Abstract
Work-related stressors are known to adversely affect employees’ stress physiology, including the cortisol awakening response (CAR) – or the spike in cortisol levels shortly after people wake up that aids in mobilizing energy. A flat or blunted CAR has been linked to chronic stress and burnout. This daily diary study tested the effects of a workplace intervention on employed parents’ CAR. Specifically, we tested whether the effects of the intervention on CAR were moderated by the type of days (workday versus non-work day). Data came from 94 employed parents from an information technology firm who participated in the baseline and 12-month diurnal cortisol components of the Work, Family, and Health Study, a group-randomized field experiment. The workplace intervention was designed to reduce work-family conflict (WFC) and implemented after the baseline data collection. Diurnal salivary cortisol was collected on 4 days at both baseline and 12 months. Multilevel modeling revealed that the intervention significantly increased employees’ CAR at 12 months on non-workdays, but this was not evident on workdays or for employees in the usual practice condition. The results provide evidence that the intervention was effective in enhancing employees’ biological stress physiology particularly during opportunities for recovery that are more likely to occur on non-work days.
Keywords: Cortisol awakening response (CAR), daily diary, workplace intervention, multilevel modeling
Introduction
Employed parents in the U.S. are finding it more difficult to balance their work and family responsibilities leading to increased work-family conflict (WFC) (Allen, Herst, Bruck, & Sutton, 2000; Nomaguchi, 2009; Winslow, 2005). WFC is defined as a type of work-related stressor that occurs when obligations and responsibilities from the work and family domains are incompatible (Greenhaus & Beutell, 1985). In addition to negatively affecting work organizations, WFC also has consequences for the health and well-being of employees and their families (Berkman et al., 2015; Fagan & Press, 2008). WFC is associated with negative health outcomes such as depression, physical symptoms, substance abuse, and sleep disorders (Buxton et al., 2016; Haines III, Marchand, Rousseau, & Demers, 2008; Jacobsen et al., 2014; Moen et al., 2015).
WFC may contribute to negative health outcomes directly via stress physiological pathways (Almeida et al., 2016) or indirectly by influencing health-related behaviors (Chandola et al., 2008). While the associations between WFC and psychological and physical health outcomes have been documented in the literature, it is not known if such links between work stress and stress physiology could be experimentally shown using a workplace intervention. This paper will assess whether the effects of a workplace intervention, which was found to significantly reduce employees’ WFC (Kelly et al., 2014), improves employees’ daily cortisol awakening response (CAR). This study will contribute to the work-family research, by showing the importance of organizational support, designed to decrease WFC that adversely affect employee health, for employees’ biological stress system functioning on a daily level. We will further assess whether the effects of a workplace intervention on employees’ CAR differs between workdays and non-workdays, information that helps improve future workplace intervention strategies and their effects on family life.
The role of CAR in health
Cortisol is a hormone secreted by the adrenal glands that affect the functioning of nearly every major organ in the body (de Kloet, Joels, & Holsboer, 2005; Sapolsky, Romero, & Munck, 2000). Secretion of cortisol has a distinct diurnal secretion pattern (Sapolsky et al., 2000). Cortisol levels are highest in the morning and gradually decline throughout the day with the lowest levels in the early part of the night (Sapolsky et al., 2000). Cortisol secretion also is characterized by a sharp spike in cortisol secretion in the first 30 min after waking in the morning called the CAR (Clow, Thorn, Evans, & Hucklebridge, 2004). CAR is responsible for mobilizing energy to prepare for daily activities. In recent years, researchers have increased attention on the role of CAR in health and well-being. Studies have found that demographic (e.g. age, socioeconomic status), health-related (e.g. chronic diseases), and psychosocial factors (e.g. stress, affect) are associated with alterations in CAR (Clow et al., 2004; Fries, Dettenborn, & Kirschbaum, 2009). A flat or blunted CAR is a biological marker of chronic stress (Klein et al., 2016). Data from numerous cross-sectional and longitudinal observational studies also suggest that a flat or blunted CAR, is associated with negative health outcomes, such as cardiovascular disease, depression, and diabetes (Baum, Cohen, & Hall, 1993; McEwen, 1998, 2007; Miller, Chen, & Zhou, 2007; Wüst, Federenko, Hellhammer, & Kirschbaum, 2000). Heightened CAR generally represents a healthy response (Clow et al., 2004; Miller et al., 2007).
Work-related stressors and CAR
There is evidence that chronic work-related stressor exposure is associated with alterations in CAR. However, the findings from these studies are inconsistent (Fries et al., 2009; Liao, Brunner, Kumari, & Oster, 2013). Some studies have reported that work-related stressors are associated with elevated CAR (Chandola et al., 2008), some studies have found no relation (Alderling, Theorell, de la Torre, & Lundberg, 2006; Liao et al., 2013), while other studies have reported that work-related stressors are associated with a blunted CAR (Grossi et al., 2005). These inconsistent findings have made it difficult for researchers to reach conclusions about the nature of the relation between work-related stressors and CAR.
The contradictory findings are possibly due to methodological differences between the studies. A majority of previous studies have only examined individual differences in average CAR. Most of these studies did not assess CAR across multiple days (e.g. Bellingrath, Weigl, & Kudielka, 2008; Hanson, Maas, Meijman, & Godaert, 2000; Kunz-Ebrecht, Kirschbaum, Marmot, & Steptoe, 2004). Previous inconsistent findings on the association between work-related stressors and CAR may be due to the fact that they did not take into account differences in CAR by the type of days (e.g. workday versus non-workday). Studies suggest the importance of considering the daily context of CAR (Clow, Hucklebridge, & Thorn, 2010; Fries et al., 2009; Mikolajczak et al., 2010). CAR tends to be lower on non-workdays compared to workdays (Schlotz, Hellhammer, Schulz, & Stone, 2004). This may be due to less anticipation of stress of the day, or more flexible morning schedules that are not bounded by preparation of work and school. Studying whether a workplace intervention can change employees’ CAR differently by workdays vs. non-workdays is important because employees’ behavior and physiology are greatly influenced by working around the social clock (Kelly & Moen, 2007).
