Abstract
Background:
Up to 40% of patients with idiopathic clubfoot who are treated with the Ponseti method experience recurrence of deformity. Many of these patients receive surgery (e.g., anterior tibial tendon transfer). An alternative approach for recurrent clubfoot is repeat Ponseti casting. The purpose of this study was to evaluate the outcome of repeat Ponseti casting in the treatment of recurrent clubfoot.
Methods:
Patients with recurrent idiopathic clubfoot who were treated at our hospital, between 2004 and 2012, with repeat serial casting and bracing (the recurrent group) were eligible for inclusion in the study. The recurrent group and a control group of randomly selected patients seen during the same period who had not had recurrence were compared with respect to demographic data, age at the time of treatment, number of casts, subsequent surgical intervention(s), and the Disease-Specific Instrument (DSI) clubfoot scale. Patients were deemed to have a successful outcome if they had a well-corrected foot (defined as dorsiflexion of ≥10°, hindfoot in valgus, and a straight lateral border) at the time of follow-up.
Results:
Of a total of 71 eligible patients with clubfeet, 35 patients participated. At the time of follow-up, success rates were 74% for the recurrent group and 83% for the control group. Dorsiflexion past neutral was significantly higher in the control group than the patient group (20° versus 12°, respectively; p < 0.001). Ninety-five percent of the control subjects had a straight lateral border in comparison with 78% in the recurrent group (p = 0.004). Likewise, 97% of controls had the hindfoot in valgus in comparison with 80% of the recurrent group (p = 0.02). There was a significant difference in the ability to squat (76% in the control group and 43% in the recurrent group; p = 0.03). There was no difference between groups in the total outcome of the DSI.
Conclusions:
Recurrence was seen in 19% (71) of 382 children who were eligible for our study who were typically discharged after the age of 5 years from our clinic, indicating the importance of continued follow-up until after that age. Treatment with casting was successful in many patients and may be a reasonable choice for recurrent idiopathic clubfeet.
Level of Evidence:
Therapeutic Level III. See Instructions for Authors for a complete description of levels of evidence.
Idiopathic clubfoot, a congenital defect with a prevalence of 0.64 to 6.8 per 1,000 births1, is characterized by fixed equinus and hindfoot varus with inversion and adduction of the midfoot and forefoot2. Without correction, clubfoot leads to substantial deformity and disability3.
The Ponseti method has become the standard treatment for the correction of idiopathic clubfoot. This primarily noninvasive method has excellent long-term outcomes, with <5% of patients requiring extensive surgical intervention4,5. The result of this treatment has been reported to be superior to extensive surgical release with respect to deformity correction, reduced risk of overcorrection, and improved functional outcome3,6,7. After initial successful treatment with the Ponseti method, however, up to 40% of patients experience recurrence. Possible causes for recurrence include the intrinsic contractile nature of the soft tissues in clubfoot deformity8, genetic and neuromuscular factors, casting techniques9, different designs of braces9, and variable brace wear time due to parental nonadherence10,11. Currently, many children with recurrence receive an anterior tibial tendon transfer as a primary approach to treat the relapse5,12.
The purpose of this study was to evaluate the outcomes for patients with idiopathic clubfoot who were treated with repeat casting and bracing for recurrent clubfoot after initial correction with successful Ponseti treatment.
Materials and Methods
The research ethics board at The Hospital for Sick Children approved this study, and all parents provided informed consent to participate.
Study Population
The study population included a consecutive series of patients with idiopathic clubfoot who were treated at our hospital between January 2004 and December 2012. Patients were identified through orthopaedic clinic lists. Eligible patients were followed for at least 2 years. Eligible patients included those who had received Ponseti treatment at our hospital before the age of 6 months, irrespective of previous treatment elsewhere. Patients were excluded if they had not been treated according to the Ponseti protocol, had treatment at a different hospital, had received surgery (other than Achilles tenotomy), had an incomplete medical record, or had nonidiopathic clubfoot (i.e., a chromosomal or connective tissue-related disorder, myopathy or myotonic dystrophy, amniotic band, or positional clubfoot), a syndromic deformity (e.g., arthrogryposis or cerebral palsy), or an associated neurological disorder.
