Abstract
The extant literature indicates negative self-perceptions are a risk factor for disordered eating (DE) and DE is a risk factor for overweight and obesity. While childhood emotional abuse (EA) is often linked to DE and obesity, it is typically not included in comprehensive models of these health problems. Further investigation of interactions among EA, self-perception, and DE is needed to refine treatments for overweight, obesity, and DE. This study evaluated a model of DE and weight difficulties in which negative self-perception mediate the relationship between EA and DE, and DE predicts body mass index (BMI) in a population of emerging adults. Further, this study investigated the utility of history of EA for prediction of DE and classification of individuals with and without DE. Self-report questionnaires on childhood trauma, psychopathology, and eating behaviors were administered to 598 undergraduate students. Latent variable analysis confirmed the hypothesized model. Recursive partitioning determined that individuals reporting a high level of EA likely meet criteria for night eating syndrome (NES) or binge eating disorder (BED), and history of EA has a moderate to high level of specificity as a predictor of BED and NES. These findings confirm the necessity of evaluating EA and DE in emerging adults with weight difficulties, and the importance of assessing self-perception and DE in individuals with a history of EA. Future studies should investigate the utility of addressing EA and self-perception in interventions for DE and obesity and to determine whether these findings can be generalized to a clinical population.
Keywords: Childhood emotional abuse, Self-perception, BMI, Disordered eating
1. Introduction
Despite increased understanding of the etiology of overweight, obesity, and disordered eating (DE), weight management interventions remain marginally effective, or are associated with weight regain (Odom et al., 2010; Magro et al., 2008; McGuire, Wing, Klem, Lang, & Hill, 1999; Shah, Simha, & Garg, 2006; Wadden, Butryn, & Byrne, 2004). These outcomes suggest the need to explore additional targets of treatment and prevention of DE, overweight and obesity.
One model providing a framework for obesity prevention derives from a Cognitive Behavioral (CBT) model of bulimia nervosa (BN). This model posits that cognitive biases, including negative evaluations of self-worth, lead to unhealthy behaviors intended to control weight (e.g., excessive fasting, overuse of diet pills) (Fairburn & Harrison, 2003). These unhealthy weight control behaviors (UWC) are often followed unrealistically, which is conducive to abandonment of dietary control efforts. Abandonment of dietary control can take the form of binge eating (BE), which may lead to compensatory behaviors, such as purging or excessive exercise. Compensatory efforts may minimize weight gain, reinforcing BE and contributing to weight and shape concerns. This reinforcement helps maintain UWC, resulting in a cycle of disordered eating.
The literature supports the application of this CBT model of BN to obesity. Notably, it indicates that negative self-perception related to self-esteem, and dissatisfaction with weight and shape increases risk of DE, including night eating syndrome (NES), emotional eating, BE, and UWC. DE, in turn, increases risk of overweight and obesity (Boutelle, Neumark-Sztainer, Story, & Resnick, 2002; Colles, Dixon, & O’Brien, 2007; Decaluwe’ & Braet, 2005; Fairburn, Cooper, Doll, Norman, & O’Conner, 2000; Mussell et al., 1995; Neumark-Sztainer et al., 2006; Tholin et al., 2009). Although the CBT model can guide conceptualization of development of DE, overweight and obesity, it inadequately addresses early environmental factors. Early environmental factors may be particularly important to address, as eating patterns are often established early on (Berkowitz et al., 2010). These patterns likely contribute to epigenetic changes and subsequent development of DE or weight difficulties (Campbell, Mill, Uher, & Schmidt, 2011). Many of these factors, such as genetic makeup, living in a single parent household, and socioeconomic status are not feasible targets of intervention or prevention (Gable & Lutz, 2000; Rosenquist et al., 2014; Sobal & Stunkard, 1989; Zeller et al., 2007). However, childhood maltreatment, such as neglect or abuse, is one early environmental factor potentially amenable to prevention or intervention.
Research has reliably demonstrated associations between childhood maltreatment and weight status (obesity, and body mass index [BMI]) (Danese & Tan, 2014; Felitti et al., 1998; Heim, Ehlert, & Helhammer, 2000; Norman et al., 2012a). Individuals with obesity often report childhood maltreatment, (Norman et al., 2012a; Grilo et al., 2005; Salwen, Hymowitz, Vivian, & O’Leary, 2014) and experiencing abuse increases obesity risk (Williamson, Thompson, Anda, Dietz, & Felitti, 2002; Rohde et al., 2008). However, mechanisms driving the relationship between childhood maltreatment and weight status have not been fully explicated.
1.1. Obesity and DE
One possible mediator of the relationship between childhood maltreatment and obesity is DE. The literature consistently suggests an association between DE and overweight and obesity, and DE and obesity have shared risk factors (Berkowitz et al., 2010; Neumark-Sztainer et al., 2006; Eddy, Tanofsky-Kraff, Thompson-Brenner, et al., 2007). Population-based studies demonstrate that UWC, including use of laxatives or diet pills, and vomiting are related to obesity cross-sectionally (Boutelle et al., 2002), and longitudinally predict weight gain, and BE (Neumark-Sztainer et al., 2006; Neumark-Sztainer, Wall, Story, & Standish, 2012). Binge eating disorder (BED) and night eating syndrome (NES) are also more common in individuals with overweight or obesity (Colles et al., 2007; Stunkard & Allison, 2003). The overlap among UWC, BE, and NES, and their association with obesity supports the consideration of these factors as mediators of the development of overweight and obesity (Haines & Neumark-Sztainer, 2006; Neumark-Sztainer et al., 2012).
