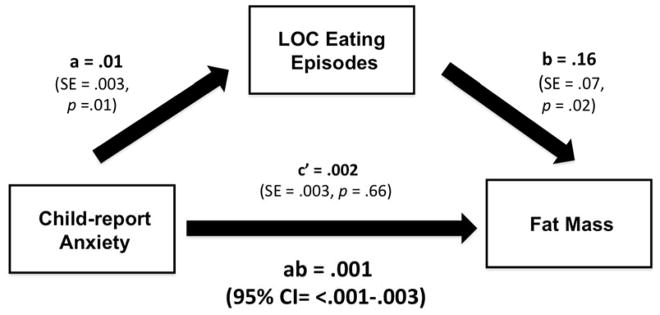
There was no significant total (c=.003, SE=.003, 95% CI= −.004–.01) or direct (c′=.002, SE=.003, 95% CI= −.005–.01) paths between child-reported anxiety and body fat mass. However, child-report of anxiety was significantly associated with LOC eating episode frequency (a=.01, SE=.003, p=.01), and the number of LOC episodes was positively associated with fat mass (b=.16, SE=.07, p=.01). Moreover, there was a significant indirect path between child-report of anxiety and body fat mass through the number of LOC episodes (ab=.001, SE=.001, 95% CI= <.001–.003; figure B).
Figure B.
Mediation model examining the relationship between child-report of anxiety, number of loss-of-control (LOC) episodes, and fat mass. Model adjusted for age, sex, race, height, and depressive symptoms.
3.2.3. Parent-Report of Child Anxiety and BMI-z and Fat Mass
There were no significant indirect (ab=.004, SE=.01, 95% CI= −.01–.03) direct (c′= −.01, SE=.05, 95% CI= −.10–.09) or total (c=−.003, SE=.05, CI=−.10–.09) paths between parent-report of child anxiety on BMI-z. Likewise, there was no indirect (ab=.001, SE=.002, 95% CI= −.002–.01) direct (c′=.001, SE=.01, 95% CI= −.02–.03) or total (c=.002, SE=.01, 95% CI= −.02–.03) paths between parent-report of child anxiety and fat mass.
4. Discussion
In a non-treatment seeking, convenience sample of youth with and without overweight, no total or direct paths were observed between child- or parent-report of anxiety and body composition after accounting for LOC eating. However, LOC eating frequency mediated the relationships between child-report of anxiety and BMI-z/body fat mass. LOC eating did not mediate the relationships between parent-report of child anxiety and BMI-z/body fat mass.
We found no direct paths between anxiety, whether child- or parent-reported, and BMI-z/body fat mass. Some (Dreber, et al., 2017; Hillman, et al., 2010; Young-Hyman, et al., 2006) but not all (Lamertz, et al., 2002) studies support a significant and positive association between anxiety and body weight, and there is significant variation based on sample and measurement characteristics. For example, in a meta-analysis that included both children and adolescents, the relationship between anxiety and body weight was stronger among females, children under the age of 12, and when using norm-referenced measures of weight (e.g., BMI-z) (Burke & Storch, 2015). Therefore, a significant association may have been evidenced had we examined anxiety in a sample of young girls with overweight. Future investigation with more homogenous samples are warranted.
As the findings from the present study suggest, the association between anxiety and body composition may be explained, in part, by frequency of LOC eating. LOC eating is associated with more anxiety symptoms in youth (Glasofer, et al., 2007; Goossens, et al., 2009; Morgan, et al., 2002; Shomaker, et al., 2010). Further, at least one study has shown that anxiety is the most salient mood state among youth with LOC eating (Shank, et al., 2017). Additionally, another study found that anxiety, but not depression, was associated with LOC eating in youth with overweight (Goossens, et al., 2009). LOC eating is a strong predictor of excess weight and fat gain in youth (Sonneville, et al., 2013; Tanofsky-Kraff, et al., 2006; Tanofsky-Kraff, Yanovski, et al., 2009) and our data support the notion that anxiety may play a role in the relationship between LOC eating and body weight/fat. While we did not find that anxiety and body weight/fat were linked directly, LOC eating represents one distinct pathway by which anxiety may contribute to weight and fat gain.