The recurrent group was a consecutive series of patients with idiopathic clubfoot who had an initial successful correction with Ponseti casting and bracing but subsequently developed a recurrence. As it was not possible to determine the exact time at which a patient developed a recurrence, recurrence was defined as the date when it was determined that the clubfoot required further intervention to restore a satisfactory functional position (alignment and range of motion). We randomly selected a control group of subjects from patients who had not had recurrence prior to December 31, 2014. If patients had been managed with recasting soon after the initial Ponseti treatment because of skin issues or to bridge a small period when a brace was not worn (e.g., because of the wrong size of the boots), they were classified as not having a recurrence. While the ideal comparison group would have been patients treated with an anterior tibial tendon transfer, this was not performed as initial treatment for recurrence at our hospital.
Information gathered included demographic data (sex, age at presentation, age at recurrence, and age at the time of follow-up), laterality of the clubfoot, whether the clubfoot was complex (defined as having a rigid equinus, severe plantar flexion of all metatarsals, a deep crease above the heel, a transverse crease in the sole of the foot, and a short hyperextended first toe)13, the number of initial casts (including post-tenotomy cast), surgical interventions, and length of follow-up.
Initial Ponseti Treatment
Patients had a cast applied weekly according to the standard Ponseti protocol3. Percutaneous Achilles tenotomy was performed in the clinic when the foot stopped improving in range and the child had <15° of dorsiflexion. Patients wore the final cast following the tenotomy for 3 weeks. Children were prescribed boots and bars that were to be worn full time for 3 months and then during the nighttime until the patient was at least 4 years old. Clubfoot correction was defined as the date at which the patient began wearing boots and bars following the initial Ponseti casting.
Casting Protocol for Recurrence
In our clinic, the criteria for casting includes (1) evidence of no dorsiflexion beyond neutral and (2) clinical examination of passive range of motion that indicates some degree of response to passive stretching of soft tissues (i.e., not a fixed-end feel). The criteria for surgery for clubfoot include failure of casting to achieve or maintain dorsiflexion beyond neutral, i.e., the foot is in equinus and/or has a varus hindfoot. Dynamic supination during swing phase is an indication to add a tibial tendon transfer to any surgical procedure. The primary course of treatment of recurrence was repeating the Ponseti casting, typically biweekly cast changes, for 6 to 8 weeks. Patients who were <4 years old resumed wearing boots and bars at nighttime at the completion of casting. For some patients, the nighttime use of boots and bars was combined with the application of an articulated ankle-foot orthosis (AFO) during the daytime. For patients who had not adhered to the use of boots and bars, an AFO was prescribed for full-time wear. Our AFO protocol included a dorsiflex-assist lateral hinge, and a flexible foot bed to facilitate peroneal recruitment and normal toe-off in the gait pattern. All further follow-up visits occurred every 6 months until patients were discharged from the clinic.
Questionnaire
The Disease-Specific Instrument (DSI) questionnaire for patients with clubfoot combines a number of questions to provide a total DSI score, a Function Subscale, and a Satisfaction Subscale14. Scores from 90 to 100 were considered “excellent”; from 80 to 89, “good”; from 70 to 79, “fair”; and <70, poor.
Outcome Measures
Patients were evaluated in the clinic for a follow-up examination. Physical examination included whether the foot was plantigrade (yes or no), the alignment of the hindfoot (valgus, neutral, or varus), and the nature of the lateral border (straight or curved). Dorsiflexion was assessed with the use of a goniometer. The primary outcome measure of “success” was defined as not having received surgery for a recurrence and having all of the following: hindfoot in valgus, dorsiflexion of ≥10°, and a straight lateral border. Some children had received multiple casting treatments for repeated recurrences.
Secondary outcome measures included the percentage of patients who achieved a plantigrade foot, had a straight lateral border, and had hindfoot alignment, and the degrees of dorsiflexion. Patient function and satisfaction were assessed using the DSI for patients with clubfoot (see Appendix)14. Data collected were entered into a password-protected electronic database created using REDCap (Research Electronic Data Capture) software15.
