Abstract
The present study examined the relationship between social capital and depressive symptoms and the moderating role of the Big Five personality constructs in a national sample of African American adults. Data were collected from a national probability sample of 803 African American men and women using a telephone survey including measures of the Big Five personality traits, social capital, and depressive symptomatology. Most interestingly, there was evidence for Personality X Social Capital interactions on depressive symptoms. Higher social capital was related to lower depressive symptomology among persons with low conscientiousness, low extraversion, or high neuroticism. However, social capital was significantly but not as strongly related to depressive symptoms among those with high conscientiousness, high extraversion, or low neuroticism. This study reinforces the importance of personality traits when considering potential protective health effects of social capital in understanding depressive symptoms. This information may be useful to practitioners and community members in prevention and treatment.
Keywords: personality, social capital, depression, African American
Introduction
The biopsychosocial model suggests that multiple factors, including personality and community support-related variables such as social capital, contribute to mental health (Chang, Chang, Sanna, & Hatcher, 2008; Giordano & Lindström, 2011; Keefe, 2011; Zellars & Perrewé, 2001). There is substantial evidence of social inequalities affecting the mental health of African Americans (e.g., Utsey & Hook, 2007). Thus it is imperative to understand how psychosocial resources, such as personality and community support-related variables, separately and synergistically, are protective of African Americans’ mental health (Palmer, 2001; Patterson, 2004; Taylor, Chatters, Hardison, & Riley, 2001). The goal of the current research is to examine the synergistic relationship between personality and social capital as it relates to depressive symptoms. Below we will review the relationship between personality and mental health among African Americans.
The Relationship Between Personality and Mental Health Among African Americans
Several studies have explored the relationship between personality and mental health among African Americans. In a sample of African American senior citizens, Baldwin, Jackson, Okoh, and Cannon (2011) found that higher dispositional optimism was related to higher resiliency and lower psychological distress. In another study, African American students who were high in neuroticism were more likely than those low in neuroticism to experience negative affect, intrusive thoughts, and report less forgiveness in response to a racist incident (Pearson et al., 2014). Neuroticism moderated the relationship between some coping strategies and distress in response to a racist incident. For example, the use of humor as a coping strategy was related to lower negative affect for those high in neuroticism. In contrast, for those low in neuroticism, the use of humor was related to higher negative affect (Pearson et al., 2014). Chang (2017) found that loneliness predicted depressive symptoms above that accounted for by perfectionism in a sample of African American college students. Clark, Holt, Wang, Williams, and Schulz (2017) reported that lower levels of openness to experience, conscientiousness, extraversion, and agreeableness as well as higher neuroticism were associated with higher levels of depressive symptoms in a sample of African American adults. In addition to personality related variables, social capital and social support related variables impact mental health.
Social Capital and Depressive Symptomatology
Social capital includes “social networks, emotional bonds and habits of reciprocity that promote trust and cooperation” (Hosen & Solovey-Hosen, 2003). Perry, Williams, Wallerstein, and Waitzkin (2008) found evidence for a three factor model and developed a measure of social capital based on residential community and neighborhood factors including interconnectedness (trust people in community, talk to others in community), social support (able to rely on neighbors for help), and community participation (ability of you and neighbors to influence decisions in the community). The Perry et al. (2008) measure has been used with African American samples (Clark, Holt, Wang, Williams, & Schulz, 2013; Perry et al., 2008). The relevance of social capital also is supported by prior research demonstrating the importance of communalism, kinship, and neighborhoods in the African American community (McAdoo, 2007; Nobles, 1991; Saleem, Busby, & Lambert, 2018).
Next, we review research on the relationship between social capital and mental health. There is little research on social capital and mental health among African Americans. For example, one qualitative study suggested that low income African American parents with limited social capital sometimes rely on the juvenile justice system as a resource for counseling and other mental health services for their at-risk sons (Richardson & Brakle, 2011). Other prior research on the relationship between social capital and mental health among African American adults found that social capital predicted better emotional functioning (Holt, Schulz, Williams, Clark, & Wang, 2012) and was related to fewer depressive symptoms mostly due to the influence of the interconnectedness dimension of social capital (Holt, Clark, Wang, Williams, & Schulz, 2015). In a sample of urban African American mothers who were teenagers when their pre-school age children were born, those reporting more of the community cohesion factor of social capital also reported fewer depressive symptoms (Lewin, Mitchell, Rasmussen, Sanders-Phillips, & Joseph, 2011). Further, participants’ satisfaction with social support aspects of social capital protected against depressive symptoms among those who witnessed violence but exacerbated depressive symptoms among those who reported high victimization (Lewin et al., 2011). In general, the authors suggested that social capital buffered against stress by helping participants cope more adaptively. Snowden (2005) noted that social capital involves engagement, interaction, reciprocity, and trust. He states that these characteristics permit efficient and coordinated action, and reconcile competing interests toward a common goal leading, in turn, to positive outcomes including higher social well-being. He argues that an understanding of social capital is an important step in eliminating racial disparities in mental health.
A relationship between social capital and depressive symptoms also has been found for younger African Americans. Higher social capital was related to lower depressive symptomatology in a sample of African American middle and high school students (Fitzpatrick, Piko, Wright, & LaGory, 2005). In a sample of low income African American adolescents, Stevenson (1998) found that compared to low kinship support students living in high social capital neighborhoods, African American teenagers with low kinship support living in neighborhoods with low social capital reported higher levels of depression. Depression levels did not differ by social capital among high kinship support teens.
The above research suggests that both personality and social capital are related to mental health, in general, and depressive symptoms in particular. Multiple theoretical approaches indicate the benefits of examining these factors simultaneously and investigating any moderation related to depressive symptoms.
Theoretical Frameworks
Several models provide a framework for the current research on the combined importance of personality and social capital to depressive symptoms. All are buffering models in which the negative consequences of risk factors are moderated by protective factors. This suggests an interaction between the two sets of predictor variables. The Psychosocial Resources Model (Fitzpatrick & LaGory, 2000) proposes two sets of resources that contribute to health outcomes. According to this model, first, there are psychological resources such as personality traits or individual differences enabling individuals to cope with challenging situations by moderating life stressors. These might include mastery, self-esteem, social competence, as well as personality traits from the Five Factor Model of Personality such as conscientiousness, extraversion, or agreeableness. Second, there are social resources that originate from one’s formal and informal social networks that serve specific needs. These factors would include family, friends, and neighbors who are important in helping an individual cope with challenging life events (Fitzpatrick & LaGory, 2000). Individuals’ relationships with family, friends, and neighbors comprise social capital. A second model is the Risk and Protective Factors Model (Hawkins, Catalano, & Arthur, 2002) as discussed in Fitzpatrick and LaGory (2000). This model suggests that protective factors can moderate the negative consequences of exposure to risk factors and thereby improve outcomes. Protective factors can include both individual (e.g., personality) and community (e.g., social capital) resources.
A third model is the Person X Environment interactionist approach (Lewin, 1935; Sansone, Morf, & Panter, 2004) which posits that attitudinal and behavioral variables are a function of the relationship between individual (e.g., personality) and environmental factors (e.g., social capital). This model also is related to social cognitive theory (Bandura, 1999). More specifically, the relationship between an individual’s personality and perceived social capital in the environment is consistent with the complementary fit model. This model suggests that the environment and the individual contribute to satisfying the needs of each other (Muchinsky & Monahan, 1987; Piasentin & Chapman, 2006; Verquer, Beehr, & Wagner, 2003). In other words, “the weakness or need of the environment is offset by the strength of the individual, or vice-versa” (Muchinsky & Monahan, 1987). For example, a student in an unsupportive environment is more likely to overcome the obstacles of achieving in school if the student is high in certain personal characteristics, such as conscientiousness.
The above delineated models share a moderation or buffering approach where the influence of one set of variables (e.g., social capital) on depressive symptoms depends on and is modified by the other set of variables (e.g., personality). While not within the scope of this study, we also acknowledge the feasibility of taking a mediational approach to examining the relationship between personality, social capital, and depressive symptoms, especially since social capital (and related constructs such as social support and neighborhood cohesion) is often assessed using a perceived social capital measure rather than some objective assessment of social capital. In other words, the relationship between one’s personality and depressive symptoms may be explained by one’s perception of their social capital. Prior studies of social capital and related constructs, such as social support (reviewed below), have used such measures as proxies for the environmental context.
