Abstract
Foreign-born Hispanics have better cardiometabolic health upon arrival in the US than their US-born counterparts, yet this advantage diminishes as duration of residence in the US increases. Underlying mechanisms explaining this paradox have been understudied. Using data from the Sacramento Area Latino Study on Aging (SALSA), this study examined immigration history (immigrant generation and duration of US residence) in relation to biomarkers of inflammation (interleukin-6 (IL-6), soluble forms of type 1 and 2 receptors of tumor necrosis factor-alpha (sTNF-R1 and sTNF-R2), C-reactive protein (CRP), leptin, adiponectin) in a sample of 1,290 predominantly Mexican-origin immigrants. Second and ≥3rd generation immigrants had higher IL-6 and leptin levels than 1st generation immigrants living in the US for less than 15 years (2nd generation percent difference = 45.9; 95% CI: 24.7, 70.7 and 3rd generation percent difference = 41.8; 95% CI: 17.7, 70.4). CRP and sTNF-R1 levels were higher among ≥3rd generation immigrants than 1st generation immigrants with less than 15 years of US residency. Worse inflammatory profiles were observed among Mexican-origin immigrants with longer US immigration histories, independent of health and behavioral factors. Additional research is warranted to understand the factors that shape trajectories of biological risk across generations of Hispanics.
INTRODUCTION
Hispanics account for nearly 17% of the United States (US) population, of which 35% are foreign-born (US Census Bureau, 2013). Among US Hispanics, 64% are of Mexican origin (Brown & Patten, 2014). Compared to US born Mexican Americans, first-generation Mexican-origin immigrants have better cardiometabolic profiles (e.g. cardiovascular and metabolic health outcomes) and lower mortality risk upon arrival in the US (Creighton et al., 2012; Crimmins et al., 2007; Kershaw et al., 2012). However, this health advantage appears to diminish in offspring born in later generations and with longer US residence, despite improvements in protective health factors, including health insurance coverage and health care utilization. (Afable-Munsuz et al., 2013; Isasi et al., 2015; Kershaw et al., 2016a; Lara et al., 2005; Le-Scherban et al., 2016). For example, a recent study of immigrant generation and type 2 diabetes risk showed greater risk of diabetes among second and third generation Mexican-origin immigrants (highest among 3rd generation immigrants) than first generation Mexican-origin immigrants, independent of sociodemographic factors including medical insurance (Afable-Munsuz et al., 2016).
Several potential explanations of the health declines observed by duration of US residence and across immigrant generations exist. First, changes in health behaviors, particularly dietary and physical activity patterns, has been emphasized in the literature. Research evidence points to acculturation – the process by which immigrants adopt the beliefs and practices of the new/dominant culture – as a contributor to changes in dietary and physical activity across immigrant generations and with longer duration of US residence. Specifically, increased acculturation has been associated with poorer dietary patterns and less physical activity (Gordon-Larsen et al., 2003; Perez-Escamilla, 2011, Perez-Escamilla, 2007; Martin et al., 2017; Perez et al., 2017) in prior research.
Second, psychosocial stressors, such as discrimination, offer another explanation. It is hypothesized that as Mexican-origin immigrants integrate into US society, they are confronted with racial/ethnic discrimination (Finch et al., 2001). Higher rates of discrimination were reported for Hispanic immigrants living in US longer and among second and third Hispanic immigrants (Perez et al., 2008). Similarly, the prevalence of reported discrimination was higher among US-born Hispanics (vs. to foreign-born Hispanics) and Hispanics with ≥10 years of US residence (Arellano-Morales et al., 2015).
Several studies have examined the influence of nativity and duration of US residence on cardiometabolic health outcomes in Mexican-origin immigrants (Dinwiddie et al., 2014; Kershaw et al., 2016a; Le-Scherban et al., 2016; Afable-Munsuz et al., 2013). While these health outcomes are important to study in their own right, it is of interest to analyze early markers of disease to better assess the changing physiological profile that may be altered in response to immigration history and life experiences in the US. Therefore, inflammatory pathways are plausible mechanisms of disease risk that warrant further exploration. Exposure to stressors related to acculturation may increase risk of cardiometabolic outcomes through dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis, one of the body’s main stress-response systems, and the stimulation of pro-inflammatory cytokines, such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α), and C-reactive protein (CRP), an acute-phase marker of systemic inflammation (Papanicolaou et al., 1998; Steptoe et al., 2007). Similarly, foreign-born Mexicans had higher inflammation profiles (e.g. CRP, fibrinogen, and albumin) than US born Mexican Americans (Crimmins et al., 2007).
To date, studies have not examined the effect of immigrant generation—the number of generations (1st, 2nd, 3rd, etc) for which Mexican-origin immigrants have been living in the US— and length of US residency on inflammation markers. Immigrant generation and time spent residing in the US may better capture cumulative exposure to US culture and stressors. Previous research on nativity and biomarker profiles in Mexican-origin immigrants have included only a limited number of inflammatory markers (Crimmins et al., 2007). A more thorough understanding of the influence of immigration history and biological precursors of disease risk may provide insights into health trajectories of Mexican-origin immigrants and their offspring, and may have strong potential for risk assessment using blood samples. To address the existing research gaps, this study examined the impact of immigration history, as defined by the time at which either the participant or their forbearers immigrated to the US (e.g. 1st, 2nd, 3rd generation or greater), and duration of time spent residing in the US among 1st generation immigrants on a comprehensive set of inflammatory markers including IL-6, CRP, soluble forms of type 1 and type 2 receptors of tumor necrosis factor-alpha (sTNF-R1 and sTNF-R2), adiponectin, and leptin using data from a large cohort of older predominantly Mexican-origin population.