The relationship between anxiety, LOC eating, and BMI-z/fat mass was significant only when children, but not parents, reported their anxiety symptoms. Previous research has underscored the need to corroborate child-report of anxiety with reports from multiple informants (i.e., parents and teachers); however, parent and child reports do not always converge (Achenbach, McConaughy, & Howell, 1987). Indeed, parent-child agreement is low for reports of anxiety symptoms and is particularly low for reports on internalizing versus externalizing disorders (Choudhury, Pimentel, & Kendall, 2003). Despite a small, but significant association between child and parent reports in the current study, several studies show that children tend to be better reporters of their subjective experiences of anxiety than their parents and some interpret these findings to mean that children are more valid informants due to an intimate knowledge of their own internal states (Cobham & Rapee, 1999; DiBartolo & Grills, 2006). The lack of association between parent-report of anxiety symptoms, LOC eating, and BMI-z/fat mass reflects the prevailing challenge of informant discrepancies when reporting child psychopathology.
Study strengths include the use of a large, diverse sample of children and adolescents, the objective assessment of body composition, and a rigorous structured clinical interview to assess LOC eating. Limitations include the cross-sectional analysis conducted, which precludes causal inferences regarding the relationship between anxiety and body weight/fat, and the employment of a convenient sample of youth. Our findings may have been more robust had we included treatment-seeking youth who may have reported more symptoms of anxiety and LOC eating episodes. Moreover, since we used a multi-symptom measure of anxiety, we were unable to examine specific anxiety disorders in relation to excess weight/fat. For example, social anxiety may be particularly relevant to girls with LOC eating (Jarcho, et al., 2015) and is correlated with obesity in treatment-seeking youth (Thompson, Phillips, McCracken, Thomas, & Ward, 2013). Future research should replicate our findings in a treatment-seeking sample and assess if the strength of the relationship between anxiety, LOC eating, and body weight/fat varies by type of anxiety disorder. Furthermore, prospective data are needed to better characterize the interplay among anxiety, LOC eating, and body weight/fat. Future research should identify other biological and psychological mechanisms that may explain the relationship between anxiety and excess weight/fat in order to inform potential targets for obesity intervention among youth with anxiety symptoms.
5. Conclusions
In conclusion, LOC eating appears to mediate the relationship between child-reported anxiety and body weight/fat in non-treatment-seeking boys and girls. Youth who report both higher levels of anxiety and LOC eating may be at increased risk for excess body weight and fat. However, these findings should be replicated with prospective data.
Acknowledgments
Role of Funding Sources: This work was supported by the Uniformed Services University of the Health Sciences grant R072IC (to MT-K), and the Intramural Research Program, Eunice Kennedy Shriver National Institute of Child Health and Human Development, NIH, grant Z1AHD00641 (to JAY). The funding sources had no involvement in study design, in the collection, analysis and interpretation of data, in the writing of the report, or in the decision to submit the article for publication.
Footnotes
Contributors: Anne Claire Grammer, Marian Tanofsky-Kraff, and Jack A. Yanovski conceived the hypothesis for this article. Anne Claire Grammer, Marian Tanofsky-Kraff, Jack A. Yanovski, and Meghan E. Byrne wrote the first draft of the manuscript. Natasha L. Burke and Anne Claire Grammer, conducted data analysis. All authors (Anne Claire Grammer, Marian Tanofsky-Kraff, Natasha L. Burke, Meghan E. Byrne, Sarah J. Mi, Manuela Jaramillo, Lisa M. Shank, Nichole R. Kelly, Monika K. Stojek, Natasha A. Schvey, Miranda M. Broadney, Sheila M. Brady, Susan Z. Yanovski, and Jack A. Yanovski) participated in data collection, reviewed and edited the manuscript, and approved the final version of the manuscript.
Disclaimers: JAY is a Commissioned Officer of the United States Public Health Service (USPHS). The opinions and assertions expressed herein are those of the authors and are not to be construed as reflecting the views of the USPHS, the Department of the Navy, USUHS or the U.S. Department of Defense.
Conflict of Interest: All authors declare no potential biomedical conflicts of interest, financial or otherwise, relevant to this article (Anne Claire Grammer, Marian Tanofsky-Kraff, Natasha L. Burke, Meghan E. Byrne, Sarah J. Mi, Manuela Jaramillo, Lisa M. Shank, Nichole R. Kelly, Monika K. Stojek, Natasha A. Schvey, Miranda M. Broadney, Sheila M. Brady, Susan Z. Yanovski, and Jack A. Yanovski).