1.2. DE and obesity in emerging adulthood
The transition period between adolescence and young adulthood (ages 18–25), referred to as emerging adulthood, is considered a distinct developmental stage warranting increased attention in the literature (Arnett, 2000; Park, Mulye, Adams, Brindis, & Irwin, 2006). Emerging adulthood is likely a critical time for development of health risks, including weight difficulties (Hunt & Eisenberg, 2010; Lau, Adams, Boscardin, & Irwin, 2014; Nelson, Story, Larson, Neumark-Stainer, & Lytle, 2008), with up to 70% of emerging adults gaining weight during college (Gropper, Simmons, Connell, & Ulrich, 2012; Gropper et al., 2009). Although mechanisms behind this weight gain are not understood, DE may play a role, as DE increases from adolescence to emerging adulthood (Finlayson, Cecil, Higges, Hill, & Hetherington, 2012; Delinsky & Wilson, 2008; Liechty & Meng-Jung, 2013).
1.3. Childhood maltreatment and DE
While childhood maltreatment in general has been associated with emotional/stress eating (Greenfield & Marks, 2010) and BE (Rohde et al., 2008), many studies evaluating childhood maltreatment and DE focus on sexual abuse, or do not distinguish between forms of childhood maltreatment (Kent & Waller, 2000; Kent, Waller, & Dagnan, 1999; Norman et al., 2012b). However, childhood emotional abuse (EA) may better predict negative psychological and behavioral outcomes than other forms of abuse or adversity (Kent et al., 1999; Spinazzola et al., 2014; Wonderlich et al., 2007). In particular, Kent, Waller, and Dagnan (Kent et al., 1999) demonstrated that EA uniquely and significantly predicts DE attitudes and behaviors (e.g. drive for thinness, binging and purging behaviors, and body dissatisfaction) above and beyond physical or sexual abuse. Additionally, individuals with BED, or NES more often report EA than non-clinical groups (Allison, Grilo, Masheb, & Stunkard, 2007). Moreover, EA can predict BE, overweight status and UWC 5 years later (Neumark-Sztainer et al., 2006). The relationship between EA and DE is also seen in emerging adults (Hund & Espelege, 2006; Mazzeo & Espelage, 2002). However, little is known regarding whether screening for EA can help identify individuals with DE, and what severity of EA increases risk for BED, NES, or UWC. Furthermore, the relationship between EA and DE is likely not direct (Hund & Espelege, 2006). One proposed mediator of this relationship is negative self-perception (Kent et al., 1999).
1.4. EA and self-perception
Experimental, longitudinal, and cross sectional studies demonstrate a link between negative self-perception related to eating, body size, and self-esteem, and DE (for review see (Stice, 2002)). Across populations, EA is consistently associated with negative perceptions about weight, shape, and self-esteem (Briere & Runtz, 1990; Heim et al., 2000), and longitudinally is more predictive of internalizing disorders than physical or sexual abuse (van Harmelen et al., 2010).
Associations between EA and negative self-perception are also present among individuals with BED. In individuals with BED seeking weight management intervention, EA was associated with body dissatisfaction, low self-esteem, and self-criticism (Dunkley, Masheb, & Grilo, 2010). Research indicating that negative self-perception (including self-criticism and body dissatisfaction) mediates the relationship between verbal victimization and DE, further justifies inclusion of negative self-perception and EA in models of DE (Wright, Crawford, & Del Castillo, 2009; Yanovski, 1993; Benas & Gibb, 2008).
1.5. Current study
In accord with a CBT model of DE and obesity, the literature indicates that eating related cognitions and global negative self-perception predict DE, and in turn, these behaviors predict obesity. However, many proposed CBT models of DE and obesity fail to incorporate early environmental components, such as EA. The few studies focusing on EA in relation to DE suggest that EA plays a central etiological role, and cognitions related to negative self-perception mediate the relationship between EA and DE (Kent et al., 1999; Yanovski, 1993; Benas & Gibb, 2008; Vartanian, Smyth, Zawadzki, Heron, & Coleman, 2014). Moreover, emerging adulthood is likely a critical period for development of weight difficulties and DE, however, little is known regarding the relationship between EA and DE during this life stage (Nelson et al., 2008).
The current study sought to extend previous theories depicting development of DE by examining whether EA impacts DE by way of selfperception and whether DE impacts BMI in emerging adulthood and thus may contribute to development of obesity. Furthermore, as EA increases risk for many medical concerns, it is important to refine ways to identify individuals with a history of EA at risk for DE. As such, secondary aims of this study were to assess whether EA can predict DE, and, if so, what severity of EA increases risk for BED, NES, or UWC in emerging adults.
Thus, this study evaluated a model suggesting that negative self-perception mediates the relationship between EA and DE, and DE predicts BMI (see Fig. 1), and utilized recursive partitioning to confirm whether EA can predict DE, and establish cutoffs on a measure of EA that can predict risk of NES, BED, or UWC.
Fig. 1.
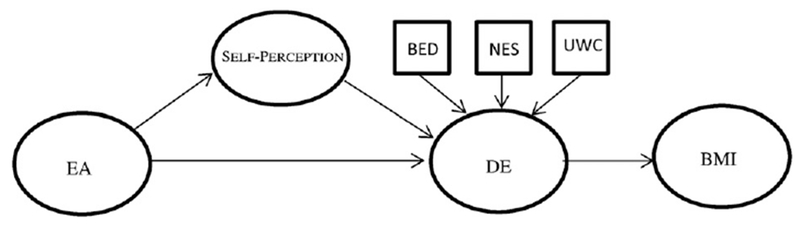
Hypothesized model of the relationships among childhood emotional abuse (EA), self-perceptions, disordered eating (DE), and obesity. BE = Binge Eating. NES = Night Eating Syndrome. UWC = Unhealthy Weight Control Behaviors. BMI = Body Mass Index.