METHODS
Sample
This study utilized baseline data from the Sacramento Area Latino Study on Aging (SALSA), a prospective study designed to study health status, cognitive decline, and dementia in older predominantly Mexican-origin adults living in the Sacramento Metropolitan Statistical Area (Haan et al., 2003). Eligible participants were ≥60 years at baseline in 1998 and self-identified as having Latino heritage. SALSA employed a two-stage sampling design. Census tracts in five contiguous counties were identified and characterized by the percentage of eligible residents. The tracts were then ranked in order of percentage eligible, and all tracts with a percentage eligible ≥5% were selected for the target population. A total of 1,789 participants were enrolled in the study and 51% (n=907) reported being born in Mexico (95% of the foreign-born sample). We restricted to participants with complete biomarker data (n=1,473). We employed listwise deletion and an additional 183 participants were excluded due to missing exposure data: nativity (n=6), parent place of birth (n=163), and duration of US residence (n=13) resulting in a final analytic sample of n=1,290. Participants excluded from the final analytic sample were older (71.6 years vs. 70.3 years), had lower educational attainment (6.7 years vs. 7.4 years) and monthly income (52.4% vs. 42.9% with <$1000 monthly gross income).
Immigration history
Immigration history was derived from measures of immigrant generation and duration of residence in the US. Self-reported origin of birth information for the SALSA participant and their parent was used to define immigrant generation. Participants were classified as: first generation Mexican-origin immigrant if they were foreign-born; second generation if they were US-born with at least one foreign-born parent; and third generation or higher if the participant and their parents were US-born. Second and third generation immigrants have been shown to have disparate risk of disease and exposure to social mobility; therefore, categorized separately (Afable-Munsuz et al., 2013; Haan et al., 2011). First generation Mexican-origin immigrants were further classified according to their duration of residence in the US: <15 years and ≥15 years (Creighton et al., 2012). This information was combined to create four categories of immigration history: 1) 1st generation residing in the US <15 years; 2) 1st generation residing in the US ≥15 years; 3) 2nd generation; and 4) 3rd generation or higher (≥3rd generation).
Inflammatory markers
Several biomarkers related to inflammation were examined in this study, including IL-6, sTNF-R1, sTNF-R2, CRP, leptin, and adiponectin. IL-6 is a pro-inflammatory cytokine that contributes to the development of coronary artery disease and type 2 diabetes independently (Danesh et al., 2008; Liu et al., 2016). CRP is a marker of low-grade inflammation and shown to play a role in the pathogenesis of atherosclerotic lesions in humans (Blake & Ridker, 2002). Leptin and adiponectin are adipocytokines with pro-inflammatory and anti-inflammatory properties, respectively, and have been shown to predict risk of cardiovascular disease and cancer (Iikuni et al., 2008; Ouchi & Walsh, 2007). Concentrations of soluble forms of receptor-bound TNF-alpha (sTNF-R1 and sTNF-R2) were examined as they have been shown to moderate the biological effects of TNF-α and can be measured with greater sensitivity and reliability than TNF-α (Aderka, 1996; Diez-Ruiz et al., 1995).
Venous blood samples were taken at baseline during home visits and stored at −70 °C. IL-6, sTNF-R1, and sTNF-R2 were assessed using the quantitative sandwich enzyme immunoassay technique (R&D Systems). High-sensitivity CRP was assessed using the CRP Ultra-Wide Range Reagent Kit, a latex-enhanced turbidimetric in-vitro immunoassay was used to assess high sensitivity CRP. Leptin and adiponectin were assessed using the radioimmunoassay kit (Linco Research Inc).
Other covariates
At baseline, demographic, social, behavioral, and health-related factors included in our study were collected from self-report, including age, gender, income level, education attainment, acculturation, physical activity, any alcohol consumption, any smoking, cancer, cardiovascular disease, and self-reported health. Age was self-reported and examined continuously. Gross household income for the last month was collected as: <$1000, $1000-$1499, $1500-$1999, $2000-$2499, and ≥$2500. We dichotomized household income as <$1000 vs. ≥$1000. Participants self-reported their highest number of years of education. Acculturation was derived from the Acculturation Rating Scale for Mexican Americans (ARSMA-II) where higher scores denote greater affinity to Anglo culture (Cuellar et al., 1995). Participants were asked, “How many hours per week do you spend on each of the following activities?” This included a list of 17 different activities (e.g. garden or yardwork, house repairs, walks, jog, bike ride, swim, or work out exercise, dance, light housework, heavy housework, etc.), which was used to calculate the number of hours per week the participant was physically active. Any alcohol consumption was collected from participants who were asked, “Do you ever drink [beer, wine, hard liquor]? Responses were then classified as ever vs. never drinkers of any alcohol. Smoking status was collected from participant responses to their smoking status: never smoked, former smoker, vs. current smoker. Because the prevalence of current smokers was only 10% in our sample, we collapsed this variable into two categories: never vs. ever smoked. Cardiovascular disease was self-reported at baseline. Diabetes was based on self-reported physician diagnosis, current use of diabetes medication, and/or a fasting glucose level ≥126 μg/dL. Participants self-reported their health status as excellent, very good, good, fair, or poor. Due to small proportion of participants who described their health as excellent or poor, we created a 3-level variable: excellent/very good, good, and fair/poor. Height in meters and weight in kilograms were measured by trained interviewers, which was used to classify body mass index (BMI) as normal (<25.0 kg/m2), overweight (25.0-29.9 kg/m2), and obese (≥30.0 kg/m2).