Workplace interventions and the CAR
The most important contribution of this study is examining CAR in the context of a workplace intervention. Most previous work has used cross-sectional, observational designs to assess the association between work stress and CAR. These approaches make it difficult to rule out potential confounding variables that account for or suppress the association between work stress and CAR, such as socioeconomic status and physical health. Lab-based experimental studies may rule out some confounding variable problems, but they lack ecological validity (Powell, Liossi, Moss-Morris, & Schlotz, 2013).
To test a causal link between reductions in work stress and CAR in participants’ own naturalistic settings, we draw upon a group-randomized field experiment implemented among employees working in information technology (IT). This work setting is characterized by high WFC (Bray et al., 2013; Kelly et al., 2014). This workplace intervention, termed STAR (short for ‘Support-Transform-Achieve-Results’), was designed to decrease WFC by increasing workplace flexibility and support (Kossek, Hammer, Kelly, & Moen, 2014). As intended, the intervention resulted in decreased WFC and increased schedule control and supervisor support for family and personal life (Kelly et al., 2014). Moreover, the intervention has been shown to reduce perceived stress, emotional exhaustion, and psychological distress at 12 months for individuals in the IT industry (Moen et al., 2016) and those with elder care responsibilities in the extended care industry (Kossek et al., 2017). In addition, the intervention increased employees’ nightly sleep duration (Lee et al., 2016; Olson et al., 2015). Thus far, there is no research examining the effect of a workplace intervention on improving employees’ biological stress system functioning. This study aimed to test the effects of the STAR workplace intervention on employees’ CAR.
The effects of the intervention on employees’ CAR may be more evident when employees are free from the immediate demands of preparing for the workday. We consider non-work days to provide opportunities for employees to recover from work stress. The intervention may result in employees’ heightened CARs on non-work days by giving them more support for personal life and less interference from the work domain, all of which provide more opportunities for recovery at home. Blunted CARs on non-work days may reflect the stress of work spilling over into family life and disrupting restoration on non-work days. Thus, we expected that the STAR workplace intervention would increase employees’ CAR on ‘recovery’ days from work more so than on work days.
Theoretical background and hypotheses
Our study is situated in the work-home resources (W-HR) model (ten Brummelhuis & Bakker, 2012), which holds that work demands deplete employees’ personal resources, including physiological energy. In turn, these reduced resources influence performance in non-work domains. Correspondingly, work resources, such as schedule control and supervisor support for personal and family life, can increase personal resources, with positive implications for performance in non-work domains. Building upon the W-HR model (ten Brummelhuis & Bakker, 2012), we examined whether resource obtainment from a workplace intervention would have positive effects on employee stress physiology, including the CAR.
Based on the W-HR model (ten Brummelhuis & Bakker, 2012), we expected that the intervention would increase employees’ CAR across all days. We hypothesized that employees in the STAR intervention condition would display significantly increased CARs at 12 months compared to employees in the usual practice (UP) condition. In addition, we expected that the effect of the intervention on employee CARs would be more apparent on non-work days when employees can mentally and physically separate themselves from work-related stressors. This prediction is a consistent W-HR model, which posits that more work resources (i.e. support for family and personal life) and less work stress (i.e. less WFC) from the intervention will have positive effects in non-work domains. Differences in CAR by intervention condition may be less apparent on work days, because employees may anticipate work demands or stressors in the morning. We hypothesized that the effect of the intervention would be more evident on non-workdays when there are more opportunities for recovery compared to workdays.
Methods
Workplace intervention overview
We used data from IT employees in a large firm who participated in the daily diary sub-study of the Work, Family, and Health Study (WFHS). The WFHS involved a group-randomized, field experiment conducted in the IT division of a large U.S. company. A total of 56 study groups were randomized to either the STAR or UP conditions. The researchers worked with company representatives to identify study groups. The composition of study groups varied – some study groups were larger work teams of employees who reported to the same manager, and other study groups were comprised of multiple work teams who either reported to the same senior leadership or worked closely together (see Bray et al., 2013 for more information on the randomization design). The effects of the workplace intervention were assessed at multiple levels, such as the organization, work team, supervisor, employee, and family.
The STAR intervention was a multifaceted intervention designed to reduce WFC by increasing supervisor and coworker support for family and personal life and increasing employees’ control over when and where they worked (Bray et al., 2013; Kelly et al., 2014). STAR included (1) supervisory training on strategies to demonstrate support for employees’ personal and family lives while also supporting employees’ job performance and (2) participatory training sessions attended by employees (with managers present) to identify new work practices and processes to increase employees’ control over work time and focus on key results, rather than face time (i.e. the amount of time employees need to be visible in the workplace). The participatory sessions for employees took 8 h and managers attended an additional 4 h. Managers also participated in a facilitated training session specific to supervisors toward the end of the STAR roll-out; this provided an opportunity to share what was working well in their teams and to ask questions of facilitators and peers (for additional details on STAR, see Kossek et al., 2014; materials are available at www.workfamilyhealthnetwork.org).
Participants
Employees were eligible to participate in the WFHS if they were employees (not contractors) in a study group in one of the two data collection cities. A total of 823 employees completed interviews at the workplace prior to the implementation of the intervention. Trained researchers conducted interviews at the workplace at baseline, 6-, 12-, and 18-month post-STAR. Employees with a child ages 9 to 17 who lived at home at least four days a week (N = 222, 26.97% of the total sample, STAR: n = 110; UP: n = 112) were recruited to participate in a home interview with their child. This recruitment took place during the WFHS work site computer-assisted personal interviews (CAPIs). A total of 147 employees completed the home interview.
Out of the 147 employees who completed the home interview, 131 diary participants completed the baseline daily diary (89.1% response rate) and 102 employees completed the 12-month follow-up assessment (77.9% retention rate). The attriters (n = 29) were not different from the non-attriters (n = 102) on basic demographics, such as age (t(129) = 0.14, p = .89), gender (χ2 (1, N = 131) = 0.20, p = .65), marital status (χ2 (2, N = 131) = 0.96, p = .62), and household income (t(118) = −0.45, p = .65). They also did not differ in the main target variables of the intervention, including schedule control (t(129) = 0.44, p = .66), supervisor support (t(128) = −0.52, p = .61), and WFC (t(129) = 1.18, p = .24), and the rates of attrition did not significantly differ between the STAR and UP conditions (20.5% vs. 24.1%).