2. Method
2.1. Participants
A total of 598 undergraduate students (60.4% women) were recruited for a study on psychopathology, eating behaviors, and interpersonal factors. Ages ranged from 18 to 24 years (M = 19.51, SD = 1.54). The majority of participants were Caucasian (45.7%), with 31.1% Asian, 8.4% Hispanic, 6.5% African-American, and 8.4% bi-racial or other. BMIs ranged from 15.78 to 49.41 (M = 24.70, SD = 5.16), with 5.4% underweight (< 18.5), 53.2% healthy weight (18.5 to 24.9), 28.4% overweight (25 to 29.9), 8.5% class I obesity (30–34.9), 2.8% class II obesity (35–9.9), and 1.7% class III obesity (>40) (National Institutes of Health National Heart Lung and Blood Institute Obesity Education Initiative Expert Panel on the Identification, Evaluation and Treatment of Obesity in Adults, 1998).
2.2. Procedure
Participants completed an online survey assessing relationships, child abuse, partner abuse, psychopathology, eating behaviors, and demographics. Participants completed one questionnaire in-person (due to copyright restrictions). Participants received course credit for participation based on the percentage of completed questionnaires. The Human Subjects Review Board approved all questionnaires and procedures.
Participants were recruited in two waves; wave one was open to all students, and wave two oversampled for participants in romantic relationships or who were overweight. Participants from these waves were not significantly different on demographic variables or other variables not directly related to weight or relationship functioning.
2.3. Variables
2.3.1. Binge eating (BE)
BE was measured by the Questionnaire of Eating and Weight Patterns- Revised (QEWP-R; (Yanovski, 1993)). Studies have shown that the BED subscale of the QWEP-R satisfactorily identifies individuals with BED (Barnes, Masheb, White, & Grilo, 2011; Celio, Wilfley, Crown, Mitchell, & Walsh, 2004; Nangle, Carr-Nangle, & Engler, 2006). Participants were asked if within the past 6 months, they ate an unusually large amount of food, and, during those times, if they often felt out of control. Participants who endorsed at least one of the aforementioned symptoms were administered 6 additional items, rated on a Likert-type scale, assessing their experiences during these occasions. While this procedure differs from DSM-5 criteria, it was used to increase variability in this measure. These participants were also administered two items assessing distress about binge eating and loss of control from 1 (not at all) to 5 (extremely). An overall score was created by summing the number of symptoms endorsed as either occurring at least once per week or as being moderately distressing. A separate diagnostic cut off for BED was created based on DSM-5 criteria. Participants included in the diagnosis group endorsed eating large portions and feeling out of control at least once per week, at least 3 of the 5 possible experiences during binges, and at least moderate distress about binge eating or loss of control. Cronbach’s alpha for this 9-item subscale was good, α = 0.92.
2.3.2. Body mass index (BMI)
BMI was derived from self-reported height and weight using the formula: (weight (lb.) / [height (in)]2) × 703.
2.3.3. Emotional abuse (EA)
EA was measured using the EA subscale of the 28-item Childhood Trauma Questionnaire (CTQ; (Bernstein et al., 2003)). The CTQ measures emotional, physical, and sexual abuse and emotional and physical neglect during childhood and adolescence. Sample item: I believe that I was emotionally abused. Items are rated on a 5-point scale ranging from 1 (never true) to 5 (very often true). Scores above 9 on this subscale indicate clinically significant EA. Cronbach’s alpha for the EA subscale was very good, α = 0.84.
2.3.4. Night eating syndrome (NES)
NES was measured with the 15-item Night Eating Questionnaire (NEQ; (Allison et al., 2008)). This measure assesses timing of eating patterns, eating during the evening or night, and sleep habits. Sample item: Do you have cravings or urges to eat snacks after supper, but before bedtime? Items are rated from 0 to 4; response choices vary by item. Participants who scored a 25 or above met criteria for NES (Allison et al., 2008). Cronbach’s alpha for this subscale was acceptable, α = 0.71, and was similar to the alpha reported by the questionnaire developers (Allison et al., 2008).
2.3.5. Self-perception
Self-perception was assessed using the Weight and Lifestyle Inventory (WALI; (Wadden & Foster, 2006)) self-perception subscale. This 6-item subscale is rated on a Likert-type scale, and assess satisfaction with overall appearance and weight, and self-esteem. Sample item: How satisfied are you with your current shape/figure/physique? Cronbach’s alpha for this subscale was good, α = 0.80.
2.3.6. Unhealthy weight control (UWC)
UWC was measured with the QEWP-R. The QEWP-R contains items assessing presence and frequency of UWC consistent with a diagnosis of BN (Yanovski, 1993). All participants were asked if following BE they engaged in UWC, including vomiting, fasting for at least 24 h, exercising for > 1 h, or taking more than twice the recommended dose of laxatives, diuretics, or diet pills. For each behavior, participants were asked if they engaged in that behavior within the past 3 months, and if so, at what frequency. A compound UWC score was created by summing the number of behaviors in which participants engaged at least once per week. For diagnostic criteria, participants who reported engaging in any UWC at least once per week were placed in the clinical group. These criteria are consistent with the compensatory behavior frequency criterion used in the DSM-5 for diagnosis of BN and with items used in previous studies evaluating relationships between UWC and BMI (Neumark-Sztainer et al., 2012). As UWC behaviors do not represent a uniform construct and do not need to occur conjointly, we did not compute a reliability coefficient. Instead, for the purposes of the model, the total number of behaviors engaged in per week was summed and coded according to DSM-5 criteria (1–3 times/week; 4–7 times/week; 8–13 times/week, or 14 or more times/week).
3. Calculation
All data were examined for missing values and normality. If >75% of items for a variable were completed, missing values were replaced with within-subject mean imputation. Participants missing >25% of the items on a questionnaire were removed from analyses. Participants who made clear mistakes on items requiring text responses (e.g. height = 5′8″) were removed from analyses. Only 3 individuals were excluded due to clear mistakes. All study variables with the exception of UWC were normally distributed. Although UWC was positively skewed, it was assumed to be an appropriate approximation of the population. Preliminary analyses were conducted using SPSS (version 24). Latent variable analysis was conducted using SPSS AMOS to evaluate the hypothesized model.