Personality, Social Capital, and Depressive Symptoms: Prior Research
Several studies have addressed the possible synergistic relationship of personality and social capital with depressive symptoms. In a sample of African American adults, Clark and colleagues (2017) used the complementary fit model to examine the moderator role of personality on the relationship between religious capital (i.e., social support, interconnectedness, and participation in one’s faith community) and depressive symptoms. They found a Conscientiousness X Religious Capital interaction such that higher religious capital was related to fewer depressive symptoms for those low in conscientiousness but not for those high in conscientiousness. They also found a similar moderation relationship between openness to experience and religious capital, but did not find clear evidence for moderation of religious capital’s relationship with depressive symptom by the traits of agreeableness, extraversion, and neuroticism.
While we could not find other research examining the role of personality and social capital on mental health, there are several studies examining the role of personality and social support and community cohesion (components of social capital) in mental health, although some of these studies did not utilize African American samples (Cutrona, Russell, Hessling, Brown, & Murry, 2000; Hoth, Christensen, Ehlers, Raichle, & Lawton, 2007; McHugh & Lawlor, 2012; Mosher, Prelow, Chen, & Yackel, 2006). For example, in a sample of adults with kidney disease, Hoth, Christensen, Ehlers, Raichle, and Lawton (2007) found that agreeableness moderated the role of social support in depressive symptom change. Specifically, they reported that greater social support among highly agreeable adults with kidney disease was associated with a decrease in depressive symptoms over time, while support had little relationship with depressive symptom change for less agreeable patients. In a sample of African American college students, Mosher, Prelow, Chen, and Yackel (2006) found that avoidant coping and social support mediated the relationship between optimism and depressive symptoms. In a sample of African American women, Cutrona et al. (2000) found evidence that under low community cohesion conditions, both high and low positive outlook participants reported relatively high levels of distress. However, under high community cohesion conditions, high positive outlook participants reported lower distress than low positive outlook participants. They also found that under low community social disorder conditions, there was little difference between high positive outlook and low positive outlook participants on distress. However, under high community social disorder conditions, high positive outlook reported lower distress than low positive outlook participants.
Other studies have indicated that social support differentially predicted mental health outcomes among individuals who vary on certain personality traits (Hotard, McFatter, McWhirter, & Stegall, 1989; Oddone, Hybels, McQuoid, & Steffens, 2011; Pai & Carr, 2010; Roberts & Gotlib, 1997; Roos & Cohen, 1987). For example, in a sample of college students, Hotard and colleagues (1989) found that social relationships predicted subjective well-being for introverted, but not extraverted, individuals. They also found that a strong relationship between extraversion and subjective well-being occurred only among persons who were highly neurotic or had poor relationships. Within a group of older patients, Oddone, Hybels, McQuoid, and Steffens (2011) reported that the relationship between both neuroticism and depression varied by level of subjective social support such that those with high subjective social support combined with low neuroticism reported lower depression. Pai and Carr (2010) examined personality, loss of support from a spouse, and relationship to depression in a sample of older adults. They found that extraversion and conscientiousness act as protective factors such that depression related to a spouse’s anticipated rather than sudden death is lowered as the person’s extraversion or conscientiousness level increases. However, there was no evidence of this trend among continually married individuals. Finally, in their study of nurses and burnout, Eastburg, Williamson, Gorsuch, and Ridley (1994) found that compared with introverted nurses, extraverted nurses required more work-related peer support to avoid emotional exhaustion. Very few of the prior studies have specifically examined the relationship between personality, social capital, and depressive symptoms in an African American adult population. The present study seeks to fill the gap in the literature.
The Present Study
The present study examined the moderating role of the Big Five personality traits on the relationship between social capital and depressive symptoms in a sample of African American adults. Previous research suggested a relationship between personality and depressive symptoms (Baldwin et al., 2011; Pearson et al., 2014). Prior research further suggested that social capital, which included the interconnectedness with the community, social support, and the reciprocal relationships, was an important contributor to African American mental health (Holt et al., 2015; Lewin et al., 2011).
Hypotheses
Consistent with buffering models discussed above (Fitzpatrick & LaGory, 2000; Hawkins et al., 2002) and the results of prior research (Clark et al., 2017; Hotard et al., 1989) we predicted that personality will moderate the relationship between social capital and depressive symptoms, especially for (but perhaps not limited to) the personality traits of conscientiousness, extraversion, and openness to experience. More specifically, we predicted a series of Personality Trait x Social Capital interactions. For participants who are low in conscientiousness, low in openness to experience, low in extraversion, low in agreeableness, or high in neuroticism, having higher social capital will be related to fewer depressive symptoms. However, for participants who are high in conscientiousness, high in openness, high in extraversion, high in agreeableness, or low in neuroticism, social capital will be less related to depressive symptoms; these persons will be relatively low in depressive symptoms regardless of the amount of social capital.
Method
Participants and Telephone Survey
The Religion and Health in African Americans (RHIAA) initiative was a national survey designed to test a theoretical model of the religion-health connection. Professional interviewers dialed telephone numbers from a purchased list of U.S. households, comprising a national probability-based sample. A professional sampling firm, Gensys, generated a call list of households from all 50 United States using probability-based methods. The firm obtained phone numbers from publicly available data such as motor vehicle records. Professional interviewers dialed telephone numbers from the call list. The interviewer identified an adult who lived at the household, and then introduced the project. If the contact expressed interest, a brief eligibility screener was administered to determine whether they were African American and age 21 or older. Interested and eligible contacts were read an informed consent script and provided verbal assent. Eligible individuals were self-identified as African American, age 21 or older, and not having had a diagnosis of cancer. Cancer history was an exclusion criterion due to the collection of cancer screening data for another part of the RHIAA initiative. Participants were mailed a $25 gift card upon completion of the 45-minute interview. The study was approved by the University of Maryland and University of Alabama-Birmingham Institutional Review Boards.
A total of 803 African Americans completed the telephone interview (424 women, 379 men). The average age was 56.0 years (SD=15.0), with an age range from 21 to 92 years and indicated a median income in the $30,000 to $40,000 category. Many (40.8%) were married or living with a partner, had a high school education (35.0%) or 1 to 3 years of college (25.8%), and worked full-time (33.1%) or were retired (30.1%). Respondents’ addresses were geocoded and categorized into regions designated by the US Census Bureau. Geographically, our participants were from the Southern (57%), Midwestern (22%), Northeastern (18%), and Western (3%) United States using the US Census regions and the distribution of regional percentages were similar to those reported for African Americans in the 2010 US Census (Rastogi, Johnson, Hoeffel, & Drewery, 2011).
The response rate is calculated as the proportion of complete interviews to the total number of eligible individuals. Only 13 individuals who were screened and eligible refused to participate, resulting in an upper bound response rate of 98% (803/816). The overall response rate is 27%, 803 accepted/(803 accepted + 2,195 refused). Another 379 individuals were not eligible for various reasons: 31 were younger than 21 years, 159 refused to provide an age for use in eligibility screening, and 189 were not African American. A total of 3,390 calls were made (summing each of these dispositions). A brief refusal survey was conducted to compare responders to nonresponders (N=73). Compared to responders, nonresponders were older (M=65.52 years old, SD=15.28 vs. M=56.01 years old, SD=15.00, respectively), more likely to be men (62.0% vs. 47.2%, respectively), less likely to have attended 1 to 3 years of college (14.1% vs. 25.8%, respectively), less likely to have attended a religious service in the past year (70.4% vs. 83.2%, respectively), and less likely to attend religious services four or more times per month (36.6% vs. 47.8%, respectively). Our overall response rate of 27% is similar to those in the Methodology Reports of the National Institutes of Health/National Cancer Institute’s Health Information National Trends Surveys (HINTS) that recruits nationally representative samples of Americans who are asked about their use of health information. HINTS 1 (2003) had a 33% telephone response rate. HINTS 2 (2005) and HINTS 3 (2007) both had a 21% response rate (National Cancer Institute, 2003–2007).