Statistical analysis
First, distributions of select baseline sociodemographic, lifestyle, and health characteristics by immigration history were compared using analysis of variance (ANOVA) for continuous variables and chi-square (χ2) for categorical variables. Because of skewed distributions, the inflammatory markers were natural log-transformed. Second, age- and sex-adjusted geometric mean inflammation levels were obtained using linear regression models and differences from 1st generation Mexican-origin immigrants with less than 15 years of US residence (the referent category) were estimated.
Third, multivariable linear regression was used to estimate the association of each log-transformed inflammatory marker with immigration history. Three separate models were estimated: (1) adjusted for age and gender; (2) adding education and income; and (3) adding adjustments for potential health-related—diabetes, cardiovascular disease, and self-reported health status—and behavioral mediating factors—smoking, physical activity, alcohol consumption, and BMI. To test whether associations differed across men and women and classifications of BMI, we tested whether inflammatory response to immigration history differed across gender and BMI. To increase interpretability of our model results, the model estimates are presented as percent differences with 95% confidence intervals (CI) from the reference group. All analyses were conducted using Stata software, version 14 (StataCorp, College Station, TX).
RESULTS
Distribution of select characteristics for the total sample and by immigration history is provided in Table 1. Of the 1,290 participants in the total sample, 42% reported monthly income less than $1,000, 59% were women, and 61% reported being married. On average, the participants were 70 years old, attained 7 years of education, and had a BMI of 30. More than half of the sample reported smoking in their lifetime (53%) and were current alcohol consumers (55%). Nearly 50% of the sample reported fair or poor health, 33% were classified as having a diabetes diagnosis, 22% reported a cardiovascular event, and 9% reported a cancer diagnosis. With regard to immigration history, 49% of the sample were 1st generation immigrants, of whom 15% had been living in the US for less than 15 years, while 41% were 2nd generation Mexican-origin immigrants and 11% were ≥3rd generation Mexican-origin immigrants. Socioeconomic factors also varied by immigration history. Mexican-origin immigrants who were ≥3rd generation attained higher levels of education, reported greater monthly income, and had higher acculturation scores. With regards to lifestyle factors and health status, a higher proportion ≥3rd generation Mexican-origin immigrants consumed alcohol and had higher prevalence of diabetes diagnosis.
Table 1.
Baseline characteristics by immigration history, Sacramento Area Latino Study on Aging (SALSA), n=1,290
| 1st generation | 2nd generation | 3rd generation | ||||
|---|---|---|---|---|---|---|
|
|
||||||
| Total Sample | <15 years | ≥15 years | Pa | |||
|
| ||||||
| (n=1290) | (n=95) | (n=534) | (n=525) | (n=136) | ||
| Sociodemographics | ||||||
| Age in years, mean ± SD | 70.3 ± 6.8 | 69.2 ± 7.8 | 71.0 ± 7.2 | 70.1 ± 5.9 | 69.2 ± 7.1 | <0.01 |
| Sex, n (%) | ||||||
| Male | 526 (41) | 26 (27) | 218 (41) | 225 (43) | 57 (42) | 0.04 |
| Female | 764 (59) | 69 (73) | 316 (59) | 300 (57) | 79 (58) | |
| Years of education, mean ± SD | 7.4 ± 5.3 | 3.2 ± 3.8 | 5.3 ± 4.7 | 9.5 ± 4.7 | 10.7 ± 5.2 | <0.001 |
| Monthly income <$1000, n (%) | ||||||
| <$1000 | 533 (42) | 81 (90) | 271 (52) | 146 (28) | 35 (26) | <0.001 |
| ≥$1000 | 738 (58) | 9 (10) | 253 (49) | 375 (72) | 101 (74) | |
| Married, n (%) | ||||||
| Married | 781 (61) | 49 (52) | 333 (62) | 315 (60) | 84 (62) | 0.26 |
| Non-married | 508 (39) | 46 (48) | 201 (38) | 209 (40) | 52 (38) | |
| Acculturation score, mean ± SDb | 22.5 ± 13.0 | 7.3 ± 4.4 | 14.5 ± 9.6 | 30.4 ± 10.2 | 33.4 ± 7.9 | <0.001 |
| Lifestyle | ||||||
| Physical activity score, mean ± SD | 17.4 ± 5.4 | 18.0 ± 5.3 | 17.8 ± 5.7 | 17.1 ± 5.2 | 16.9 ± 5.5 | 0.13 |