Portions of this study were presented at the Annual American Psychological Association, Washington, DC, August, 2017 and at the Annual Obesity Society, Washington, DC, November, 2017.
References
- Achenbach TM, Dumenci L, Rescorla LA. DSM-Oriented and Empirically Based Approaches to Constructing Scales From the Same Item Pools. Journal of Clinical Child & Adolescent Psychology. 2003;32:328–340. doi: 10.1207/S15374424JCCP3203_02. [DOI] [PubMed] [Google Scholar]
- Achenbach TM, McConaughy SH, Howell CT. Child/adolescent behavioral and emotional problems: Implications of cross-informant correlations for situational specificity. Psychological Bulletin. 1987;101:213–232. [PubMed] [Google Scholar]
- Anderson SE, Cohen P, Naumova EN, Jacques PF, Must A. Adolescent obesity and risk for subsequent major depressive disorder and anxiety disorder: prospective evidence. Psychosomatic Medicine. 2007;69:740–747. doi: 10.1097/PSY.0b013e31815580b4. [DOI] [PubMed] [Google Scholar]
- Anderson SE, Cohen P, Naumova EN, Must A. Association of depression and anxiety disorders with weight change in a prospective community-based study of children followed up into adulthood. Archives of Pediatric & Adolescent Medicine. 2006;160:285–291. doi: 10.1001/archpedi.160.3.285. [DOI] [PubMed] [Google Scholar]
- BeLue R, Francis LA, Colaco B. Mental health problems and overweight in a nationally representative sample of adolescents: effects of race and ethnicity. Pediatrics. 2009;123:697–702. doi: 10.1542/peds.2008-0687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blaine B. Does Depression Cause Obesity?: A Meta-analysis of Longitudinal Studies of Depression and Weight Control. Journal of Health Psychology. 2008;13:1190–1197. doi: 10.1177/1359105308095977. [DOI] [PubMed] [Google Scholar]
- Bryant-Waugh RJ, Cooper PJ, Taylor CL, Lask BD. The use of the eating disorder examination with children: A pilot study. International Journal of Eating Disorders. 1996;19:391–397. doi: 10.1002/(SICI)1098-108X(199605)19:4<391::AID-EAT6>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- Burke NL, Storch EA. A meta-analysis of weight status and anxiety in children and adolescents. Journal of Developmental & Behavioral Pediatrics. 2015;36:133–145. doi: 10.1097/DBP.0000000000000143. [DOI] [PubMed] [Google Scholar]
- Carey M, Gresham F, Ruggiero L, Faulstich M, Enyart P. Children’s Depression Inventory: Construct and Discriminant Validity Across Clinical and Nonreferred (Control) Populations. Journal of Consulting and Clinical Psychology. 1987;55:755–761. doi: 10.1037//0022-006x.55.5.755. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. 2000 CDC growth charts for the United States. Methods and development. Vital & Health Statistics. 2000;246:1–190. [PubMed] [Google Scholar]
- Choudhury MS, Pimentel SS, Kendall PC. Childhood Anxiety Disorders: Parent–Child (Dis) Agreement Using a Structured Interview for the DSM-IV. Journal of the American Academy of Child & Adolescent Psychiatry. 2003;42:957–964. doi: 10.1097/01.CHI.0000046898.27264.A2. [DOI] [PubMed] [Google Scholar]
- Cobham VE, Rapee RM. Accuracy of Predicting a Child’s Response to Potential Threat: A Comparison of Children and Their Mothers. Australian Journal of Psychology. 1999;51:25–28. [Google Scholar]
- Cummings CM, Caporino NE, Kendall PC. Comorbidity of anxiety and depression in children and adolescents: 20 years after. Psychological Bulletin. 2014;140:816–845. doi: 10.1037/a0034733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiBartolo PM, Grills AE. Who is best at predicting children’s anxiety in response to a social evaluative task?: A comparison of child, parent, and teacher reports. Journal of Anxiety Disorders. 2006;20:630–645. doi: 10.1016/j.janxdis.2005.06.003. [DOI] [PubMed] [Google Scholar]