Measures
The NEO Five-Factor Inventory–Form S was used to assess the five factor model (Big Five) personality dimensions (Costa & McCraw, 2004). Conscientiousness was defined as being organized, reliable, hard-working, self-disciplined, punctual, scrupulous, neat, ambitious, and persevering. Extraversion was characterized by being sociable, active, talkative, person-oriented, optimistic, fun-loving, and affectionate. Openness to experience was described as being curious, having broad interests, creative, original, imaginative, and untraditional. Agreeableness was considered as being soft-hearted, good-natured, trusting, helpful, forgiving, gullible, and straight-forward. Neuroticism was characterized as worrying, nervous, emotional, insecure, inadequate, and hypochondrial (Costa Jr, Busch, Zonderman, & McCrae, 1986). The scales assessed Conscientiousness (e.g., “Make plans and stick to them”), Extraversion (e.g., “Make friends easily”), Openness to Experience (e.g., “Enjoy hearing new ideas”), Agreeableness (e.g., “Accept people as they are”), and Neuroticism (e.g., “Have frequent mood swings”). Each of these personality traits was measured by five items. Participants responded on a Likert-type scale (1=strongly disagree to 5=strongly agree). Higher scores indicate more of the trait. Both convergent and discriminant validity have been established (Costa, 1996; Piedmont & Weinstein, 1994). This is a widely used instrument based on the NEO Personality Inventory with high internal consistency (α=0.76-0.90). Internal consistencies were also adequate for the current sample: Conscientiousness α=0.77, Extraversion α=0.75, Openness to Experience α=0.67, Neuroticism α=0.79, and Agreeableness α=0.75.
Social capital was operationalized as resources gained through involvement with one’s community. Using a systematic process, Perry et al. (2008) developed a theory-based social capital scale and evaluated its psychometric properties. The social capital measure includes an interconnectedness dimension (e.g., “Would you say most people in this community can be trusted”), a social support dimension (e.g., “If a medical emergency arose in your home, would you be likely to call on your neighbors for help”), and a community participation dimension (e.g., “Would you say you can influence decisions that affect your community”). The items concentrate on neighbors and neighborhood. Validity of the scale is supported by Perry et al. (2008) who derived the items from the epidemiological, community psychology, and public health intervention literatures and reported evidence for an inverse relationship with perceived barriers to healthcare and a positive correlation with satisfaction with healthcare. Validity of the scale is also supported by Holt et al. (2015) who found a positive correlation between social capital and emotional functioning.
The social capital scale items were originally assessed on a yes/no/don’t know format but a 4-point Likert-type format was used in the current study (1=strongly disagree to 4=strongly agree) to better capture variability in our sample. The three factors are somewhat intercorrelated (Clark et al., 2013). Higher scores indicated greater social capital and the overall scale demonstrated good internal reliability in the present sample (α=0.83).
Depressive symptoms were assessed with the short form (20 items) of the Center for Epidemiological Studies Depression Scale [CES-D; (Radloff, 1977)]. The CES-D was selected because it has been previously validated with an African American population (Makambi, Williams, Taylor, Rosenberg, & Adams-Campbell, 2009; Roth, Ackerman, Okonkwo, & Burgio, 2008). Participants were asked the frequency of depressive symptoms in the past (e.g., “I had crying spells” and “I felt that everything I did was an effort”; rarely/less than 1 day… all of the time/5-7 days). Higher scores indicate more depressive symptomatology. Test-retest reliability and internal consistency were high in previous normal and patient populations (α=0.87). Reliability using the current study’s data was acceptable (α=0.88).
A standard demographic module was also administered. The items assessed several participant characteristics including gender, age, education, and household income before taxes. For education, participants were asked “What is the highest grade or year of school you completed?” Responses were coded as one of eight options: Never attended school or only attended kindergarten, grades 1 through 8 (elementary), grades 9 through 11 (some high school), grade 12 or GED (high school graduate), college 1 year to 3 years (some college or technical school), college 4 years or more (college graduate), master’s degree, doctoral or other advanced degree (e.g., law, medicine). For income, participants were asked “What is the total income of everyone in your household per year, before taxes?” with 8 response categories (Less than $5,000, $5,001 - $10,000, $10,001 - $20,000, $20,001 - $30,000, $30,001 - $40,000, $40,001 - $50,000, $50,001 - $60,000, More than $60,000). Finally, as noted above, respondents’ addresses were geocoded and categorized into regions designated by the US Census Bureau (South, Midwest, Northeast, West).
Results
Overview
We performed five multiple regression analyses, one for each personality trait with the outcome variable being depressive symptomatology. Guided by the buffering/moderation models discussed above, we were interested in examining moderation relationships of personality and social capital on depressive symptoms. With our telephone interview methodology, we used our perceived social capital measure as a proxy for a more objective assessment of social capital. For each regression, we entered the control variables of age, education, income, and geographical region; the predictor variables of personality (one of the Big Five), social capital, and the Personality X Social Capital interaction (e.g., Conscientiousness main effect, Social Capital main effect, Conscientiousness X Social Capital interaction; see Table 2 for regression analyses). The current analytic sample sizes range from 585 to 671 depending on the analysis.
Table 2.
Summary of Multiple Linear Regression Analyses for the Moderating Role of Study Variables on Depressive Symptoms
| Variable | B | SE B | β | p | R2 |
|---|---|---|---|---|---|
| Model 1: Openness | .17 | ||||
| Age | −1.56 | .74 | −.08 | .035 | |
| Education | −1.69 | .78 | −.09 | .030 | |
| Income | −2.74 | .77 | −.14 | .000 | |
| Geographic Region | 0.26 | .29 | .03 | .370 | |
| Openness | −1.54 | .54 | −.49 | .004 | |
| Social Capital | −0.90 | .45 | −.46 | .043 | |
| Openness X Social Capital | .03 | .02 | .40 | .187 | |
| Model 2: Conscientiousness | .17 | ||||
| Age | −1.51 | .73 | −.08 | .040 | |
| Education | −2.30 | .77 | −.12 | .003 | |
| Income | −2.85 | .77 | −.15 | .000 | |
| Geographic Region | 0.43 | .29 | .06 | .142 | |
| Conscientiousness | −1.74 | .52 | −.57 | .001 | |
| Social Capital | −1.05 | .41 | −.54 | .011 | |
| Conscientiousness X Social Capital | 0.04 | .02 | .55 | .062 | |
| Model 3: Extraversion | .13 | ||||
| Age | −0.94 | .75 | −.05 | .214 | |
| Education | −1.79 | .80 | −.09 | .027 | |
| Income | −3.23 | .79 | −.17 | .000 | |
| Geographic Region | 0.34 | .30 | .04 | .255 | |
| Extraversion | −1.99 | .62 | −.59 | .001 | |
| Social Capital | −1.56 | .49 | −.79 | .001 | |
| Extraversion X Social Capital | 0.06 | .02 | .84 | .012 | |
| Model 4: Agreeableness | .13 | ||||
| Age | −1.31 | .75 | −.07 | .081 | |
| Education | −2.15 | .79 | −.11 | .007 | |
| Income | −3.11 | .79 | −.16 | .000 | |
| Geographic Region | 0.40 | .30 | .05 | .174 | |
| Agreeableness | −1.09 | .65 | −.29 | .093 | |
| Social Capital | −0.75 | .55 | −.39 | .169 | |
| Agreeableness X Social Capital | 0.02 | .03 | .27 | .443 | |
| Model 5: Neuroticism | .38 | ||||
| Age | −1.88 | .63 | −.10 | .003 | |
| Education | −0.12 | .68 | −.01 | .858 | |
| Income | −1.80 | .67 | −.09 | .007 | |
| Geographic Region | 0.04 | .25 | .01 | .864 | |
| Neuroticism | 3.06 | .41 | 1.14 | .000 | |
| Social Capital | 0.39 | .18 | .20 | .027 | |
| Neuroticism X Social Capital | −0.06 | .02 | −.66 | .000 |
Note: SE=standard error.