3.1. Conditional inference trees
The predictive relationship between EA and BED, NES and UWC was investigated through the non-parametric method of conditional inference trees using the R system for statistical computing (3.0.2). This statistic first identifies a binary split in the predictor variable (EA); this process is recursively repeated until there are no more cut-offs and each subgroup is maximally homogeneous. Above each cut-off, EA is strongly associated with and predictive of the outcome variable, and below, the relationship is weaker (Hothorn, Hornik, & Zeileis, 2006; Strobl, Malley, & Tutz, 2009)
4. Results
The prevalence of EA (scoring above the “normal/none” cutoff) was 27.3% (M = 8.40, SD = 3.70). With regard to DE, 11.5% of participants met criteria for BED (M = 3.36 symptoms, SD = 3.32), 3.3% scored above the clinical cut off for NES (M = 14.14, SD = 5.50), and 26.4% reported engaging in at least one UWC per week (M = 0.72 UWC behaviors/week, SD = 1.63). Table 1 shows correlations among study variables.
Table 1.
Correlations among study variables.
| EA | Self-perception | BE | NES | UWC | BMI | |
|---|---|---|---|---|---|---|
| EA | - | 0.26*** | 0.25*** | 0.37*** | 0.15*** | 0.20*** |
| Self-perception | - | 0.27*** | 0.27*** | 0.24*** | 0.39*** | |
| BE | - | 0.32*** | 0.24*** | 0.21*** | ||
| NES | - | 0.22*** | 0.15*** | |||
| UWC | - | 0.14*** |
p < 0.001.
EA = Emotional Abuse. BE = Binge Eating. NES = Night Eating Syndrome. UWC = Unhealthy Weight Control Behaviors. DE = Disordered Eating. BMI = Body Mass Index.
The hypothesized model was evaluated with latent variable analysis. The Comparative Fit Index (CFI), Root Mean Square Error of Approximation (RMSEA), and PCLOSE were also examined. The initial model in which EA predicted the latent variable of DE, which then predicted BMI did not meet acceptable standards of fit, X2 (2, N = 598) = 7.85, p = 0.02, CFI = 0.98, RMSEA = 0.07 with a 95% confidence interval from 0.02 to 0.13, and PCLOSE = 0.20.
With the addition of the mediator self-perception the model showed an excellent fit, X2 (2, N = 598) = 3.85, p = 0.15 (see Fig. 2). The relationships between EA and self-perception, self-perception and DE, and DE and BMI were all positive and significant, βs = 0.26, 0.85, and 0.43, respectively, all ps < 0.001. The meditational model also showed a very good fit across other indices and conformed to the standards of acceptable model fit (Byrne, 2010): CFI = 1.00, RMSEA = 0.04 with a 90% confidence interval from 0.00 to 0.10, and PCLOSE = 0.52. Thus, the hypothesized model was supported.
Fig. 2.
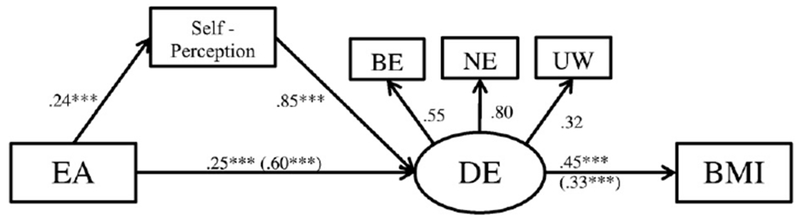
Mediational model of the relationships among childhood emotional abuse (EA), self-perceptions, disordered eating, and obesity. For the relationship between EA and DE, 0.60 is the unmediated beta and 0.25 is the beta after inclusion of Self-perception as a mediator. ***p < 0.001. EA = Emotional Abuse. BE = Binge Eating. NES = Night Eating Syndrome. UWC = Unhealthy Weight Control Behaviors. DE = Disordered Eating. BMI = Body Mass Index.
We further evaluated the fit of this model after demographic covariates, including age, gender, and ethnicity, were added. This model also showed a good fit, X2 (7, 598) = 12.36, p = 0.09 CFI = 0.99, RMSEA = 0.04 (95% confidence interval from 0.00 to 0.07), PCLOSE = 0.73. Nested model comparisons indicated that including covariates did not significantly affect fit, X2 (5, N = 598) = 8.51, p = 0.13.
To evaluate the strength of the indirect effect of EA on DE through self-perception, we examined the indirect effect of EA for each indicator on the latent variable of DE using bootstrapping procedures with 5000 samples (Hayes, 2013). The indirect effect of EA on DE was significant (0.22, 95% CI 0.15–0.30) as was the indirect effect of EA on BMI (0.20, 95% CI 0.11–0.28). Additionally, the indirect effects of EA on specific forms of DE were all significant: BE = 0.25 (95% CI 0.17–0.33), NE = 0.31 (0.23–0.39), and UWC = 0.20 (0.09–0.31).
4.1. Cut-offs for predicting BED
The algorithm identified two cut-offs for prediction of BED scores on EA, creating three nodes (low, medium, and high risk). Participants who scored above a 9 on the EA subscale of the CTQ were most likely to meet criteria for BED (p < 0.001). This cut off for the prediction of BED has a sensitivity of 51%, specificity of 76%, and Positive and Negative Predictive Values of 21% and 92%, respectively. Participants who scored above 6.67 and equal to or below 9 were categorized as moderate risk; those scoring below or equal to 6.67 were categorized as low risk. Using the second cut-off to detect BED includes all participants who scored above 6.67 (p = 0.01) on EA. Sensitivity and specificity for this threshold are 86% and 41%; positive and Negative Predictive Values are 16% and 96%, respectively.