Among the 102 sample who provided daily diary data at baseline and 12 months, 94 employees (58 STAR, 36 UP) also provided their saliva samples both at baseline and 12 months. This is the final analytic sample of this study. Table 1 shows the demographic characteristics of the participants, by the intervention condition. There was no significant difference between the STAR and UP employees in sociodemographic background characteristics. Fifty-two percent were men and the mean age was 45.07 years (SD = 5.82). Sixty-nine percent were White, non-Hispanic. The majority (79%) had 4 or more years of college education and an additional 21% reported taking college courses (1–3 years) or graduating from technical school. Most (80.85%) were married, and the mean number of children was 2.04 (SD = 1.08). The mean annual household income ranged from $110,000–129,999. Average tenure with the company was 13 years (SD = 7.00). The mean number of work hours per week was 46.17 (SD = 5.85).
Table 1.
Baseline descriptive statistics, by the STAR workplace intervention condition.
| Total (N = 94)
|
STAR (n = 58)
|
UP (n = 36)
|
Diff Tests t-test/x2 |
||||
|---|---|---|---|---|---|---|---|
| M or % | (SD) | M or % | (SD) | M or % | (SD) | ||
| Gender (%) | |||||||
| Women | 47.87 | 53.45 | 38.89 | 1.89 | |||
| Men | 52.13 | 46.55 | 61.11 | ||||
| Age (in years) | 45.07 | (5.82) | 45.60 | (6.03) | 44.22 | (5.43) | −1.12 |
| Race (%) | |||||||
| White, Non-Hispanic | 69.15 | 68.97 | 69.44 | 0.00 | |||
| Non-Whitea | 30.85 | 31.03 | 30.56 | ||||
| Education (%) | |||||||
| College graduates | 78.72 | 77.59 | 80.56 | 0.12 | |||
| Some college or technical school | 21.28 | 22.41 | 19.44 | ||||
| Partnered status (%) | |||||||
| Married | 80.85 | 79.31 | 82.33 | 0.23 | |||
| Cohabiting | 6.38 | 6.90 | 5.56 | ||||
| Single | 12.77 | 13.79 | 11.11 | ||||
| Number of children | 2.04 | (1.08) | 1.95 | (0.85) | 2.19 | (1.37) | 0.97 |
| Household income rangeb | 8.55 | (3.02) | 8.81 | (2.91) | 8.14 | (3.17) | −1.03 |
| Company tenure | 13.04 | (7.00) | 13.70 | (7.62) | 11.98 | (5.83) | −1.16 |
| Work hours | 46.17 | (5.85) | 46.50 | (6.08) | 45.64 | (5.49) | −0.69 |
Non-White includes Hispanic, Asian Indian, Other Asian Indian, Other Pacific Islander, Black, and more than one race.
Household income ranges from 1 = Less than $49,999 to 12 = More than 150,000, and 8 indicates $110,000–119,999 and 9 indicates $120,000–129,999.
Procedure
Daily diary study procedure
Daily diary data collection involved a series of eight consecutive nightly telephone interviews conducted by a large University’s Survey Research Center. During the nightly telephone interviews, the employees were asked about their family experiences, physical and emotional well-being, and experiences of stress during the day of the call. The same protocol was used at the baseline and 12-month assessments. On average, the telephone interviews lasted about 20 min. The total incentive for the daily diary participants was $250 for both baseline and 12-month follow-up. Institutional Review Board approved the data collection protocol. Consent was obtained during the worksite Computer Aided Personal Interview (CAPI) after the field interviewers fully explained the procedures to the participants.
Daily saliva collection and assay procedure
During the home interview, field interviewers distributed home saliva collection kits to participants. The saliva collection kits included Salivettes with cotton swabs (20/kit; Sarstedt, Inc., Newton, NC) that participants used to collect their saliva samples. Participants were asked to provide 5 saliva samples (upon waking, 30 min after waking, before lunch, before dinner, and before going to bed at night) a day for four consecutive days (days 2–5 of daily diary phone calls) both at baseline and the 12-month follow-up. Thus, our sample of 94 employees contributed to total 752 cortisol days across the two time periods.
Specifically, participants were instructed to roll the cotton swab across their tongue for 2 min until the swab was completely saturated with saliva. Participants were also asked to record saliva collection times on a home saliva collection sheet at the end of the day. Instructions for saliva collection and questionnaire completion were provided on a digital video as part of their recruitment and also were reviewed during the first daily diary telephone interview. As saliva samples are sensitive to several confounds, participants were asked during the daily interviews to report medication use (including steroids; Granger, Hibel, Fortunato, & Kapelewski, 2009), tobacco smoking status and, for females, menstrual cycle information (Kirschbaum, Kudielka, Gaab, Schommer, & Hellhammer, 1999).
Participants were asked to keep samples refrigerated until the end of the saliva collection period when they shipped saliva samples via overnight pre-addressed, pre-paid courier packages to the Biomarker Core Laboratory at the research site of the current study. Samples were shipped after the daily diary was completed for baseline, and also when the daily diary was completed 12 months after the intervention. Upon receipt the morning after being shipped, saliva samples were immediately were frozen at −80°C until assayed. Saliva samples were assayed for salivary free (unbound) cortisol in duplicate in a single assay batch per participant via a commercially available enzyme immunoassay (EIA; Salimetrics LLC). The sample test volume was 25 μL of saliva (for singlet determinations). The assay had had a range of sensitivity from 0.007 to 1.8 μg/dL, with average inter- and intra-assay coefficient covariances of less than 10% and 5%, respectively. Cortisol values were converted from μg/dL to nmol/L (μg/dL * 27.59).
Measures
Burst
Because the data involved two time points – baseline and 12 months later, a burst variable was created to examine changes between the baseline and 12-month bursts (1 = 12 months, 0 = baseline).