| Smoking status, n (%) | ||||||
| Never | 601 (47) | 51 (54) | 264 (50) | 231 (44) | 55 (41) | 0.07 |
| Ever | 687 (53) | 44 (46) | 269 (50) | 294 (56) | 80 (59) | |
| Any alcohol consumption, n (%) | ||||||
| No | 584 (45) | 49 (52) | 265 (50) | 222 (42) | 48 (36) | <0.01 |
| Yes | 705 (55) | 46 (48) | 269 (50) | 303 (58) | 87 (64) | |
| Body mass index (kg/m2), mean ± SD | 29.7 ± 5.7 | 29.3 ± 5.2 | 29.4 ± 5.5 | 29.9 ± 5.7 | 30.1 ± 6.4 | 0.33 |
| Health status | ||||||
| Self-reported health status, n (%) | ||||||
| Excellent/Very good | 256 (20) | 9 (10) | 80 (16) | 135 (26) | 32 (24) | <0.001 |
| Good | 403 (32) | 29 (32) | 154 (30) | 171 (33) | 49 (37) | |
| Fair/Poor | 596 (47) | 53 (58) | 277 (54) | 214 (41) | 52 (39) | |
| Diabetes diagnosis, n (%) | ||||||
| Yes | 424 (33) | 29 (31) | 146 (27) | 195 (37) | 54 (40) | <0.01 |
| No | 866 (67) | 66 (69) | 388 (73) | 330 (63) | 82 (60) | |
| Cardiovascular event, n (%) | ||||||
| Yes | 22 (22) | 12 (13) | 98 (18) | 133 (25) | 34 (25) | <0.01 |
| No | 1,010 (78) | 83 (87) | 435 (82) | 391 (75) | 101 (75) | |
P-vaue based on analysis of variance for continuous variables, chi-square test for categorical variables
Range for acculturation score: 0 – 56
Age- and sex-adjusted geometric means of inflammation biomarkers by immigration history are displayed in Table 2. IL-6, sTNF-R1, sTNF-R2, CRP, and leptin were highest among the ≥3rd generation immigrants. Compared to 1st generation immigrants with <15 years of US residence, ≥3rd generation immigrants had significantly higher CRP levels (p<0.05). Leptin levels were significantly higher for all categories of immigration history when compared to 1st generation immigrants with <15 years of US residence (p<0.001).
Table 2.
Age- and sex-adjusted geometric means (95% CI) biomarker levels by immigration history in the US, Sacramento Area Latino Study on Aging (SALSA), 1998 (n=1,290)
| 1st Generation | 2nd Generation | 3rd Generation | ||
|---|---|---|---|---|
|
|
||||
| <15 years | ≥15 years | |||
|
| ||||
| (n=95) | (n=534) | (n=525) | (n=136) | |
| Biomarkers a | ||||
| IL-6, pg/mL | 3.62 (3.14 – 4.18) | 3.45 (3.21 – 3.70) | 3.85 (3.58 – 4.13) | 4.14 (3.67 – 4.66) |
| sTNF-R1, pg/mL | 1609.9 (1492.7 – 1736.3) | 1525.9 (1469.7 – 1584.3) | 1629.4 (1567.0 – 1688.1) | 1674.5 (1572.5 – 1783.1) |
| sTNF-R2, pg/mL | 2609.4 (2426.8 – 2805.7) | 2366.9 (2283.1 – 2453.8)b | 2551.4 (2462.1 – 2643.9) | 2625.5 (2472.4 – 2788.0) |
| CRP, mg/L | 2.01 (1.56 – 2.59) | 1.99 (1.76 – 2.25) | 2.24 (1.98 – 2.53) | 2.89 (2.35 – 3.57)b |
| Leptin, ng/mL | 5.13 (4.44 – 5.92) | 7.08 (6.59 – 7.60)c | 7.93 (7.39 – 8.51)c | 7.71 (6.84 – 8.69)c |
| Adiponectin, ng/mL | 9015.0 (8136.5 – 9988.3) | 8783.1 (8348.6 – 9240.3) | 8872.7 (8436 – 9331.4) | 8965.1 (8232.6 – 9762.8) |
Adjusted for age and sex from generalized linear models.
Significantly different from 1st generation/<15 years duration of residence, p<0.05
Significantly different from 1st generation/<15 years duration of residence, p<0.001
Figure 1 displays the associations between immigration history and inflammation biomarkers as percent differences with 95% confidence intervals. Overall, we observed differences in inflammation profiles by immigration history after adjustment for sociodemographic factors (Model 2). Compared to 1st generation immigrants living in the US <15 years, IL-6 levels were 19.6% (95% CI: 2.3, 39.8) higher for 2nd generation and 30.6% (95% CI: 8.7, 56.8) higher for ≥3rd generation immigrants. Similar patterns of association were observed between STNF-R1, sTNF-R2, and CRP in relation to immigration history. Leptin levels were significantly higher for 1st generation immigrants residing in the US for at least 15 years (percent difference = 33.9; 95% CI: 15.3, 55.7), 2nd generation (percent difference = 45.9; 95% CI: 24.7, 70.7), and ≥3rd generation Mexican-origin immigrants (percent difference = 41.8; 95% CI: 17.7, 70.4) compared to 1st generation immigrants with <15 years of US residency. There was no evidence of an association between adiponectin and immigration history.