4.2. Cut-offs for predicting NES
Two cut-offs were identified for the prediction of NES scores on EA, creating three nodes (low, medium and high risk). Participants who scored above an 18 on EA were most likely to meet criteria for NES and were identified as high-risk (p < 0.001). This cut-off for the prediction of NES has a sensitivity of 25% and a specificity of 97%. Positive and Negative Predictive Values are 25% and 97%, respectively. Participants who scored above 8 and equal to or below 18 were categorized as moderate risk, and those scoring below or equal to 8 were categorized as low risk. Using the second cut-off to detect NES includes all participants who scored above 8 (p = 0.02) on EA. Sensitivity and specificity for this threshold are 75% and 67%; positive and Negative Predictive Values are 07% and 99%, respectively.
4.3. Cut-offs for predicting UWC
The algorithm identified one cut-off on EA for the prediction of UWC; participants who scored above an 11 on EA were more likely to meet criteria for UWC than those who scored at or below 11 (high risk; p = 0.01). This cut-off has a sensitivity of 25% and a specificity of 85%. Positive and Negative Predictive Values are 38% and 76%, respectively.
5. Discussion
These findings support a model of obesity in which negative selfperception mediates the association between EA and DE (BE, NES, and UWC). In turn, DE predicts higher BMI, bolstering Kent and Waller’s (Kent & Waller, 2000) supposition that EA impacts self-esteem, thus contributing to DE. Additionally, these findings support previous findings demonstrating a relationship between DE and overweight and obesity (Eddy et al., 2007) and research indicating associations among high levels of childhood verbal aggression and lower self-esteem and global self-worth (Solomon & Serres, 1999). Other research supports this association and suggests that EA provides an individual with self-criticisms that become automatic, are triggered by external stimuli and result in unhealthy behaviors (Chaiken & Trope, 1999; Gawronski & Bodenhausen, 2006; Haeffel et al., 2007; Sachs-Ericsson, Verona, Joiner, & Preacher, 2006).
These results also suggest that emerging adults reporting high levels of EA, are more likely to meet criteria for NES or BED, and EA has a moderate to high level of specificity as a predictor of BED and NES. Additionally, these findings indicate that emerging adults without a history of EA are highly unlikely to meet criteria for BED or NES.
Contrasting with expectations, in our sample of emerging adults EA was not a sensitive predictor of UWC. This low sensitivity may be due to variability among items measuring UWC. Although BE and UWC are symptoms of BN, the criteria used for this study were not adherent to DSM-5 criteria for BN, thus they may not adequately distinguish between a clinical group and a non-clinical group.
5.1. Limitations
Though predictors in the model flowed from distal to proximal, the cross-sectional study design limited conclusions regarding causality. Although relationships among BMI, self-perceptions, and DE are likely cyclical, longitudinal data support the hypothesized directional paths tested in this study. Second, as some researchers argue that emerging adulthood is a critical stage for development of unhealthy dietary patterns, and obesity (Nelson et al., 2008) and a growing percentage of emerging adults attend college, or university, this study focused on an undergraduate student sample; however, this limits generalizability of study findings. Third, this study relied upon retrospective self-reports; however, retrospective self-reports may be more likely to lead to underreporting of events rather than false positives (Hardt & Rutter, 2004). Fourth, although BMI can be a good predictor of overweight and obesity and of weight outcomes in individuals with eating disorders (Guo, Wu, Chumlea, & Roche, 2002; Witt et al., 2014), inclusion of additional measures of weight status (e.g. waist and hip measurements) would strengthen these findings.
5.2. Conclusions
These data confirm a CBT model that includes EA as a risk factor for cognitive biases and subsequent development of DE and weight difficulties in emerging adulthood. Furthermore, these findings support the necessity of evaluating self-perception, NES and BE in emerging adults with a history of EA, These findings suggest that emerging adults demonstrating certain eating patterns may be more likely to develop overweight or obesity, further justifying the need to consider such factors when developing preventive programs. Use of recursive partitioning confirmed EA can predict DE, and helped establish cutoffs on a measure of EA for use in deciding whether further screening for NES, BED, or UWC is warranted.
References
- Allison KC, Grilo CM, Masheb RM, & Stunkard AJ (2007). High self-reported rates of neglect and emotional abuse, by persons with binge eating disorder and night eating syndrome. Behaviour Research and Therapy, 45(12), 2874–2883. 10.1016/j.brat.2007.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allison KC, Lundgren JD, O’Reardon JP, Martino NS, Sarwer DB, Wadden TA, … Stunkard AJ (2008). The Night Eating Questionnaire (NEQ): Psychometric properties of a measure of severity of the night eating syndrome. Eating Behaviors, 9,62–72. [DOI] [PubMed] [Google Scholar]
- Arnett JJ (2000). Emerging adulthood: Theory of development from the late teens through the twenties. American Psychologist, 55, 469–480. 10.1037//0003-066X.55.5.469. [DOI] [PubMed] [Google Scholar]