Statistical Methods
The Fisher exact test was used to compare all categorical variables. The Wilcoxon rank-sum test was used for continuous variables.
Results
Study Population
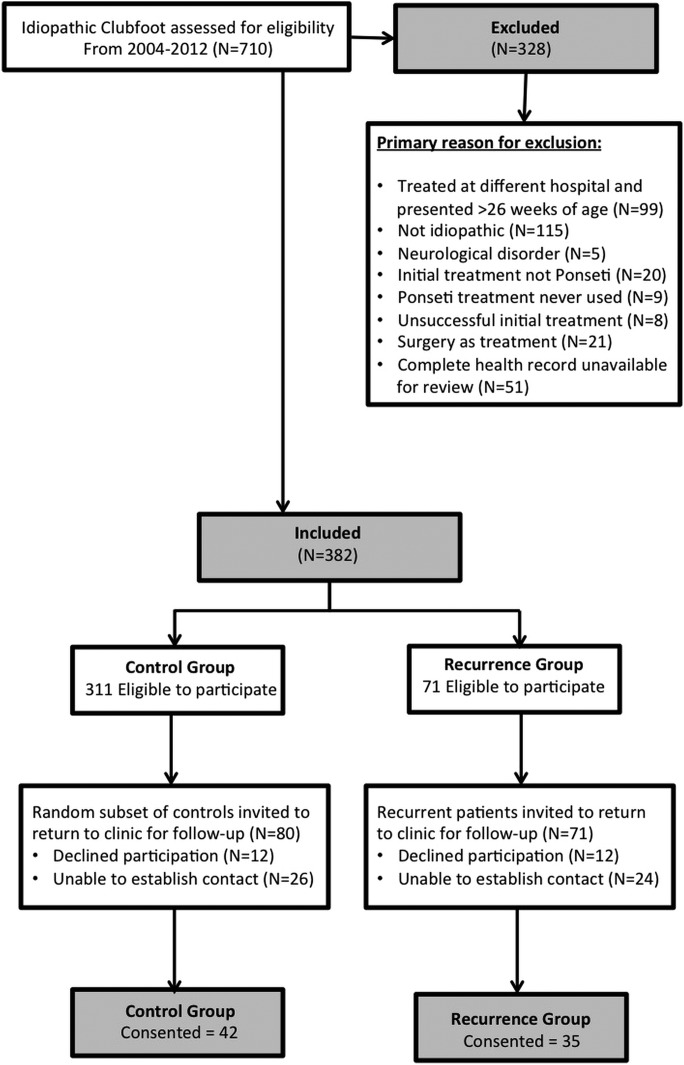
A total of 710 patients with clubfoot were treated at our hospital between 2004 and 2012 and were followed for 2 years. Two trained physiotherapists, whose sole clinical focus was clubfoot, led the clubfoot treatment. We previously reported the results of a physiotherapist-led clinic, and the results were superior to a physician-led clinic4,5. Of the 710 patients, 382 met the inclusion criteria for participation in this study. Of this group, 71 patients (19%) had a recurrence, and 35 of them (49 feet) were available to be seen in the clinic. The control group of 42 patients (63 feet) who had not had a recurrence were randomly selected from the 311 patients successfully treated for clubfoot. Figure 1 represents a flowchart of the study patients. There was no significant difference between patients and controls in terms of sex (p = 0.22) and age at presentation (p = 0.75); both groups were seen at approximately 5 to 6 weeks of age. There was also no difference between the 2 groups with respect to follow-up (p = 0.26). The groups did not differ in terms of complexity (p = 0.69) of the clubfoot or laterality (p = 0.17). The groups did not differ with respect to the percentage of feet receiving tenotomies (p = 0.81) (Table I). Twenty-seven patients in the control group and 41 in the recurrent group reported brace wear for a minimum of 12 hours, and 24 patients in the control group and 41 in the recurrent group reported nighttime brace wear.
Fig. 1.
Flowchart showing participant inclusion and exclusion criteria and participation information.
TABLE I.