Within-person level (WP) workplace intervention effects
We created a WP STAR variable to effectively compare changes from baseline to 12 months between STAR and UP. Because all baseline assessments were conducted prior to the STAR implementation, all participants were coded as 0 at the baseline assessment. Employees who were assigned to the STAR condition were coded as 1 at 12 months (i.e. after the intervention was implemented), and employees who were assigned to UP condition were coded as 0 at the 12-month assessment. Thus, this variable combines burst with condition by indicating whether individuals in the STAR condition change CAR at 12 months compared to their baseline assessments. Using the WP STAR variable is especially helpful when examining changes in CAR by the type of days, because it avoids using a three-way interaction (burst × condition × type of day), while estimating the same effect. A basic assumption for using the WP STAR is that there must no difference between the STAR and UP at baseline in levels of CARs and CARs by type of day. Results from t-tests indeed showed that there was no baseline difference between the STAR and UP condition in terms of their CARs (t(391) = 1.12, p = .26) and CARs on workdays (t(271) = 1.54, p = .13) as well as on non-workdays (t(112) = −0.56, p = .58). Therefore, our assumption was justified.
Type of day item came from time use questions that were adapted from the Daily Inventory of Stressful Events (Almeida, 2005). We asked, ‘Since this time yesterday, did you work at your [primary] job?’ Responses were coded as 1 (= workday) or 0 (= non-work day).
CAR (nmol/L) was calculated for each saliva collection day by subtracting cortisol sample upon waking from cortisol sample 30 min after waking. Thus, the difference in CAR between these two time points each day indicates CAR. In line with other studies on chronic stress and burnout, higher scores reflect a more active CAR (Miller et al., 2007).
Covariates
Employees’ gender (1 = male, 0 = female), age, educational level, and race (1 = white, 0 = non-white) were included in our analysis as demographic controls. Because STAR and UP differed in the levels of schedule control at baseline among this study sample, we also controlled for the extent of schedule control measured by Thomas and Ganster’s (1995) Control over Work Schedule Scale (8 items). Moreover, between baseline and 12 months, there was an announcement of an organizational merger. Data collection was staggered so some respondents were informed about the merger before the baseline survey, while others were not. To take into account potential differences from this, we included an indicator of the timing of baseline data collection as compared to the merger announcement (1 = post-merger announcement, 0 = pre-merger announcement) in our analysis. We also took into account employees’ smoking status and other tobacco use status (1 = yes, 0 = no), medication known to affect cortisol secretion (e.g. Estrogen, Depo-Provera; 1 = used, 0 = not used), body mass index, time of saliva sample A (waking time), and saliva collection day (0 = first day to 3 = fourth day) in our analyses. All continuous variables were centered at the sample mean. In addition, a cortisol flag variable was created to test and adjust for potential measurement concerns (Stawski, Cichy, Piazza, & Almeida, 2013). The flag variable indicates whether an individual was awake for less than 12 or more than 20 h, woke up after 12:00 pm, a later biological or circadian time that might attenuate CAR effects, or if there was less than 15 or greater than 60 min between the first and second cortisol samples (i.e. outside of the standard CAR window of sampling).
Statistical analyses
To decompose level 1 (within-person level) and level 2 (between-person level) variances in CAR as a function of burst, WP STAR, and type of day, multilevel models were conducted using SAS 9.3 (Raudenbush & Bryk, 2002). Below equations describe our analytic models. β1i represents changes in CAR from baseline to 12 months. β2i indicates the WP STAR effect which is the difference between the STAR and UP employees’ changes in CAR from baseline to 12 months (which can be understood as a difference-in-difference estimator). β3i means differences in CAR by work days versus non-work days, while β4i indicates how changes in STAR employees’ CAR from baseline to 12-month differ by type of day.
Within-person
| Level 1 |
Between-person
| Level 2 |
Results
Before conducting multilevel models with predictors, we calculated Intra-Class Correlations to examine variance components in employees’ CAR. Of the total variance in CAR, 24% was due to differences between persons, and 76% was attributable to day-today fluctuations within persons. This suggests that the use of multilevel modeling is appropriate (Raudenbush & Bryk, 2002). More variance in the daily level also supports the necessity of investigating CAR by type of days. Among the total 752 cortisol days clustered within 94 employees, 556 days were work days and 196 days were non-work days.
Table 2 presents results from multilevel models predicting employees’ CAR. First of all, several variables, such as schedule control and race/ethnicity, were added to the model as covariates in order to control for any potential confounds. Results indicated that many of these variables were associated with CAR. Employees displayed significantly higher CARs if they reported greater schedule control (B = 1.49, SE = .54, p < .01), identified their race/ethnicity as White (B = 1.91, SE = .88, p < .05), they took medications known to affect cortisol secretion (B = 2.06, SE = .88, p < .05), and woke up earlier than usual on that day (B = −1.20, SE = .23, p < .001). Model 1 indicates the effect of WP STAR on changes in CAR from baseline to 12 months. There was no significant effect of burst, indicating that the levels of CAR were not significantly different between baseline and the 12-month assessment. The type of day (work or non-work day) also did not significantly predict employees’ CAR: levels of CAR did not differ between workdays and non-work days, overall. Moreover, contrary to our first hypothesis, WP STAR alone was not a significant predictor of CAR. Employees in the STAR condition did not significantly increase in CAR from baseline to 12 months, compared to the UP employees.
Table 2.
Changes in CAR as a function of a workplace intervention (STAR).
| Model 1
|
Model 2
|
|||
|---|---|---|---|---|
| Estimate | (SE) | Estimate | (SE) | |
| Fixed effects | ||||
| Intercept | 1.28 | (3.73) | 0.96 | (3.74) |
| Burst (12 months) | 1.37 | (0.73) | 1.30 | (0.73) |
| Type of day (Workday) | 0.62 | (0.62) | 1.28 | (0.69) |
| WP STAR | −0.93 | (0.81) | 1.11 | (1.23) |
| WP STAR × Type of Day | – | – | −2.60* | (1.19) |
| Random effects | ||||
| Variance intercept (ID) | 10.01*** | (2.30) | 10.06*** | (2.30) |
| Variance residual | 35.87*** | (2.01) | 35.65*** | (2.00) |
Note: Model 1 shows the main effect of the STAR workplace intervention on changes in CAR; Model 2 shows the effect of the STAR workplace intervention on changes in CAR by the type of days (workdays vs. non-workdays). Gender, age, race, educational level, days of study, levels of schedule control, merger announcement indicator, smoking and other tobacco use status, medication use, BMI, time of saliva sample A, and cortisol flag variables were included in the analysis as control variables. Total 752 valid observations were obtained from 94 employees across the two bursts.