- Barnes RD, Masheb RM, White MA, & Grilo CM (2011). Comparison of methods for identifying and assessing obese patients with binge eating disorder in primary care settings. International Journal of Eating Disorders, 44,157–163. 10.1002/eat.20802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benas JS, & Gibb BE (2008). Weight-related teasing, dysfunctional cognitions, and symptoms of depression and eating disturbances. Cognitive Therapy and Research, 32,143–160. [Google Scholar]
- Berkowitz RI, Moore RH, Faith MS, Stallings VA, Krall TVE, & Stunkard AJ (2010). Identification of an obese eating style in 4-year-old children born at high and low risk for obesity. Obesity, 18, 505–512. 10.1038/oby.2009.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, … Zule W, (2003). Development of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse & Neglect, 27, 169–190. 10.1016/S0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- Boutelle K, Neumark-Sztainer D, Story M, & Resnick M (2002). Weight control behaviors among obese, overweight, and nonoverweight adolescents. Journal of Pediatric Psychology, 27,531–540. [DOI] [PubMed] [Google Scholar]
- Briere J, & Runtz M (1990). Differential adult symptomatology associated with three types of child abuse histories. Child Abuse & Neglect, 14,357. [DOI] [PubMed] [Google Scholar]
- Byrne BM (2010). Structural equation modeling with AMOS: Basic concepts, applications and programming (2nd ed.). New York, NY: Routledge. [Google Scholar]
- Campbell IC, Mill J, Uher R, & Schmidt U (2011). Eating disorders, gene-environment interactions and epigenetics. Neuroscience and Biobehavioral Reviews, 35, 784–793. [DOI] [PubMed] [Google Scholar]
- Celio AA, Wilfley DE, Crown SJ, Mitchell J, & Walsh BT (2004). A comparison of the binge eating scale, questionnaire for eating and weight patterns-revised, and eating disorder examination questionnaire with instructions with the eating disorder examination in the assessment of binge eating disorder and its symptoms. International Journal of Eating Disorders, 36,434–444. 10.1002/eat.20057. [DOI] [PubMed] [Google Scholar]
- Chaiken S, & Trope Y (1999). Dual-process theories in social and cognitive psychology. New York: Guilford. [Google Scholar]
- Colles SL, Dixon JB, & O’Brien PE (2007). Night eating syndrome and nocturnal snacking: Association with obesity, binge eating and psychological distress. International Journal of Obesity, 31, 1722–1730. 10.1038/sj.ijo.0803664. [DOI] [PubMed] [Google Scholar]
- Danese A, & Tan M (2014). Childhood maltreatment and obesity: A systematic review and meta-analysis. Molecular Psychiatry, 19, 544–554. [DOI] [PubMed] [Google Scholar]
- Decaluwe’ V, & Braet C (2005). The cognitive behavioural model for eating disorders: A direct evaluation in children and adolescents with obesity. Eating Behaviors, 6, 211–220. [DOI] [PubMed] [Google Scholar]
- Delinsky S, & Wilson T (2008). Weight gain, dietary restraint, and disordered eating in the freshman year of college. Eating Behaviors, 9, 82–90. [DOI] [PubMed] [Google Scholar]
- Dunkley DM, Masheb RM, & Grilo CM (2010). Childhood maltreatment, depressive symptoms and body dissatisfaction in patients with binge eating disorder: The mediating role of self-criticism. International Journal of Eating Disorders, 43, 274–281. 10.1002/eat.20796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eddy KT, Tanofsky-Kraff M, Thompson-Brenner H, et al. (2007). Eating disorder pathology among overweight treatment-seeking youth: Clinical correlates and cross-sectional risk modeling. Behaviour Research and Therapy, 45, 2360–2371. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, & Harrison PJ (2003). Eating disorders. Lancet, 361,407–416. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z, Doll HA, Norman P, & O’Conner M (2000). The natural course of bulimia nervosa and binge eating disorder in young women. Archives of General Psychiatry, 57, 659–665. [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, … Marks JS, (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences (ACE) study. American Journal of Preventive Medicine, 14,245–258. [DOI] [PubMed] [Google Scholar]
- Finlayson G, Cecil J, Higges S, Hill A, & Hetherington M (2012). Susceptibility to weight gain. Eating behavior traits and physical activity as predictors of weight gain during the first year of university. Appetite, 58,1091–1098. [DOI] [PubMed] [Google Scholar]
- Gable S, & Lutz S (2000). Household, parent, and child contributions to childhood obesity. Family Relations, 49, 293–300. [Google Scholar]
- Gawronski B, & Bodenhausen GV (2006). Associative and propositional processes in evaluation: An integrative review of implicit and explicit attitude change. Psychological Bulletin, 132, 692–731. [DOI] [PubMed] [Google Scholar]
- Greenfield EA, & Marks NF (2010). Identifying experiences of physical and psychological violence in childhood that jeopardize mental health in adulthood. Child Abuse & Neglect, 34, 161–171. 10.1016/j.chiabu.2009.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM, Masheb RM, Brody M, Toth C, Burke-Martindale CH, & Rothschild BS (2005). Childhood maltreatment in extremely obese male and female bariatric surgery candidates. Obesity Research, 13,123–130. 10.1038/oby.2005.16. [DOI] [PubMed] [Google Scholar]
- Gropper S, Simmons KP, Connell LJ, & Ulrich PV (2012). Changes in body weight, composition, and shape: A 4-year study of college students. Physiology, Nutrition, and Metabolism, 37, 1118–1123. 10.1139/H2012-139. [DOI] [PubMed] [Google Scholar]
- Gropper S, Simmons KP, Gaines A, Drawdy K, Saunders D, Ulrich P, & Connell LJ (2009). The freshman 15–A closer look. Journal of American College Health, 58, 223–231. 10.1080/07448480903295334. [DOI] [PubMed] [Google Scholar]
- Guo S, Wu W, Chumlea WC, & Roche A (2002). Predicting overweight and obesity in adulthood from body mass index values in childhood and adolescence. American Journal of Clinical Nutrition, 76, 653–658. [DOI] [PubMed] [Google Scholar]