Baseline Information at Initial Treatment
| Characteristic | Recurrent Group (N = 35) | Control Group (N = 42) | P Value |
| Sex (no. [%]) | 0.22 | ||
| Male | 22 (63) | 32 (76) | |
| Female | 13 (37) | 10 (24) | |
| Age* | |||
| At presentation (wk) | 5.34 ± 4.34 (0-17) | 6.55 ± 6.31 (1-22) | 0.75 |
| At first recurrence†‡ (mo) | 40.97 ± 29.95 (3-107) | 76.00 ± 25.11 (39-122) | 0.01 |
| At time of follow-up (mo) | 90.94 ± 33.08 (39-144) | 82.60 ± 31.81 (35-141) | 0.26 |
| Duration of follow-up* (mo) | 89.58 ± 33.10 (35.75-141) | 81.63 ± 31.27 (34.50-140.5) | 0.28 |
| Complex presentation (no. [%]) | 4 (11) | 3 (7) | 0.69 |
| Laterality§ (no. [%]) | 0.17 | ||
| Bilateral | 15 (43) | 21 (50) | |
| Left foot | 13 (37) | 7 (17) | |
| Right foot | 7 (20) | 14 (33) | |
| No. of casts per participant*† | 5.63 ± 1.42 (2-9) | 4.90 ± 1.43 (1-8) | 0.04 |
| Tenotomy performed# (no. [%]) | 23 (66) | 27 (64) | 0.81 |
Data are given as the mean and the standard deviation, with the range in parentheses.
Significant difference (α < 0.05).
Seven control patients had recurrence.
One participant with bilateral recurrence at study follow-up had recurrence only in the right foot.
Tenotomy information was not available for 1 participant in the recurrent group.
Outcome
Recurrence
The mean age when recurrence was first treated was 41 months (range, 3 to 107 months) in the recurrent group. Of 35 patients in the recurrent group, 19 had 1 recurrence, 9 had 2 recurrences, 4 had 3 recurrences, 2 had 4 recurrences, and 1 had 5 recurrences. Of 42 patients in the control group who had satisfactory correction as of December 31, 2014, 7 had a recurrence when they were invited back to the clinic for a follow-up visit.
Eighty-three percent of the control group compared with 74% of the recurrent group had a successful result at the time of follow-up (p = 0.40). The control and recurrent groups were compared on several foot measurements. Control subjects had significantly better dorsiflexion (p < 0.001) and valgus hindfoot position (p = 0.02), and more had a straight lateral border (p = 0.004). Control subjects and patients did not differ with respect to the percentage of feet that were plantigrade (p = 0.08), and most were in valgus. A significant difference was detected with respect to the ability to squat, with 76% of control subjects versus 43% of patients in the recurrent group being able to do so (p = 0.03) (Table II). When patients with a successful result in the control group (Figs. 2-A and 2-B) and the recurrent group (Figs. 3-A and 3-B) were compared, the only significant difference in the foot measurements was the degrees of dorsiflexion (p < 0.001) (Table III). Of those with 1 recurrence, 18 had a successful outcome and 1 did not; of those with ≥2 recurrences, 8 had a successful outcome and 8 did not (p = 0.004). Of the patients with 1 or 2 recurrences, 22 had a successful outcome and 6 did not; of those with ≥3 recurrences, 4 had a successful outcome and 3 did not (p = 0.26). Thus, while the success rate decreased with the number of recurrences, no number of castings was found to be associated with universally unsuccessful outcome.
Figs. 2-A and 2-B Photographs, made during the follow-up visit, of a patient with successfully corrected clubfoot. The left foot was treated with casting for recurrence of clubfoot.
Fig. 2-A.

Note the slightly curved lateral border of the left foot.
Fig. 2-B.

The hindfoot on the left foot is close to neutral, while the hindfoot of the right foot is in valgus.