Figure 1.
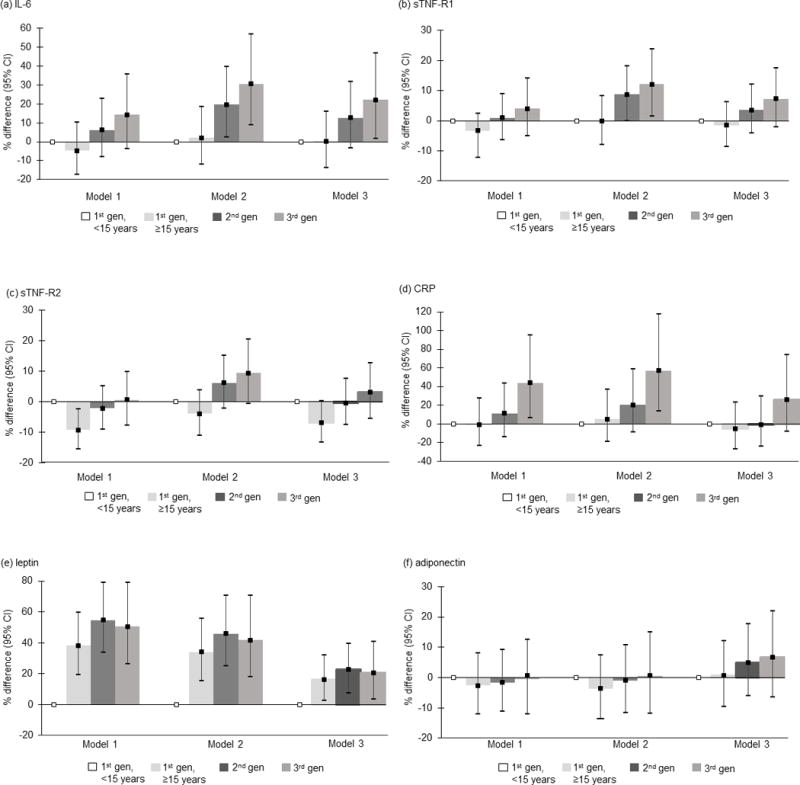
Associations of immigration history with with (a) IL-6; (b) sTNF-R1; (c) sTNF-R2; (d) CRP; (e) leptin; and (f) adiponectin levels. Model 1 represents the unadjusted association. Model 2 adjusts for age, gender, education, and income. Model 3 adjusts for diabetes, cardiovascular disease, arthritis, self-reported health status, smoking status, physical activity score, alcohol consumption, and body mass index.
Health-related and behavioral factors that may act as potential mediators of observed associations between immigration history and inflammation biomarker were examined to assess the robustness of our estimates (Model 3, Figure 1). Associations between immigration history and sTNF-R1 were mainly explained by behavioral and health-related factors. However, observed differences in IL-6, CRP, and leptin levels in relation to immigration history remained after additional adjustment for potential mediating pathways in Model 3. Lastly, effect modification by gender and BMI status was not found.
DISCUSSION
In a predominantly Mexican-origin population of older adults, our study provided evidence of an association between immigration history and inflammation biomarkers. Specifically, 2nd and 3rd generation Mexican-origin immigrants had worse inflammation profiles than 1st generation immigrants. In comparison to 1st generation immigrants with <15 years of US residence, IL-6 and leptin levels were higher for 2nd and ≥3rd generation Mexican-origin immigrants, independent of sociodemographic characteristics. Further, ≥3rd generation immigrants had higher levels of sTNF-R1 and CRP than 1st generation immigrants with <15 years of US residence. There was also evidence suggesting higher leptin levels among 1st generation Mexican-origin immigrants residing in the US for at least 15 years of US in comparison to 1st generation immigrants with less than 15 years of US residence.
The significant associations between immigration history and CRP are consistent with prior studies examining similar associations using data from the National Health and Nutrition Examination Survey (NHANES). Crimmins et al., reported higher inflammation risk—CRP, fibrinogen, and albumin—for US-born Mexicans than those born outside the US (Crimmins et al., 2007).
Leptin levels were also significantly higher among 1st generation immigrants with longer duration of US residence. Leptin functions as a pro-inflammatory cytokine that is highly correlated with energy balance and body fat and has been linked to chronic inflammation and inflammation-related diseases (Iikuni et al., 2008). Because of leptin’s association with energy balance, it is conceivable that longer duration of US residence results in higher levels of leptin through adoption of obesogenic behaviors. However, the observed associations remained significant after further adjustment for BMI and physical activity. Unfortunately, our data did not allow for the exploration of dietary behaviors, which are also known to change over time as immigrants become more assimilated to the diet of the host culture. Future studies are needed to explore whether dietary behaviors act as a mediator of the association between immigration history and leptin levels among US Hispanic immigrants.