Correlations
The means, standard deviations, and correlation matrix are displayed in Table 1. All the primary study variables were intercorrelated. Of special note, depressive symptoms were negatively correlated with social capital, openness to experience, conscientiousness, extraversion, agreeableness, but positively correlated with neuroticism. Additionally, social capital was positively correlated with openness to experience, conscientiousness, extraversion, agreeableness, but negatively correlated with neuroticism.
Table 1.
Correlations, Means and Standard Deviations of Study Variables
| Variable | M (SD) | Open | Consc | Extrav | Agree | Neurot | SocialCap | Depress |
|---|---|---|---|---|---|---|---|---|
| Open | 20.10 (3.12) | |||||||
| Consc | 19.74 (3.16) | .53** | ||||||
| Extrav | 19.91 (2.84) | .49** | .48** | |||||
| Agree | 20.97 (2.58) | .50** | .47** | .50** | ||||
| Neurot | 9.96 (3.43) | −.34** | −.29** | −.22** | −.22** | |||
| SocialCap | 25.51 (4.78) | .14** | .23** | .19** | .18** | −.13** | ||
| Depress | 31.02 (9.32) | −.28** | −.27** | −.19** | −.18** | .51** | −.21** |
Note: N=671. Open=Openness to experience; Consc=Conscientiousness; Extrav=Extraversion; Agree=Agreeableness; Neurot=Neuroticism; SocialCap=Social Capital; Depress=Depressive symptoms.
Correlation is significant at the p=.01 level.
Openness to Experience
There was a main effect for Openness to Experience (β=−0.49, p=.004) such that participants who were higher on openness were lower in depressive symptomatology. There was a main effect for Social Capital (β=−0.46, p=.043) such that persons with higher social capital reported lower depressive symptomatology. Contrary to our hypotheses, the Openness X Social Capital interaction was not significant (β=0.40, ns).
Conscientiousness
There was a significant main effect for Conscientiousness (β=−0.57, p=.001) such that higher conscientiousness was associated with lower depressive symptoms. There also was, again, a main effect for Social Capital (β=−0.54, p=.011) such that participants with higher social capital reported lower depressive symptoms. Somewhat consistent with our hypotheses, these effects were qualified by a marginally significant Conscientiousness X Social Capital interaction (β=0.55, p=.062; Figure 1). We performed simple slopes analyses on social capital using the values of +/− 1 standard deviation from the mean for conscientiousness and social capital. For high conscientious participants, there was a significant negative slope in the relationship between social capital and depressive symptoms (b=−1.04, p=.008) indicating that as social capital increased, levels of depressive symptoms decreased. For low conscientious participants, there was also a significant negative slope in the relationship between social capital and depressive symptoms (b=−1.19, p=.01) also indicating that as social capital increased, the levels of depressive symptoms decreased, but the slope was smaller for high conscientious participants compared to low conscientious participants. High conscientious participants were relatively low in depressive symptomatology regardless of social capital level.
Figure 1.
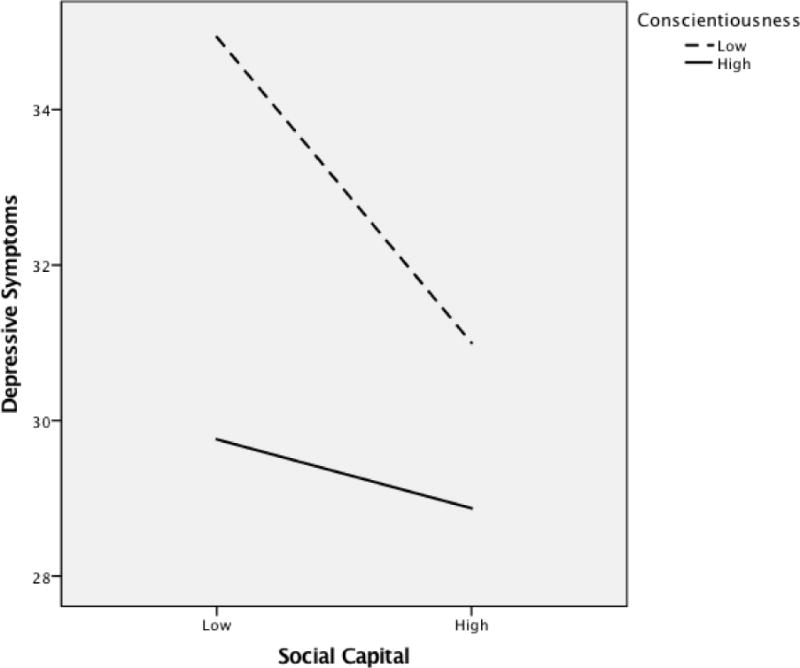
Depressive symptoms as a function of conscientiousness and social capital.
Extraversion
There was a main effect for Extraversion (β=−0.59, p=.001) such that those participants with higher extraversion also reported less depressive symptoms. There was, again, a significant main effect of Social Capital (β=−0.79, p=.001) with individuals with higher social capital reporting lower depressive symptoms. These main effects were qualified by a significant Extraversion X Social Capital interaction (β=0.84, p=.012; Figure 2). We performed simple slopes analyses on social capital using the values of +/− 1 standard deviations from the means for extraversion and social capital. For high extraversion participants, there was a significant negative slope in the relationship between social capital and depressive symptoms (b=−1.51, p=.001) indicating that as social capital increased, levels of depressive symptoms decreased. For low extraversion participants, there was also a significant negative slope in the relationship between social capital and depressive symptoms (b=−1.63, p=.001) indicating that as social capital increased, the levels of depressive symptomatology decreased, but the slope was smaller for high extraversion participants than low extraversion participants. High extraversion participants were relatively low in depressive symptomatology regardless of the level of social capital.
Figure 2.
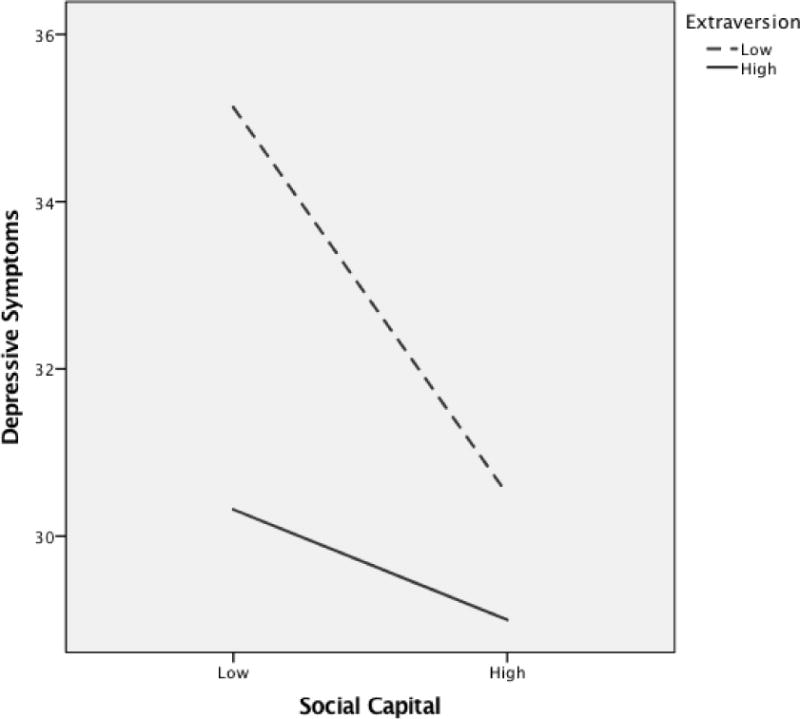
Depressive symptoms as a function of extraversion and social capital.
Agreeableness
There was a marginally significant main effect for Agreeableness (β=−0.29, p=.093) in that participants with higher agreeableness reported less depressive symptoms. Unlike the analyses with the prior personality traits, the main effect for Social Capital was not significant (β=−0.39, ns), so social capital did not uniquely contribute to depressive symptomatology when the personality trait of Agreeableness was included in the regression equation. The Agreeableness X Social Capital interaction was also not statistically significant (β=0.27, ns).