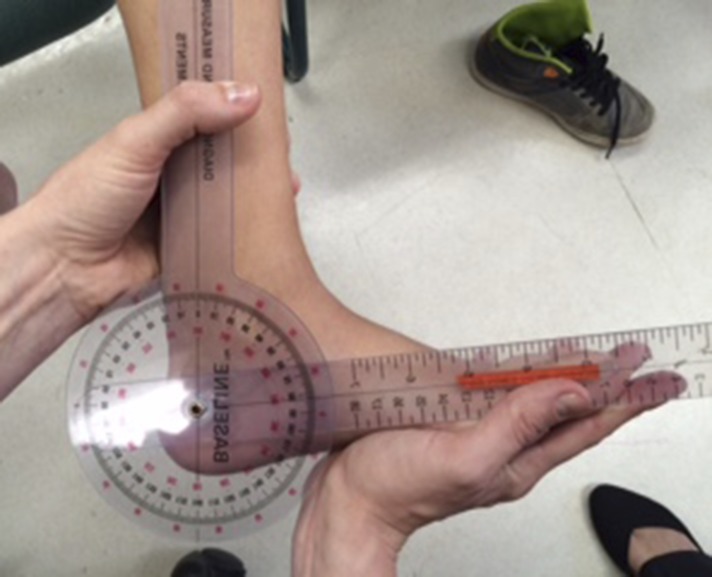
Figs. 3-A and 3-B A patient who was previously treated for recurrence of clubfoot in his left foot.
Fig. 3-A.

The patient was not able to squat.
Fig. 3-B.
He had no recurrence of clubfoot on the left side during the follow-up visit, but the range of motion was limited (dorsiflexion of 7°). A goniometer was used to perform this measurement.
TABLE II.
Residual and Recurrent Deformity and Range and Outcome Scores at Time of Follow-up for All Patients
| Variable | Recurrent Group (N = 49 Feet) | Control Group (N = 63 Feet) | P Value |
| Dorsiflexion*† (deg) | 12.2 ± 8.93 | 19.51 ± 7.37 | <0.001 |
| Hindfoot position† (no. [%] of feet) | 0.02 | ||
| Valgus | 39 (80) | 61 (97) | |
| Neutral or varus | 8 (16) | 2 (3) | |
| Unknown | 2 (4) | 0 (0) | |
| Plantigrade position (no. [%] of feet) | 0.08 | ||
| Plantigrade | 46 (94) | 63 (100) | |
| Not plantigrade | 3 (6) | 0 | |
| Straight lateral border† (no. [%] of feet) | 0.004 | ||
| Yes | 38 (78) | 60 (95) | |
| No | 10 (20) | 2 (3) | |
| Unknown | 1 (2) | 1 (2) | |
| Ability to squat†‡ (no. [%] of patients) | 0.03 | ||
| Yes | 15 (43) | 32 (76) | |
| No | 13 (37) | 8 (19) | |
| Unknown | 7 (20) | 2 (5) | |
| Disease-Specific Instrument score§ | |||
| Total score | 83.35 ± 15.24 (50.03-100) | 88.09 ± 12.53 (53.37-100) | 0.19 |
| Function subscale | 85.52 ± 16.71 (40.04-100) | 87.84 ± 18.84 (33.38-100) | 0.29 |
| Satisfaction subscale | 81.17 ± 17.72 (46.70-100) | 88.34 ± 13.97 (46.72-100) | 0.06 |
The values are given as the mean and the standard deviation.
Significant difference (α < 0.05).
Data are recorded per patient, with 35 in the recurrent group and 42 in the control group.
The values are given as the mean and the standard deviation, with the range in parentheses. The questionnaire was completed by 29 patients in the recurrent group and 40 in the control group.
TABLE III.
Residual and Recurrent Deformity and Range and Outcome Scores at Time of Follow-up for Patients with a Successful Outcome in Both Groups
| Variable | Recurrent Group (N = 37 Feet) | Control Group (N = 53 Feet) | P Value |
| Dorsiflexion*† (deg) | 14.54 ± 5.16 | 20.58 ± 6.82 | <0.001 |
| Hindfoot position (no. [%] of feet) | 0.40 | ||
| Valgus | 34 (92) | 53 (100) | |
| Neutral or varus | 1 (3) | 0 | |
| Unknown | 2 (5) | ||
| Plantigrade position (no. [%] of feet) | >0.9 | ||
| Plantigrade | 37 (100) | 53 (100) | |
| Not plantigrade | 0 | 0 | |
| Straight lateral border (no. [%] of feet) | >0.9 | ||
| Yes | 35 (95) | 50 (94) | |
| No | 1 (3) | 2 (4) | |
| Unknown | 1 (3) | 1 (2) | |
| Ability to squat‡ (no. [%] of patients) | 0.11 | ||
| Yes | 14 (56) | 30 (86) | |
| No | 7 (28) | 5 (14) | |
| Unknown | 4 (16) | 0 | |
| Disease-Specific Instrument§ | |||
| Total score | 86.68 ± 13.83 (50.03-100) | 89.71 ± 10.64 (60.03-100) | 0.41 |
| Function subscale | 87.88 ± 15.48 (46.68-100) | 90.79 ± 15.82 (40.04-100) | 0.26 |
| Satisfaction subscale | 85.47 ± 15.05 (53.38-100) | 88.64 ± 14.16 (46.72-100) | 0.30 |
The values are given as the mean and the standard deviation.