Immigrant generation and time in the US may reflect assimilation to the US and the cumulative exposure to US social, cultural, behavioral and lifestyle risk factors. This hypothesis was partially explored in the fully adjusted models, which accounted for physical activity, BMI, smoking, and alcohol consumption in addition to health-related factors (e.g. cardiovascular disease, diabetes, and self-reported health). Associations between immigration history and IL-6 and leptin remained after inclusion of these lifestyle and health-related factors in our regression models. It is possible that other factors, such as psychosocial stressors and discrimination, play an important role in the association between immigration history and inflammation. Previous research in Hispanic populations have shown that as Hispanic immigrants live in the US longer and become more acculturated, they also self-report experiencing greater exposure to psychosocial stressors (Arellano-Morales et al., 2015; Perez et al., 2008), which have documented links to inflammation (Cunningham et al., 2012; Kershaw et al., 2016b; Lewis et al., 2010). Unfortunately, our study did not collect data on exposure to discrimination; therefore, it is important for future work to explore the role of discrimination in the association between immigration status and inflammation.
We did not find associations between immigration history and adiponectin levels. Adiponectin is an adipose-tissue derived hormone that exerts anti-inflammatory actions (Ouchi & Walsh, 2007). Given adiponectin’s anti-inflammatory properties, it is unlikely that we would observe increases in adiponectin levels by immigration history unless factors associated with immigration to the US produced significantly protective effect to increase adiponectin. For example, obesity and adiponectin are correlated (Arita et al., 1999) and obesity would need to be similarly associated with immigration history to increase adiponectin levels; however, obesity was not associated with immigration history in our study. What we would expect to find is decreasing adiponectin levels across immigration history (i.e. longer duration of residence and higher immigrant generation). There was suggestion of such associations when accounting for demographic factors (age, gender, income, and education); yet, paradoxically, higher adiponectin levels were observed when lifestyle- and health-related factors were included in the models. Future studies should further explore this finding to better understand adiponectin response to social and contextual factors, particularly among immigrant populations.
With the exception of sTNF-R2, similar patterns of associations were demonstrated across the pro-inflammatory markers examined, in that, Mexican-origin immigrants with longer immigration histories had higher levels of inflammation. We would expect to see similar patterns of associations between the pro-inflammatory markers, particularly IL-6 and CRP, as they are closely related to immune and related inflammatory response. However, the physiological processes of sTNF-R1 and sTNF-R2 are not as clear. sTNF-R1 is believed to modulate metabolic actions on TNF-α, including inflammatory response, and is present in almost all cell types (Diez-Ruiz et la., 1995). However, less is known about the role of sTNF-R2 and is not as prevalent across all cell types. The physiological nuance of sTNF-R2 might explain the associational differences observed, yet future research is warranted to better understand this biomarker.
The findings of our study have important implications in light of research documenting rising chronic disease risk among Mexican-origin immigrants. Upon arrival into the US, immigrants may experience what is known as a healthy immigrant effect (Antecol & Bedard, 2006), in which immigrants have a health advantage over demographically similar US-born individuals. However, over time and across generations this health advantage seems to diminish and the risk of chronic disease increases. While these associations have largely been attributed to behavioral and lifestyle changes, our findings suggest that immigration history may influence inflammatory markers through alternate pathways besides lifestyle factors and health-related factors. As a result, future studies of Hispanic immigrants’ health trajectories should consider the social experiences and stressors faced by immigrants and their offspring, and how these experiences may affect their health.
Our study had several limitations. First, we relied on cross-sectional data from baseline assessments, which precludes inferences of any causal effects. However, the link between immigration history and inflammation remains unknown and reduces the likelihood that our findings were influenced by participants’ recall of their age at migration or place of birth. Second, SALSA was a population-based study, which allows for conclusions about disease burden among Mexican Americans and immigrants in the Sacramento area. While our findings are unlikely generalizable to the experiences of Mexican-origin populations across the entire US, our results are generalizable to the Sacramento Mexican American population at the time that our study was conducted. Third, our sample comprised elderly community-dwelling Mexican-origin immigrants who were healthy and able to participate in the SALSA study. The average age of our participants at baseline was 70 years. We were unable to determine whether the findings of our study are a result of selection of healthy survivors; however, this is a limitation of all studies of elderly populations.
Despite these limitations, our study is one of the first to comprehensively investigate inflammation biomarkers in relation to immigration history among a primarily Mexican descent population. We found generational differences in several inflammation biomarkers that were independent of behavioral and health-related factors. These findings provide some preliminary evidence supporting inflammation as a potential pathway through which immigration experience leads to diminished health over time and across generations in US racial and ethnic minorities. Given the well-documented burden of chronic diseases among Mexican-origin immigrants, it is essential that future research studies aim to understand trajectories of biological risk as this population assimilates to identify specific tipping points and targets for intervention.
Supplementary Material
Acknowledgments
Funding: SALSA was supported by a grant from the National Institute on Aging, National Institute of Health (R01AG012975). Additional support for this work was provided by the National Cancer Institute (T32CA128582), and National Institute of Environmental Health Sciences (T32ES007018).
Footnotes
Disclosure Statement: The authors have no conflicts of interest to report.