- Dreber H, Reynisdottir S, Angelin B, Tynelius P, Rasmussen F, Hemmingsson E. Mental distress in treatment seeking young adults (18–25 years) with severe obesity compared with population controls of different body mass index levels: cohort study. Clinical Obesity. 2017 doi: 10.1111/cob.12170. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z. The Eating Disorder Examination. In: Fairburn CG, Cooper Z, editors. Binge Eating: Nature, Assessment and Treatment. 12. New York: Guilford; 1993. [Google Scholar]
- Ferdinand RF. Validity of the CBCL/YSR DSM-IV scales Anxiety Problems and Affective Problems. Journal of Anxiety Disorders. 2008;22:126–134. doi: 10.1016/j.janxdis.2007.01.008. [DOI] [PubMed] [Google Scholar]
- Glasofer DR, Tanofsky-Kraff M, Eddy KT, Yanovski SZ, Theim KR, Mirch MC, Ghorbani S, Ranzenhofer LM, Haaga D, Yanovski JA. Binge eating in overweight treatment-seeking adolescents. Journal of Pediatric Psychology. 2007;32:95–105. doi: 10.1093/jpepsy/jsl012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldschmidt AB, Tanofsky-Kraff M, Wilfley DE. A laboratory-based study of mood and binge eating behavior in overweight children. Eating Behaviors. 2011;12:37–43. doi: 10.1016/j.eatbeh.2010.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goossens L, Braet C, Van Vlierberghe L, Mels S. Loss of control over eating in overweight youngsters: the role of anxiety, depression and emotional eating. European Eating Disorders Review. 2009;17:68–78. doi: 10.1002/erv.892. [DOI] [PubMed] [Google Scholar]
- Hawkins RC, Clement PF. Binge eating: Measurement problems and a conceputal model. In: Hawkins RC II, Fremou WJ, Clement PF, editors. The binge-purge syndrome: Diagnosis, treatment, and research. Springer; New York: 1984. pp. 229–253. [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Guilford Press; New York, NY, US: 2013. [Google Scholar]
- Hillman JB, Dorn LD, Huang B. Association of anxiety and depressive symptoms and adiposity among adolescent females using Dual Energy X-ray Absorptiometry. Clinical Pediatrics. 2010;49:671–677. doi: 10.1177/0009922810363155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarcho JM, Tanofsky-Kraff M, Nelson EE, Engel SG, Vannucci A, Field SE, Romer AL, Hannallah L, Brady SM, Demidowich AP, Shomaker LB, Courville AB, Pine DS, Yanovski JA. Neural activation during anticipated peer evaluation and laboratory meal intake in overweight girls with and without loss of control eating. Neuroimage. 2015;108:343–353. doi: 10.1016/j.neuroimage.2014.12.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenardy J, Arnow B, Agras WS. The Aversiveness of Specific Emotional States Associated with Binge-Eating in Obese Subjects. Australian & New Zealand Journal of Psychiatry. 1996;30:839–844. doi: 10.3109/00048679609065053. [DOI] [PubMed] [Google Scholar]
- Kovacs M. Children’s Depression Inventory (CDI) manual. New York: Multi-Health Systems; 1992. [Google Scholar]
- Lamertz CM, Jacobi C, Yassouridis A, Arnold K, Henkel AW. Are obese adolescents and young adults at higher risk for mental disorders? A community survey. Obesity Research. 2002;10:1152–1160. doi: 10.1038/oby.2002.156. [DOI] [PubMed] [Google Scholar]
- Lim CS, Espil FM, Viana AG, Janicke DM. Associations Between Anxiety Symptoms and Child and Family Factors in Pediatric Obesity. Journal of Developmental & Behavioral Pediatrics. 2015;36:664–672. doi: 10.1097/DBP.0000000000000225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, He J-p, Burstein M, Swanson SA, Avenevoli S, Cui L, Benjet C, Georgiades K, Swendsen J. Lifetime Prevalence of Mental Disorders in US Adolescents: Results from the National Comorbidity Study-Adolescent Supplement (NCS-A) Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan CM, Yanovski SZ, Nguyen TT, McDuffie J, Sebring NG, Jorge MR, Keil M, Yanovski JA. Loss of control over eating, adiposity, and psychopathology in overweight children. International Journal of Eating Disorders. 2002;31:430–441. doi: 10.1002/eat.10038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muris P, Merckelbach H, Ollendick T, King N, Bogie N. Three traditional and three new childhood anxiety questionnaires: their reliability and validity in a normal adolescent sample. Behaviour Research and Therapy. 2002;40:753–772. doi: 10.1016/s0005-7967(01)00056-0. [DOI] [PubMed] [Google Scholar]