Significant difference (α <0.05).
Data are recorded per patient, with 25 patients with a successful outcome in the recurrent group and 35 in the control group.
The values are given as the mean and the standard deviation, with the range in parentheses. Questionnaire was answered by 22 patients in the recurrent group and 34 patients in the control group.
Questionnaire
While scores were higher in the control group, no difference was found between the groups with respect to function or satisfaction scores on the DSI for clubfeet, whether the comparison included all patients or only those with a successful outcome (Tables II and III). Both groups had excellent to good outcomes.
Discussion
The primary treatment of clubfoot has shifted from extensive clubfoot release to the Ponseti method. Most patients treated with the Ponseti method, compared with those managed with extensive release, had a more flexible and functional foot3,6,16. However, up to 40% of patients treated with the Ponseti method have been reported to have a recurrence9. While the indications for further treatment remain unclear, many patients with recurrence receive some form of surgical treatment including an anterior tibial tendon transfer9.
After an average age of 7 years of follow-up in our study, 74% of the patients in the recurrent group who had repeat Ponseti casting had a satisfactory outcome. We chose a control group of patients who had not had a recurrence and who had been discharged from clinic care to determine if recurrent clubfoot treated with casting could achieve outcomes similar to those in a group of patients without recurrence. Not surprisingly, patients treated for a recurrence had a successful outcome less frequently than a control group of patients. While the patients who had received treatment for a recurrence and had a successful outcome were able to dorsiflex the ankle past neutral, the range of motion was less than that in the control group. Thus, while most patients with recurrent clubfoot can be treated with casting, the results are not the same as those for patients who do not have recurrent clubfoot.
Multiple factors could explain why the results were different in the 2 groups. First, it is unknown whether there was a difference between the groups with respect to brace wear adherence, which is known to be a key factor behind recurrence10,11. Secondly, the group that had recurrence may have had a more severe deformity because of some genetic factor(s). Thus, treatment in this group would be less effective.
Another interesting observation regarding our study is that some patients, for whom regular follow-up visits had already been discontinued (which is typically done at the age of 5 years), had a recurrence of the clubfoot when they returned for the follow-up visit conducted for the purposes of the study. Discontinuation of follow-up visits at the age of 5 years is in line with the statement by Ponseti that recurrences in fully and partially corrected feet are rare after that age17. We used the intention-to-treat principle in comparing our recurrent and control groups, whereby we classified patients as those who had a recurrence or those who had not (the control subjects) as of December 2014 and compared their results at a research follow-up visit. Interestingly, although failure was less common in the control group than in the recurrent group, 7 (17%) of the 42 control patients did not meet our criteria of success at the time of follow-up. For these 7 patients who did not have fully corrected feet during the follow-up, the ultimate outcome is uncertain. Mild or early recurrences may be hard to detect17, and thus some patients may have an incompletely corrected clubfoot yet have reasonable function in the long term. However, the finding of a substantial percentage of unsatisfactory feet after an average follow-up of >7 years in our study suggests that patients should be followed until at least until the age of 7 years. Patients with clubfoot should be followed past this age.
There are multiple aspects of recurrence, with some that are more responsive to serial casting and others that are more indicative of the need for surgical intervention. Loss of normal alignment and range of motion, particularly in the subtalar and ankle joints, usually represent some degree of soft-tissue contracture, which is more likely to respond to serial manipulation and casting. Inherent muscle weakness in the peronei (evertors), either primary or secondary to loss of alignment, is more likely to ultimately require further surgery, specifically anterior tibial tendon transfer.