References
- Aderka D. The potential biological and clinical significance of the soluble tumor necrosis factor receptors. Cytokine Growth Factor Rev. 1996;7:231–240. doi: 10.1016/s1359-6101(96)00026-3. [DOI] [PubMed] [Google Scholar]
- Afable-Munsuz A, Mayeda ER, Perez-Stable EJ, Haan MN. Immigrant generation and diabetes risk among Mexican Americans: the Sacramento Area Latino Study on Aging. Am J Public Health. 2013;103:e45–52. doi: 10.2105/AJPH.2012.300969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antecol H, Bedard K. Unhealthy assimilation: Why do immigrants converge to American health status levels? Demography. 2006;43:337–360. doi: 10.1353/dem.2006.0011. [DOI] [PubMed] [Google Scholar]
- Arellano-Morales L, Roesch SC, Gallo LC, Emory KT, Molina KM, Gonzalez P, et al. Prevalence and Correlates of Perceived Ethnic Discrimination in the Hispanic Community Health Study/Study of Latinos Sociocultural Ancillary Study. J Lat Psychol. 2015;3:160–176. doi: 10.1037/lat0000040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arita Y, Kihara S, Ouchi N, Takahashi M, Maeda K, Miyagawa J, et al. Paradoxical decrease of an adipose-specific protein, adiponectin, in obesity. Biochem Biophys Res Commun. 1999;257:79–83. doi: 10.1006/bbrc.1999.0255. [DOI] [PubMed] [Google Scholar]
- Blake GJ, Ridker PM. Inflammatory bio-markers and cardiovascular risk prediction. J Intern Med. 2002;252:283–294. doi: 10.1046/j.1365-2796.2002.01019.x. [DOI] [PubMed] [Google Scholar]
- Brown A, Patten E. Statistical Portrait of Hispanics in the United States, 2012. Washington, DC: Pew Research Center; 2014. [Google Scholar]
- Cook B, Alegria M, Lin JY, Guo J. Pathways and correlates connecting Latinos’ mental health with exposure to the United States. Am J Public Health. 2009;99:2247–2254. doi: 10.2105/AJPH.2008.137091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creighton MJ, Goldman N, Pebley AR, Chung CY. Durational and generational differences in Mexican immigrant obesity: is acculturation the explanation? Soc Sci Med. 2012;75:300–310. doi: 10.1016/j.socscimed.2012.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crimmins EM, Kim JK, Alley DE, Karlamangla A, Seeman T. Hispanic paradox in biological risk profiles. Am J Public Health. 2007;97:1305–1310. doi: 10.2105/AJPH.2006.091892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuellar I, Arnold B, Maldonado R. Acculturation Rating-Scale for Mexican-Americans Ii - a Revision of the Original Arsma Scale. Hispanic Journal of Behavioral Sciences. 1995;17:275–304. [Google Scholar]
- Cunningham TJ, Seeman TE, Kawachi I, Gortmaker SL, Jacobs DR, Kiefe CI, et al. Racial/ethnic and gender differences in the association between self-reported experiences of racial/ethnic discrimination and inflammation in the CARDIA cohort of 4 US communities. Soc Sci Med. 2012;75:922–931. doi: 10.1016/j.socscimed.2012.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danesh J, Kaptoge S, Mann AG, Sarwar N, Wood A, Angleman SB, et al. Long-term interleukin-6 levels and subsequent risk of coronary heart disease: two new prospective studies and a systematic review. PLoS Med. 2008;5:e78. doi: 10.1371/journal.pmed.0050078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez-Ruiz A, Tilz GP, Zangerle R, Baier-Bitterlich G, Wachter H, Fuchs D. Soluble receptors for tumour necrosis factor in clinical laboratory diagnosis. Eur J Haematol. 1995;54:1–8. doi: 10.1111/j.1600-0609.1995.tb01618.x. [DOI] [PubMed] [Google Scholar]
- Dinwiddie GY, Zambrana RE, Garza MA. Exploring risk factors in Latino cardiovascular disease: the role of education, nativity, and gender. Am J Public Health. 2014;104:1742–1750. doi: 10.2105/AJPH.2013.301280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon-Larsen P, Harris KM, Ward DS, Popkin BM. Acculturation and overweight-related behaviors among Hispanic immigrants to the US: the National Longitudinal Study of Adolescent Health. Soc Sci Med. 2003;57:2023–2034. doi: 10.1016/s0277-9536(03)00072-8. [DOI] [PubMed] [Google Scholar]
- Haan MN, Mungas DM, Gonzalez HM, Ortiz TA, Acharya A, Jagust WJ. Prevalence of dementia in older latinos: the influence of type 2 diabetes mellitus, stroke and genetic factors. J Am Geriatr Soc. 2003;51:169–177. doi: 10.1046/j.1532-5415.2003.51054.x. [DOI] [PubMed] [Google Scholar]