Model 2 further shows the effect of STAR on changes in CAR by the type of days (workday vs. non-workday). There was a significant interaction between WP STAR and type of the day predicting CAR. Employees in the STAR condition showed increased levels of CAR at 12 months compared to their baseline levels, but this effect was only evident on non-work days (see Figure 1). There was no effect on workdays and for the UP employees. Therefore, our hypothesis based on the W-HR model (ten Brummelhuis & Bakker, 2012) that the effect of STAR on increased CAR would be more evident on non-work days rather than on workdays was supported.
Figure 1.
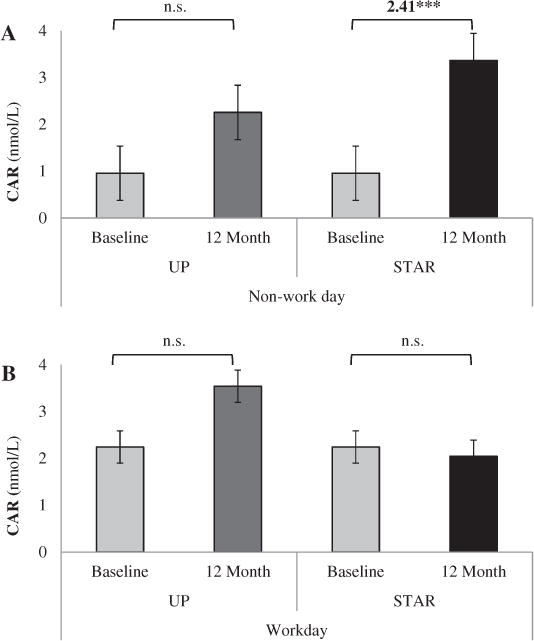
Moderating effect of type of days in the effect of a workplace intervention (STAR) versus UP on employees’ CAR. Note: Panel A shows the significant effect of the intervention on non-work days. STAR employees significantly increased CARs on non-work days at 12 months compared to their baseline (B = 2.41, SE = 1.07, p < .05); UP employees did not significantly increase. Panel B shows non-significant effect of the intervention on workdays. The effects were adjusted for covariates.
Discussion
Guided by the Work-Home Resources (W-HR) Model (ten Brummelhuis & Bakker, 2012), the goal of this study was to investigate the effects of a workplace intervention – shown to reduce employees’ WFC (Kelly et al., 2014) – on IT employees’ Cortisol Awakening Response or CAR. CAR is an indicator of the body’s ability to mobilize energy to initiate daily activities. As such a blunted or diminished CAR can be interpreted as fatigue and burnout. Our findings revealed that the STAR workplace intervention was effective in enhancing employees’ CAR on non-work days at the 12-month post-intervention follow-up compared to their baseline. This result is noteworthy because it shows within-person changes in CAR (after ruling out between-person differences) among employees who received the intervention, but not among employees in the control condition. This study adds to the work-family literature by demonstrating the positive workplace intervention effects on employees’ physiological response evident on non-work days. The STAR workplace intervention resulted in within-person level increased CAR on non-workdays, which may be translated as more mobilization of energy on days that employees are recovering from work.
Building on prior correlational research, often collected at one point in time, on the associations between work-related stressors and CAR, this study utilized daily diary data collected before and after a group-randomized field experiment to test whether the STAR intervention affected employees’ CAR and how the effects differed by the type of days (i.e. workdays and non-work days). There was no main effect of STAR on employees’ CAR across day, but, we found a significant interaction effect between STAR and the type of days predicting employees’ CAR. Compared to UP employees, the employees in the STAR group displayed increased CARs from baseline to 12 months on non-workdays, but this was not the case on workdays. To the extent that the social clock (i.e. morning schedules) influences employee behaviors (Kelly & Moen, 2007), the intervention might not have been able to change employee CARs on workdays when the morning times are routinized and rather hectic. In contrast, non-workdays may be less bounded by a strict social clock and have allowed the intervention employees perceive more temporal and psychological resources in the morning times (W-HR; ten Brummelhuis & Bakker, 2012). By reducing WFC (Kelly et al., 2014) the intervention decreased an important source of chronic stress that was evidenced by a heightened CAR on non-work days. Restorations of CAR on non-work may help mobilize energy in these employed parents to manage family needs and responsibilities.
Results from past research examining the associations between work-related stressors and CAR (i.e. at the between-person level – individual differences in CAR with respect to the amount of morning rise) are inconsistent (Fries et al., 2009; Liao et al., 2013), with studies finding that work-related stressors are associated with elevated CAR (Chandola et al., 2008), diminished CAR (Grossi et al., 2005), or no relation (Alderling et al., 2006; Liao et al., 2013). Results from the present experimental study found no relation between the implementation of a workplace intervention (which previous research found to be associated with WFC; Kelly et al., 2014) and average CAR across days. The lack of findings for average CAR is not surprising, given that only about 25% of the variance in CAR occurred at the between-person level.
A majority of the variance in CAR occurred at the within-person level, across days of the study, which provided strong evidence for the importance of examining the role of the intervention on CAR across daily contexts. This finding is in line with previous research that highlighted the need for studying CAR in context (Clow et al., 2010). The present study found that the intervention increased CAR on non-work days. The results support previous research by Mikolajczak and colleagues (2010) that found perceived stress to be associated with lower CAR on weekends. Thus, the STAR intervention, known to decrease WFC, increased CAR on ‘recovery’ days from work. Blunted CARs on non-work days may reflect the stress of work spilling over into family life and disrupting restoration on non-work days. Our results show that the STAR intervention increased the mobilization of energy (i.e. higher CAR) on these non-work days suggesting the employed parents can take better advantage of these recovery days. This effect was robust after controlling for the effects of employees’ sociodemographic and work characteristics as well as bio-behavioral markers (e.g. BMI, smoking status) and waking and saliva collection times that may affect CAR.