After Ponseti treatment, 19% to 40% of patients needed further treatment for recurrence7. Commonly, patients with recurrent clubfoot receive an anterior tibial tendon transfer. Thus, the better control group for our study would have been a group of patients treated with anterior tibial tendon transfer for the primary relapse. However, at our hospital, all patients received casting as the first approach to primary relapse, rather than an anterior tibial tendon transfer. Anterior tibial tendon transfer, performed to treat the muscle imbalance between the anterior tibial tendon and the antagonists, has been reported to restore balance fully in 87% and partially in 11% of patients18. While anterior tibial tendon transfer might restore balance in the foot, patients treated with anterior tibial tendon transfer for recurrence and residual deformity after initial treatment with the Ponseti method have been reported to have a 40% recurrence rate after surgery19. Many of these patients required additional surgical procedures19. The failure rate of 40% is higher than that observed in our patients who were managed with casting19. Furthermore, the mean age at the time of follow-up in the study by Park et al., in 2009, was only 3.6 years, which suggests that a longer follow-up period might have yielded an even higher recurrence rate19. Thus, patients who have a recurrence after initial success with Ponseti casting are difficult to treat with whatever method. There is high variability in patients who present for surgical intervention after repeated relapse, as well as in the causes of relapse. Reserving surgery for only those who have failure after repeat casting might reduce the number of repeat surgeries for these children. Repeated surgery for residual and recurrent clubfeet can result in stiff, painful, and arthritic feet later in life6,7.
There are several limitations to this study. First, as noted above, our control group consisted of patients with nonrecurrent clubfeet. It would also be beneficial to compare outcomes with those of surgically managed clubfoot relapse. Second, some patients were lost to follow-up, so it is possible that we did not capture all recurrences in our recurrent group. There was also substantial variability in the number of recurrence episodes in the study group (range, 1 to 5 recurrences), which could affect the response to treatment and the failure rate. The patients who had multiple episodes of casting were offered, but the families refused, surgery. In general, after 1 or 2 episodes of casting for recurrence, further casting is unlikely to achieve success. While we cannot comment specifically, casting at an early age may be more effective.
In conclusion, using Ponseti casting for recurrent idiopathic clubfoot achieved a satisfactory result in most patients. Although outcomes in the recurrent group were somewhat less successful than in the nonrecurrent group, casting appears to have reduced the number of children receiving surgery. Longer follow-up of patients is required to identify the prevalence of recurrent deformity.
Appendix
A table showing the DSI questionnaire for patients with clubfoot is available with the online version of this article as a data supplement at jbjs.org (http://links.lww.com/JBJS/E692).
Acknowledgments
Note: The authors thank Gurpreet Lakhanpal, Kate Gargan, and Stephanie Cho for their help on this project.
Footnotes
Investigation performed at The Hospital for Sick Children (SickKids), Toronto, Ontario, Canada
A commentary by R. Mervyn Letts, MD, MSc, FRCSC, is linked to the online version of this article at jbjs.org.
Disclosure: Internal funding was provided by the Robert B. Salter Chair. The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJS/E691).