- Haan MN, Al-Hazzouri Z, Aiello AE. Life-span socioeconomic trajectory, nativity, and cognitive aging in Mexican Americans: the Sacramento Area Latino Study on Aging. J Gerontol B Psychol Sci Soc Sci. 2011;66B:i102–i110. doi: 10.1093/geronb/gbq071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iikuni N, Lam QL, Lu L, Matarese G, La Cava A. Leptin and Inflammation. Curr Immunol Rev. 2008;4:70–79. doi: 10.2174/157339508784325046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isasi CR, Ayala GX, Sotres-Alvarez D, Madanat H, Penedo F, Loria CM, et al. Is acculturation related to obesity in Hispanic/Latino adults? Results from the Hispanic community health study/study of Latinos. J Obes. 2015;2015:186276. doi: 10.1155/2015/186276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kershaw KN, Giacinto RE, Gonzalez F, Isasi CR, Salgado H, Stamler J, et al. Relationships of nativity and length of residence in the U.S. with favorable cardiovascular health among Hispanics/Latinos: The Hispanic Community Health Study/Study of Latinos (HCHS/SOL) Prev Med. 2016a;89:84–89. doi: 10.1016/j.ypmed.2016.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kershaw KN, Greenlund KJ, Stamler J, Shay CM, Daviglus ML. Understanding ethnic and nativity-related differences in low cardiovascular risk status among Mexican-Americans and non-Hispanic Whites. Prev Med. 2012;55:597–602. doi: 10.1016/j.ypmed.2012.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kershaw KN, Lewis TT, Diez Roux AV, Jenny NS, Liu K, Penedo FJ, et al. Self-reported experiences of discrimination and inflammation among men and women: The multi-ethnic study of atherosclerosis. Health Psychol. 2016b;35:343–350. doi: 10.1037/hea0000331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lara M, Gamboa C, Kahramanian MI, Morales LS, Bautista DE. Acculturation and Latino health in the United States: a review of the literature and its sociopolitical context. Annu Rev Public Health. 2005;26:367–397. doi: 10.1146/annurev.publhealth.26.021304.144615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le-Scherban F, Albrecht SS, Bertoni A, Kandula N, Mehta N, Diez Roux AV. Immigrant status and cardiovascular risk over time: results from the Multi-Ethnic Study of Atherosclerosis. Ann Epidemiol. 2016;26:429–435 e421. doi: 10.1016/j.annepidem.2016.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis TT, Aiello AE, Leurgans S, Kelly J, Barnes LL. Self-reported experiences of everyday discrimination are associated with elevated C-reactive protein levels in older African-American adults. Brain Behav Immun. 2010;24:438–443. doi: 10.1016/j.bbi.2009.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C, Feng X, Li Q, Wang Y, Li Q, Hua M. Adiponectin, TNF-alpha and inflammatory cytokines and risk of type 2 diabetes: A systematic review and meta-analysis. Cytokine. 2016;86:100–109. doi: 10.1016/j.cyto.2016.06.028. [DOI] [PubMed] [Google Scholar]
- Martin CL, Tate DF, Schaffner A, Brannen A, Hatley KE, Diamond M, Munoz-Christian K, Pomeroy J, Sanchez T, Mercado A, Hagobian T. Acculturation Influences Postpartum Eating, Activity, and Weight Retention in Low-Income Hispanic Women. J Womens Health (Larchmt) 2017;26:1333–1339. doi: 10.1089/jwh.2016.6154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouchi N, Walsh K. Adiponectin as an anti-inflammatory factor. Clin Chim Acta. 2007;380:24–30. doi: 10.1016/j.cca.2007.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papanicolaou DA, Wilder RL, Manolagas SC, Chrousos GP. The pathophysiologic roles of interleukin-6 in human disease. Ann Intern Med. 1998;128:127–137. doi: 10.7326/0003-4819-128-2-199801150-00009. [DOI] [PubMed] [Google Scholar]
- Perez DJ, Fortuna L, Alegria M. Prevalence and Correlates of Everyday Discrimination among U.S. Latinos. J Community Psychol. 2008;36:421–433. doi: 10.1002/jcop.20221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez LG, Chavez A, Marquez DX, Soto SC, Haughton J, Arredondo EM. Associations of acculturation with self-report and objective physical activity and sedentary behaviors among Latinas. Health Educ Behav. 2017;44:431–438. doi: 10.1177/1090198116669802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez-Escamilla R, Putnik P. The role of acculturation in nutrition, lifestyle, and incidence of type 2 diabetes among Latinos. J Nutr. 2007;137:860–70. doi: 10.1093/jn/137.4.860. [DOI] [PubMed] [Google Scholar]
- Perez-Escamilla R. Acculturation nutrition and health disparities in Latinos. Am J Clin Nutr. 2011;93:1163s–1167s. doi: 10.3945/ajcn.110.003467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steptoe A, Hamer M, Chida Y. The effects of acute psychological stress on circulating inflammatory factors in humans: a review and meta-analysis. Brain Behav Immun. 2007;21:901–912. doi: 10.1016/j.bbi.2007.03.011. [DOI] [PubMed] [Google Scholar]
- US Census Bureau, A.C.S. 2013 selected Population Profile in the United States, Hispanic or Mexican 2013 [Google Scholar]
- Viruell-Fuentes EA. Beyond acculturation: immigration, discrimination, and health research among Mexicans in the United States. Soc Sci Med. 2007;65:1524–1535. doi: 10.1016/j.socscimed.2007.05.010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