Limitations and future research directions
In this study, we attempted to address methodological gaps in previous studies by utilizing a group field experiment design and incorporating multiple CAR days and more workdays and non-work days than previously considered in past research. Nonetheless, our study has limitations. First, although our sample was randomly selected from the IT division of a large company, it does not represent the whole IT industry. Our findings may not be generalizable to all employees in the IT industry. Also, it is unclear whether our results would be replicated in other types of industries, which may have different work stressors or metabolic demands. Second, this study compared CARs on workdays versus non-workdays. However, there may be other factors that contribute to differences in CAR by the type of days. For example, some employed parents might have enjoyable events during non-workdays, like sport activities with their child or family gatherings, and such events might increase their CARs regardless of the extent of WFC they experienced. On the other hand, those UP employees not subjected to the favorable intervention may have found their non-work day to include more work or career-related stressors that make their stress physiology more identical to a workday. Other possible factors, including specific events happening on that day, and the indirect effect of STAR through diminished WFC on employees’ CAR should be carefully considered and examined in future studies. Unfortunately our sample size and the number of collection days precluded our ability to carry out these analyses.
For future directions, researchers should examine how specific aspects of work-related stressors, such as the duration of stressor exposure and the type of work-related stressors, affect CAR (Fries et al., 2009; Miller et al., 2007). Longitudinal research may be particularly important when studying CAR and how the duration of stressor exposure plays a role. It is plausible that work-related stressors initially may lead to elevations in CAR, but, over time, chronic exposure to work-related stressors may lead to a diminished CAR (Fries et al., 2009; Miller et al., 2007). Prospective studies are also needed to clarify the longer term trajectories of CAR. Furthermore, work-related stressors may affect CAR differently depending on the type of stressors (e.g. WFC, physical work conditions, job insecurity), and future studies should investigate the relations between specific types of work-related stressors and CAR. In addition, future research should examine the effects of non-workday heightened CAR on long-term health outcomes.
Conclusion
In conclusion, this study investigated the effects of a workplace intervention targeting WFC on employees’ CAR. Although the effect of the intervention was not apparent on average CAR across days, it had an effect on increased CAR on non-workdays. The findings suggest that this workplace intervention, which has been found to have positive implications for employees’ WFC (Kelly et al., 2014), emotional exhaustion (Moen et al., 2016), family functioning (Davis et al., 2015), and sleep health (Lee et al., 2016; Olson et al., 2015), and also has positive implications for employees’ physiological functioning. Findings from this study may be informative for researchers seeking to better understanding the mechanism through which work-related factors change employees’ adaptive physiological responses and also to practitioners seeking to develop more specific logic models for future workplace interventions.
Acknowledgments
The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of these institutes and offices.
Funding
This research was conducted as part of the Work, Family and Health Network, which is funded by a cooperative agreement through the National Institutes of Health and the Centers for Disease Control and Prevention: National Institute of Child Health and Human Development (U01HD051217, U01HD051218, U01HD051256, U01HD051276), National Institute on Aging (U01AG027669), Office of Behavioral and Social Sciences Research, and National Institute for Occupational Safety and Health (U010H008788). Special acknowledgement goes to Extramural Staff Science Collaborator, Rosalind Berkowitz King, PhD (NICHD) and Lynne Casper, PhD (now of the University of Southern California) for design of the original Workplace, Family, Health and Well-Being Network Initiative. We also thank Alfred P. Sloan Foundation (2004-12-4), The W.T. Grant Foundation (9844), The Penn State General Clinical Research Center (NIH Grant M01-RR-10732), and the Penn State Social Science Research Institute for providing additional support for this research.
Footnotes
Disclosure statement
No potential conflict of interest was reported by the authors.
Notes on contributors
David M. Almeida is a professor at the Pennsylvania State University in the department of Human Development and Family Studies and affiliated with the Center for Healthy Aging.
Soomi Lee is an assistant research professor at the Pennsylvania State University in the department of Biobehavioral Health and affiliated with the Center for Healthy Aging.
Kimberly N. Walter is a postdoctoral fellow, NIAAA T32 Institutional Training Grant at the University of Connecticut School of Medicine in the department of Psychiatry.
Katie M. Lawson is an assistant professor at Ball State University in the department of Psychological Science.
Erin L. Kelly is a professor in Work and Organization Studies at the MIT Sloan School of Management and affiliated with the Institute for Work and Employment Research.
Orfeu M. Buxton is an associate professor at the Pennsylvania State University in the department of Biobehavioral Health, an assistant professor at Harvard Medical School in the Division of Sleep Medicine, associate neuroscientist at Brigham and Women’s Hospital in the department of Medicine, and an adjunct associate professor at Harvard Chan School of Public Health in the Department of Social and Behavioral Sciences.