Neuroticism
The main effect for Neuroticism was statistically significant (β=1.14, p<.001) with those reporting higher neuroticism also reporting higher levels of depressive symptomatology. Unlike the prior moderation analyses, there was a significant main effect for Social Capital (β=0.20, p=.027) with participants reporting higher social capital also reporting higher levels (not lower levels) of depressive symptomatology. These effects were qualified by a significant Neuroticism X Social Capital interaction (β=−0.66, p<.001). We performed simple slopes analyses on social capital using the values of +/−1 standard deviation from the means for neuroticism and social capital. Unlike the prior analyses, for high neuroticism participants, there was a significant positive slope in the relationship between social capital and depressive symptoms (b=0.33, p=.044) indicating that as social capital increased, levels of depressive symptomatology increased. Similarly, unlike prior analyses, for low neuroticism participants, there also was a significant positive slope in the relationship between social capital and depressive symptoms (b=0.46, p=.018) indicating that as social capital increased, the levels of depressive symptomatology increased, but the slope was smaller for high neuroticism participants than low neuroticism participants. However, these simple slopes analyses are deceiving since when we graphed the regression equation (Figure 3), the results were consistent with our expectations. Among high neuroticism participants, there was a negative slope indicating that participants with higher social capital reported less depressive symptoms than those with lower social capital (as in most of our other analyses). Among low neuroticism participants, there also was a negative slope indicating that higher social capital participants reported less depressive symptoms that those with lower social capital. However, the slope was smaller than for low neuroticism participants. That is, low neuroticism participants were relatively low on depressive symptoms regardless of their social capital level.
Figure 3.
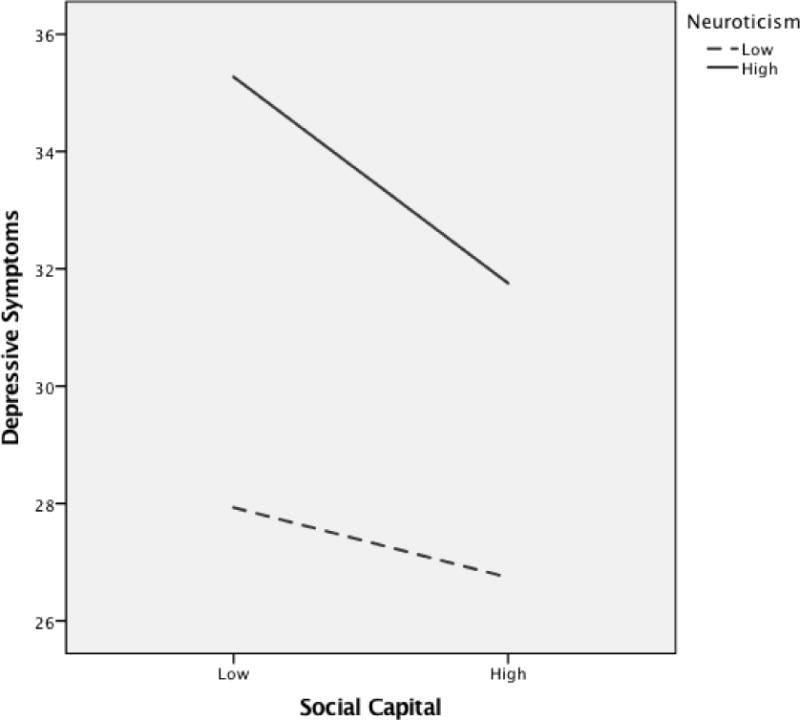
Depressive symptoms as a function of neuroticism and social capital.
Discussion
The biopsychosocial model suggests that multiple factors, including personality and community support-related variables, contribute to mental health (Chang et al., 2008; Keefe, 2011). The current study was guided by theories employing buffering models such as the psychosocial resources model (Fitzpatrick & LaGory, 2000), the risk and protective factors model (Fitzpatrick & LaGory, 2000; Hawkins et al., 2002), and the complementary fit model (Muchinsky & Monahan, 1987) to examine the moderating role of the Big Five personality traits on the relationship between social capital and depressive symptomatology in African Americans. These models posit that the individual’s personality characteristics might buffer the negative characteristics of the environment or the neighborhood in which they live. Given the relevance of communalism, kinship, and neighborhood variables to the African American community, it is important to examine the role of both social capital and personality traits in mental health outcomes (Lewin et al., 2011; McAdoo, 2007; Nobles, 1991). Furthermore, we are aware of no previous studies that have examined the moderating role of personality on the social capital-depressive symptomatology relationship in an African American sample.
Our examination of the relationship between personality, social capital, and depressive symptoms in a national sample of African American adults found that higher levels of conscientiousness, openness to experience, extraversion, and lower levels of neuroticism were related to lower levels of depressive symptoms. Persons high on conscientiousness, openness, extraversion, and low on neuroticism may have higher self-esteem, self-efficacy, or perceived control, which in turn can be protective against depressive symptoms. While higher agreeableness was associated with lower depressive symptoms when examining correlations (Table 1), the unique contribution of agreeableness (main effect) to depressive symptoms was only marginally significant in the regression equation with social capital and the Agreeableness X Social Capital interaction included. We also found fairly consistent evidence that higher social capital was related to lower depressive symptomatology, but with two exceptions. First, social capital was not a unique predictor of depressive symptoms when agreeableness was in the regression equation. Second, when neuroticism was examined as a moderator, social capital was positively (not negatively) related to depressive symptomatology. These issues are discussed below.
These findings must be qualified by the Personality by Social Capital interactions found for conscientiousness, extraversion, and neuroticism. Consistent with buffering models, higher social capital was related to lower depressive symptoms for both high and low levels of conscientiousness and extraversion, however the effect was stronger at low levels of conscientiousness and extraversion. Participants with high levels of conscientiousness and extraversion had relatively low levels of depressive symptoms regardless of social capital levels. Having high social capital, which includes social support, interconnectedness, and community participation, acts as a buffer for those low in conscientiousness or low in extraversion in potentially inhibiting depressive symptoms. Further, an examination of the Figures 1 and 2 suggests that those who are low on both social capital and conscientiousness/extraversion have the highest level of depressive symptoms.
Interestingly and contrary to the hypotheses, the Agreeableness x Social Capital interaction and the Openness X Social Capital interactions were not significant. The lack of moderation for agreeableness seems to contradict the results of Hoth et al. (2007). However, Hoth et al. used a social support measure that differed significantly from our social capital measure. Additionally, the Hoth et al. study employed a longitudinal design and examined change in depressive symptoms over 1.5 years among a sample of chronic kidney patients, whereas our analysis was cross-sectional and utilized a national sample.
Further, lack of an Agreeableness X Social Capital interaction could be explained by the shared variance between agreeableness, social capital, and depressive symptomatology (Table 1). In the regression analysis with agreeableness, social capital, and their interaction, the social capital main effect was not significant in predicting depressive symptoms, as it was in the regression equations with the other four personality traits, suggesting shared variance between the three variables. Being agreeable may be an important factor in eliciting social support, making connections, and participating in the community which are the factors that comprise social capital.
Neuroticism was related to higher depressive symptomatology and the Neuroticism X Social Capital interaction was significant but the simple slopes analyses unexpectedly suggested that for high neuroticism participants, there was a significant positive slope (not negative slope as in the other analyses) in the relationship between social capital and depressive symptoms indicating that as social capital increased, levels of depressive symptomatology increased. For low neuroticism participants, there also was a significant positive (not negative) slope in the relationship between social capital and depressive symptoms also indicating that as social capital increased, the levels of depressive symptomatology increased, however the slope was somewhat smaller for high neuroticism participants than low neuroticism participants. This is similar to the findings of Clark and colleagues (2017) in their investigation of religious capital. However, when we graphed the regression equation (Figure 3), the results were more consistent with expectations in that higher social capital was related to lower depressive symptoms for those high in neuroticism, but this social capital effect was weaker for those low in neuroticism; those low in neuroticism are relatively low in depressive symptoms regardless of social capital level. We suspect that the misleading simple slopes findings indicate statistical suppression due mostly to the relatively high correlation between neuroticism (worrying, self-pitying, etc.) and depressive symptoms (r=0.51; Table 1). Consistent with the other moderation analyses reported above, social capital is significantly and negatively correlated with depressive symptomatology (r=−0.21; Table 1). The correlation between neuroticism and social capital may reflect the discomfort and anxiety that high neuroticism persons feel about issues related to capital, such as social support, interconnectedness, and community participation.