References
- 1.Barker S, Chesney D, Miedzybrodzka Z, Maffulli N. Genetics and epidemiology of idiopathic congenital talipes equinovarus. J Pediatr Orthop. 2003. Mar-Apr;23(2):265-72. Epub 2003 Feb 27. [PubMed] [Google Scholar]
- 2.Hefti F. Pediatric orthopedics in practice. New York: Springer; 2015. p 425-8. [Google Scholar]
- 3.Morcuende JA. Congenital idiopathic clubfoot: prevention of late deformity and disability by conservative treatment with the Ponseti technique. Pediatric annals. 2006. February;35(2):128-30, 32-6. [DOI] [PubMed] [Google Scholar]
- 4.Janicki JA, Narayanan UG, Harvey BJ, Roy A, Weir S, Wright JG. Comparison of surgeon and physiotherapist-directed Ponseti treatment of idiopathic clubfoot. J Bone Joint Surg Am. 2009. May;91(5):1101-8. Epub 2009 May 5. [DOI] [PubMed] [Google Scholar]
- 5.Mayne AI, Bidwai AS, Beirne P, Garg NK, Bruce CE. The effect of a dedicated Ponseti service on the outcome of idiopathic clubfoot treatment. Bone Joint J. 2014. October;96-B(10):1424-6. [DOI] [PubMed] [Google Scholar]
- 6.van Gelder JH, van Ruiten AG, Visser JD, Maathuis PG. Long-term results of the posteromedial release in the treatment of idiopathic clubfoot. J Pediatr Orthop. 2010. Oct-Nov;30(7):700-4. Epub 2010 Sep 25. [DOI] [PubMed] [Google Scholar]
- 7.Halanski MA, Davison JE, Huang JC, Walker CG, Walsh SJ, Crawford HA. Ponseti method compared with surgical treatment of clubfoot: a prospective comparison. J Bone Joint Surg Am. 2010. February;92(2):270-8. Epub 2010 Feb 4. [DOI] [PubMed] [Google Scholar]
- 8.Colburn M, Williams M. Evaluation of the treatment of idiopathic clubfoot by using the Ponseti method. J Foot Ankle Surg. 2003. Sep-Oct;42(5):259-67. [DOI] [PubMed] [Google Scholar]
- 9.Zhao D, Li H, Zhao L, Liu J, Wu Z, Jin F. Results of clubfoot management using the Ponseti method: do the details matter? A systematic review. Clin Orthop Relat Res. 2014. April;472(4):1329-36. Epub 2014 Jan 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Willis RB, Al-Hunaishel M, Guerra L, Kontio K. What proportion of patients need extensive surgery after failure of the Ponseti technique for clubfoot? Clin Orthop Relat Res. 2009. May;467(5):1294-7. Epub 2009 Jan 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dobbs MB, Rudzki JR, Purcell DB, Walton T, Porter KR, Gurnett CA. Factors predictive of outcome after use of the Ponseti method for the treatment of idiopathic clubfeet. J Bone Joint Surg Am. 2004. January;86(1):22-7. [DOI] [PubMed] [Google Scholar]
- 12.Ponseti IV, Campos J. The classic: observations on pathogenesis and treatment of congenital clubfoot. 1972. Clin Orthop Relat Res. 2009. May;467(5):1124-32. Epub 2009 Feb 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ponseti IV, Zhivkov M, Davis N, Sinclair M, Dobbs MB, Morcuende JA. Treatment of the complex idiopathic clubfoot. Clin Orthop Relat Res. 2006. October;451:171-6. Epub 2006 Jun 22. [DOI] [PubMed] [Google Scholar]
- 14.Roye BD, Vitale MG, Gelijns AC, Roye DP., Jr Patient-based outcomes after clubfoot surgery. J Pediatr Orthop. 2001. Jan-Feb;21(1):42-9. Epub 2001 Feb 15. [DOI] [PubMed] [Google Scholar]
- 15.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009. April;42(2):377-81. Epub 2008 Sep 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Haasbeek JF, Wright JG. A comparison of the long-term results of posterior and comprehensive release in the treatment of clubfoot. J Pediatr Orthop. 1997. Jan-Feb;17(1):29-35. Epub 1997 Jan 1. [PubMed] [Google Scholar]
- 17.Ponseti IV. Relapsing clubfoot: causes, prevention, and treatment. Iowa Orthop J. 2002;22:55-6. Epub 2002 Aug 16. [PMC free article] [PubMed] [Google Scholar]
- 18.Thompson GH, Hoyen HA, Barthel T. Tibialis anterior tendon transfer after clubfoot surgery. Clin Orthop Relat Res. 2009. May;467(5):1306-13. Epub 2009 Feb 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Park SS, Kim SW, Jung BS, Lee HS, Kim JS. Selective soft-tissue release for recurrent or residual deformity after conservative treatment of idiopathic clubfoot. J Bone Joint Surg Br. 2009. November;91(11):1526-30. Epub 2009 Nov 3. [DOI] [PubMed] [Google Scholar]