References
- Alderling M, Theorell T, de la Torre B, Lundberg I. The demand control model and circadian saliva cortisol variations in a Swedish population based sample (The PART study) BMC Public Health. 2006;6(1):288. doi: 10.1186/1471-2458-6-288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen TD, Herst D, Bruck CS, Sutton M. Consequences associated with work-to-family conflict: A review and agenda for future research. Journal of Occupational Health Psychology. 2000;5(2):278–308. doi: 10.1037/1076-8998.5.2.278. [DOI] [PubMed] [Google Scholar]
- Almeida DM. Resilience and vulnerability to daily stressors assessed via diary methods. Current Directions in Psychological Science. 2005;14(2):64–68. doi: 10.1111/j.0963-7214.2005.00336.x. [DOI] [Google Scholar]
- Almeida DM, Davis KD, Lee S, Lawson KM, Walter KN, Moen P. Supervisor support buffers daily psychological and physiological reactivity to work-to-family conflict. Journal of Marriage and Family. 2016;78(1):165–179. doi: 10.1111/jomf.12252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baum A, Cohen L, Hall M. Control and intrusive memories as possible determinants of chronic stress. Psychosomatic Medicine. 1993;55(3):274–286. doi: 10.1097/00006842-199305000-00005. [DOI] [PubMed] [Google Scholar]
- Bellingrath S, Weigl T, Kudielka BM. Cortisol dysregulation in school teachers in relation to burnout, vital exhaustion, and effort-reward-imbalance. Biological Psychology. 2008;78(1):104–113. doi: 10.1016/j.biopsycho.2008.01.006. [DOI] [PubMed] [Google Scholar]
- Berkman LF, Liu SY, Hammer L, Moen P, Klein LC, Kelly E, Buxton OM. Work-family conflict, cardiometabolic risk, and sleep duration in nursing employees. Journal of Occupational Health Psychology. 2015;20:420–433. doi: 10.1037/a0039143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bray J, Kelly E, Hammer L, Almeida D, Dearing J, King R, Buxton O. An integrative, multilevel, and transdisciplinary research approach to challenges of work, family, and health. Methods Report (RTI Press) 2013:1–38. doi: 10.3768/rtipress.2013.mr.0024.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buxton OM, Lee S, Beverly C, Berkman LF, Moen P, Kelly EL, Almeida DM. Work-family conflict and employee sleep: Evidence from IT workers in the work, family and health study. Sleep. 2016;39(10):1911–1918. doi: 10.5665/sleep.6172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandola T, Britton A, Brunner E, Hemingway H, Malik M, Kumari M, Marmot M. Work stress and coronary heart disease: What are the mechanisms? European Heart Journal. 2008;29(5):640–648. doi: 10.1093/eurheartj/ehm584. [DOI] [PubMed] [Google Scholar]
- Clow A, Hucklebridge F, Thorn L. The cortisol awakening response in context. International Review of Neurobiology. 2010;93:153–175. doi: 10.1016/S0074-7742(10)93007-9. [DOI] [PubMed] [Google Scholar]
- Clow A, Thorn L, Evans P, Hucklebridge F. The awakening cortisol response: Methodological issues and significance. Stress-the International Journal on the Biology of Stress. 2004;7(1):29–37. doi: 10.1080/10253890410001667205. [DOI] [PubMed] [Google Scholar]
- Davis KD, Lawson KM, Almeida DM, Kelly EL, King RB, Hammer L, McHale SM. Parents’ daily time with their children: A workplace intervention. Pediatrics. 2015;135(5):875–882. doi: 10.1542/peds.2014-2057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Kloet ER, Joels M, Holsboer F. Stress and the brain: from adaptation to disease. Nature Reviews Neuroscience. 2005;6(6):463–475. doi: 10.1038/nrn1683. [DOI] [PubMed] [Google Scholar]
- Fagan J, Press J. Father influences on employed mothers’ work-family balance. Journal of Family Issues. 2008;29(9):1136–1160. doi: 10.1177/0192513X07311954. [DOI] [Google Scholar]
- Fries E, Dettenborn L, Kirschbaum C. The cortisol awakening response (CAR): Facts and future directions. International Journal of Psychophysiology. 2009;72(1):67–73. doi: 10.1016/j.ijpsycho.2008.03.014. [DOI] [PubMed] [Google Scholar]
- Granger DA, Hibel LC, Fortunato CK, Kapelewski CH. Medication effects on salivary cortisol: Tactics and strategy to minimize impact in behavioral and developmental science. Psychoneuroendocrinology. 2009;34(10):1437–1448. doi: 10.1016/j.psyneuen.2009.06.017. [DOI] [PubMed] [Google Scholar]
- Greenhaus JH, Beutell NJ. Sources of conflict between work and family roles. Academy of Management Review. 1985;10(1):76–88. doi: 10.5465/AMR.1985.4277352. [DOI] [Google Scholar]
- Grossi G, Perski A, Ekstedt M, Johansson T, Lindström M, Holm K. The morning salivary cortisol response in burnout. Journal of Psychosomatic Research. 2005;59(2):103–111. doi: 10.1016/j.jpsychores.2005.02.009. [DOI] [PubMed] [Google Scholar]
- Haines VY, III, Marchand A, Rousseau V, Demers A. The mediating role of work-to-family conflict in the relationship between shiftwork and depression. Work and Stress. 2008;22(4):341–356. doi: 10.1080/02678370802564272. [DOI] [Google Scholar]
- Hanson EKS, Maas CJM, Meijman TF, Godaert GLR. Cortisol secretion throughout the day, perceptions of the work environment, and negative affect. Annals of Behavioral Medicine. 2000;22(4):316–324. doi: 10.1007/BF02895668. [DOI] [PubMed] [Google Scholar]
- Jacobsen HB, Reme SE, Sembajwe G, Hopcia K, Stoddard AM, Kenwood C, Buxton OM. Work-family conflict, psychological distress, and sleep deficiency among patient care workers. Workplace Health & Safety. 2014;62(7):282–291. doi: 10.3928/21650799-20140617-04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly EL, Moen P. Rethinking the clockwork of work: Why schedule control may pay off at work and at home. Advances in Developing Human Resources. 2007;9(4):487–506. doi: 10.1177/1523422307305489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly EL, Moen P, Oakes JM, Fan W, Okechukwu C, Davis KD, Casper LM. Changing work and work-family conflict: Evidence from the work, family, and health network. American Sociological Review. 2014;79(3):485–516. doi: 10.1177/0003122414531435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirschbaum C, Kudielka BM, Gaab J, Schommer NC, Hellhammer DH. Impact of gender, menstrual cycle phase, and oral contraceptives on the activity of the hypothalamus-pituitary-adrenal axis. Psychosomatic Medicine. 1999;61(2):154–162. doi: 10.1097/00006842-199903000-00006. [DOI] [PubMed] [Google Scholar]