The current study largely corresponds with prior research. Our results are consistent with Fitzpatrick et al. (2005), as well as other studies, who found that higher social capital was related to lower depressive symptoms. Our results also found moderation or protective effects similar to prior research. For example, our results were similar to those of Stevenson (1998) who found that low kinship support combined with low social capital (compared to low kinship support combined with high social capital) was related to lower depressive symptoms. Our results are similar to Clark, et al. (2017) who reported that conscientiousness and openness helped protect against depressive symptoms for African American participants’ with low religious capital. The current study found moderation of social capital by conscientiousness, extraversion, and neuroticism, but not agreeableness or openness. Our results are consistent with Oddone et al. (2011) who reported that social support combined with low neuroticism was associated with lower depressive symptoms. Our results are also commensurate with Pai and Carr (2010) who found that conscientiousness and extraversion protect against depressive symptoms after a spouse’s anticipated (but not sudden) death.
However, some of the current study’s findings were less consistent with prior studies. As noted, Hoth et al. (2007) found that social support’s relationship with depressive symptoms was moderated by agreeableness, whereas agreeableness was not a significant moderator in the current study. Finally our results were contrary to those of Eastburg et al. (1994) who found that extraverted nurses required more (not less) work-related support to avoid emotional exhaustion. This difference may be due to Eastburg and colleagues examining work-related support instead of social capital and emotional exhaustion as an outcome instead of depressive symptoms.
Limitations of the Present Study
There are limitations to the present study. We rely on participants’ self-report of the personality, social capital, and depressive symptoms. Participants may misreport on these scales due to social desirability concerns or recall bias. Additionally, this is a cross-sectional study and we did not randomly assign participants to conditions and manipulate an independent variable, so we cannot infer causation. Another limitation is that our social capital measure, based on the measure developed by Perry et al. (2008), included some items that were phrased in a hypothetical manner (e.g., “If a medical emergency arose…”) instead of asking participants to recall actual experiences (e.g., “When you experienced emergencies, how many times…”), although the latter would be open to the self-report problems mentioned above. Also related to social capital measurement, further research should be done on developing more objective or concrete measures of social capital (e.g., number/type of community organizations). Further, while we utilized a large, national sample of African American men and women, our sample is not representative of all African American adults and there were some differences between responders and nonresponders. Also, most of our participants were from the southern United States (57%), but our distribution of participants across regions (described above) is similar to 2010 US Census data for African Americans (Rastogi et al., 2011). In addition, our minimum age for inclusion in the study was 21 years old, excluding younger adults, ages 18-20 years, from our sample. This decision was guided by the National Institutes of Health’s (NIH) who funded the research. At the initiation of data collection, the NIH’s definition of adult was 21 years or older. If we had collected data from persons under 21 years old, we would have needed parental consent, which was not feasible using our telephone interview methodology. Still, the average age of the sample may also have been older than national averages because older adults (e.g., those who are retired) may be more likely to be available for a lengthy telephone interview.
Future Research, Applications, and Conclusions
Future research should examine these personality, social capital, and depressive symptoms longitudinally to provide more insight into possible causal relationships. Using a cross-lagged panel design, examining personality, social capital, and depressive symptoms over several months or years would provide additional information about causal directions. Relatedly, the stress generation hypothesis suggests a different causal sequence, such that personality may influence depression, which in turn may lead to perceptions of lower social capital or self-selecting into lower social capital environments (Alloy, Liu, & Bender, 2010; Hammen, 1991). These issues would be best tested by mediation analyses utilizing a prospective design (Alloy et al., 2010). Another causal path suggested by prior research was that persons with certain personality traits or individual differences may be better (or worse) at increasing their social capital (e.g., elicit social support, make beneficial connections with others, participate in community activities), which in turn may influence mental health (Mosher et al., 2006; Swickert, 2009). Another potential area for future research would be to carry out an in-depth examination of what facets of each of the personality traits (e.g., some of the facets of extraversion are warmth, assertiveness, and activity) and what factors of social capital (e.g., interconnectedness) are most important in predicting depressive symptoms and other aspects of mental health. Prior research suggests that the interconnectedness and community cohesion aspects of social capital might be particularly important in protecting African Americans against depressive symptoms (Holt et al., 2015; Lewin et al., 2011). To better capture the complexity of personality and similar to Vollrath and Torgersen (2002), future research may examine different clusters of personality traits in these relationships (e.g., comparing those who are both high conscientiousness and low extraversion with those who are both low conscientiousness and high extraversion). These clusters of traits could be combined with reports of social capital to predict depressive symptoms. Finally, the current study only examined depressive symptoms while future research could examine other psychopathology outcomes.
Understanding the synergistic role of personality and social capital may help mental health professionals better tailor their interventions for their clients. This could be especially beneficial for African Americans given the importance of kinship, neighborhood, and collectivism to African Americans (McAdoo, 2007; Nobles, 1991) and their relationship to social capital. For example, Gilbert, Harvey, and Belgrave (2009) describe culturally sensitive interventions for African American youth based on an Africentric approach that impact attitudes, individual differences, and the utilization of social capital. Constantine, Redington, and Graham (2009) note that when African Americans experience distress, their social network is often viewed as a resource for assistance. They, and others (Boyd-Franklin, 2006) also suggest developing interventions that encourage African American clients to use community support systems, including family, friends, mentors, and role models. Our research suggests that therapists should recognize that the usefulness of this strategy may vary by the client’s personality. Knowing that an individual with depressive symptoms who also has certain personality traits (e.g., low conscientiousness, low extraversion) would benefit from increased social capital (e.g., interconnectedness with others) might help in developing a specific set of therapeutic goals for the individual. Our results also suggest that individuals with lower social capital might benefit from interventions to change their personality or related attitudes–for example, interventions to increase conscientiousness, extraversion, or decrease neuroticism. Piedmont (2001) found, in a mostly African American sample, that an outpatient drug rehabilitation program significantly changed clients on all of the Big Five personality constructs from pre- to post-treatment over 15 months. These changes in personality may be related to the sense of communalism that is important to increasing their social capital (see the modest but significant correlations between personality and social capital in Table 1). Tailoring interventions for African Americans based on cultural and behavioral factors has been used in changing physical health behaviors and perhaps could be extended to treating mental health in this population. Kreuter et al. (2005) tailored health messages on several variables including personality/individual differences and social capital related variables. The current research may be important in identifying risk factors for depressive symptoms and, relatedly, the prevention of depressive symptoms. Consistent with the buffering models discussed earlier, having certain combinations of personality traits (e.g., high neuroticism, low conscientiousness) and low social capital can forewarn those in an individual’s social network that the person may be at risk for certain mental health problems and allow them to take preventive action. Providing training to family members and community workers can help in these efforts (Fitzpatrick et al., 2005). The current study reinforces the importance of examining personality traits when considering potential protective health effects of social capital in African American communities.
Finally, social capital processes may depend on the racial dynamics and equity within one’s community or nation. Gilbert, Quinn, Goodman, Butler, and Wallace (2013) suggest that comparisons of social capital’s relationship to health among different ethnic groups is needed. Islam, Merlo, Kawachi, Lindstrom, and Gerdtham (2006) found that the association between social capital and health was more consistently reported in countries marked by high poverty and racial segregation than those that were more egalitarian. Song (2011) found that European Americans reported more social capital than African Americans and that social capital mediated the relationship between ethnicity (being Black or being White) and psychological distress, although the mediational model was only marginally significant. In a study of African American adolescents and depression, Fitzpatrick et al. (2005) note that exercising social capital (e.g., sharing a meal, discussing problems) provides social network members with important strategies for managing the individual’s well-being. However, racial discrimination or other negative experiences may lead to feelings of distrust or alienation from formal sources of social capital, such as political, justice, and transportation institutions (Hanks, 2008). Continued research on social capital can help us better understand the role of social networks in fostering personal well-being, in general, and their potential to reduce racial and ethnic disparities in mental health, in particular (Snowden, 2005).
Acknowledgments
The team acknowledges the work of OpinionAmerica, Tina Madison, and Penny Southward who conducted participant recruitment/retention and data collection activities for the present study. We also thank Dr. Caryn Bell for her assistance in securing the geographic region information for the manuscript.