- Haeffel GJ, Abramson LY, Brazy PC, Shah JY, Teachman BA, & Nosek BA (2007). Explicit and implicit cognition: A preliminary test of a dual-process theory of cognitive vulnerability to depression. Behaviour Research and Therapy, 45,1155–1167, 10.1016/j.brat2006.09.003. [DOI] [PubMed] [Google Scholar]
- Haines J, & Neumark-Sztainer D (2006). Prevention of obesity and eating disorders: A consideration of shared risk factors. Health Education Research, 21, 770–782. [DOI] [PubMed] [Google Scholar]
- Hardt J, & Rutter M (2004). Validity of adult retrospective reports of adverse childhood experiences: Review of the evidence. Journal of Child Psychology and Psychiatry, 45, 260–273. [DOI] [PubMed] [Google Scholar]
- Hayes AF (2013). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York: Guilford Press; 10.1016/j.biopsych.2006.03.040. [DOI] [Google Scholar]
- Heim C, Ehlert U, & Helhammer DH (2000). The potential role of hypocortisolism in the pathophysiology of stress-related bodily disorders. Psychoneuroendocrinology, 25, 1–35. 10.1016/S0306-4530(99)00035-9. [DOI] [PubMed] [Google Scholar]
- Hothorn T, Hornik K, & Zeileis A (2006). Unbiased recursive partitioning: A conditional inference framework. Journal of Computational and Graphical Statistics, 15, 651–674. [Google Scholar]
- Hund AR, & Espelege DL (2006). Childhood emotional abuse and disordered eating among undergraduate females: Mediating influence of alexithymia and distress. Child Abuse & Neglect, 30,393–407. [DOI] [PubMed] [Google Scholar]
- Hunt J, & Eisenberg D (2010). Mental health problems and help-seeking behavior among college students. Journal of Adolescent Health, 46,3–10. [DOI] [PubMed] [Google Scholar]
- Kent A, & Waller G (2000). Childhood emotional abuse and eating psychopathology. Clinical Psychology Review, 20, 887–903. [DOI] [PubMed] [Google Scholar]
- Kent A, Waller G, & Dagnan D (1999). A greater role of emotional than physical or sexual abuse in predicting disordered eating attitudes: The role of mediating variables. International Journal of Eating Disorders, 25, 159–167. [DOI] [PubMed] [Google Scholar]
- Lau JS, Adams SH, Boscardin J, & Irwin CW (2014). Young adults’ health care utilization and expenditures prior to the affordable care act. Journal of Adolescent Health, 54, 663–671. 10.1016/j.jadohealth.2014.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liechty J, & Meng-Jung L (2013). Longitudinal predictors of dieting and disordered eating in young adults in the US. International Journal of Eating Disorders, 46, 790–800. [DOI] [PubMed] [Google Scholar]
- Magro DO, Geloneze B, Delfini R, Pareja BC, Callejas F, & Pareja JC (2008). Longterm weight regain after gastric bypass: A 5-year prospective study. Obesity Surgery, 18,648–651. 10.1007/s11695-007-9265-1. [DOI] [PubMed] [Google Scholar]
- Mazzeo SE, & Espelage DL (2002). Association between childhood physical and emotional abuse and disordered eating behaviors in female undergraduates: An investigation of the mediating role of alexithymia and depression. Journal of Counseling Psychology, 49, 86–100. 10.1037//0022-0167.49.1.86. [DOI] [Google Scholar]
- McGuire MT, Wing RR, Klem ML, Lang W, & Hill JO (1999). What predicts weight regain in a group of successful weight losers. Journal of Consulting and Clinical Psychology, 67, 177–185. [DOI] [PubMed] [Google Scholar]
- Mussell MP, Mitchell JE, Weller CL, Raymond NC, Crow SJ, & Crosby RD (1995). Onset of binge eating, dieting, obesity and mood disorders among subjects seeking treatment for binge eating disorder. International Journal of Eating Disorders, 17,395–401. [DOI] [PubMed] [Google Scholar]
- Nangle DW, Carr-Nangle R#, & Engler LB (2006). Binge eating disorder and the proposed DSM-IV criteria: Psychometric analysis of the questionnaire of eating and weight patterns. International Journal of Eating Disorders, 16,147–157. [DOI] [PubMed] [Google Scholar]
- National Institutes of Health National Heart Lung and Blood Institute Obesity Education Initiative Expert Panel on the Identification, Evaluation and Treatment of Obesity in Adults (1998d). Clinical guidelines on the identification, evaluation and treatment of overweight and obesity in adults. Bethesda, MD: National Heart Lung and Blood Institute. [Google Scholar]
- Nelson MC, Story M, Larson N, Neumark-Stainer D, & Lytle LA (2008). Emerging adulthood and college- aged youth: An overlooked age for weight-related behavior change. Obesity, 16,2205–2211. 10.1038/oby.2008.365. [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Wall M, Guo J, Story M, Haines J, & Eisenberg M (2006). Obesity, disordered eating and eating disorders in a longitudinal study of adolescents: How do dieters fare 5 years later? Journal of the American Dietetic Association, 106, 559–568. 10.1016/j.jada.2006.01.003. [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Wall M, Story M, & Standish AR (2012). Dieting and unhealthy weight control behaviors during adolescence: Associations with 10-year changes in body mass index. Journal of Adolescent Health, 50, 80–86. 10.1016/j.jadohealth.2011.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman RE, Byambaa M, De R, Butchard A, Scott J, & Vos T (2012b). The long-term health consequences of child physical abuse, emotional abuse and neglect: A systematic review and meta-analysis. PLoS Medicine, 9, e1001349 10.1371/journal.pmed.1001349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman RE, Byambaa M, De R, Butchard A, Scott J, & Vos T (2012a). The long-term health consequences of child abuse, emotional abuse, and neglect: A systematic review and meta-analysis. PLoS Medicine. 10.1371/journal.pmed.1001349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odom J, Zelesin KC, Washington TL, Miller WW, Hakmeh B, Zaremba DL, … McCullough PA (2010). Behavioral predictors of weight regain after bariatric surgery. Obesity Surgery, 20, 349–356. 10.1007/s11695-009-9895-6. [DOI] [PubMed] [Google Scholar]