- Klein LC, Kim K, Almeida DM, Femia EE, Rovine MJ, Zarit SH. Anticipating an easier day: Effects of adult day services on daily cortisol and stress. The Gerontologist. 2016;56(2):303–312. doi: 10.1093/geront/gnu060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kossek EE, Hammer LB, Kelly EL, Moen P. Designing work, family & health organizational change initiatives. Organizational Dynamics. 2014;43:53–63. doi: 10.1016/j.orgdyn.2013.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kossek EE, Thompson RJ, Lawson KM, Bodner T, Perrigino MB, Hammer LB, Berkman LF. Caring for the elderly at work and home: Can a randomized organizational intervention improve psychological health? Journal of Occupational Health Psychology. 2017 doi: 10.1037/ocp0000104. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunz-Ebrecht SR, Kirschbaum C, Marmot M, Steptoe A. Differences in cortisol awakening response on work days and weekends in women and men from the Whitehall II cohort. Psychoneuroendocrinology. 2004;29:516–528. doi: 10.1016/S0306-4530(03)00072-6. [DOI] [PubMed] [Google Scholar]
- Lee S, Almeida DM, Berkman L, Olson R, Moen P, Buxton OM. Age differences in workplace intervention effects on employees’ nighttime and daytime sleep. Sleep Health. Advance Access Publication. 2016;2:289–296. doi: 10.1016/j.sleh.2016.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao J, Brunner EJ, Kumari M, Oster H. Is there an association between work stress and diurnal cortisol patterns? Findings from the Whitehall II study. PloS One. 2013;8(12):e81020. doi: 10.1371/journal.pone.0081020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen BS. Stress, adaptation, and disease: Allostasis and allostatic load. Annals of the New York Academy of Sciences. 1998;840(1):33–44. doi: 10.1111/j.1749-6632.1998.tb09546.x. [DOI] [PubMed] [Google Scholar]
- McEwen BS. Physiology and neurobiology of stress and adaptation: Central role of the brain. Physiological Reviews. 2007;87(3):873–904. doi: 10.1152/physrev.00041.2006. [DOI] [PubMed] [Google Scholar]
- Mikolajczak M, Quoidbach J, Vanootighem V, Lambert F, Lahaye M, Fillée C, de Timary P. Cortisol awakening response (CAR)’s flexibility leads to larger and more consistent associations with psychological factors than CAR magnitude. Psychoneuroendocrinology. 2010;35(5):752–757. doi: 10.1016/j.psyneuen.2009.11.003. [DOI] [PubMed] [Google Scholar]
- Miller GE, Chen E, Zhou ES. If it goes up, must it come down? Chronic stress and the hypothalamic-pituitary-adrenocortical axis in humans. Psychological Bulletin. 2007;133(1):25–45. doi: 10.1037/0033-2909.133.1.25. [DOI] [PubMed] [Google Scholar]
- Moen P, Kaduk A, Kossek EE, Hammer L, Buxton OM, O’Donnell E, Casper L. Is work-family conflict a multilevel stressor linking job conditions to mental health? Evidence from the work, family and health network. Research in the Sociology of Work. 2015;26:177–217. doi: 10.1108/S0277-283320150000026014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moen P, Kelly EL, Fan W, Lee SR, Almeida D, Kossek EE, Buxton OM. Does a flexibility/support organizational initiative improve high-tech employees well-being? Evidence from the work, family, and health network. American Sociological Review. 2016;81(1):134–164. doi: 10.1177/0003122415622391. [DOI] [Google Scholar]
- Nomaguchi KM. Change in work-family conflict among employed parents between 1977 and 1997. Journal of Marriage and Family. 2009;71(1):15–32. doi: 10.1111/j.1741-3737.2008.00577.x. [DOI] [Google Scholar]
- Olson R, Crain TL, Bodner TE, King R, Hammer LB, Klein LC, Buxton OM. A workplace intervention improves sleep: Results from the randomized controlled work, family, and health study. Sleep Health. 2015;1(1):55–65. doi: 10.1016/j.sleh.2014.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell DJH, Liossi C, Moss-Morris R, Schlotz W. Unstimulated cortisol secretory activity in everyday life and its relationship with fatigue and chronic fatigue syndrome: A systematic review and subset meta-analysis. Psychoneuroendocrinology. 2013;38(11):2405–2422. doi: 10.1016/j.psyneuen.2013.07.004. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. Vol. 1. Newbury Park, CA: Sage; 2002. [Google Scholar]
- Sapolsky RM, Romero LM, Munck AU. How do glucocorticoids influence stress responses? Integrating permissive, suppressive, stimulatory, and preparative actions. Endocrine Reviews. 2000;21(1):55–89. doi: 10.1210/edrv.21.1.0389. [DOI] [PubMed] [Google Scholar]
- Schlotz W, Hellhammer J, Schulz P, Stone A. Perceived work overload and chronic worrying predict weekend-weekday differences in the cortisol awakening response. Psychosomatic Medicineedicine. 2004;66:207–214. doi: 10.1097/01.psy.0000116715.78238.56. [DOI] [PubMed] [Google Scholar]
- Stawski RS, Cichy KE, Piazza JR, Almeida DM. Associations among daily stressors and salivary cortisol: Findings from the national study of daily experiences. Psychoneuroendocrinology. 2013;38(11):2654–2665. doi: 10.1016/j.psyneuen.2013.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ten Brummelhuis LL, Bakker AB. A resource perspective on the work-home interface: The work-home resources model. The American Psychologist. 2012;67(7):545–556. doi: 10.1037/a0027974. [DOI] [PubMed] [Google Scholar]
- Thomas LT, Ganster DC. Impact of family-supportive work variables on work-family conflict and strain: A control perspective. Journal of Applied Psychology. 1995;80(1):6–15. doi: 10.1037/0021-9010.80.1.6. [DOI] [Google Scholar]
- Winslow S. Work-Family conflict, gender, and parenthood, 1977–1997. Journal of Family Issues. 2005;26(6):727–755. doi: 10.1177/0192513X05277522. [DOI] [Google Scholar]
- Wüst S, Federenko I, Hellhammer DH, Kirschbaum C. Genetic factors, perceived chronic stress, and the free cortisol response to awakening. Psychoneuroendocrinology. 2000;25(7):707–720. doi: 10.1016/S0306-4530(00)00021-4. [DOI] [PubMed] [Google Scholar]