Funding: This work was supported by grants from the Duke University Center for Spirituality, Theology, and Health, through the John Templeton Foundation (#11993), National Institutes of Health/National Cancer Institute (#R01CA105202), and was approved by the University of Alabama – Birmingham (#X051116001) and University of Maryland (#08-0329) Institutional Review Boards.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Alloy LB, Liu RT, Bender RE. Stress generation research in depression: a commentary. International Journal of Cognitive Therapy. 2010;3(4):380–388. doi: 10.1521/ijct.2010.3.4.380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baldwin DR, Jackson D, III, Okoh I, Cannon RL. Resiliency and optimism: An African American senior citizen’s perspective. Journal of Black Psychology. 2011;37(1):24–41. doi: 10.1177/0095798410364394. [DOI] [Google Scholar]
- Bandura A. Social cognitive theory of personality. In: Pervin LA, John OP, Pervin LA, John OP, editors. Handbook of personality: Theory and research. New York, NY, US: Guilford Press; 1999. pp. 154–196. [Google Scholar]
- Boyd-Franklin N. Black families in therapy: Understanding the African American experience. New York, NY: The Guilford Press; 2006. [Google Scholar]
- Chang E. Perfectionism and Loneliness as Predictors of Depressive and Anxious Symptoms in African American Adults: Further Evidence for a Top-Down Additive Model. Cognitive Therapy & Research. 2017;41(5):720–729. doi: 10.1007/s10608-017-9843-z. [DOI] [Google Scholar]
- Chang R, Chang EC, Sanna LJ, Hatcher RL. Optimism and pessimism as personality variables linked to adjustment. In: Boyle GJ, Matthews G, Saklofske DH, Boyle GJ, Matthews G, Saklofske DH, editors. The SAGE handbook of personality theory and assessment, Vol 1: Personality theories and models. Thousand Oaks, CA, US: Sage Publications, Inc; 2008. pp. 470–485. [Google Scholar]
- Clark EM, Holt CL, Wang MQ, Williams BR, Schulz E. The relationship between spiritual and health locus of control and social and religious capital. Counseling et spiritualité. 2013;32(2):105–121. doi: 10.2143/CS.32.2.3017319. [DOI] [Google Scholar]
- Clark EM, Holt CL, Wang MQ, Williams BR, Schulz E. Which personality traits moderate the relationship between religious capital and depressive symptomology in a national sample of African Americans? Journal of Black Psychology. 2017;43(5):517–537. doi: 10.1177/0095798416654835. [DOI] [Google Scholar]
- Constantine MG, Redington RM, Graham SV. Counseling and psychotherapy with African Americans. In: N HA, Tynes BM, Utsey SO, editors. Handbook of African American Psychology. Thousand Oaks, CA: SAGE Publications; 2009. [Google Scholar]
- Costa PT, Jr, Busch CM, Zonderman AB, McCrae RR. Correlations of MMPI Factor Scales With Measures of the Five Factor Model of Personality. Journal of Personality Assessment. 1986;50(4):640. doi: 10.1207/s15327752jpa5004_10. [DOI] [PubMed] [Google Scholar]
- Costa PT., Jr Work and personality: Use of the NEO-PI-R in industrial/organisational psychology. Applied Psychology: An International Review. 1996;45(3):225–241. doi: 10.1111/j.1464-0597.1996.tb00766.x. [DOI] [Google Scholar]
- Costa PT, Jr, McCraw RR. NEO Personality Inventory–Form S. Psychological Assessment Resources, Inc; 2004. [Google Scholar]
- Cutrona CE, Russell DW, Hessling RM, Brown PA, Murry V. Direct and moderating effects of community context on the psychological well-being of African American women. Journal of Personality and Social Psychology. 2000;79(6):1088–1101. doi: 10.1037/0022-3514.79.6.1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eastburg MC, Williamson M, Gorsuch R, Ridley C. Social support, personality, and burnout in nurses. Journal of Applied Social Psychology. 1994;24(14):1233–1250. doi: 10.1111/j.1559-1816.1994.tb00556.x. [DOI] [Google Scholar]
- Fitzpatrick KM, LaGory M. Unhealthy places: The ecology of risk in the urban landscape. New York, NY: Routledge; 2000. [Google Scholar]
- Fitzpatrick KM, Piko BF, Wright DR, LaGory M. Depressive Symptomatology, Exposure to Violence, and the Role of Social Capital Among African American Adolescents. American Journal of Orthopsychiatry. 2005;75(2):262–274. doi: 10.1037/0002-9432.75.2.262. [DOI] [PubMed] [Google Scholar]
- Gilbert DJ, Harvey AR, Belgrave FZ. Advancing the Africentric paradigm shift discourse: Building toward evidence-based Africentric interventions in social work practice with African Americans. Social Work. 2009;54(3):243–252. doi: 10.1093/sw/54.3.243. [DOI] [PubMed] [Google Scholar]
- Gilbert KL, Quinn SC, Goodman RM, Butler J, Wallace J. A meta-analysis of social capital and health: A case for needed research. Journal of Health Psychology. 2013;18(11):1385–1399. doi: 10.1177/1359105311435983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giordano GN, Lindström M. Social capital and change in psychological health over time. Social Science & Medicine. 2011;72(8):1219–1227. doi: 10.1016/j.socscimed.2011.02.029. [DOI] [PubMed] [Google Scholar]
- Hammen C. Generation of stress in the course of unipolar depression. Journal of Abnormal Psychology. 1991;100(4):555–561. doi: 10.1037//0021-843x.100.4.555. [DOI] [PubMed] [Google Scholar]
- Hanks CA. Social capital in an impoverished minority neighborhood: Emergence and effects on children's mental health. Journal of Child and Adolescent Psychiatric Nursing. 2008;21(3):126–136. doi: 10.1111/j.1744-6171.2008.00145.x. [DOI] [PubMed] [Google Scholar]
- Hawkins JD, Catalano RF, Arthur MW. Promoting science-based prevention in communities. Addictive Behaviors. 2002;27(6):951–976. doi: 10.1016/s0306-4603(02)00298-8. [DOI] [PubMed] [Google Scholar]
- Holt CL, Schulz E, Williams B, Clark EM, Wang MQ. Social, religious, and spiritual capital and physical/emotional functioning in a national sample of African Americans. Journal of Community and Applied Social Psychology. 2012;22(4):346–362. doi: 10.1002/casp.1116. [DOI] [Google Scholar]
- Holt CL, Clark EM, Wang MQ, Williams BR, Schulz E. The religion–health connection among African Americans: What is the role of social capital? Journal of Community and Applied Social Psychology. 2015;25(1):1–18. doi: 10.1002/casp.2191. [DOI] [Google Scholar]
- Hosen R, Solovey-Hosen D. The instructional value of fostering social capital in the classroom. Journal of Instructional Psychology. 2003;30:84–92. [Google Scholar]
- Hotard SR, McFatter RM, McWhirter RM, Stegall ME. Interactive Effects of Extraversion, Neuroticism, and Social Relationships on Subjective Well Being. Journal of Personality & Social Psychology. 1989;57(2):321–331. [Google Scholar]
- Hoth K, Christensen A, Ehlers S, Raichle K, Lawton W. A Longitudinal Examination of Social Support, Agreeableness and Depressive Symptoms in Chronic Kidney Disease. Journal of Behavioral Medicine. 2007;30(1):69–76. doi: 10.1007/s10865-006-9083-2. [DOI] [PubMed] [Google Scholar]
- Islam MK, Merlo J, Kawachi I, Lindström M, Gerdtham UG. Social capital and health: Does egalitarianism matter? A literature review. International Journal for Equity in Health. 2006;5:3–28. doi: 10.1186/1475-9276-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keefe FJ. Behavioral medicine: A voyage to the future. Annals of Behavioral Medicine. 2011;41(2):141–151. doi: 10.1007/s12160-010-9239-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreuter MW, Skinner CS, Holt CL, Clark EM, Haire-Joshu D, Fu Q, Steger-May K, Booker AC, Bucholtz DC. Cultural tailoring for mammography and fruit and vegetable consumption among low-income African American women in urban public health centers. Preventive Medicine. 2005;41(1):53–62. doi: 10.1016/j.ypmed.2004.10.013. [DOI] [PubMed] [Google Scholar]