- Nicholson JC, McDuffie JR, Bonat SH, Russell DL, Boyce KA, McCann S, Michael M, Sebring NG, Reynolds JC, Yanovski JA. Estimation of Body Fatness by Air Displacement Plethysmography in African American and White Children. Pediatric Research. 2001;50:467. doi: 10.1203/00006450-200110000-00008. [DOI] [PubMed] [Google Scholar]
- Price M, Higa-McMillan C, Ebesutani C, Okamura K, Nakamura BJ, Chorpita BF, Weisz J. Symptom differentiation of anxiety and depression across youth development and clinic-referred/nonreferred samples: An examination of competing factor structures of the Child Behavior Checklist DSM-oriented scales. Development and Psychopathology. 2013;25:1005–1015. doi: 10.1017/S0954579413000333. [DOI] [PubMed] [Google Scholar]
- Puder J, Munsch S. Psychological correlates of childhood obesity. International Journal of Obesity. 2010;34:S37–S43. doi: 10.1038/ijo.2010.238. [DOI] [PubMed] [Google Scholar]
- Ranzenhofer LM, Hannallah L, Field SE, Shomaker LB, Stephens M, Sbrocco T, Kozlosky M, Reynolds J, Yanovski JA, Tanofsky-Kraff M. Pre-meal affective state and laboratory test meal intake in adolescent girls with loss of control eating. Appetite. 2013;68:30–37. doi: 10.1016/j.appet.2013.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts RE, Duong HT. Do Anxiety Disorders Play a Role in Adolescent Obesity? Annals of Behavioral Medicine. 2016;50:613–621. doi: 10.1007/s12160-016-9786-8. [DOI] [PubMed] [Google Scholar]
- Rofey DL, Kolko RP, Iosif AM, Silk JS, Bost JE, Feng W, Szigethy EM, Noll RB, Ryan ND, Dahl RE. A Longitudinal Study of Childhood Depression and Anxiety in Relation to Weight Gain. Child Psychiatry & Human Development. 2009;40:517–526. doi: 10.1007/s10578-009-0141-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shank LM, Crosby RD, Grammer AC, Shomaker LB, Vannucci A, Burke NL, Stojek M, Brady SM, Kozlosky M, Reynolds JC, Yanovski JA, Tanofsky-Kraff M. Examination of the interpersonal model of loss of control eating in the laboratory. Comprehensive Psychiatry. 2017;76:36–44. doi: 10.1016/j.comppsych.2017.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shomaker LB, Tanofsky-Kraff M, Elliott C, Wolkoff LE, Columbo KM, Ranzenhofer LM, Roza CA, Yanovski SZ, Yanovski JA. Salience of loss of control for pediatric binge episodes: does size really matter? International Journal of Eating Disorders. 2010;43:707–716. doi: 10.1002/eat.20767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shomaker LB, Tanofsky-Kraff M, Stern EA, Miller R, Zocca JM, Field SE, Yanovski SZ, Hubbard VS, Yanovski JA. Longitudinal study of depressive symptoms and progression of insulin resistance in youth at risk for adult obesity. Diabetes Care. 2011;34:2458–2463. doi: 10.2337/dc11-1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonneville KR, Horton NJ, Micali N, Crosby RD, Swanson SA, Solmi F, Field AE. Longitudinal associations between binge eating and overeating and adverse outcomes among adolescents and young adults: Does loss of control matter? JAMA Pediatrics. 2013;167:149–155. doi: 10.1001/2013.jamapediatrics.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielberger CD. Anxiety as an emotional state. In: Spielberger CD, editor. Anxiety: Current trends in theory and research. Vol. 1. San Diego, CA: Academic Press; 1972. [Google Scholar]
- Spielberger CD. Manual for the State-Trait Anxiety Inventory for Children. Palo Alto, CA: Consulting Psychologists Press; 1973. [Google Scholar]