- Park MJ, Mulye TP, Adams SH, Brindis CD, & Irwin CE (2006). The health status of young adults in the United States. Journal of Adolescent Health, 39, 305–317. [DOI] [PubMed] [Google Scholar]
- Rohde P, Ichikawa L, Simon GE, Ludman EJ, Linde JA, Jeffery RW, & Operskalski BH (2008). Associations of child sexual and physical abuse with obesity and depression in middle-aged women. Child Abuse & Neglect, 32,878–887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenquist JN, Lehrerb SF, O’Mallevd J, Zaslavskye AM, Smollerf JW, & Christakisg NA (2014). Cohort of birth modifies the association between FTO genotype and BMI. Proceedings of the National Academy of Sciences. 10.1073/pnas.1411893111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sachs-Ericsson N, Verona E, Joiner T, & Preacher KJ (2006). Parental verbal abuse and the mediating role of self-criticism in adult internalizing disorders. Journal of Affective Disorders, 93(1–3), 71–78. 10.1016/j.jad.2006.02.014. [DOI] [PubMed] [Google Scholar]
- Salwen JK, Hymowitz GF, Vivian D, & O’Leary KD (2014). Childhood abuse, adult interpersonal abuse, and depression in individuals with extreme obesity. Child Abuse & Neglect. 10.1016/j.chiabu.2013.12.005. [DOI] [PubMed] [Google Scholar]
- Shah M, Simha V, & Garg A (2006). Review: Long-term impact of bariatric surgery on bodyweight, co-morbidities and nutritional status. The Journal of Clinical Endocrinology & Metabolism. 10.1210/jc.2006-0557. [DOI] [PubMed] [Google Scholar]
- Sobal J, & Stunkard AJ (1989). Socioeconomic status and obesity: A review of the literature. Psychological Bulletin, 105, 260–275. [DOI] [PubMed] [Google Scholar]
- Solomon CR, & Serres F (1999). Effects of parental verbal aggression on children’s self-esteem and school marks. Child Abuse& Neglect, 23, 339–351. 10.1016/S0145-2134(99)00006-X. [DOI] [PubMed] [Google Scholar]
- Spinazzola J, Hodgdon H, Briggs EC, Liang L-J, Layne CM, Pynoos R, … Kisiel C (2014). Unseen wounds: The contribution of psychological maltreatment to child and adolescent mental health and risk outcomes. Psychological Trauma: Theory, Research, Practice, and Policy, 6, S18–S28. 10.1037/a0037766. [DOI] [Google Scholar]
- Stice E (2002). Risk and maintenance factors for disordered eating: A meta-analytic review. Psychological Bulletin, 128, 825–848. [DOI] [PubMed] [Google Scholar]
- Strobl C, Malley J, & Tutz G (2009). An introduction to recursive partitioning: Rationale, application, and characteristics of classification and regression trees, bagging, and random forests. Psychological Methods, 14, 323–348. 10.1037/a0016973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stunkard A, & Allison KC (2003). Two forms of disordered eating in obesity: Binge eating and night eating. International Journal of Obesity, 27, 1–12. [DOI] [PubMed] [Google Scholar]
- Tholin S, Lindroos A, Tynellius P, Akerstedt T, Stunkard AJ, Bulik CM, & Rasmussen F (2009). Prevalence of night eating in obese and nonobese twins. Obesity Research, 17, 1050–1055. 10.1038/oby.2008.676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Harmelen AL, de Jong PJ, Glashouwer KA, Spinhoven P, Penninx BW, & Elzinga BM (2010). Child abuse and negative explicit and automatic self-associations: The cognitive scars of emotional maltreatment. Behaviour Research and Therapy, 48, 486–94. 10.1016/j.brat.2010.02.003. [DOI] [PubMed] [Google Scholar]
- Vartanian L, Smyth JM, Zawadzki MJ, Heron KE, & Coleman SRM (2014). Early adversity, personal resources, body dissatisfaction and disordered eating. International Journal of Eating Disorders, 47, 620–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wadden TA, & Foster GD (2006). Weight and Lifestyle Inventory (WALI). Obesity, 14, 99S–118S. [DOI] [PubMed] [Google Scholar]
- Wadden TA, Butryn ML, & Byrne KJ (2004). Efficacy of lifestyle modification for long-term weight control. Obesity Research, 12, 151S–162S. 10.1038/oby.2004.282. [DOI] [PubMed] [Google Scholar]
- Williamson DF, Thompson TJ, Anda RF, Dietz WH, & Felitti V (2002). Body weight and obesity in adults and self-reported abuse in childhood. International Journal of Obesity, 26,1075–1082. [DOI] [PubMed] [Google Scholar]
- Witt AA, Berkowitz SA, Gillberg C, Lowe MR, Rastam M, & Wentz E (2014). Weight suppression and body mass index interact to predict long-term weight outcomes in adolescent onset anorexia nervosa. Journal of Consulting and Clinical Psychology, 82, 1207–1211. 10.1037/a0037484. [DOI] [PubMed] [Google Scholar]
- Wonderlich SA, Rosenfeldt S, Crosby RD, Mitchell JE, Engel SG, Smyth J, & Miltenberger R (2007). The effects of childhood trauma on daily mood lability and comorbid psychopathology in bulimia nervosa. Journal of Traumatic Stress, 20, 77–87. [DOI] [PubMed] [Google Scholar]
- Wright MOD, Crawford E, & Del Castillo D (2009). Childhood emotional maltreatment and later psychological distress among college students: The mediating role of maladaptive schemas. Child Abuse & Neglect, 33, 59–68. 10.1016/j.chiabu.2008.12.007. [DOI] [PubMed] [Google Scholar]
- Yanovski SZ (1993). Binge eating disorder: Current knowledge and future directions. Obesity Research, 1, 306–324. [DOI] [PubMed] [Google Scholar]
- Zeller MH, Reiter-Purtill J, Modi AC, Gutzwiller J, Vanatta K, Davies WH (2007). Controlled study of critical parent and family factors in the obesigenic environment. Obesity, 15. [DOI] [PubMed] [Google Scholar]