- Lewin A, Mitchell SJ, Rasmussen A, Sanders-Phillips K, Joseph JG. Do human and social capital protect young African American mothers from depression associated with ethnic discrimination and violence exposure? Journal of Black Psychology. 2011;37(3):286–310. doi: 10.1177/0095798410381242. [DOI] [Google Scholar]
- Lewin K. A dynamic theory of personality. New York, NY, US: McGraw-Hill; 1935. [Google Scholar]
- Makambi KH, Williams CD, Taylor TR, Rosenberg L, Adams-Campbell LL. An assessment of the CES-D scale factor structure in black women: The Black Women’s Health Study. Psychiatry Research. 2009;168(2):163–170. doi: 10.1016/j.psychres.2008.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAdoo H. Black families. 2007 Retrieved 2018/05/03. [Google Scholar]
- McHugh JE, Lawlor BA. Social support differentially moderates the impact of neuroticism and extraversion on mental wellbeing among community-dwelllng older adults. Journal of Mental Health. 2012;21(5):448–458. doi: 10.3109/09638237.2012.689436. [DOI] [PubMed] [Google Scholar]
- Mosher CE, Prelow HM, Chen WW, Yackel ME. Coping and Social Support as Mediators of the Relation of Optimism to Depressive Symptoms among Black College Students. Journal of Black Psychology. 2006;32(1):72–86. [Google Scholar]
- Muchinsky PM, Monahan CJ. What is Person-Environment Congruence? Supplementary versus Complementary Models of Fit. Journal of Vocational Behavior. 1987;31(3):268–277. [Google Scholar]
- National Cancer Institute. Health Informatics national Trends Survey (HINTS) Rockville, MD: National Institutes of Health; 2003–2007. Retrieved March 3, 2017 from https://hints.cancer.gov/data/methodology-reports.aspx. [Google Scholar]
- Nobles WW. African philosophy: Foundations for black psychology. In: Jones RL, Jones RL, editors. Black psychology. Berkeley, CA, US: Cobb & Henry Publishers; 1991. pp. 47–63. [Google Scholar]
- Oddone CG, Hybels CF, McQuoid DR, Steffens DC. Social support modifies the relationship between personality and depressive symptoms in older adults. The American Journal of Geriatric Psychiatry. 2011;19(2):123–131. doi: 10.1097/JGP.0b013e3181f7d89a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pai M, Carr D. Do personality traits moderate the effect of late-life spousal loss on psychological distress? Journal of Health and Social Behavior. 2010;51(2):183–199. doi: 10.1177/0022146510368933. [DOI] [PubMed] [Google Scholar]
- Palmer CJ., Jr African Americans, depression, and suicide risk. Journal of Black Psychology. 2001;27:100–111. [Google Scholar]
- Patterson KL. A longitudinal study of African American women and the maintenance of a healthy self-esteem. Journal of Black Psychology. 2004;30(3):307–328. [Google Scholar]
- Pearson MR, Derlega VJ, Henson JM, Holmes KY, Ferrer RA, Harrison SB. Role of neuroticism and coping strategies in psychological reactions to a racist incident among African American university students. Journal of Black Psychology. 2014;40(1):81–111. doi: 10.1177/0095798412471682. [DOI] [Google Scholar]
- Perry M, Williams RL, Wallerstein N, Waitzkin H. Social capital and health care experiences among low-income individuals. American Journal of Public Health. 2008;98(2):330–336. doi: 10.2105/AJPH.2006.086306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piasentin KA, Chapman DS. Subjective Person-Organization Fit: Bridging the Gap between Conceptualization and Measurement. Journal of Vocational Behavior 2006;69:202–221. [Google Scholar]
- Piedmont RL, Weinstein HP. Predicting supervisor ratings of job performance using the NEO personality inventory. Journal of Psychology. 1994;128(3):255. [Google Scholar]
- Piedmont RL. Cracking the plaster cast: Big five personality change during intensive outpatient counseling. Journal of Research in Personality. 2001;35(4):500–520. doi: 10.1006/jrpe.2001.2326. [DOI] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Rastogi S, Johnson TD, Hoeffel EM, Drewery MP. 2010 Census Briefs. U.S. Census Bureau; 2011. The Black Population: 2010. Retrieved February 2, 2018 from https://www.census.gov/prod/cen2010/briefs/c2010br-06.pdf. [Google Scholar]
- Richardson JB, Jr, Brakle MV. A qualitative study of relationships among parenting strategies, social capital, the juvenile justice system, and mental health care for at-risk African American male youth. Journal of Correctional Health Care. 2011;17(4):319–328. doi: 10.1177/1078345811413081. [DOI] [PubMed] [Google Scholar]
- Roberts JE, Gotlib IH. Social support and personality in depression: Implications from quantitative genetics. In: Pierce GR, Lakey B, Sarason IG, Sarason BR, Pierce GR, Lakey B, Sarason IG, Sarason BR, editors. Sourcebook of social support and personality. New York, NY, US: Plenum Press; 1997. pp. 187–214. [Google Scholar]
- Roos PE, Cohen LH. Sex roles and social support as moderators of life stress adjustment. Journal of Personality and Social Psychology. 1987;52(3):576–585. doi: 10.1037/0022-3514.52.3.576. [DOI] [PubMed] [Google Scholar]
- Roth DL, Ackerman ML, Okonkwo OC, Burgio LD. The four-factor model of depressive symptoms in dementia caregivers: A structural equation model of ethnic differences. Psychology and Aging. 2008;23(3):567–576. doi: 10.1037/a0013287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saleem FT, Busby DR, Lambert SF. Neighborhood social processes as moderators between racial discrimination and depressive symptoms for african american adolescents. Journal of Community Psychology. 2018 doi: 10.1002/jcop.21970. [DOI] [Google Scholar]
- Sansone C, Morf CC, Panter AT. The Sage handbook of methods in social psychology. Thousand Oaks, CA, US: Sage Publications, Inc; 2004. [Google Scholar]
- Snowden LR. Racial, cultural and ethnic disparities in health and mental health: toward theory and research at community levels. American Journal Of Community Psychology. 2005;35(1–2):1–8. doi: 10.1007/s10464-005-1882-z. [DOI] [PubMed] [Google Scholar]
- Song L. Social capital and psychological distress. Journal of Health and Social Behavior. 2011;52(4):478–492. doi: 10.1177/0022146511411921. [DOI] [PubMed] [Google Scholar]
- Stevenson HC. Raising safe villages: Cultural-ecological factors that influence the emotional adjustment of adolescents. Journal of Black Psychology. 1998;24(1):44–59. doi: 10.1177/00957984980241004. [DOI] [Google Scholar]
- Swickert R. Personality and social support. In: Corr PJ, Mattews G, editors. The Cambridge Handbook of Personality Psychology. Cambridge, UK: Cambridge University Press; 2009. [Google Scholar]
- Taylor RJ, Chatters LM, Hardison CB, Riley A. Informal social support networks and subjective well-being among African Americans. Journal of Black Psychology. 2001;27(4):439–463. [Google Scholar]
- Utsey SO, Hook JN. Heart rate variability as a physiological moderator of the relationship between race-related stress and psychological distress in African Americans. Cultural Diversity and Ethnic Minority Psychology. 2007;13(3):250–253. doi: 10.1037/1099-9809.13.3.250. [DOI] [PubMed] [Google Scholar]
- Verquer ML, Beehr TA, Wagner SH. A Meta-Analysis of Relations between Person-Organization Fit and Work Attitudes. Journal of Vocational behavior 2003;63:473–489. [Google Scholar]
- Vollrath M, Torgersen S. Who takes health risks? A probe into eight personality types. Personality & Individual Differences. 2002;32(7):1185. [Google Scholar]
- Zellars KL, Perrewé PL. Affective Personality and the Content of Emotional Social Support: Coping in Organizations. Journal of Applied Psychology. 2001;86(3):459–467. doi: 10.1037/0021-9010.86.3.459. [DOI] [PubMed] [Google Scholar]