- Stein RI, Kenardy J, Wiseman CV, Dounchis JZ, Arnow BA, Wilfley DE. What’s driving the binge in binge eating disorder?: A prospective examination of precursors and consequences. International Journal of Eating Disorders. 2007;40:195–203. doi: 10.1002/eat.20352. [DOI] [PubMed] [Google Scholar]
- Swanson SA, Crow SJ, Le Grange D, Swendsen J, Merikangas KR. Prevalence and correlates of eating disorders in adolescents: Results from the national comorbidity survey replication adolescent supplement. Archives of General Psychiatry. 2011;68:714–723. doi: 10.1001/archgenpsychiatry.2011.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Cohen ML, Yanovski SZ, Cox C, Theim KR, Keil M, Reynolds JC, Yanovski JA. A Prospective Study of Psychological Predictors of Body Fat Gain Among Children at High Risk for Adult Obesity. Pediatrics. 2006;117:1203. doi: 10.1542/peds.2005-1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Goossens L, Eddy KT, Ringham R, Goldschmidt A, Yanovski SZ, Braet C, Marcus MD, Wilfley DE, Olsen C, Yanovski JA. A Multisite Investigation of Binge Eating Behaviors in Children and Adolescents. Journal of Consulting and Clinical Psychology. 2007;75:901–913. doi: 10.1037/0022-006X.75.6.901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Marcus MD, Yanovski SZ, Yanovski JA. Loss of Control Eating Disorder in Children Age 12y and Younger: Proposed Research Criteria. Eating Behaviors. 2008;9:360–365. doi: 10.1016/j.eatbeh.2008.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, McDuffie JR, Yanovski SZ, Kozlosky M, Schvey NA, Shomaker LB, Salaita C, Yanovski JA. Laboratory assessment of the food intake of children and adolescents with loss of control eating. The American Journal of Clinical Nutrition. 2009;89:738–745. doi: 10.3945/ajcn.2008.26886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Shomaker LB, Olsen C, Roza CA, Wolkoff LE, Columbo KM, Raciti G, Zocca JM, Wilfley DE, Yanovski SZ, Yanovski JA. A prospective study of pediatric loss of control eating and psychological outcomes. Journal of Abnormal Psychology. 2011;120:108–118. doi: 10.1037/a0021406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Shomaker LB, Wilfley DE, Young JF, Sbrocco T, Stephens M, Brady SM, Galescu O, Demidowich A, Olsen CH, Kozlosky M, Reynolds JC, Yanovski JA. Excess Weight Gain Prevention in Adolescents: Three-Year Outcome Following a Randomized Controlled Trial. Journal of Consulting and Clinical Psychology. 2016 doi: 10.1037/ccp0000153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Wilfley DE, Morgan CM, Yanovski SZ, Marmarosh C, Yanovski JA. Eating-Disordered Behaviors, Body Fat, and Psychopathology in Overweight and Normal-Weight Children. Journal of Consulting and Clinical Psychology. 2004;72:53–61. doi: 10.1037/0022-006X.72.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Yanovski SZ, Schvey NA, Olsen CH, Gustafson J, Yanovski JA. A Prospective Study of Loss of Control Eating for Body Weight Gain in Children at High Risk for Adult Obesity. The International Journal of Eating Disorders. 2009;42:26–30. doi: 10.1002/eat.20580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson JE, Phillips BA, McCracken A, Thomas K, Ward WL. Social anxiety in obese youth in treatment setting. Child and Adolescent Social Work Journal. 2013;30:37–47. [Google Scholar]
- Van Vlierberghe L, Braet C, Goossens L, Mels S. Psychiatric disorders and symptom severity in referred versus non-referred overweight children and adolescents. European Child and Adolescent Psychiatry. 2009;18:164–173. doi: 10.1007/s00787-008-0717-5. [DOI] [PubMed] [Google Scholar]
- Young-Hyman D, Tanofsky-Kraff M, Yanovski SZ, Keil M, Cohen ML, Peyrot M, Yanovski JA. Psychological Status and Weight-Related Distress in Overweight or At-Risk-for-Overweight Children. Obesity. 2006;14:2249–2258. doi: 10.1038/oby.2006.264. [DOI] [PMC free article] [PubMed] [Google Scholar]